Abstract
Antenatal and post‐natal depression has demonstrated a significant burden in sub‐Saharan Africa, with rates ranging from 10% to 35%. However, perinatal women living with HIV in Tanzania have reported an even greater prevalence of depression (43–45%). The primary goal of this study was to examine the relationship between maternal depression and infant malnutrition among women living with HIV. The design was a retrospective cohort study within the context of a randomised controlled trial among women living with HIV and their infants. Within this trial, 699 mother–child pairs were analysed for the present study. Although antenatal depression was not associated with infant malnutrition and post‐natal depression was negatively associated [relative risk (RR = 0.80, P = 0.04], cumulative depression demonstrated a positive association with infant wasting (RR = 1.08, P < 0.01) and underweight (RR = 1.03, P < 0.01) after controlling for confounding factors. Variation in the association between depression and infant nutritional status was observed for episodic vs. chronic depression. These findings suggest that providing evidence‐based services for persistent depression among women living with HIV may have an effect on infant malnutrition. In addition, other positive outcomes may be related to infant cognitive development as well as HIV disease prognosis and survival among women.
Keywords: HIV‐positive, post‐natal, antenatal, prenatal, maternal depression, sub‐Saharan Africa, infant malnutrition
Introduction
Depression among perinatal women living with HIV has significant implications for health outcomes in women as well as their infants. Economic insecurity and stigma related to the illness may increase the risk of depression as well as child malnutrition in this vulnerable population. While studies on depression among pregnant women in sub‐Saharan Africa have been limited, the prevalence of post‐natal depression has been found to be high, with estimates ranging from 10% in Uganda (Cox 1979) to 34.7% in South Africa (Tomlinson et al. 2006). In Tanzania, elevated rates of depression have been reported among women living with HIV (Kaaya et al. 2002). Antelman et al. (2007) reported depression rates of 43% antenatally and 45% post‐natally among a cohort of women living with HIV, suggesting a significant burden that can have an effect on the health status of the mother as well as her infant.
Maternal depression has been associated with infant malnutrition in a number of studies (Surkan et al. 2007, 2011). Possible mechanisms or mediators of the association have been postulated, including impaired mother–child interactions (Ammaniti et al. 2004; Perez et al. 2005; Stewart 2007), decreased health‐seeking behaviours and breastfeeding, increased incidence of low birthweight among depressed mothers, as well as a number of socio‐cultural and economic factors (Stewart 2007; Wachs et al. 2009; Surkan et al. 2011). Some researchers have further hypothesised that the association between maternal depression and infant malnutrition may be exacerbated in situations of financial insecurity or limited social resources (Patel et al. 2004; Surkan et al. 2007).
However, there have been inconsistent findings on the relationship between maternal depression and infant nutritional status. For example, cross‐sectional and cohort studies in South Asia and Brazil have demonstrated strong associations between maternal depression and low birthweight, infant underweight and stunting, even after controlling for a number of socio‐economic factors (De Miranda et al. 1996; Patel et al. 2003, 2004; Anoop et al. 2004; Rahman et al. 2006, 2007; Nasreen et al. 2010; Surkan et al. 2011). In contrast, findings from Peru (Harpham et al. 2005), Jamaica (Baker‐Henningham et al. 2005), Ethiopia (Harpham et al. 2005) and South Africa (Tomlinson et al. 2006) have found no association between maternal depression and infant underweight or stunting after controlling for possible confounders, such as infant birthweight, socio‐economic status, maternal age and education and family size. In a recent meta‐analysis by Surkan et al. (2011), maternal depression was associated with stunting and underweight among children under 5 years of age. Although this aggregate analysis indicates a relationship, variability in this association may be related to context‐specific factors to some extent.
This study seeks to examine whether a relationship exists between maternal antenatal, post‐natal and cumulative depression and infant malnutrition (wasting, stunting and low weight‐for‐age) in the urban setting of Dar es Salaam, Tanzania, among a large cohort of women living with HIV. A better understanding of this relationship may help to inform interventions targeting depression among women living with HIV and infant malnutrition in Tanzania and similar resource‐limited settings.
Key messages.
This research demonstrates that cumulative depression is positively associated with infant malnutrition among women living with HIV/AIDS.
Evidence‐based mental health services for women living with HIV/AIDS could potentially reduce the burden of depression among women and promote the nutritional status of their infants.
Other positive outcomes related to reducing depression would include promoting infant cognitive development and women's HIV‐related prognosis and survival.
