Abstract
Objective:
Driving after drinking (DAD) among college students remains a significant public health concern and is perhaps the single riskiest drinking-related behavior. Counselor-delivered and web-based Brief Alcohol Interventions (BAIs) have been shown to reduce DAD among college students, but to date no study has evaluated the efficacy of a single-session mobile phone–based BAI specific to DAD. The present study examined whether a driving-specific BAI delivered via mobile phone would significantly decrease DAD among college students compared to an informational control.
Method:
Participants were 84 college students (67.1% women; average age = 23; 52.4% White) who endorsed driving after drinking two or more drinks at least twice in the past 3 months. After completing baseline measures, participants were randomly assigned to receive either (a) DAD information or (b) DAD mobile BAI that included personalized feedback and interactive text messaging. Participants completed outcome measures at 3-month follow-up.
Results:
Repeated-measures mixed modeling analyses revealed that students receiving the mobile phone–based BAI reported significantly greater reductions in likelihood of DAD (three or more drinks) and the number of drinks consumed before driving than students in the information condition at 3-month follow-up.
Conclusions:
These findings provide preliminary support for the short-term efficacy of a mobile phone–based BAI for reducing DAD among college students.
Driving after drinking (dad) is a national public health concern. Each year more than 10,000 people die as a result of alcohol-related crashes, and costs of alcohol-related traffic accidents total around $59 billion (National Highway Traffic Safety Administration, 2014). Despite widespread prevention efforts, approximately 3.4 million college students (30% of all U.S. college students) report driving after drinking alcohol, and alcohol-related traffic accidents remain the leading cause of alcohol-related death among college students (Hingson et al., 2009).
Although a variety of policy-based public health interventions (i.e., raising the legal drinking age, lowering the legal blood alcohol concentration driving limit, sobriety checkpoints, zero tolerance laws, server training, etc.), campus programs, and media campaigns have been implemented to decrease DAD, the frequency of DAD remains high, particularly among college students (Hingson et al., 2017). Brief alcohol interventions (BAIs) attempt to identify and correct faulty normative beliefs and highlight consequences of alcohol use (such as driving after drinking) in order to increase motivation to change. Recent meta and integrated-analyses indicate that BAIs generally succeed in reducing alcohol use (frequency, quantity, level of intoxication) and a variety of alcohol-related problems (Cronce et al., 2012; Mun et al., 2014), although effect sizes are typically small (Foxcroft et al., 2016; Huh et al., 2015). BAIs typically consist of one or two individual therapeutic meetings (approximately 50 minutes per session; Carey et al., 2007) that are delivered in a motivational interviewing (MI; Miller & Rollnick, 2013) style and include personalized feedback. Personalized feedback is created based on a series of questionnaires completed by students before their BAI session, and although specific feedback components differ by study, a personalized drinking profile, information on social norms, prior alcohol-related consequences experienced by the student (including drinking and driving if endorsed), practical costs (e.g., money spent on alcohol and caloric intake from alcohol), and information on strategies to limit alcohol-related risk are typically included (see Miller et al., 2013). In addition, research suggests that personalized feedback delivered without a one-on-one intervention may effectively reduce alcohol use and problems at short-term follow-ups (up to 4 months; Cadigan et al., 2015).
Previous research has shown that BAIs can successfully reduce DAD among DUI offenders and emergency department patients (Brown et al., 2010; D’Onofrio et al., 2012; Ouimet et al., 2013; Spirito et al., 2004; Wells-Parker & Williams, 2002). Counselor-delivered BAIs can also reduce DAD among college students and other young adults (Monti et al., 1999; Schaus et al., 2009; Teeters et al., 2015). Unfortunately, despite the demonstrated efficacy of BAIs, it is often not feasible for universities to hire and train staff to deliver in-person BAIs to a large number of risky drinking college students. In addition, very few heavy drinking college students seek out alcohol prevention or treatment services available on campus or in the surrounding community (Buscemi et al., 2010), and even when incentivized with research credit it is often difficult to get students to attend in-person sessions. This has led researchers to attempt to develop innovative ways of delivering BAIs to reach a larger audience based on effective components of in-person BAIs (Cronce et al., 2015).
Mobile message–based interventions
BAIs have traditionally been delivered in person or via computer either in the laboratory or remotely delivered via email (White, 2006). Mobile phones are now a ubiquitous form of communication and represent an important alternative delivery method for delivering BAIs. According to the latest data from the Pew Research Center (2017), 100% of Americans ages 18–29 own a cell phone and 97% of cell phone owners in this age group report using their cell phones to send and receive text messages. Evidence from clinical trials indicates that personalized text messages are efficacious in promoting physical activity (Hurling, 2007), weight loss management (Gerber et al., 2009), smoking cessation (Free, 2009), diabetes self-management (Kim, 2007), and medication adherence (Cocosila, 2009).
Although research indicates that participants prefer text messages to telephone calls and emails and rate this medium positively (Moore et al., 2013), only a few published studies in the alcohol literature have implemented a text-messaging intervention. Suffoletto and colleagues (2014) conducted a standardized, automated text-messaging–based intervention with 765 risky drinking young adult emergency department patients and found evidence of decreased alcohol consumption at 3-month follow-up. In addition, Suffoletto and colleagues (2016) examined an automated text-messaging program as a booster to in-person alcohol education classes with college students mandated to complete alcohol education because they violated campus alcohol policies and found decreases in binge drinking over the 6-week textmessaging period and that commitment to a low-risk drinking goal was associated with reductions in binge drinking intentions.
Text messages may be a particularly advantageous way to provide BAIs as they can be highly personalized to the individual, accessed at any time that suits the individual’s needs, and allow for engagement and interaction between the interventionist and participant (Fjeldsoe et al., 2009). By mitigating many potential limitations of traditional web-based feedback—the lack of interaction with a clinician, and the minimal/uncertain comprehension and processing of intervention material—text messaging interventions may represent a valuable method for reaching high-risk drinkers as well as online students who may not be willing to complete an in-person intervention session (Irvine et al., 2012).
