Abstract
Purpose
This study examines the effect of a history of childhood maltreatment on parenting sense of competence, taking into account the influence of resilience and postpartum depressive symptoms as moderators of this relationship.
Methods
Participants (N = 131) were a community sample of women recruited into a larger study of maternal childhood maltreatment. Women completed questionnaires over the phone at 4 months postpartum and parenting sense of competence (PSOC) was assessed during a home visit at 6 months postpartum.
Results
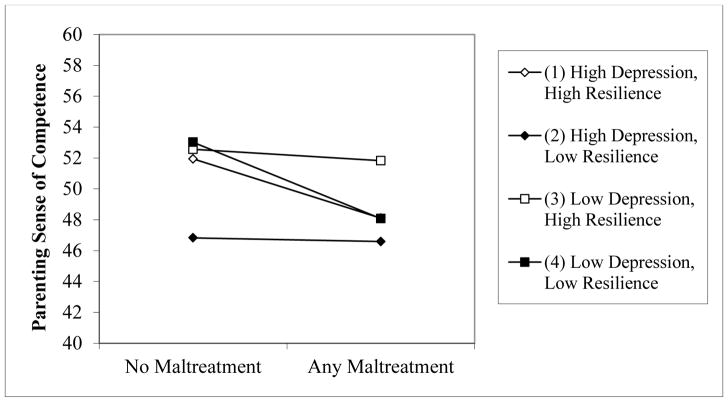
A three-way interaction emerged; women with low depression and high resilience factors maintained high levels of PSOC, even when they had a CM history. In contrast, among women with one postpartum risk factor (depression or low resilience) CM was associated with decreased PSOC.
Conclusions
Results suggest that a mother’s well-being postpartum moderates the effect of a childhood maltreatment history on her parenting sense of competence. Reducing postpartum depressive symptoms and enhancing resilience may be important components for interventions that address parenting confidence with maltreated women.
Keywords: Childhood Maltreatment, Parenting Competence, Depression, Resilience
INTRODUCTION
Childhood maltreatment is defined by the World Health Organization (WHO) as physical, sexual, or psychological acts towards or neglect of a child (under 18-years-old) by a parent or caregiver. This maltreatment can include any behavior or lack of a behavior on the part of the caregiver that results in actual or potential harm to the child’s health, survival, development of dignity (WHO, 2016). Women with a history of childhood maltreatment (CM) are more likely to abuse or neglect their children, report using more physical punishment, and show less sensitive and more intrusive mother-child interactions (Banyard, Williams, & Seigal, 2003; DiLillo & Damashek, 2003; Moehler, Biringen, & Poustka, 2007; Roberts, O’Conner Dunn & Golding, 2004; Schuetz & Eiden, 2005). Parenting behaviors are informed by women’s mental states regarding parenting, that is, the various frameworks through which they perceive themselves as parents (Michl et al., 2015; Slagt et al., 2012), including parenting sense of competence (PSOC): parents’ beliefs that they are capable of the job of parenting and ensuring positive outcomes for their children, and a sense of being satisfied with “how they are doing” in the parenting role (Caldwell, Shaver, Li, & Minzberg, 2011). A large body of research has linked PSOC with parenting behaviors and the quality of mother-infant relationships (for review see Jones & Prinz, 2005) and parenting interventions have found that increases in PSOC are associated with more effective parenting behaviors and decreased child behavior problems (Gross et al., 1995; Miller Heyl et al., 1998), highlighting the key role of parenting self-efficacy.
While research generally supports that a history of CM influences women’s PSOC (Banyard, 1997; Banyard, Williams & Siegel, 2003; Fitzgerald et al., 2005), studies report somewhat mixed findings regarding direction of effects. Caldwell, Shaver, Li, and Minzenberg (2011) reported links between maltreatment experiences (inclusive of physical, sexual, and emotional abuse, as well as neglect) and PSOC among a group of at-risk mothers (i.e., low SES, addiction, or early motherhood). Similarly, Bailey and colleagues (2012), Pazdera, McWey, Mullis and Carbonell (2013), and Schuetz and Eiden (2005) reported that childhood sexual abuse was associated with a decreased PSOC. In contrast, Zuravin and Fontanella (1999) found only physical neglect during childhood associated with lower levels of PSOC, whereas there was no association of PSOC with sexual abuse in their sample. Unexpectedly, Lang et al. (2010) documented that physical abuse was not associated with PSOC, while emotional abuse was linked with lower levels of frustration in the child and more pleasure in the relationship, two aspects related to more adaptive PSOC (Lang et al., 2010). Discrepant findings may reflect heterogeneity of outcomes for CM survivors, which has also been reported in regards to maternal behaviors: a significant number of women who were maltreated as children display high levels of maternal warmth and sensitivity, support, assistance, and infant affection during interactions (Fitzgerald et al., 2005; Martinez-Torteya et al., 2014).
