Abstract
Aim
To determine if delivering electronic messages from nurses during the first six months postpartum is feasible, acceptable and effective in improving mood and decreasing parenting stress.
Background
Competing demands during the postpartum hospitalization make focused time for nurses to provide education and support difficult. Unmet needs following discharge may increase the incidence of postpartum depression. Untreated depression negatively affects families, especially for vulnerable women with limited access to health care.
Design
This is a longitudinal cohort study in three phases. Feasibility and acceptability were assessed during Phases 1 & 2. Phase 3 is a randomized controlled trial (RCT) with three conditions.
Methods
This protocol was approved by the Institutional Review Board of the maternity hospital on 12 May 2015 and reviewed annually. Women are enrolled during the maternity hospitalization, after which randomization occurs. The control group receives usual care. Intervention I participants receive a standardized electronic message four times/week for six months postpartum. Intervention II participants receive the messages and the option to request a call from a nurse. Electronic surveys at 3 weeks, 3 months and 6 months postpartum measure depressive symptoms using the Edinburgh Postnatal Depression Scale and parenting stress using the Parenting Stress Index-Short form. Patient satisfaction, nursing time and expertise required are also measured.
Discussion
Phase 1 and 2 have demonstrated the intervention is feasible and acceptable to women. Phase 3 enrollment is completed, and the last follow-up surveys were emailed to participants in February 2018. Results will help inform efforts to continue nursing care after hospital discharge.
Keywords: postpartum, nursing, technology, depression, parenting stress, maternity
INTRODUCTION
It is vital to address the improvement of maternal mental health. Untreated perinatal mood disorders are a significant public health concern in both developed and developing countries and the effects extend beyond the mother to negative impacts on the growth and development of infants and children. Women with limited resources disproportionately bear the burden of postpartum depression (Fisher et al., 2012). Interventions for prevention and early intervention of perinatal mood disorders (including postpartum depression) which are accessible and cost-effective (Stein et al., 2014) must be developed and evaluated. Women frequently experience a vacuum in care during the postpartum period (Danbjørg, Wagner, & Clemensen, 2014; Guerra-Reyes, Christie, Prabhakar, & Siek, 2017; Kanotra et al., 2007) or are reluctant to seek care for mood-related concerns (Rahman et al., 2013). New strategies to improve postpartum outreach is a priority for maternity care world-wide (World Health Organization, 2014). Interventions provided by nurses from the maternity hospital could provide needed continuity of care using educational and supportive strategies (Rahman et al., 2013). Using technology, such strategies could reach women in their homes and be readily adapted to the community/population being served, expanding nursing care to address unmet needs for postpartum care and support.
Background
A key element of perinatal nursing care is to provide health teaching and health promotion (American Nurses Association, 2015). During the brief maternity hospitalization, there is little time for face-to-face discharge education due to the competing demands of rest and recovery from birth and establishing newborn feeding and family visits. The need for education and support after hospital discharge is also largely unmet and this vacuum is a risk factor for postpartum depression. Depressed mothers may not be able to provide necessary attention and care to newborns and as such put them in danger (Chung, McCollum, Elo, Lee, & Culhane, 2004).
While the prevalence and associated factors of postpartum mood disorders differs by country and cultural group (Abdollahi, Lye, Md Zain, Shariff Ghazali, & Zarghami, 2011), it is known that there are multiple adverse effects of untreated depression on women (Chung et al., 2004; Lindahl, Pearson, & Colpe, 2005; McLennan & Kotelchuck, 2000), fathers (Paulson, Dauber, & Leiferman, 2006) and children (Earls & The Committee on Psychosocial Aspects of Child and Family Health, 2010), particularly when other risk factors such as low socioeconomic status are also present (Stein et al., 2014).