Additional structural issues contributing to depression, such as HIV‐related stigma and economic insecurity, should also be considered given that related interventions may reduce the overall burden of depression in this vulnerable population.
Materials and methods
Study design and population
Data analysed for this retrospective cohort study were obtained from a randomised controlled trial conducted in Dar es Salaam, Tanzania. The principal aims of the primary study were to investigate the effects of vitamin supplementation on perinatal HIV transmission, pregnancy outcomes, progression of HIV and mortality (Fawzi et al. 2002). Inclusion criteria were HIV‐positive pregnant women less than 27 weeks of gestation at enrolment and permanent residence in Dar es Salaam, Tanzania. One thousand seventy‐eight pregnant women living with HIV were enrolled between April 1995 and July 1997 from urban antenatal clinics. Study nurses collected data on age, education, socio‐economic and marital status, obstetric history and anthropometry from women at enrolment. Study physicians conducted complete physical examinations; blood samples were collected for assessment of anaemia. Participants were followed up monthly until 2000 and then every 3 months until the study completion in June 2003. Details on the primary study design and methods have been published elsewhere (Fawzi et al. 1999). Given that the data were collected longitudinally, all of the women's assessments occurred before the infants' measurements.
Assessment of maternal depression
A subset of participants (n = 1020) was assessed for depressive and anxiety symptoms using the Hopkins Symptom Checklist (HSCL‐25). The baseline HSCL‐25 measure was administered approximately 2 months after enrolment and women were subsequently re‐screened every 6 months until 2001, and every 12 months thereafter, until the conclusion of the study in June 2003 (Fawzi et al. 2003). Kaaya et al. (2002) conducted a validation study of the HSCL‐25 among this population and determined that a modified subscale of eight items and a depression cut‐off score of >1.06 could be used to identify symptom levels comparable with major depressive disorder with high sensitivity (88%) and specificity (89%) when compared to assessment by a psychiatrist using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, to identify major depressive disorder.
Assessment of infant underweight, stunting and wasting
The World Health Organization defines underweight as weight‐for‐age less than −2 standard deviation (SD) of the WHO Child Growth Standards median (World Health Organization (WHO) Multicentre Growth Reference Study Group 2006). Stunting is defined as height‐for‐age less than −2 SD of the WHO Child Growth Standards median and reflects the cumulative effects of undernutrition and infections since and even before birth. Wasting is defined as weight‐for‐height less than −2 SD of the WHO Child Growth Standards median and is considered to be acute undernutrition from insufficient food or high rates of infectious diseases, especially diarrhoea. The percentage of children who are underweight (weight‐for‐age less than −2 SD) is a composite measure that includes children with low weight‐for‐height (wasting) and low height‐for‐age (stunting).
In order to measure these indicators, women were encouraged to deliver at the Muhimbili National Hospital, one of the study sites. Details on the techniques used for newborn and infant biophysical measurements have been published elsewhere (Fawzi et al. 2002). Briefly, newborns were weighed to the nearest 0.1 kg at delivery and recumbent length was measured to the nearest 0.1 cm. At monthly follow‐up study clinic visits, infants were physically examined, with repeat measurements of recumbent length and weight conducted by study physicians and research nurses.
Data analysis
For the statistical analysis, maternal depression was defined as a score of >1.06 using eight items from the HSCL‐25 as outlined earlier. Pre‐delivery maternal depression was measured at one visit during the pregnancy. The median days between the visit and delivery was 72 days (interquartile range: 53–91 days). Post‐delivery maternal depression was a time‐varying variable and measured at visits after delivery. Cumulative depression was the total number of times the woman had a depression score above the HSCL subscale cut‐off described earlier at visits after delivery. Women underwent an average of six depression assessments throughout the course of the study.
Social support was measured at the visit before delivery. A 10‐item social support scale was used in this study (Broadhead et al. 1988); the lowest 10th percentile of mean score for 10 items was used as a cut‐off to define lack of social support. In this analysis, child malnutrition was time‐varying and defined as weight‐for‐age, height‐for‐age or weight‐for‐height z‐score less than −2 SD (World Health Organization 2009).