Moreover, inconsistent findings may also reflect more proximal factors, including mothers’ well-being during the postpartum period. Post-partum depression, is a robust predictor of decreased parenting capacity, including diminished PSOC (Jones & Prinz, 2005; Roberts et al., 2004) and can mediate the effects of childhood abuse on a variety of parenting outcomes, including mother-child bonding and PSOC (Morelen et al., 2016; Seng et al., 2013). Parents’ assessment of their caregiving capacity, may be affected by the general negative world-view that is symptomatic of depression, and women who think of themselves as bad parents may then be likely to behave in ways that are consistent with this belief (Fitzgerald et al., 2005). Also, the depressive symptoms of pervasive deep sadness and anhedonia may get in the way of engaging in playful interactions with the children, and these difficulties in bonding may decrease confidence in one’s abilities as a parent.
Maternal postpartum wellbeing is also influenced by maternal strengths and resilience. Resilience can be defined as “the personal qualities that enable one to thrive in the face of adversity” (Conner & Davidson, 2003). Conceptualizations of resilience typically include the use of specific coping-strategies, including, social support and religious participation, as well as a broader sense of being able to overcome difficulties (Mguni, Bacon, & Brown 2012). Notably, resilience factors can enhance mental health outcomes for woman with histories of maltreatment and decrease risk for depression (Schulz et al., 2014; Wingo et al., 2010). In fact, analyses with our sample previously documented that, among mothers with the highest quartile of resilience factors, none met criteria for MDD even if they experienced CM; in contrast, among mothers in the lowest quartile of resilience, 25% of those with low CM and 68% of those with high CM met criteria for MDD (Sexton et al., 2015). In addition, transactional effects between resilience and depression likely shape the parenting outcomes of women with CM histories. Seltmann & Wright (2013) found an interaction between maternal depression and social support (one aspect of resilience) predicted positive parenting outcomes among sexual abuse survivors: social support promoted positive parenting in the context of low depressive symptoms, but was unrelated to parenting when they were significantly depressed. However, research specific to PSOC has not evaluated the interplay between CM experiences and various wellness and mental health factors in the postpartum period.
Current Study Aims
The current research evaluates the effects of women’s childhood maltreatment history, postpartum depressive symptoms and resilience on later maternal parenting sense of competence. This research addresses limitations of previous studies by using a prospective design, assessing women’s wellness postpartum, specifically depression and resilience, along with their CM history, and evaluating direct and interactive (moderation) effects of these factors on PSOC levels. We hypothesize that CM and maternal postpartum depression predict lower maternal PSOC, while maternal resilience factors predict higher PSOC. Second, we hypothesize that resilience will buffer the negative effects of CM on PSOC, while postpartum depressive symptoms will increase the negative effects of CM on PSOC.
METHOD
Participants and Procedures
The women in this study (n = 131) were drawn from a larger study cohort (N = 268) examining the effects of maternal history of childhood maltreatment on mothers’ postpartum adaptation, parenting, and their children’s outcomes (Maternal Anxiety during the Childbearing Years “MACY” study; NIMH K23 MH080147). MACY enrolled 256 community mothers within the first 4 months postpartum and oversampled for women with CM (66%). Participants were recruited from either a pregnancy survey of women care at eight maternity clinics in three Health Systems in the Midwest (n = 145; see Seng, Low, Sperlich, Ronis, & Liberzon, 2009 for details) or through community advertisement via flyers posted in pediatric and primary care clinics, resource centers (e.g., Women Infant and Children - WIC offices), or businesses and infant play groups (n = 111). The flyer invited participation of women who had “experienced difficult childhood upbringing,” and were now parenting an infant. Criteria for eligibility were: at least 18-years-old, able to speak English, and being mother to a healthy full-term 0 to 4 months old baby. Exclusionary criteria were: history of schizophrenia or bipolar disorder, or alcohol or illicit substance abuse within the last three months. Data collection for the parent study spanned from 4 to 18 months postpartum. At different time points in the study, assessments were conducted in the home, the University-based playroom, or by phone. Although some women were recruited during pregnancy, no data were collected during pregnancy.