Increasing access to postpartum care, including mental health, is an international priority (World Health Organization, 2014). In the United States, the standard follow-up visit after childbirth is at 6 weeks postpartum, but as many as 40% of women do not attend even this visit (American College of Obstetricians and Gynecologists (ACOG), 2016) and those who do may still not feel their needs have been met (Martin, Horowitz, Balbierz, & Howell, 2014). In addition, obstetrical providers may not address or screen for mood disorders during follow-up visits (Kim et al., 2009). Infants may be seen multiple times for well-baby checks in their first year but women may not feel they can disclose their depressive symptoms to the child’s pediatric provider (Heneghan, Mercer, & DeLeone, 2004) and treatment for adult mental health symptoms does not fall within the pediatric scope of practice. While there are readily available, accurate and valid screening instruments (Myers et al., 2013) for depression, which are acceptable to both women and health care providers (Brealey, Hewitt, Green, Morrell, & Gilbody, 2010), there is no universal agreement about whether such screening should be the responsibility of pediatric, obstetric or primary care practices.
Perinatal nurses may be in a unique position to fill the void of providing support and screening for postpartum mood disorders, but there is minimal time during the maternity hospitalization and no consistent mechanism for nursing follow-up after discharge. Nurses, as part of a multidisciplinary team, are charged with the responsibility of participating in the education, screening and management of women experiencing postpartum mood and anxiety disorders (Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN), 2015). Education about postpartum mood problems during the maternity hospitalization may not be effective (McCarter-Spaulding & Shea, 2016), but nursing care which extends to include support and screening into the post-discharge period may be structured as a continuation of a relationship developed during the intrapartum experience and decrease the stigma associated with accessing mental health services (Smith et al., 2009; Sword, Busser, Ganann, McMillan, & Swinton, 2008). Nurses can identify women at risk during the maternity hospitalization, as a history of anxiety and/or depression is known to be a risk factor for postpartum mood disorders (Hutto, Kim-Godwin, Pollard, & Kemppainen, 2011). Nurse screening for depression is acceptable to women (Segre, O’Hara, Arndt, & Beck, 2010), but it is not known how much nursing time and expertise would be required to extend this care after discharge.
Digital technology applications have been proposed as a way to reach socioeconomically and culturally diverse populations (Aguilera & Berridge, 2014; Drake, Howard, & Kinsey, 2014) and studies have addressed the feasibility, acceptability and success of using technology-based screening (Drake et al., 2014; Le, Perry, & Sheng, 2009), particularly when paired with a personal encounter (Danaher et al., 2012; Piette & Schillinger, 2007). Virtually all women of reproductive age in the United States have use of a cell phone, regardless of socioeconomic status, education, race or residence (Pew Research Center, 2017) and most also have access to other devices. This study seeks to evaluate whether using a digital technology intervention to facilitate nursing support for mothers for six months postpartum would reduce symptoms of postpartum depression and parenting stress and to identify women who need referral for further evaluation and treatment and to determine the amount of nursing time and expertise needed to provide this service. Results of this study may help inform the development of innovative nursing care models for outreach and support for mothers after hospital discharge. It is hypothesized that an intervention designed to increase support to new mothers would decrease parenting stress and postpartum depression.
THE STUDY
Aims
The overarching goal of the study is twofold: (1) Describe risk factors for depression identified during the postpartum hospitalization; (2) Evaluate whether nurse-led digital messaging intervention reduces symptoms of depression and parenting stress. The first goal seeks to use the hospital resources with maximum efficiency by targeting moms and families who are a priority for intervention. The second goal explores how the intervention should be done and its effectiveness.
Design/Methodology
This is a longitudinal cohort study in three phases. Phase 1 was designed to determine the feasibility of using digital technology as an adjunct to nurse outreach and follow-up. Phase 2 was designed to implement and evaluate the acceptability of a digital messaging intervention for postpartum support. Phase 3 of the study is an open, parallel, randomized, controlled trial with three groups. The control group receives the usual post-discharge care, which consists of a phone call made to each patient at approximately 2 weeks post-discharge by a lactation consultant. If the patient is not reached, a message is left to call back if desired. There are two intervention groups, designed to determine the impact of the messages independently from the option for nurse contact. In Intervention I, the participant receives four standardized messages each week for six months. In Intervention II, the participant receives the same four standardized messages/week and in addition, two of the messages offer the option of requesting a phone call from a nurse by responding either yes or no to the message when offered. On a “yes” response from the participant, the messaging system sends an emailed report to the principal investigator and the patient is called by a maternity nurse. Patients may choose to opt out of receiving messages at any time by a simple click at the end of the message.