The association between maternal depression, lack of social support and child malnutrition was examined by generalised estimating equations with an exchangeable working covariance structure specified for repeated measures. Separate models were run for antenatal depression, post‐natal depression and cumulative depression on the three outcomes of stunting, underweight and wasting. In multivariate models, some covariates are time‐varying, including child's HIV status, breastfeeding status, maternal counselling attendance and other disease events, while other covariates are time‐fixed including maternal age, marital status, education, financial dependence, weight, height, anaemia and HIV stage at enrolment, as well as child's gender, birthweight and gestational age. To ensure the temporality between exposure and outcome, maternal depression measurements included in the analysis occurred prior to infant nutritional status assessment. The first infant visit after each measurement of maternal depression (pre‐delivery and post‐delivery until the infant was 24 months of age) was included in the analysis. Effect estimates [relative risk (RR)] and their corresponding 95% confidence intervals were calculated. A missing indicator was created when there was a missing value. Including this indicator allowed inclusion of that record in multivariate models (Miettinen 1985). All statistical analyses were carried out using the statistical software package SAS, Release 9.2.
The Research and Publications Committee of Muhimbili University of Health and Allied Sciences, the Ethical Committee of the National AIDS Control Program of the Tanzanian Ministry of Health and the Institutional Review Board at the Harvard School of Public Health approved the study protocol, which included written informed consent for all participants.
Results
Maternal and child characteristics
Among the 872 women who had depression assessments before delivery, 870 had an assessment within 24 months after delivery. Out of this group, 699 mother–child pairs were included in the analysis (see Fig. 1). When comparing the 699 subset and remainder of the initial sample (379 out of 1078), there were no differences in age, marital status, income and pre‐delivery depression. However, there was a difference for having less than completed primary education (10.8% vs. 6.8%, P = 0.04) and anaemia (14.3% vs. 10.3%, P = 0.05), with the 699 subset demonstrating a lower prevalence for each of these factors.
Figure 1.
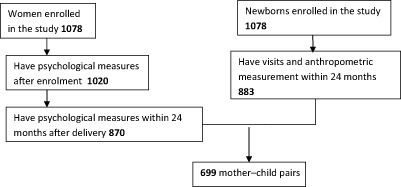
Flowchart for analysis sample.
All mothers were living with HIV at the time of enrolment. At baseline, 71.4% of pregnant women were between the ages of 20 and 29 years and nearly 12% were 15–19 years old. The majority (89.0%) was married or co‐habiting and most (82.1%) had a primary level education (equivalent to 7 years of study). Seventy‐four per cent of mothers reported being financially supported by another individual (no independent income). The remainder reported being either self‐employed or partially self‐employed. All women in the study reported a daily income of 1–2 USD per day. Ten per cent (10.3%) of the women were anaemic at baseline. Thirty‐eight per cent of women were found to be depressed prior to delivery at the enrolment interview. From the time of delivery to the end of the follow‐up period (maximum of 2 years), 36.3% of women were found to be depressed during one or more assessments.
Of the 699 children included in the study, 51.9% were male and almost one‐third (31.0%) were HIV‐positive. Only singleton births were included in the analysis. The HIV status was unknown for 19.6% of the children. Forty‐three per cent of the children were found to be underweight (with a weight‐for‐age z‐score less than −2 SD) at least once during the study period, while 48.5% were observed to be stunted (height‐for‐age z‐score less than −2 SD) and 23.3% were found to be wasted (weight‐for‐height z‐score less than −2 SD by 24 months) (see Table 1).
Table 1.
Characteristics of women living with HIV and their infants (n = 699)
| n (%) | |
|---|---|
| Characteristics of women | |
| Age category | |
| 15–19 | 80 (11.8) |
| 20–24 | 276 (39.5) |
| 25–29 | 223 (31.9) |
| ≥30 | 120 (17.2) |
| Marital status | |
| Single | 77 (11.0) |
| Married | 447 (64.0) |
| Co‐habiting | 175 (25.0) |
| Education level | |
| None or under primary | 48 (6.8) |
| Primary | 574 (82.1) |
| Secondary and above | 76 (10.9) |
| Missing | 1 (0.1) |
| Income resource | |
| Not totally supported | 178 (24.5) |
| Totally supported | 505 (74.4) |
| Missing | 1 (0.1) |
| Pre‐delivery depression | |
| No | 367 (52.5) |
| Yes | 267 (38.2) |
| Missing | 35 (9.3) |
| Any post‐delivery depression | |
| No | 445 (63.7) |
| Yes | 254 (36.3) |
| Anaemia | |
| No | 620 (89.7) |
| Yes | 71 (10.3) |
| Characteristics of infants | |
| Gender | |
| Male | 363 (51.9) |
| Female | 336 (48.1) |
| HIV status by 24 months | |
| Negative | 345 (49.4) |
| Positive | 217 (31.0) |
| Unknown | 137 (19.6) |
| Vitamin A* | |
| No | 340 (48.6) |
| Yes | 359 (51.4) |
| Multivitamin † | |
| No | 339 (48.5) |
| Yes | 360 (51.5) |
| Any weight‐to‐age z‐score less than −2 by 24 months | |
| No | 397 (56.8) |
| Yes | 302 (43.2) |
| Any height‐to‐age z‐score less than −2 by 24 months | |
| No | 360 (51.5) |
| Yes | 339 (48.5) |
| Any weight‐to‐height z‐score less than −2 by 24 months | |
| No | 536 (76.7) |
| Yes | 163 (23.3) |
*Indicates the percent of infants enrolled in the vitamin A intervention arm of the trial. †Reflects the percent of infants assigned to the multivitamins arm of the trial.