Current study
No previously published studies have examined the effects of a DAD-specific BAI among college student drinkers who report recent DAD. The overall goal of the current study is to develop and evaluate a brief, mobile phone–based DAD-focused intervention to decrease DAD among college students. To do this, we delivered an intervention that included text-based motivational interviewing with a clinician combined with personalized feedback elements specifically targeting DAD. We evaluated the efficacy of the mobile phone–based DAD-specific intervention compared to a mobile phone–based generic alcohol information intervention in the context of a randomized two-group (alcohol information vs. DAD-specific personalized feedback) pilot trial with 84 college students. Hypotheses are as follows:
Hypothesis 1.
Students receiving the mobile phone–based DAD intervention would report greater reductions in driving after drinking (three or more drinks) at 3-month follow-up compared to students receiving the mobile phone–based alcohol information intervention.
Hypothesis 2.
Students receiving the mobile phone–based DAD intervention would report significantly greater reductions in the total number of drinks consumed before driving at 3-month follow-up compared to students receiving the mobile phone–based alcohol information intervention.
Method
Participants
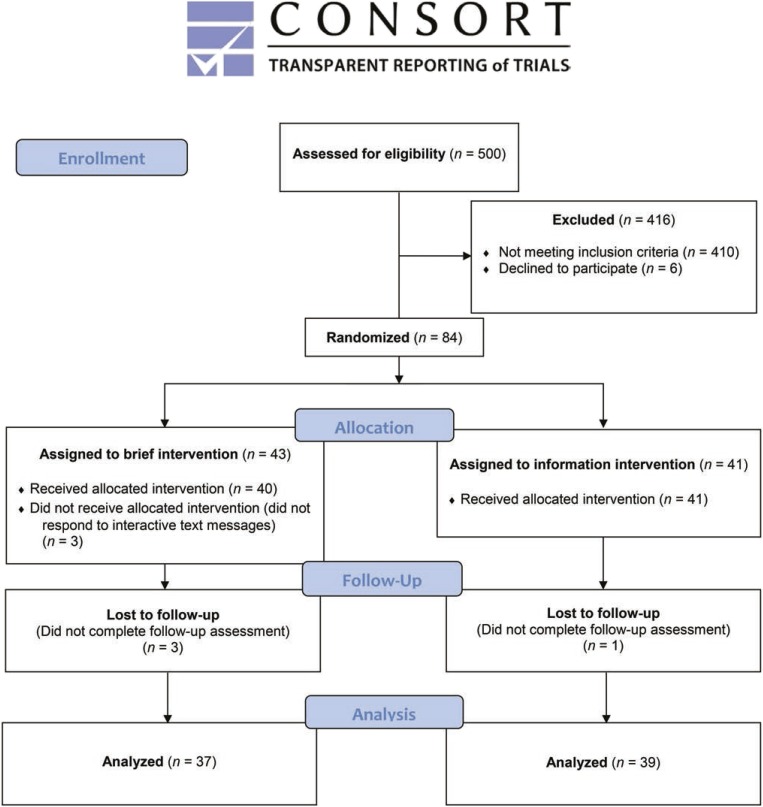
Participants were undergraduate students from an ethnically diverse public university in the southern United States. Students were eligible to participate if they were at least 18 years old, had access to a motor vehicle, and reported driving after drinking two or more drinks at least twice in the past 3 months. If the participant met eligibility criteria, the researcher contacted the participant, explained the project procedures and confidentiality, and invited the participant to participate in further phases of the study. See Figure 1 for a flowchart illustrating recruitment, intervention assignment, and follow-up assessment. Five hundred students (recruited from a university-wide email system, the psychology subject pool, undergraduate classrooms, and by posted flyers) completed a brief (3–5 minute) screening survey to identify those students eligible to participate in this study. One hundred were eligible and 84 agreed to participate in the pilot trial (67.1% women, 32.9% men; 18.3% freshmen, 19.5% sophomores, 34.1% juniors, and 28% seniors). The average age of participants was 22.5 years, SD = 4.99; 64% were older than 21. The sample was ethnically diverse: 52.4% White, 42.7% African American, 4.9% Hispanic or Latino, 1.2% American Indian, 1.2% Native Hawaiian/Pacific Islander, and the remainder not specifying their ethnicity.
Figure 1.
Flowchart illustrating recruitment, intervention, and follow-up assessment. All participation occurred remotely via text messages and email/web links.
Measures
Demographics.
Participants completed a brief questionnaire regarding age, race/ethnicity, and gender.
Alcohol use.
Typical drinks per week were assessed by the Daily Drinking Questionnaire (DDQ; Collins et al., 1985). Students were asked to estimate the total number of standard drinks they consumed on each day during a typical week in the past month. The DDQ is frequently used to assess alcohol consumption patterns among college students and is correlated with self-monitoring and retrospective drinking measures (Kivlahan et al., 1990).
Impaired driving questions
Driving after drinking behavior.
DAD was assessed with questions adapted from prior studies that classified impaired driving as driving after consuming three or more drinks (LaBrie et al., 2011, 2012; Teeters & Murphy, 2015). Participants were also asked how many drinks they had consumed before driving on their most recent driving episode.
Norms.
An open-ended question asking participants to estimate the percentage of drinkers at their university that report past-3-month alcohol-impaired driving was used to assess participants’ normative perception of peer driving after drinking.
Procedures
All procedures were approved by the University Institutional Review Board, and participants were assured that all data would be kept confidential and protected by a federal Certificate of Confidentiality. Participants who met eligibility criteria and agreed to participate completed a remote consent and baseline assessment session via mobile phone. After completing the baseline measures, participants were randomized (stratified by gender) to an alcohol information condition (which provided nonpersonalized information on alcohol use and driving after drinking) or a DAD BAI condition using a random number generator.