The sample for the current substudy (n=131) is restricted to women who completed assessments at both four (phone) and six months (home visit) postpartum. One hundred and fifty three women from the original cohort completed the six months postpartum home visit, while 103 women could not be reached or declined participation primarily due to scheduling conflicts. This study’s final sample of 131 women excludes women with incomplete data on the measures for the main constructs of interest. Women were primarily White, middle class, and living with a romantic partner (Table 1). Sixty percent of mothers had infant boys (n = 78). Participants in this study were not significantly different from the additional women in the larger parent study sample (n = 125) on key demographic variables such as race and income, their rates of CM, or mean scores for postpartum depression, resilience, and PSOC.
Table 1.
Participant Characteristics
| Variable | Frequency | Percentage | |
|---|---|---|---|
|
| |||
| Age | M = 29 years (SD = 5.59) | ||
|
| |||
| Baby Gender | Female | 64 | 48.9% |
| Male | 67 | 51.1% | |
|
| |||
| Mother Ethnicity | Caucasian | 88 | 67.2% |
| African American | 24 | 18.3% | |
| Latino | 6 | 4.6% | |
| Asian/Other Pacific Island | 5 | 3.8% | |
| Bi-racial | 3 | 2.3% | |
| Other | 3 | 2.3% | |
| No Answer | 2 | 1.5% | |
|
| |||
| Yearly Income | < 15,000 | 27 | 20.6% |
| 15,000 to 24,999 | 13 | 9.9% | |
| 25,000 to 49,999 | 29 | 22.1% | |
| >= 50,000 | 60 | 45.8% | |
| No answer | 2 | 1.5% | |
|
| |||
| Marital Status | Married | 94 | 71.8% |
| Never Married | 27 | 20.6% | |
| Living with birth father | 8 | 6.1% | |
| Living with partner other than birth father | 1 | 0.8% | |
| Widowed | 1 | 0.8% | |
|
| |||
| Occupation status | Working for Pay or Self Employed | 63 | 48.1% |
| Homemaker | 33 | 25.2% | |
| Looking for Employment | 15 | 11.5% | |
| Full-time Student | 8 | 6.1% | |
| Part-time Student | 4 | 3.1% | |
| Maternity or Sick Leave | 2 | 1.5% | |
| Permanently Disabled | 2 | 1.5% | |
| Other | 4 | 3.1% | |
Maltreatment history, depression symptoms and resilience characteristics were assessed over the phone during the 4 months postpartum call, while PSOC was assessed during the 6 months postpartum home visit. The short longitudinal design permits evaluation of the effects of early postpartum adaptation on later parenting sense of competence. Also, most women who develop postpartum depression do so in the first 4 months after birth (Kettunen et al., 2014) making this a key time to screen for depressive symptoms. Last, six months after birth, parental self-efficacy is likely to be more stable than during the early postpartum months, and studies that assessed PSOC during this first year postpartum report links with later parenting behaviors (Teti & Gelfand, 1991).
Measures
Childhood Maltreatment: the Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998) is a standardized, retrospective 28-item self-report scale that measures childhood physical abuse (e.g., “I was punished with a belt, a board, a cord or some other hard object”), emotional abuse (e.g., “People in my family said hurtful or insulting things to me”), sexual abuse (e.g., “Someone tried to make me do sexual things or watch sexual things”), emotional neglect (e.g., “I felt loved” [reverse coded]) and physical neglect (e.g., “I didn’t have enough to eat”). Respondents rate the truth of each statement on a 5-point Likert scale, from “Never true when I was growing up” to “Very often true when I was growing up.” The CTQ has demonstrated good psychometric properties (Scher et al., 2001). The scale was normed with a non-clinical sample of females and cut off scores are provided to determine “any” abuse and “severe” abuse. We used a dichotomous maltreatment score (presence of any type vs. absence) based on norm-derived cut off scores for each subscale. The cut-off scores were derived from and designed to maximize sensitivity (79 to 89%) and specificity (82 to 86%; Bernstein & Fink, 1998). Using the total score (alpha =.75; M = 43.48, SD = 18.13).