Univariate and multivariate analyses
Maternal pre‐delivery depression was not found to be significantly associated with infant underweight, stunting or wasting in univariate or multivariate analysis (Table 2). Maternal post‐delivery depression was found to be negatively associated with underweight (RR 0.81, P < 0.01) in the univariate analysis and this association remained significant after adjusting for confounding variables (RR 0.80, P = 0.04). Maternal post‐delivery depression was also found to be negatively associated with stunting (RR 0.78, P < 0.01) in the univariate analysis, but this effect was no longer significant after adjustment for possible confounders (RR 0.86, P = 0.10).
Table 2.
The association between maternal depression, social support and child malnutrition
| Weight‐to‐age z‐score ≤−2 (visits = 8337) | Height‐to‐age z‐score ≤−2 (visits = 7546) | Weight‐to‐height z‐score ≤−2 (visits = 7488) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate | Multivariate* | Univariate | Multivariate* | Univariate | Multivariate* | |||||||
| RR (95% CI) | P‐value | RR (95% CI) | P‐value | RR (95% CI) | P‐value | RR (95% CI) | P‐value | RR (95% CI) | P‐value | RR (95% CI) | P‐value | |
| Maternal pre‐ delivery depression (1.06) | 0.29 | 0.21 | 0.39 | 0.08 | 0.05 | 0.76 | ||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 0.95 (0.87, 1.04) | 0.86 (0.68, 1.09) | 1.04 (0.95, 1.14) | 0.83 (0.67, 1.02) | 1.20 (1.00, 1.44) | 1.06 (0.74, 1.51) | ||||||
| Maternal post‐ delivery depression (1.06) | <0.01 | 0.04 | <0.01 | 0.10 | 0.72 | 0.06 | ||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 0.81 (0.71, 0.93) | 0.80 (0.65, 0.99) | 0.78 (0.68, 0.89) | 0.86 (0.72, 1.03) | 1.05 (0.82, 1.34) | 0.59 (0.35, 1.01) | ||||||
| Cumulative depression | 1.03 (1.02, 1.05) | <0.01 | 1.03 (1.01, 1.04) | <0.01 | 1.03 (1.01, 1.04) | <0.01 | 1.02 (1.00, 1.04) | 0.09 | 1.11 (1.08, 1.14) | <0.01 | 1.08 (1.04, 1.12) | <0.01 |
| Perceived low social support | 0.88 | 0.54 | 0.30 | 0.53 | <0.01 | 0.75 | ||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 1.01 (0.87, 1.18) | 0.88 (0.60, 1.31) | 0.92 (0.79, 1.08) | 1.09 (0.84, 1.41) | 1.50 (1.15, 1.96) | 1.12 (0.57, 2.19) | ||||||
CI, confidence interval; RR, relative risk. *All multivariate models controlled for maternal perceived low social support, age, marital status, education, financial dependence, anaemia, weight, height, HIV stage at enrolment and counselling session attendance, child's gender, birthweight, gestational age, breastfeeding, HIV status, vitamin A, multivitamin and other disease events.
Cumulative depression post‐delivery was positively associated with underweight (RR 1.03, P < 0.01), stunting (RR 1.03, P < 0.01) and wasting (RR 1.11, P < 0.01), and this effect remained significant after adjusting for confounders for underweight (RR 1.03, P < 0.01) and wasting (RR 1.08, P < 0.01) only. Perceived social support was not significantly associated with underweight or stunting. Although low social support was positively associated with wasting (RR 1.50, P < 0.01) in the univariate analysis, this effect was no longer significant after adjusting for confounding variables (RR 1.12, P = 0.75).