Participants were then sent a link via text message to a mobile-optimized secure website containing either their personalized feedback document or a generic alcohol information document. Participants were instructed to view either the informational or the personalized feedback document on their mobile phone and to respond to a number of questions embedded in the documents as a fidelity check. After completing the BAI or information intervention (described below), participants sent a text message indicating completion to the study administrator and were then emailed two documents: the first document contained strategies for avoiding DAD and the second document contained information on substance abuse resources available on campus and in the local community. Participants were informed that they would receive their choice of extra course credit or a $20 Amazon gift card. A follow-up assessment to examine changes in the outcome variables occurred 3 months after the intervention. A text message containing the secure web survey was sent to each participant. Participants received a $20 Amazon gift card or extra credit for completing the follow-up assessment.
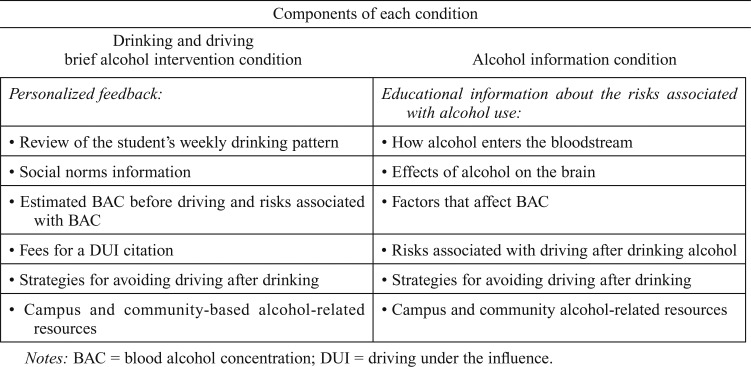
Driving after drinking mobile phone–based brief alcohol intervention.
Following completion of the baseline assessment measures, participants were asked to send a text message to the study administrator verifying completion of all measures. Immediately following receipt of the participant’s completion text message, the study administrator sent the participant a link via text message to a secure mobileoptimized website containing DAD-specific personalized feedback. Feedback included the following elements: a personalized drinking profile and DAD profile, information on social norms related to drinking and DAD, personalized information on BAC before driving, costs associated with a DUI citation, and information on combined drug and alcohol impaired driving risk (if endorsed).
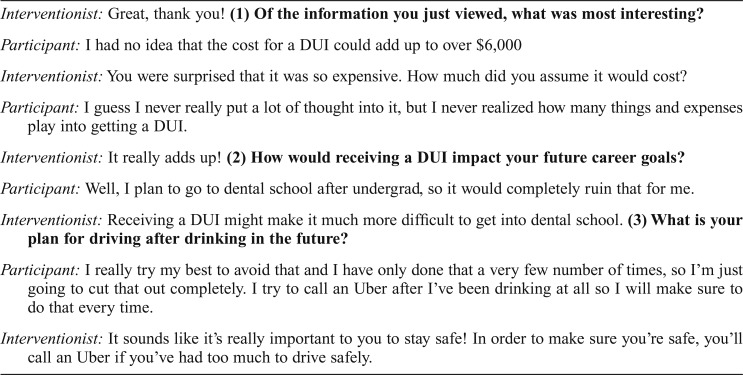
The goals of this session were to raise concern about potential consequences relating to DAD, correct faulty normative perceptions of drinking and DAD behavior, provide information about BAC in relation to driving, and assist students in strategizing means for avoiding future episodes of DAD. Participants were instructed to view the personalized feedback document on their mobile phone and to respond to a number of questions embedded in the feedback document as a comprehension and fidelity check (e.g., “What percentage of college students reported driving after drinking three or more drinks?”). Participants were instructed that they would have an interactive text-message exchange about the feedback with a study research assistant immediately after viewing the personalized feedback document and were asked to send a text message to the study administrator when they were ready to respond to a series of text messages about the feedback document. After confirming receipt and processing of the feedback document, the study administrator immediately1 sent the participant three text messages containing the following open-ended questions (see Table 1 for example conversation): (a) Of the information you just viewed, what was most interesting, (b) how would receiving a DUI impact your future career goals, and (c) what is your plan for driving after drinking in the future? Consistent with MI style, based on participant responses to these standardized open-ended questions, the interventionist sent personalized follow-up text message reflections and further open-ended questions to convey empathy, develop discrepancy, and/or facilitate goal setting. All interventionists were trained in MI, and a licensed clinical psychologist with expertise in MI supervised the text messaging interactions. The interactive text messages were expected to enhance intervention retention/processing and to provide an interpersonal/interactive element that may enhance efficacy (Walters et al., 2009).
Table 1.
Example of (de-identified) interactive text messaging session
| Interventionist: Great, thank you! (1) Of the information you just viewed, what was most interesting? |
| Participant: I had no idea that the cost for a DUI could add up to over $6,000 |
| Interventionist: You were surprised that it was so expensive. How much did you assume it would cost? |
| Participant: I guess I never really put a lot of thought into it, but I never realized how many things and expenses play into getting a DUI. |
| Interventionist: It really adds up! (2) How would receiving a DUI impact your future career goals? |
| Participant: Well, I plan to go to dental school after undergrad, so it would completely ruin that for me. |
| Interventionist: Receiving a DUI might make it much more difficult to get into dental school. (3) What is your plan for driving after drinking in the future? |
| Participant: I really try my best to avoid that and I have only done that a very few number of times, so I’m just going to cut that out completely. I try to call an Uber after I’ve been drinking at all so I will make sure to do that every time. |
| Interventionist: It sounds like it’s really important to you to stay safe! In order to make sure you’re safe, you’ll call an Uber if you’ve had too much to drive safely. |
Information condition.
Students randomized to the information condition received standard information about alcohol and DAD via a link to a mobile-optimized website delivered through text message immediately on receipt of the text message from the participant confirming completion of all baseline measures. The informational document provided detailed information about how alcohol and other drugs affect the brain and nervous system, memory, and driving performance and is similar to alcohol education programs commonly found on college campuses. The alcohol-related information was not personalized and the control intervention did not include goal setting or interactive text messaging. Participants were instructed to view the informational document on their mobile phones and to respond to a number of questions embedded in the informational document as a comprehension and fidelity check. Students were provided the opportunity to ask any questions related to the information provided via text message. (See Table 2 for a description of the components in the two conditions.)