Maternal Depression: the Postpartum Depression Screening Scale (PDSS; Beck & Gamble, 2002) is a 35-item self-report measure that assesses seven dimensions of depression during the past two weeks: sleeping/eating disturbances, anxiety/insecurity, emotional liability, cognitive impairment, loss of self, guilt/shame, and contemplating harming oneself. Women rate these on a 5-point Likert scale, from “Strongly disagree” to “Strongly agree.” The measure has good psychometric properties and total scores >= 80 or higher denote clinically significant symptomology (Beck & Gable, 2002; Boyd, Le & Somberg, 2005). We used the total score (alpha = .96; M = 62.05, SD = 21.39).
Maternal Resilience: the Connor-Davidson Resilience scale (CD-RISC) has 25 items, each rated on a 5-point agreement scale, with higher total scores reflecting greater resilience, including tenacity and high standards (e.g., “You work to attain your goals”), acceptance of change (e.g. “I can deal with whatever comes my way”), ability to tolerate negative affect (e.g., “Coping with stress strengthens”), security of relationships (e.g., “Close and secure relationships”), control (e.g. “In control of your life”), and spiritual influences (e.g., “Sometimes fate or god can help.”) The measure has good psychometric properties (Conner & Davidson, 2003). We used the total score (alpha = .90; M = 76.72, SD = 12.03).
Parenting Sense of Competence: the adapted Parenting Sense of Competence Scale focuses on the satisfaction scale (PSCS; Mowbray et al., 2005) and includes 11-items rated on a 5-point Likert scale, ranging from “Very dissatisfied” to “Very satisfied.” (e.g., “How satisfied are you with your ability to care for and protect your child?”). This measure has good reliability (Johnston & Mash, 1989; Ohan, Leung & Johnston 2000). The validity of the parenting sense of competence scores has been demonstrated through links with various parenting behaviors (e.g., supportive behaviors, ineffective disciplining) in both cross-sectional and longitudinal studies (Shumow & Lomax, 2002; Slagt et al., 2012; Teti & Gelfand, 1991). We used a Total score (alpha = .87; M = 49.64, SD = 5.38).
Data Analysis Plan
Step-wise multiple regression with 1,000 bootstrap samples on IBM SPSS 25.0 were used to evaluate the effects of maltreatment, depressive symptoms, and resilience on PSOC. Continuous variables were centered to prevent issues with multicollinearity. The first step of the model included the main effects for each predictor. Two-way interaction terms (i.e., CM-by-Depression, CM-by-Resilience, and Depression-by-Resilience) were computed and added to the second step of the regression. The three-way interaction was added as a third step in the regression model.
RESULTS
Descriptive Statistics and Bivariate Correlations
Emotional abuse and emotional neglect were most commonly reported (52% and 43%, respectively), followed by sexual abuse (37%), physical abuse (30%) and physical neglect (13%). Sixty-eight percent of women reported experiencing any type of abuse. Mean levels of depression were in the normative range (M = 62.05, SD = 21.39). Seventeen percent (n = 25) of women reported scores that were clinically significant. Point-biserial correlations showed a significant positive relationship between CM and depression (r = .33, p < .05), as well as negative relationships between CM and resilience (r = -,28, p < .05), and CM and PSOC (r = -,23, p < .05). Pearson’s correlations showed negative associations between depression and resilience (r = −.54, p < .05) and depression with PSOC (r = −.31, p < .05). Sense of competence was positively associated with resilience (r = .32, p < .05) but not associated with demographic risk (family income and maternal education); thus, these variables were not used as covariates in analyses.
Moderator Analyses
The step-wise approach showed that the three-way interaction was a significant predictor of PSOC; thus, the results of Model 3 are reported here (See Table 1 for statistics for the three models). The model predicted a significant proportion of the variance in PSOC, r-squared = .18, F (7,123) = 3.93, p = .001.. Childhood maltreatment history predicted decreases in PSOC, b = −2.41, p = .029, but the effects of resilience and depression were not significant. The 2-way interactions were not significant predictors, but the 3-way-interaction had a significant effect, b = −.01, p < .025. PSOC levels were plotted out for women with and without CM histories, and at +1 and −1 SDs from the mean for depression and resilience, following Aiken & West (1991; see Figure 1). Among women with low levels of depression and high levels of resilience (i.e., the “healthiest” group) there was no association between CM and PSOC; these women reported high levels of PSOC regardless of maltreatment experiences. Similarly, the women who were most at risk during the postpartum period due to high levels of depression and low levels of resilience had the lowest PSOC scores, regardless of CM history. In contrast, CM was strongly associated with decreases in PSOC for women who experienced one “type” of adversity during the postpartum period and were either experiencing high depression or low resilience (but not both).
Figure 1.