Discussion
Although we found no significant association between pre‐delivery depression and malnutrition and a negative association for post‐delivery depression and underweight among infants of women living with HIV, at 2 years of follow‐up, cumulative depression post‐delivery was associated with wasting and underweight after controlling for confounding variables. However, cumulative depression was not associated with stunting among infants after controlling for confounding in this study.
A number of studies have demonstrated an association between post‐natal depression and infant nutritional and health outcomes (Rahman et al. 2006; Avan et al. 2010; Okronipa et al. 2012). In South Africa, women with depression at 6 months post‐partum were more likely to have children who were stunted by 2 years of age (Avan et al. 2010). Similar findings were observed in Pakistan, in which infants of depressed mothers were 4 and 2.6 times more likely to be underweight compared with infants of non‐depressed mothers, at 6 months and 12 months of age, respectively; in addition, stunting and diarrhoeal disease were more prevalent among infants with depressed mothers (Rahman et al. 2004). Among post‐natal women living with HIV in Ghana, infants of women who were depressed were more than five times more likely to have diarrhoeal disease compared with infants whose mothers did not have depression, which has implications for nutritional status as well (Okronipa et al. 2012).
However, some studies demonstrated mixed findings or no association between maternal depression and infant nutritional status. For example, Harpham et al. (2005) conducted a study in Vietnam, India, Ethiopia and Peru. They observed a relationship between high maternal depression and poor child nutritional status in India (stunting) and Vietnam (underweight), but could not find clear evidence for a similar association in Peru and Ethiopia (Harpham et al. 2005). Another study in Ethiopia found that infants of women with common mental disorders (which included depression) were not more likely to be underweight or stunted at 6 or 12 months of age compared with women not suffering from common mental disorders (Medhin et al. 2010).
One potential interpretation of these mixed findings is that it is possible that there are cultural differences in the quality and amount of social support that depressed mothers receive from their families and communities. Medhin et al. (2010) suggested that, in the context of Ethiopia, women often share parenting within families and communities, which may be related to their observing no association between common mental disorders and infant's nutritional status. Lack of support of the woman's partner may also be a factor. For example, among pregnant women in Cape Town, 39% had antenatal depression, which was associated with a lack of partner support and a higher degree of intimate partner violence (Hartley et al. 2011). Another factor that may result in disparate findings across studies is potential differences in chronicity of depression in different settings. Medhin et al. (2010) also indicated that there was a minimal burden of persisting symptoms of common mental disorders. Among Latina women in the United States with post‐partum depression, those experiencing chronic depression had infants with a lower mean weight‐for‐length z‐score at 12 months and 2 years of age compared with women who had no depression. Similar to the findings of the present study, women with episodic depression demonstrated no significant difference in infant mean z‐score at these time points compared with women who were not depressed (Wojcicki et al. 2011).
These findings correspond with this study's results as we observed no effect, or a negative effect, of isolated pre‐ and post‐natal depression, in contrast to a positive association of cumulative depression and infant wasting as well as underweight in this population of women living with HIV in Tanzania. The social support that women may receive in this context can include practical help from relatives and friends, which may offset the potential impact of maternal depression on infant nutritional status. This may be a factor that contributed to the null or negative associations observed for isolated antenatal and post‐natal depression. However, Lugina et al. (2001) indicated that this support may be changing in Tanzania, particularly in urban areas. It is possible that the potentially protective effect of social support for the mother in this context may be insufficient to offset the impact of chronic maternal depression on infant stunting.
A key issue related to this study is that it was conducted among women living with HIV, who may be more vulnerable to depression related to isolation and HIV‐related stigma (Surkan et al. 2010). This suggests that when planning HIV‐related services for pregnant women, such as PMTCT (prevention of mother‐to‐child transmission of HIV)‐plus, there should be consideration for strategies to enhance assessing and treating perinatal depression and preventing chronicity, for their own welfare and for their infants' growth outcomes. In addition, depression has demonstrated an association with HIV progression and mortality among perinatal women living with HIV (Antelman et al. 2007).
Despite this, a persisting problem within the context of HIV services is the limited integration of care for other chronic conditions, including depression (Dodds et al. 2004). Programmatic initiatives to integrate HIV and mental health care may reduce the chronicity of depression among women living with HIV, potentially improving infant nutritional status as well as the mental health and HIV‐related outcomes in this vulnerable population.