Table 2.
Description of components included in each condition
| Components of each condition | |
| Drinking and driving brief alcohol intervention condition | Alcohol information condition |
| Personalized feedback: | Educational information about the risks associated with alcohol use: |
| • Review of the student’s weekly drinking pattern | • How alcohol enters the bloodstream |
| • Social norms information | • Effects of alcohol on the brain |
| • Estimated BAC before driving and risks associated with BAC | • Factors that affect BAC |
| • Fees for a DUI citation | • Risks associated with driving after drinking alcohol |
| • Strategies for avoiding driving after drinking | • Strategies for avoiding driving after drinking |
| • Campus and community-based alcohol-related resources | • Campus and community alcohol-related resources |
Notes: BAC = blood alcohol concentration; DUI = driving under the influence.
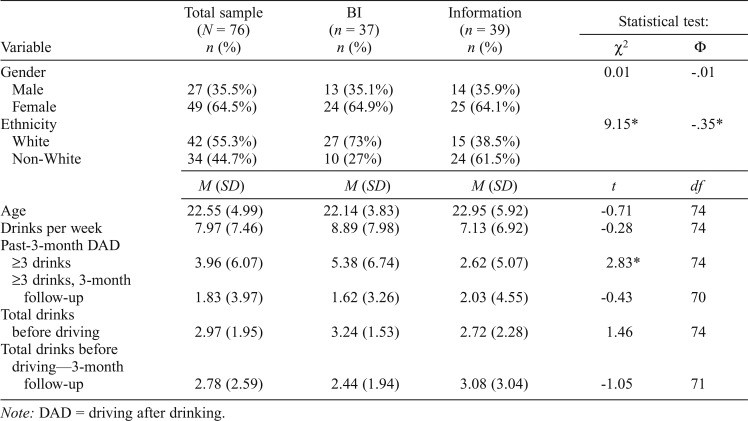
Data analysis plan.
Analyses were conducted using SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY) and R version 2.12.0. Baseline descriptive characteristics of the overall sample were conducted, including demographic information (gender, age, ethnicity) as well as the means and standard deviations for the primary outcome variables (alcohol-impaired driving, number of drinks consumed before driving). In addition, t tests and chi square analyses were performed to determine whether the intervention group and the control group were significantly different at baseline on any demographic or alcohol-related variables (Table 3).
Table 3.
Descriptive statistics for outcome variables and covariates: Baseline and 3-month follow-up
| Statistical test: |
|||||
| Variable | Total sample (N = 76) n (%) | BI (n = 37) n (%) | Information (n = 39) n (%) | χ2 | Φ |
| Gender | 0.01 | -.01 | |||
| Male | 27 (35.5%) | 13 (35.1%) | 14 (35.9%) | ||
| Female | 49 (64.5%) | 24 (64.9%) | 25 (64.1%) | ||
| Ethnicity | 9.15* | -.35* | |||
| White | 42 (55.3%) | 27 (73%) | 15 (38.5%) | ||
| Non-White | 34 (44.7%) | 10 (27%) | 24 (61.5%) | ||
| M (SD) | M (SD) | M (SD) | t | df | |
| Age | 22.55 (4.99) | 22.14 (3.83) | 22.95 (5.92) | -0.71 | 74 |
| Drinks per week | 7.97 (7.46) | 8.89 (7.98) | 7.13 (6.92) | -0.28 | 74 |
| Past-3-month DAD ≥3 drinks | 3.96 (6.07) | 5.38 (6.74) | 2.62 (5.07) | 2.83* | 74 |
| ≥3 drinks, 3-month follow-up | 1.83 (3.97) | 1.62 (3.26) | 2.03 (4.55) | -0.43 | 70 |
| Total drinks before driving | 2.97 (1.95) | 3.24 (1.53) | 2.72 (2.28) | 1.46 | 74 |
| Total drinks before driving—3-month follow-up | 2.78 (2.59) | 2.44 (1.94) | 3.08 (3.04) | -1.05 | 71 |
Note: DAD = driving after drinking.
The primary study analyses examined whether there was a statistically significant difference between treatment groups on changes in self-reported DAD. Repeated-measures mixed modeling analyses were conducted to examine Hypothesis 1 (students receiving the DAD intervention will report greater reductions in driving after drinking at 3-month follow-up compared with control participants) and Hypothesis 2 (students receiving the DAD intervention will report significantly greater reductions in drinks consumed before driving at 3-month follow-up compared with control participants).
Generalized linear mixed models (GLMM) represent an extension of linear mixed models to nonnormal data. GLMM with a negative binomial distribution, which allows for overdispersion in count outcomes, were used for outcomes of nonnormally distributed count data (i.e., total number of times DAD). Driving after drinking three or more drinks was found to be overdispersed (i.e., variance exceeds mean). In addition, this variable contained greater than 15% zeros. A negative binomial hurdle (NBH) model in which all participants can be considered “at-risk” for an outcome was chosen for these analyses because all individuals included in the present study reported DAD at least twice in the past 3 months. The NBH regression involves first identifying sampling zeroes (the “hurdle” part of the model) followed by examining those who cross the hurdle (values > 0; “binomial” part of the model). Thus, our analyses separately predicted sampling zeroes (i.e., not endorsing the outcome variable) and counts > 0 (i.e., outcome variable > 0). For each model tested, one of the primary outcome variables served as the dependent variable. Repeated-measures mixed models analyses were conducted for number of drinks consumed before driving (normally distributed). Cohen’s D effect sizes (for the mean differences between baseline and follow-up) were computed and interpreted using the conventional metrics of d = 0.2, 0.5, and 0.8 indicating small, medium, and large effects (Cohen, 1992).