Three-way interaction between CM, depression and resilience predicting parenting sense of competence
DISCUSSION
This study sought to clarify the impact of CM history, postpartum depression, and maternal resilience on parenting sense of competence at 6 months postpartum. Results in the current study showed complex interactions between CM history and depression and resilience during the postpartum period. A significant three-way interaction between CM, postpartum depression, and resilience emerged. Results suggests that the effect of CM on a parenting sense of competence is contingent on mothers’ level of resilience and depression postpartum; both depression and low resilience potentiated the negative effects of CM on PSOC. But, a combination of low depression and high resilience buffered the negative effects of CM, and these maltreated women with healthy postpartum adaptation maintained high levels of PSOC that were similar to those of non-maltreated women and were higher than those of non-maltreated women who experienced high depression and low resilience postpartum.
The effects of CM appear to be buffered for women with low depression and high resilience. Our findings align with the results of Seltmann and Wright’s (2013) who report that a combination of high partner support (i.e., one form of resilience) and low depression was protective against mother-child communication problems among childhood sexual abuse survivors. Our finding is also consistent with previous research that documents that high levels of resilience predict higher PSOC (Banyard et el., 2003; Hass et al., 2003), as well as findings that resilience buffers the negative effects of CM history on other adult outcomes (Wingo et al., 2010). Different types of resilience factors likely enhance parenting sense of competence through multiple mechanisms. For example, social support can include instrumental or child care support, which may help parents better meet their child’s needs, enhancing their sense of competence, and fostering more positive perceptions and interpretations of child behavior (Levine, Garcia-Coll, & Oh, 1985; Mercer, Hackley, & Bostrom, 1984). In addition, social supports may provide encouragement and positive feedback, giving mothers more emotional resources to handle difficult child behavior. On the other hand, religious coping has been linked with more general (not caregiving) self-efficacy and life satisfaction (Bagley & Mallick, 1997; Pergament, 1997), which may extend to the realm of caregiving.
On the other hand, among women who experienced only one of the assessed post-partum risk factors (low resilience or high depression), CM was a powerful predictor of decreased PSOC. This finding is consistent with cumulative risk models (Sameroff, Seifer, & McDonough, 2004), such that aggregate postpartum adversity made women most susceptible to the deleterious influence of CM; these mothers may not have had positive examples of parenting, and therefore be unable to use positive memories and practices from their own families of origin to rely on during difficult postpartum circumstances (Banyard, Williams, & Seigal, 2003).
Women with high levels of depression and low resilience reported low levels of PSOC regardless of their CM status. Depression is a powerful influence on women’s interactions with their children: on one hand, symptoms of sadness and irritability can decrease the threshold for frustrations and lead to harsher reactions to children’s behavior, while symptoms of anhedonia and fatigue can decrease engagement and joy during interactions, making the experience of parenting less satisfying (Fitzgerald et al., 2005). These negative and unsatisfying interactions then influence how women see themselves as mothers. Depression also decreases PSOC through decreased hopefulness about the future and a higher propensity for worry (Banyard, 1997).
Last, our results showed that with this specific sample, primarily white, middle class, and with relatively high education levels, demographic variables were not predictive of PSOC. This is a finding that has occurred in various studies of PSOC (Ohan, Leung & Johnston, 2000). Other studies of parenting competence have found significant correlations to demographics such as maternal education, family income and infant age (both positively correlated). This same study found that mothers who lived with or were married to their partners had high maternal competence than those without partners (Teti & Gelfand, 1991).
The limitations of the study should be noted. All measures were assessed via maternal report, increasing the risk that associations are inflated due to reporter biases. Specifically, it may be that current depression or low resilience influenced women’s recall for their maltreatment experiences growing up. Future studies would benefit from a multi-method, multi-informant approach. Second, our “longitudinal” follow-up period of two months is short. Longer follow-up can help understand developmental changes on PSOC among this group of women, as they gather more experiences with their children. This future study could also allow the provision of looking and child outcomes as well. In addition, the current research focused on depression because it is a common mental health outcome for CM survivors and has strong links with parenting outcomes (Banyard, Williams & Seigal 2003). However, future research should also assess substance abuse problems, which are often co-morbid with internalizing problems among trauma-exposed women (MacMillan et al., 2001). Finally, our sample was recruited from the community, making it so that experiences of those women who were most impaired may not have been captured; clinical and community studies are needed to complement our knowledge of women’s postpartum experiences. In addition, women with relatively high education and middle-income levels are over represented, and these characteristics are associated with higher parenting competency and lower rates of childhood maltreatment. Ethnically, the demographics somewhat mirror, national proportions but have a lower representation of Latina participants. This makes our study limited in its generalizability to populations with lower education levels, much lower or much higher income, or slightly more ethnically diverse groups.