Limitations
This study has a number of methodological limitations. The data were derived from a randomised controlled trial without consideration for confounding factors related to the research questions of this study, thereby limiting the inclusion of a number of confounders in our analytical models. Factors such as rate of infant immunisation (Rahman et al. 2006) and parenting behaviours (Surkan et al. 2007) have been identified as possible confounders/mediators of the association between maternal depression and infant malnutrition; however, these variables were not included in this study. This may have been a factor in the paradoxical association observed between episodic post‐delivery depression and infant underweight, even after controlling for confounding variables. However, our list includes many of the factors/confounders previously identified in the literature, including marital status, maternal educational level, maternal anaemia, multivitamin use, financial dependence, HIV status, infant's gender, birthweight, gestational age, breastfeeding status and certain disease events (Rahman et al. 2006; Surkan et al. 2007). In addition, this study also had a relatively high number of children with unknown HIV status (19.6%), which can result in residual confounding by this factor. The subset of women included in the analysis (n = 699) had a lower level of anaemia and a slightly higher level of education than the women who were not included (n = 379); this may have resulted in a bias that would underestimate the effect of maternal depression on infant stunting. Also, cumulative depression may have been underestimated for women who had missed assessments. If this group with missing data also had a higher number of cumulative months of depression than indicated, then this finding would also result in a bias towards the null. Finally, the generalisability of our results may be limited by the fact that our participants comprised a group of urban women living with HIV who agreed to participate in a randomised controlled trial and received HIV counselling and testing. Although this study was performed before wide availability of antiretroviral therapy in Tanzania, they may have received closer antenatal and post‐natal follow‐up, which may have reduced the association between maternal depression and infant nutritional status as compared to other populations.
Strengths
Our study has a number of strengths. A large number of women living with HIV were included in our cohort and the follow‐up period was longer than in many previous studies in resource‐limited settings. In prior studies, there has been concern over the timing of assessments (Stewart 2007). However, our study was longitudinal and allowed for the observation of depression prior to assessing infants' nutritional status. Additionally, we used a depression tool that has been validated in our study population. Furthermore, although some studies have examined maternal depression at discrete time points, we chose to identify maternal depression at a number of assessments during the antenatal and post‐natal time periods, allowing us to evaluate cumulative depression over time.
Conclusion
Although there have been inconsistencies in the relationship between maternal depression and infant nutritional status in developing countries, the findings from the present study suggest that cumulative or chronic depression among women living with HIV can have an effect on the burden of wasting and underweight in their infants. Interestingly, the findings from isolated depression during antenatal and post‐natal periods were not consistent with this finding. This may be related to the complex nature of maternal depression and the potential relationship with infant nutritional status, which may vary according to the chronic nature of the woman's depression and the degree of support she may receive from her family and broader community.
Considering the present findings in the context of other studies, it appears that providing evidence‐based services for depression among pregnant and post‐natal women living with HIV over the duration of this critical period may demonstrate benefits for their infant's nutritional status. The significant investment in HIV services worldwide provides an opportunity in many resource‐limited settings to integrate mental health care in settings where PMTCT‐plus services are available. For pregnant and post‐natal women living with HIV, potentially reducing the burden of depression may be context‐specific, and providers may need to consider issues of chronicity as well as social support from the family and community to determine whether longer‐term care over the post‐natal period is necessary. Broader structural issues that may contribute to depression should be considered as well, such as addressing HIV‐related stigma and poor economic and food security, to explore the potential for intervention at that level as well.
In light of the remaining overall inconsistent evidence on the effect of maternal depression on infant nutritional status, even if improvement in infants' nutritional status may be modest, reducing the burden of depression among women may result in promoting other dimensions of the infants' well‐being, such as cognitive development. Equally important would be the potential for improving HIV‐related prognosis and survival among the women themselves.
Source of funding
Supported by the National Institute of Child Health and Human Development (NICHD RO1 32257), the National Institute of Mental Health (NIMH RO3 MH55451), and the Fogarty International Center (NIH D43 TW00004 and D43 TW01265).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
SK & MCSF contributed to the design and implementation of the study; as well as analysis and writing of the manuscript. MEC contributed to writing the manuscript. NL & DS contributed significantly to data analysis and reviewing drafts of the manuscript. JL & WT contributed to writing and reviewing drafts of the manuscript.
Acknowledgement
The authors gratefully acknowledge the women who participated in the study, the research assistants, staff at Muhimbili National Hospital, the Muhimbili University College of Health Sciences, and City of Dar es Salaam Health Department for their support. Special thanks are extended to Illuminata Ballonzi, Juliana Mghamba, Gertrude Kessy, Izera Marko, and Dr. Heavington Mshiu.