Results
Baseline characteristics
Overall, participants reported driving an average of 3.96 times (SD = 6.07) after consuming three or more drinks in the past 3 months. All participants (100%) reported driving after drinking two or more drinks and 72.4% reported driving after consuming three or more drinks in the past 3 months. Participants reported drinking an average of 12.0 standard drinks (SD = 16.96) in a typical week and engaging in an average of 3.66 binge episodes (SD = 3.73) in the past month. The intervention group reported driving after drinking three or more drinks significantly more times than the control group (Table 3). Approximately 84% of participants in the intervention group and 54% of participants in the control group reported at least two instances of driving after drinking three or more drinks and at baseline. There was also a significant baseline difference in ethnicity. There were no other significant baseline differences. Seventy-six participants completed the 3-month follow-up (91.7% overall follow-up rate).
Analysis of study outcomes
Results for the mixed-models analyses are presented in Tables 4 and 5. Gender, age, and ethnicity were included as covariates in all initial models. However, results revealed that these variables were not statistically significant and did not change the pattern of results. As a result, they were removed from the final models.
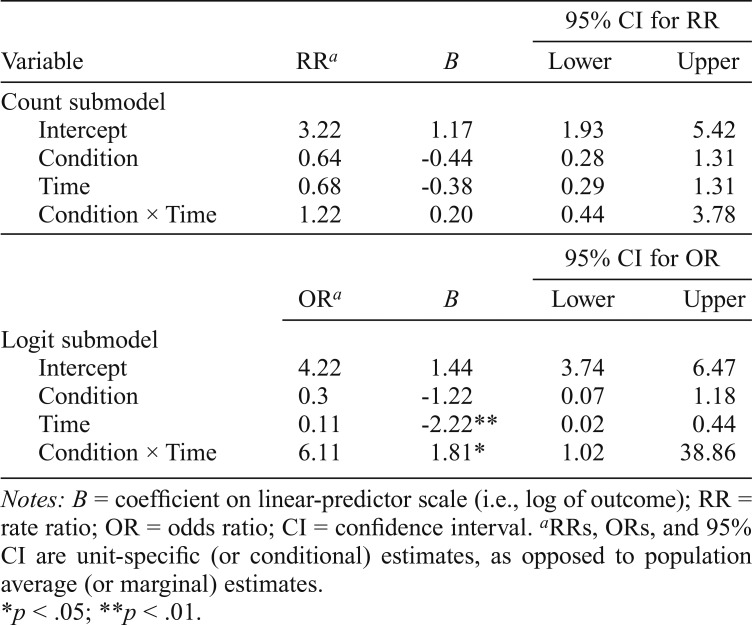
Table 4.
Negative binomial hurdle mixed model results for driving after three or more drinks
| 95% CI for RR |
||||
| Variable | RRa | B | Lower | Upper |
| Count submodel | ||||
| Intercept | 3.22 | 1.17 | 1.93 | 5.42 |
| Condition | 0.64 | -0.44 | 0.28 | 1.31 |
| Time | 0.68 | -0.38 | 0.29 | 1.31 |
| Condition × Time | 1.22 | 0.20 | 0.44 | 3.78 |
| % CI for OR |
||||
| ORa | B | Lower | Upper | |
| Logit submodel | ||||
| Intercept | 4.22 | 1.44 | 3.74 | 6.47 |
| Condition | 0.3 | -1.22 | 0.07 | 1.18 |
| Time | 0.11 | -2.22** | 0.02 | 0.44 |
| Condition × Time | 6.11 | 1.81* | 1.02 | 38.86 |
Notes: B = coefficient on linear-predictor scale (i.e., log of outcome); RR = rate ratio; OR = odds ratio; CI = confidence interval.
RRs, ORs, and 95% CI are unit-specific (or conditional) estimates, as opposed to population average (or marginal) estimates.
p < .05;
p < .01.
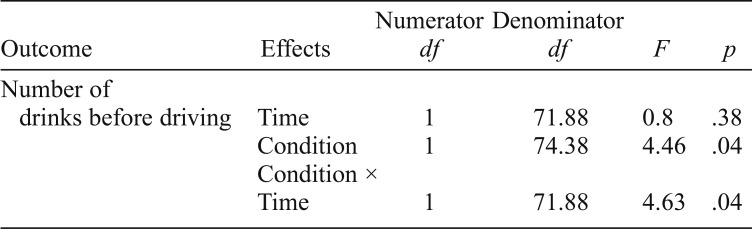
Table 5.
Repeated measures mixed model results for eBAC and drinks before driving
| Numerator Denominator |
|||||
| Outcome | Effects | df | df | F | p |
| Number of drinks before driving | Time | 1 | 71.88 | 0.8 | .38 |
| Condition | 1 | 74.38 | 4.46 | .04 | |
| Condition × Time | 1 | 71.88 | 4.63 | .04 | |
Driving after drinking.
GLMM with a negative binomial distribution were used to determine if driving after consuming “three or more drinks” differed over time for participants who received the DAD intervention versus those who received the information intervention.2 There were significant reductions in DAD over time and a significant interaction between condition and time for driving after drinking three or more drinks. The DAD intervention was associated with larger reductions in the likelihood of driving after drinking three or more drinks than the information intervention at the 3-month follow-up (ds = 0.70 and 0.12, respectively).
Total drinks consumed before driving.
There was a significant interaction between condition and time, F(1, 71.88) = 4.63, p = .04. Consistent with this Treatment Condition × Time interaction, the DAD intervention was associated with larger effect size reduction in number of drinks consumed before driving than the education intervention at the 3-month follow-up (ds = 0.46 and 0.13, respectively).
Discussion
Alcohol-impaired driving is a significant public health concern, and college students are more likely than any other age group to report driving under the influence of alcohol (Hingson et al., 2017). The purpose of the present study was to develop and evaluate a brief, mobile phone–based personalized feedback and interactive text messaging intervention for college students who reported recent DAD. The overall pattern of results provides initial support for the efficacy of this intervention. Specific findings are discussed below in conjunction with study limitations.