IMPLICATIONS FOR PRACTICE, APPLICATION AND POLICY
Findings highlight the importance of appropriate mental health intervention for postpartum depression for women, particularly survivors of CM. Significant evidence demonstrates that intensive postpartum support can effectively reduce depressive symptoms (Dennis, 2005). However, research also shows that intervention-related improvements in depressive symptoms do not directly translate into parenting gains (Muzik, Marcus, Heringhausen, & Flynn, 2009). Our findings suggest that enhancing resilience factors (e.g., spirituality, social support) may be a fruitful target of intervention and may be incorporated to treatment efforts that more explicitly focus on the parent-child relationship (e.g., Mom Power intervention; Muzik et al., 2015). Qualitative work that documents CM survivor mothers’ accounts of their health care needs during postpartum, supports that comprehensive services that address multiple domains of risk and protection are desired (Muzik et al., 2013). In addition, this research provides evidence for placing more time and resources into the reduction of child maltreatment as the effects of child maltreatment are not only impacting the affected person but may be passed on for generations.
In sum, our results suggest complex interactions between CM experiences and resilience and depression, and how these factors help to shape women’s parenting sense of competence during the first year of their infants’ lives. Notably, women with low depression and high resilience factors were protected from the negative effects of CM and maintained high levels of PSOC. In contrast, a combination of postpartum adversity (high depression and/or low resilience) and CM lead to significantly lower levels of PSOC two months later. This research has implications for practice, suggesting the importance of addressing depression and promoting resilience factors among women who have suffered childhood maltreatment in order to improve their parenting outcomes.
Table 2.
Childhood Maltreatment-by-Depression-by-Resilience Interaction Predicts PSOC
| Predictor Variables | B | SE | p | 95% CI |
|---|---|---|---|---|
| Model 1: Main Effects | ||||
| Childhood Maltreatment | −1.73 | 1.01 | .046 | −3.32, −.20 |
| Depression | −.05 | .02 | .059 | −.10, −.01 |
| Resilience | .09 | .04 | .020 | −.02, .16 |
| Model 2:Two-way Interactions | ||||
| Childhood Maltreatment | −1.71 | 1.08 | .087 | −3.91, .06 |
| Depression | −.07 | .05 | .141 | −.14, .03 |
| Resilience | .05 | .10 | .4855 | −.09, .17 |
| CM-by-Depression | .01 | .06 | .809 | −.10, .10 |
| CM-by-Resilience | .05 | .11 | .489 | −.08, .21 |
| Depression-by-Resilience | −.00 | .00 | .192 | −.01, .00 |
| Model 3: Three-way Interaction | ||||
| Childhood Maltreatment | −2.41 | 1.17 | .029 | −4.59, −.42 |
| Depression | −.08 | .05 | .055 | −.15, .01 |
| Resilience | −.10 | .11 | .125 | −.03, .26 |
| CM-by-Depression | .02 | .06 | .679 | −.09, .11 |
| CM-by-Resilience | .00 | .12 | .982 | −.18, .16 |
| Depression-by-Resilience | .01 | .01 | .091 | −.00, .01 |
| 3-way-interaction | −.01 | .00 | .025 | −.02, −.00 |
Acknowledgments
This research was conducted at the University of Michigan supported by the National Institute of Health-Michigan Mentored Clinical Scholars Program awarded to M Muzik (K12 RR017607-04, PI: D. Schteingart); the National Institute of Mental Health -Career Development Award K23 (NIH, PI: Muzik); and the Michigan Institute for Clinical and Health Research (MICHR, UL1TR000433, PI: Muzik). The authors have no financial disclosures to make.
Contributor Information
Cecilia Martinez-Torteya, Associate Professor, DePaul University, Department of Psychology, 2219 N Kenmore Ave, Chicago, IL 60614, and Department of Psychopedagogy, Universidad de Monterrey, Mexico.
Katherine Lisa Rosenblum, Professor, University of Michigan, Department of Psychiatry, and Center for Human Growth & Development, University of Michigan, Ann Arbor.
Tiamo Katsonga-Phiri, Graduate student, DePaul University, Department of Psychology, 2219 N Kenmore Ave, Chicago, IL 60614.