Kaaya, S. , Garcia, M. E. , Li, N. , Lienert, J. , Twayigize, W. , Spiegelman, D. , and Smith Fawzi, M. C. (2016) Association of maternal depression and infant nutritional status among women living with HIV in Tanzania. Maternal & Child Nutrition, 12: 603–613. doi: 10.1111/mcn.12154.
References
- Ammaniti M., Ambruzzi A.M., Lucarelli L., Cimino S. & D'Olimpio F. (2004) Malnutrition and dysfunctional mother‐child feeding interactions: clinical assessment and research implications. Journal of the American College of Nutrition 23, 259–271. [DOI] [PubMed] [Google Scholar]
- Anoop S., Saravanan B., Joseph A., Cherian A. & Jacob K.S. (2004) Maternal depression and low maternal intelligence as risk factors for malnutrition in children: a community based case‐control study from South India. Archives of Disease in Childhood 89, 325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antelman G., Kaaya S., Wei R., Mbwambo J., Msamanga G.I., Fawzi W.W. et al (2007) Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. Journal of Acquired Immune Deficiency Syndromes 44, 470–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avan B., Richter L.M., Ramchandani P.G., Norris S.A. & Stein A. (2010) Maternal postnatal depression and children's growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Archives of Disease in Childhood 95, 690–695. [DOI] [PubMed] [Google Scholar]
- Baker‐Henningham H., Powell C., Walker S. & Grantham‐McGregor S. (2005) The effect of early stimulation on maternal depression: a cluster randomised controlled trial. Archives of Disease in Childhood 90, 1230–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadhead W.E., Gehlbach S.H., Degruy F.V. & Kaplan B.H. (1988) The duke‐UNC functional social support questionnaire. Medical Care 26, 709–723. [DOI] [PubMed] [Google Scholar]
- Cox J.L. (1979) Psychiatric morbidity and pregnancy: a controlled study of 263 semi‐rural Ugandan women. The British Journal of Psychiatry: The Journal of Mental Science 134, 401–405. [DOI] [PubMed] [Google Scholar]
- De Miranda C.T., Turecki G., Mari Jde J., Andreoli S.B., Marcolim M.A., Goihman S. et al (1996) Mental health of the mothers of malnourished children. International Journal of Epidemiology 25, 128–133. [DOI] [PubMed] [Google Scholar]
- Dodds S., Nuehring E.M., Blaney N.T., Blakely T., Lizzotte J.M., Lopez M. et al (2004) Integrating mental health services into primary HIV care for women: the Whole Life project. Public Health Reports 119, 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawzi W., Msamanga G.I., Hunter D., Renjifo B., Antelman G. & Bang H. (2002) Randomized trial of vitamin supplements in relation to transmission of HIV‐1 through breastfeeding and early child mortality. AIDS (London, England) 16, 1935–1944. [DOI] [PubMed] [Google Scholar]
- Fawzi W.W., Msamanga G.I., Spiegelman D., Urassa E.J.N. & Hunter D.J. (1999) Rationale and design of the Tanzania Vitamin and HIV Infection Trial. Controlled Clinical Trials 20, 75–90. [DOI] [PubMed] [Google Scholar]
- Fawzi W.W., Msamanga G.I., Wei R., Spiegelman D., Antelman G., Villamor E. et al (2003) Effect of providing vitamin supplements to human immunodeficiency virus‐infected, lactating mothers on the child's morbidity and CD4+ cell counts. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America 36, 1053–1062. [DOI] [PubMed] [Google Scholar]
- Harpham T., Huttly S., De Silva M.J. & Abramsky T. (2005) Maternal mental health and child nutritional status in four developing countries. Journal of Epidemiology and Community Health 59, 1060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley M., Tomlinson M., Greco E., Comulada W.S., Stewart J., le Roux I. et al (2011) Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri‐urban settlements. Reproductive Health 8, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaaya S.F., Fawzi M., Mbwambo J., Lee B., Msamanga G. & Fawzi W. (2002) Validity of the Hopkins Symptom Checklist‐25 amongst HIV‐positive pregnant women in Tanzania. Acta Psychiatrica Scandinavica 106, 9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugina H.I., Christensson K., Massawe S., Nystrom L. & Lindmark G. (2001) Change in maternal concerns during the six weeks postpartum period: a study of primiparous mothers in Dar es Salaam, Tanzania. Journal of Midwifery & Women's Health 46, 248–257. [DOI] [PubMed] [Google Scholar]