Number of times driving after drinking
Consistent with previous research examining the impact of in-person BAIs on DAD in emergency room settings (D’Onofrio et al., 2008; Schermer et al., 2006), with DUI offenders (Wells-Parker et al., 1995), and among adolescent and college-aged drinkers (Monti et al., 1999; Schaus, 2009; Teeters et al., 2015), the DAD intervention delivered in the present study successfully reduced DAD behaviors over time compared with a generic alcohol information intervention. Specifically, students in the mobile phone–based DAD intervention condition reported reduced likelihood of driving after drinking two or more drinks at follow-up. However, there were no significant differences between intervention and control on counts of driving after drinking three or more drinks among students who reported driving after drinking three or more drinks at baseline.
Total drinks consumed before driving
Participants who received the mobile phone–based DAD intervention significantly reduced the total number of drinks they consumed before driving compared with those receiving the information intervention at 3-month follow-up. Students receiving the DAD BAI decreased their consumption before driving on their last DAD occasion by approximately one standard drink, whereas students in the information condition increased their reported number of drinks before driving. Although there are a number of factors that influence intoxication level before driving, the reductions shown by the intervention group from three standard drinks to two standard drinks may reflect a clinically meaningful reduction in risk.
Implications
Overall, the results of the present study indicate that a brief, mobile phone–based intervention with personalized feedback and interactive text messaging shows some evidence of reducing likelihood of DAD and the number of drinks consumed before driving among a sample of college students with a previous pattern of DAD. This study extends previous research on interventions for DAD, which have traditionally included general samples of heavy drinkers, accident victims, and individuals arrested for DUI. In contrast, the present study screened and recruited participants based on DUI risk (reporting recent DAD). This allowed us to directly target DAD among those arguably most at risk for experiencing consequences related to DAD.
The present study also adds to the literature on mobile phone–based interventions. Only a few published studies in the alcohol literature have implemented text messaging as an intervention, and this is the first to use interactive texting with a study counselor. In a young adult emergency room sample, Suffoletto and colleagues (2014, 2015) found reductions in heavy episodic drinking episodes and drinks consumed per drinking episode in response to a text-messaging intervention at 3-month, 6-month, and 9-month follow-ups. In addition, Suffoletto and colleagues (2016) demonstrated reductions in binge drinking during a 6-week text-messaging intervention. The results of the present study complement and extend these findings by demonstrating some evidence that a mobile phone–based personalized feedback and interactive text-messaging based intervention can reduce driving after drinking three or more drinks and the number of drinks consumed before driving in a sample of college students.
In addition, web-based feedback interventions have been criticized because of potential concerns about variance in the actual amount of processing and comprehension of the information presented in the feedback document. Of note, web-based or feedback-only interventions have demonstrated smaller effect sizes than in-person interventions at follow-ups longer than 4 months (Cadigan et al., 2015). To negate concerns about the lack of interaction with a clinician and the minimal/uncertain comprehension and processing of intervention material that might occur with remote web-based interventions, interactive text messages were used in the present study to integrate theoretically active MI elements including reflections intended to convey empathy and tailored open-ended questions intended to develop discrepancy and facilitate goal setting. Because this intervention did not compare a DAD feedback only condition to the DAD + brief text conversation condition, it is not possible to determine the extent to which the interactive text messages used in this study were responsible for reductions in DAD behaviors. However, the effect sizes generated in this study are larger than effect sizes cited in other studies of electronically delivered BAIs, potentially suggesting that the interactive component used in this study may have resulted in larger effect sizes than non-interactive text-based studies (see Mason et al., 2015, for meta-analysis). However, because no research currently exists directly comparing interactive text-based interventions to non-interactive text-based interventions, the previous assertion is speculative and needs to be empirically tested in future studies.
Limitations
Several limitations should be considered when interpreting these findings. Because of the design of this pilot trial, it is not possible to parse out which parts of the intervention were most potent. Dismantling studies are necessary to elucidate which elements of the personalized feedback are most salient. In addition, it is not clear from this study whether interactive text messages are a crucial part of the intervention because this study did not compare a DAD feedback only condition to the DAD feedback + interactive texts condition. Future research is also needed to determine how this intervention compares to an in-person personalized feedback intervention targeting DAD and to standard in-person alcohol BAIs. All alcohol use data were collected via retrospective self-reports and may have been subject to biases. Significant baseline differences between the intervention and the control group were found for the number of times driving after drinking “three or more drinks.” Unfortunately, the baseline differences on the number of times driving after drinking outcome makes it difficult to rule out the possibility that regression to the mean influenced these specific study results. Last, future studies should use a longer follow-up period to determine if the observed effects persist beyond the 3-month follow-up.
Despite these limitations, this study has potential public health implications and makes a contribution to the DAD and technology-based intervention literatures. The findings of this study provide preliminary support for the short-term efficacy of a mobile phone–based intervention including personalized feedback and interactive text-messaging for reducing DAD among college students.
Footnotes
The delivery of the intervention elements occurred immediately after the study administrator received the confirmation text message from the participant between 8 a.m. and 9 p.m. There were a few instances when the study administrator received the text messages after 9 p.m. and waited until the following morning to respond.
We also conducted supplemental repeated-measures mixed modeling analyses to examine change in driving after drinking from baseline to the 3-month follow-up allowing us to examine short-term intervention outcomes for all of the participants who were randomized to an intervention (an intent-to-treat analysis). These outcomes were functionally identical to the repeated-measures analyses described above in terms of statistical significance and effect size.
This research was supported by a grant from the American Psychological Association (principal investigator: Jenni B. Teeters) and National Institute on Alcohol Abuse and Alcoholism (R01AA020829, principal investigator: James G. Murphy).