Hamilton Lindsay, Graduate student, Bowling Green State University, Bowling Green, OH.
Maria Muzik, Associate Professor, University of Michigan, Department of Psychiatry, and Center for Human Growth & Development, University of Michigan, Ann Arbor.
References
- Banyard VL. The impact of childhood sexual abuse and family functioning on four dimensions of women’s later parenting. Child abuse & neglect. 1997;21(11):1095–1107. doi: 10.1016/s0145-2134(97)00068-9. [DOI] [PubMed] [Google Scholar]
- Banyard VL, Williams LM, Siegel JA. The impact of complex trauma and depression on parenting: An exploration of mediating risk and protective factors. Child maltreatment. 2003;8(4):334–349. doi: 10.1177/1077559503257106. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Postpartum Depression Screening Scale: development and psychometric testing. Nursing Research. 2000;49(5):272–282. doi: 10.1097/00006199-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Boyd RC, Le HN, Somberg R. Review of screening instruments for postpartum depression. Archives of Women’s Mental Health. 2005;8(3):141–153. doi: 10.1007/s00737-005-0096-6. [DOI] [PubMed] [Google Scholar]
- Caldwell JG, Shaver PR, Li CS, Minzenberg MJ. Childhood maltreatment, adult attachment, and depression as predictors of parental self-efficacy in at-risk mothers. Journal of aggression, maltreatment & trauma. 2011;20(6):595–616. [Google Scholar]
- Dennis CL. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. Bmj. 2005;331(7507):15. doi: 10.1136/bmj.331.7507.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLillo D, Damashek A. Parenting characteristics of women reporting a history of childhood sexual abuse. Child Maltreatment. 2003;8(4):319–333. doi: 10.1177/1077559503257104. [DOI] [PubMed] [Google Scholar]
- Fitzgerald MM, Shipman KL, Jackson JL, McMahon RJ, Hanley HM. Perceptions of parenting versus parent-child interactions among incest survivors. Child abuse & neglect. 2005;29(6):661–681. doi: 10.1016/j.chiabu.2004.10.012. [DOI] [PubMed] [Google Scholar]
- JonesT L, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: A review. Clinical Psychology Review. 2005;25(3):341–363. doi: 10.1016/j.cpr.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Kettunen P, Koistinen E, Hintikka J. Is postpartum depression a homogenous disorder: time of onset, severity, symptoms and hopelessness in relation to the course of depression. BMC pregnancy and childbirth. 2014;14(1):402. doi: 10.1186/s12884-014-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, Gartstein MA, Rodgers CS, Lebeck MM. The impact of maternal childhood abuse on parenting and infant temperament. Journal of Child and Adolescent Psychiatric Nursing. 2010;23(2):100–110. doi: 10.1111/j.1744-6171.2010.00229.x. [DOI] [PubMed] [Google Scholar]
- Levine L, Coll CTG, Oh W. Determinants of mother-infant interaction in adolescent mothers. Pediatrics. 1985;75(1):23–29. [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, … Beardslee WR. Childhood abuse and lifetime psychopathology in a community sample. Childhood. 2001;158(11) doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- Martinez-Torteya C, Dayton CJ, Beeghly M, Seng JS, McGinnis E, Broderick A, Muzik M. Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment. Development and psychopathology. 2014;26(02):379–392. doi: 10.1017/S0954579414000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer RT, Hackley KC, Bostrom A. Adolescent motherhood: Comparison of outcome with older mothers. Journal of Adolescent Health Care. 1984;5(1):7–13. doi: 10.1016/s0197-0070(84)80238-7. [DOI] [PubMed] [Google Scholar]
- Mguni N, Bacon N, Brown JF. The wellbeing and resilience paradox. London: The Young Foundation; 2012. [Google Scholar]
- Michl LC, Handley ED, Rogosch F, Cicchetti D, Toth SL. Self-criticism as a mechanism linking childhood maltreatment and maternal efficacy beliefs in low-income mothers with and without depression. Child maltreatment. 2015;20(4):291–300. doi: 10.1177/1077559515602095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moehler E, Biringen Z, Poustka L. Emotional availability in a sample of mothers with a history of abuse. American Journal of Orthopsychiatry. 2007;77(4):624. doi: 10.1037/0002-9432.77.4.624. [DOI] [PubMed] [Google Scholar]