- Medhin G., Hanlon C., Dewey M., Alem A., Tesfaye F., Lakew Z. et al (2010) The effect of maternal common mental disorders on infant undernutrition in Butajira, Ethiopia: the P‐MaMiE study. BMC Psychiatry 10, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miettinen O. (1985) Theoretical Epidemiology: Principles of Occurrence Research in Medicine. Wiley: New York. [Google Scholar]
- Nasreen H., Kabir Z., Forsell Y. & Edhborg M. (2010) Low birth weight in offspring of women with depressive and anxiety symptoms during pregnancy: results from a population based study in Bangladesh. BMC Public Health 10, 515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okronipa H., Marquis G.S., Lartey A., Brakohiapa L., Perez‐Escamilla R. & Mazur R.E. (2012) Postnatal depression symptoms are associated with increased diarrhea among infants of HIV‐positive Ghanaian mothers. AIDS and Behavior 16, 2216–2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., DeSouza N. & Rodrigues M. (2003) Postnatal depression and infant growth and development in low income countries: a cohort study from Goa, India. Archives of Disease in Childhood 88, 34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Rahman A., Jacob K. & Hughes M. (2004) Effect of maternal mental health on infant growth in low income countries: new evidence from South Asia. BMJ (Clinical Research Ed.) 328, 820–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez E.M., Hendricks M.K., Beard J.L., Murray‐Kolb L.E., Berg A., Tomlinson M. et al (2005) Mother‐infant interactions and infant development are altered by maternal iron deficiency anemia. Journal of Nutrition 135, 850–855. [DOI] [PubMed] [Google Scholar]
- Rahman A., Iqbal Z., Bunn J., Lovel H. & Harrington R. (2004) Impact of maternal depression on infant nutritional status and illness: a cohort study. Archives of General Psychiatry 61, 946–952. [DOI] [PubMed] [Google Scholar]
- Rahman A., Bunn J., Lovel H. & Creed F. (2006) Maternal depression increases infant risk of diarrhoeal illness: a cohort study. Archives of Disease in Childhood 92, 24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A., Bunn J., Lovel H. & Creed F. (2007) Association between antenatal depression and low birthweight in a developing country. Acta Psychiatrica Scandinavica 115, 481–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart R.C. (2007) Maternal depression and infant growth: a review of recent evidence. Maternal and Child Nutrition 3, 94–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan P.J., Kawachi I., Ryan L.M., Berkman L.F., Carvalho Vieira L.M. & Peterson K.E. (2007) Maternal depressive symptoms, parenting self‐efficacy, and child growth. American Journal of Public Health 97, 125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan P.J., Mukherjee J.S., Williams D.R., Eustache E., Louis E., Jean‐Paul T. et al (2010) Perceived discrimination and stigma toward children affected by HIV/AIDS and their HIV‐positive caregivers in central Haiti. AIDS Care 22, 803–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan P.J., Kennedy C.E., Hurley K.M. & Black M.M. (2011) Maternal depression and early childhood growth in developing countries: systematic review and meta‐analysis. Bulletin of the World Health Organization 89, 607–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M., Cooper P.J., Stein A., Swartz L. & Molteno C. (2006) Post‐partum depression and infant growth in a South African peri‐urban settlement. Child: Care, Health and Development 32, 81–86. [DOI] [PubMed] [Google Scholar]
- Wachs T.D., Black M.M. & Engle P.L. (2009) Maternal depression: a global threat to children's health, development, and behavior and to human rights. Child Development Perspectives 3, 51–59. [Google Scholar]
- Wojcicki J.M., Holbrook K., Lustig R.H., Epel E., Caughey A.B., Muñoz R.F. et al (2011) Chronic maternal depression is associated with reduced weight gain in Latino infants from birth to 2 years of age. PLoS ONE 6, e16737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2009) World Health Organization: Infant and Young Child Feeding Model Chapter for Textbooks for Medical Students and Allied Health Professionals. World Health Organization: Geneva. [PubMed] [Google Scholar]
- World Health Organization (WHO) Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards: Length/height‐for‐Age, Weight‐for‐Age, Weight‐for‐Length, Weight‐for‐Height and Body Mass Index‐for‐Age: Methods and Development. World Health Organization: Geneva. [Google Scholar]