References
- Brown T. G., Dongier M., Ouimet M. C., Tremblay J., Chanut F., Legault L., Ng Ying Kin N. M. Brief motivational interviewing for DWI recidivists who abuse alcohol and are not participating in DWI intervention: A randomized controlled trial. Alcoholism: Clinical and Experimental Research. 2010;34:292–301. doi: 10.1111/j.1530-0277.2009.01092.x. doi:10.1111/j.1530-0277.2009.01092.x. [DOI] [PubMed] [Google Scholar]
- Buscemi J., Murphy J. G., Martens M. P., McDevitt-Murphy M. E., Dennhardt A. A., Skidmore J. R. Help-seeking for alcohol use in college students: Correlates and preferred resources. Psychology of Addictive Behaviors. 2010;24:571–580. doi: 10.1037/a0021122. doi:10.1037/a0021122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadigan J. M., Haeny A. M., Martens M. P., Weaver C. C., Takamatsu S. K., Arterberry B. J. Personalized drinking feedback: A metaanalysis of in-person versus computer-delivered interventions. Journal of Consulting and Clinical Psychology. 2015;83:430–437. doi: 10.1037/a0038394. doi:10.1037/a0038394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey K. B., Scott-Sheldon L. A., Carey M. P., DeMartini K. S. Individual-level interventions to reduce college student drinking: a metaanalytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. doi:10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cocosila M., Archer N., Haynes R. B., Yuan Y. Can wireless text messaging improve adherence to preventive activities? Results of a randomised controlled trial. International Journal of Medical Informatics. 2009;78:230–238. doi: 10.1016/j.ijmedinf.2008.07.011. doi:10.1016/j.ijmedinf.2008.07.011. [DOI] [PubMed] [Google Scholar]
- Collins R. L., Parks G. A., Marlatt G. A. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. doi:10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. doi:10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cronce J. M., Bittinger J. N., Liu J., Kilmer J. R. Electronic feedback in college student drinking prevention and intervention. Alcohol Research: Current Reviews. 2014;36:47–62. [PMC free article] [PubMed] [Google Scholar]
- Cronce J. M., Larimer M. E., White H. R., Rabiner D. L. College student drinking and drug use: Multiple perspectives on a complex problem (pp. 161–183) Guilford Press; 2012. Brief individual-focused alcohol interventions for college students. [Google Scholar]
- D’Onofrio G., Fiellin D. A., Pantalon M. V., Chawarski M. C., Owens P. H., Degutis L. C., O’Connor P. G. A brief intervention reduces hazardous and harmful drinking in emergency department patients. Annals of Emergency Medicine. 2012;60:181–192. doi: 10.1016/j.annemergmed.2012.02.006. doi:10.1016/j.annemergmed.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjeldsoe B. S., Marshall A. L., Miller Y. D. Behavior change interventions delivered by mobile telephone short-message service. American Journal of Preventive Medicine. 2009;36:165–173. doi: 10.1016/j.amepre.2008.09.040. doi:10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- Fowler L. A., Holt S. L., Joshi D. Mobile technology-based interventions for adult users of alcohol: A systematic review of the literature. Addictive Behaviors. 2016;62:25–34. doi: 10.1016/j.addbeh.2016.06.008. doi:10.1016/j.addbeh.2016.06.008. [DOI] [PubMed] [Google Scholar]
- Foxcroft D. R., Coombes L., Wood S., Allen D., Almeida Santimano N. M., Moreira M. T. Motivational interviewing for the prevention of alcohol misuse in young adults. Cochrane Database of Systematic Reviews, Issue. 2016 doi: 10.1002/14651858.CD007025.pub4. 7, Article No.CD007025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C., Whittaker R., Knight R., Abramsky T., Rodgers A., Roberts I. G. Txt2stop: A pilot randomised controlled trial of mobile phone-based smoking cessation support. Tobacco Control. 2009;18:88–91. doi: 10.1136/tc.2008.026146. doi:10.1136/tc.2008.026146. [DOI] [PubMed] [Google Scholar]
- Gerber B. S., Stolley M. R., Thompson A. L., Sharp L. K., Fitzgibbon M. L. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: A feasibility study. Health Informatics Journal. 2009;15:17–25. doi: 10.1177/1460458208099865. doi:10.1177/1460458208099865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R., Zha W., Smyth D. Magnitude and trends in heavy episodic drinking, alcohol-impaired driving, and alcohol-related mortality and overdose hospitalizations among emerging adults of college ages 18–24 in the United States, 1998–2014. Journal of Studies on Alcohol and Drugs. 2017;78:540–548. doi: 10.15288/jsad.2017.78.540. doi:10.15288/jsad.2017.78.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hox J. Multilevel analysis: Techniques and applications. NewYork, NY: Routledge; 2010. [Google Scholar]
- Huh D., Mun E. Y., Larimer M. E., White H. R., Ray A. E., Rhew I. C., Atkins D. C. Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcoholism: Clinical and Experimental Research. 2015;39:919–931. doi: 10.1111/acer.12714. doi:10.1111/acer.12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurling R., Catt M., De Boni M., Fairley B. W., Hurst T., Murray P., Sodhi J. S. Using internet and mobile phone technology to deliver an automated physical activity program: Randomized controlled trial. Journal of Medical Internet Research. 2007;9(2):e7. doi: 10.2196/jmir.9.2.e7. doi:10.2196/jmir.9.2.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvine L., Falconer D. W., Jones C., Ricketts I. W., Williams B., Crombie I. K. Can text messages reach the parts other process measures cannot reach: An evaluation of a behavior change intervention delivered by mobile phone? PLoS One. 2012;7(12):e52621. doi: 10.1371/journal.pone.0052621. doi:10.1371/journsl.pone.0052621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H. S. A randomized controlled trial of a nurse short-message service by cellular phone for people with diabetes. International Journal of Nursing Studies. 2007;44:687–692. doi: 10.1016/j.ijnurstu.2006.01.011. doi:10.1016/j.ijnurstu.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Kivlahan D. R., Marlatt G. A., Fromme K., Coppel D. B., Williams E. Secondary prevention with college drinkers: Evaluation of an alcohol skills training program. Journal of Consulting and Clinical Psychology. 1990;58:805–810. doi: 10.1037//0022-006x.58.6.805. doi:10.1037/0022-006X.58.6.805. [DOI] [PubMed] [Google Scholar]