- Morelen D, Menke R, Rosenblum KL, Beeghly M, Muzik M. Understanding bidirectional mother-infant affective displays across contexts: effects of maternal maltreatment history and postpartum depression and PTSD symptoms. Psychopathology. 2016;49(4) doi: 10.1159/000448376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Ads M, Bonham C, Lisa Rosenblum K, Broderick A, Kirk R. Perspectives on trauma-informed care from mothers with a history of childhood maltreatment: A qualitative study. Child Abuse & Neglect. 2013;37(12):1215–1224. doi: 10.1016/j.chiabu.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, Kohler ES. Mom Power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Archives of Women’s Mental Health. 2015;18(3):507–521. doi: 10.1007/s00737-014-0490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Marcus SM, Heringhausen JE, Flynn H. When depression complicates childbearing: guidelines for screening and treatment during antenatal and postpartum obstetric care. Obstetrics and gynecology clinics of North America. 2009;36(4):771–788. doi: 10.1016/j.ogc.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohan JL, Leung DW, Johnston C. The Parenting Sense of Competence scale: Evidence of a stable factor structure and validity. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement. 2000;32(4):251. [Google Scholar]
- Pazdera AL, McWey LM, Mullis A, Carbonell J. Child sexual abuse and the superfluous association with negative parenting outcomes: the role of symptoms as predictors. Journal of Marital and Family Therapy. 2013;39(1):98–111. doi: 10.1111/j.1752-0606.2011.00272.x. [DOI] [PubMed] [Google Scholar]
- Roberts R, O’Connor T, Dunn J, Golding J ALSPAC Study Team. The effects of child sexual abuse in later family life; mental health, parenting and adjustment of offspring. Child abuse & neglect. 2004;28(5):525–545. doi: 10.1016/j.chiabu.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Sameroff A, Seifer R, McDonough SC. Contextual contributors to the assessment of infant mental health. Handbook of infant, toddler, and preschool mental health assessment. 2004:61–76. [Google Scholar]
- Scher CD, Stein MB, Asmundson GG, McCreary DR, Forde DR. The childhood trauma questionnaire in a community sample: Psychometric properties and normative data. Journal Of Traumatic Stress. 2001;14(4):843–857. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- Schuetz P, Eiden RD. The relationship between sexual abuse during childhood and parenting outcomes: Modeling direct and indirect pathways. Child Abuse & Neglect. 2005;29:645–659. doi: 10.1016/j.chiabu.2004.11.004. [DOI] [PubMed] [Google Scholar]
- Schulz A, Becker M, Van der Auwera S, Barnow S, Appel K, Mahler J, … Grabe HJ. The impact of childhood trauma on depression: Does resilience matter? Population-based results from the Study of Health in Pomerania. Journal of psychosomatic research. 2014;77(2):97–103. doi: 10.1016/j.jpsychores.2014.06.008. [DOI] [PubMed] [Google Scholar]
- Seltmann LA, Wright MOD. Perceived parenting competencies following childhood sexual abuse: A moderated mediation analysis. Journal of family violence. 2013;28(6):611–621. [Google Scholar]
- Seng JS, Low LMK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics and Gynecology. 2009;114(4):839. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I. Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. Journal of Midwifery & Women’s Health. 2013;58(1):57–68. doi: 10.1111/j.1542-2011.2012.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton MB, Hamilton L, McGinnis EW, Rosenblum KL, Muzik M. The roles of resilience and childhood trauma history: Main and moderating effects on postpartum maternal mental health and functioning. Journal of Affective Disorders. 2015;174:562–568. doi: 10.1016/j.jad.2014.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shumow L, Lomax R. Parental self-efficacy: Predictor of parenting behavior and adolescent outcomes. Parenting: Science and Practice. 2002;2:127–150. doi: 10.1207/S15327922PAR0202_03. [DOI] [Google Scholar]
- Slagt M, Deković M, de Haan AD, van den Akker AL, Prinzie P. Longitudinal associations between mothers’ and fathers’ sense of competence and children’s externalizing problems: The mediating role of parenting. Developmental Psychology. 2012;48(6):1554–1562. doi: 10.1037/a0027719. [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM. Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Child maltreatment factsheet. Media Center; Sep, 2016. < http://www.who.int/mediacentre/factsheets/fs150/en/>. [Google Scholar]
- Zuravin SJ, Fontanella C. Parenting behaviors and perceived parenting competence of child sexual abuse survivors. Child abuse & neglect. 1999;23(7):623–632. doi: 10.1016/s0145-2134(99)00045-9. [DOI] [PubMed] [Google Scholar]