- LaBrie J. W., Kenney S. R., Mirza T., Lac A. Identifying factors that increase the likelihood of driving after drinking among college students. Accident Analysis and Prevention. 2011;43:1371–1377. doi: 10.1016/j.aap.2011.02.011. doi:10.1016/j.aap.2011.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie J. W., Napper L. E., Ghaidarov T. M. Predicting driving after drinking over time among college students: The emerging role of injunctive normative perceptions. Journal of Studies on Alcohol and Drugs. 2012;73:726–730. doi: 10.15288/jsad.2012.73.726. doi:10.15288/jsad.2012.73.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason M., Ola B., Zaharakis N., Zhang J. Text messaging interventions for adolescent and young adult substance use: A meta-analysis. Prevention Science. 2015;16:181–188. doi: 10.1007/s11121-014-0498-7. doi:10.1007/s11121-014-0498-7. [DOI] [PubMed] [Google Scholar]
- Miller W. R., Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford Press; 2012. [Google Scholar]
- Monti P. M., Colby S. M., Barnett N. P., Spirito A., Rohsenow D. J., Myers M., Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. doi:10.1037/0022-006X.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moore S. C., Crompton K., van Goozen S., van den Bree M., Bunney J., Lydall E. A feasibility study of short message service text messaging as a surveillance tool for alcohol consumption and vehicle for interventions in university students. BMC Public Health. 2013;13:1011. doi: 10.1186/1471-2458-13-1011. doi:10.1186/1471-2458-13-1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mun E.-Y., de la Torre J., Atkins D. C., White H. R., Ray A. E., Kim S.-Y., Huh D. the Project INTEGRATE Team. Project INTEGRATE: An integrative study of brief alcohol interventions for college students. Psychology of Addictive Behaviors. 2015;29:34–48. doi: 10.1037/adb0000047. doi:10.1037/adb0000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration. Screening and brief intervention toolkit for college and university campuses. 2014 Retrieved from http://www.nhtsa.gov/links/sid/3672Toolkit/pages/SupportingRes.html.
- Ouimet M. C., Dongier M., Di Leo I., Legault L., Tremblay J., Chanut F., Brown T. G. A randomized controlled trial of brief motivational interviewing in impaired driving recidivists: A 5-year follow-up of traffic offenses and crashes. Alcoholism: Clinical and Experimental Research. 2013;37:1979–1985. doi: 10.1111/acer.12180. doi:10.1111/acer.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. Mobile fact sheet. 2014 Retrieved from http://www.pewinternet.org/fact-sheets/mobile-technology-fact-sheet/
- Schaus J. F., Sole M. L., McCoy T. P., Mullett N., O’Brien M. C. Alcohol screening and brief intervention in a college student health center: A randomized controlled trial. Journal of Studies on Alcohol and Drugs, Supplement. 2009;16:131–142. doi: 10.15288/jsads.2009.s16.131. doi:10.15288/jsads.2009.s16.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schermer C. R., Moyers T. B., Miller W. R., Bloomfield L. A. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. Journal of Trauma: Injury, Infection, and Critical Care. 2006;60:29–34. doi: 10.1097/01.ta.0000199420.12322.5d. doi:10.1097/01.ta.0000199420.12322.5d. [DOI] [PubMed] [Google Scholar]
- Spirito A., Monti P. M., Barnett N. P., Colby S. M., Sindelar H., Rohsenow D. J., Myers M. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. Journal of Pediatrics. 2004;145:396–402. doi: 10.1016/j.jpeds.2004.04.057. doi:10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- Suffoletto B., Kristan J., Callaway C., Kim K. H., Chung T., Monti P. M., Clark D. B. A text message alcohol intervention for young adult emergency department patients: A randomized clinical trial. Annals of Emergency Medicine. 2014;64:664–72. doi: 10.1016/j.annemergmed.2014.06.010. e4. doi:10.1016/j.annemergmed.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffoletto B., Kristan J., Chung T., Jeong K., Fabio A., Monti P., Clark D. B. An interactive text message intervention to reduce binge drinking in young adults: A randomized controlled trial with 9-month outcomes. PLoS One. 2015;10(11):e0142877. doi: 10.1371/journal.pone.0142877. doi:10.1371/journal.pone.0142877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffoletto B., Merrill J. E., Chung T., Kristan J., Vanek M., Clark D. B. A text message program as a booster to in-person brief interventions for mandated college students to prevent weekend binge drinking. Journal of American College Health. 2016;64:481–489. doi: 10.1080/07448481.2016.1185107. doi:10.1080/07448481.2016.1185107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters J. B., Borsari B., Martens M. P., Murphy J. G. Brief motivational interventions are associated with reductions in alcohol-impaired driving among college drinkers. Journal of Studies on Alcohol and Drugs. 2015;76:700–709. doi: 10.15288/jsad.2015.76.700. doi:10.15288/jsad.2015.76.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells-Parker E., Bangert-Drowns R., McMillen R., Williams M. Final results from a meta-analysis of remedial interventions with drink/drive offenders. Addiction. 1995;90:907–926. doi: 10.1046/j.1360-0443.1995.9079074.x. doi:10.1111/j.1360-0443.1995.tb03500.x. [DOI] [PubMed] [Google Scholar]
- Wells-Parker E., Williams M. Enhancing the effectiveness of traditional interventions with drinking drivers by adding brief individual intervention components. Journal of Studies on Alcohol. 2002;63:655–664. doi: 10.15288/jsa.2002.63.655. doi:10.15288/jsa.2002.63.655. [DOI] [PubMed] [Google Scholar]
- White H. R. Reduction of alcohol-related harm on United States college campuses: The use of personal feedback interventions. International Journal on Drug Policy. 2006;17:310–319. doi:10.1016/j.drugpo.2006.02.006. [Google Scholar]