Digital messages
The messages were developed by experienced maternal-child health nurses employed by the study hospital. The content was designed to be a mix of educational messages about infant care and maternal self-care and supportive, inspirational messages. The text of the messages can be accessed at the following url: https://drive.google.com/file/d/1-Hd4HFQkoJWwLFO4zMahyrgq4Q9tWCSz/view?usp=sharing (accessed 3 May 2018). The messages begin on the week following enrollment in the study and continue until six months postpartum.
The messages are delivered using Televox, an electronic system for communication (http://www.televox.com/company/about/; accessed 3 May 2018), designed primarily as a mechanism for sending appointment reminders. This was chosen because it was affordable, commercially available and could be modified to use for patient support. Patients indicate their choice to receive messages via text or email. In Phase 1 of the study, the technology and procedures for enrollment and follow-up were tested and modified as needed and in Phase 2, the feasibility of sending messages using this system and the acceptability to participants in the receipt of these messages was evaluated.
Sample size determination
The effectiveness of the electronic messaging intervention will be evaluated by examining changes in the Edinburgh Postnatal Depression Scale (EPDS) in the three groups. We want to detect if Intervention I or II improve the score compared with the control group. Clinical use of scores on the EPDS suggest three categories. EPDS scores <10 appear to indicate a low risk for depression, scores 10-12 suggest further evaluation and scores of 13 or higher indicate a high probability of major depression (Davies, Howells, & Jenkins, 2003; Matthey, Henshaw, Elliott, & Barnett, 2006). This level of minimal detectable difference between groups is sufficient to identify whether the intervention reduces the risk of postpartum depression with the difference between the three clinically significant categories equal to 2 points on the EPDS (effect size=0.44). A power calculation suggests that for an N= 44 in each group the power of detecting the difference of at least one category on the EPDS score is 80% with the type I error 5% under the assumption that the standard deviation of EPDS scores is 4.5 based on previous studies. As follows from our previous studies, about 30% of participants are not responders or are lost to follow up. Therefore, we aim to have at least 63 participants in each group to reach statistical significance.
Setting, inclusion and randomization
Participants were recruited from the postpartum unit of an urban hospital in the state of New Hampshire, USA, at which approximately 1000 women give birth each year. Participants were eligible if they were at least 18 years old and could read and speak English and had access to an electronic device which can receive either text or email messages. Women with healthy newborns as well as those with newborns who have been evaluated by or admitted to a Level II Special Care Nursery were eligible, as women with high-risk newborns or multiples appear to be at increased risk of postpartum depression (Hawes, McGowan, O’Donnell, Tucker, & Vohr; Wenze, Battle, & Tezanos, 2015).
The research protocol was reviewed by the Institutional Review Board of the hospital from which the participants were recruited and was approved initially on 12 May 2015 and reviewed annually. Recruitment for the RCT (Phase 3) occurred from May 2016 - August 2017. All potential participants were approached on the day prior to discharge by a member of the research team and offered participation in the study. If interested, informed consent was obtained in writing and the initial study surveys were administered using a tablet computer. The initial study surveys were administered using the off-line option of the Qualtrics survey platform. The survey took approximately 10 minutes to complete, after which the tablet was retrieved and sanitized. Once the tablet is connected to a secure server, the survey results are uploaded. Participants are given a refrigerator magnet with contact information for the study and their participant ID. Once initial surveys are completed and uploaded, the Qualtrics survey software uses the simple randomization feature to allocate participants equally to one of the three groups. Follow-up surveys are sent by email via Qualtrics at three weeks, three months and six months postpartum. The approximate time required to complete the on-line follow-up surveys is 15 minutes.
Participant incentives
To encourage study retention, participants receive a small gift (a towel with the study logo) at enrollment, valued at approximately $5 US. For each of the three follow-up assessments, they receive a $10 US Amazon gift card via email after the survey is completed online.
Instruments
Demographic data and risk factors
At the time of initial data collection in the hospital, participants provide demographic data, delivery and infant feeding data and contact information, devices they have available for electronic messaging and what their preferred mode of communication is. Low-income women are identified by self-report of their eligibility for the Special Supplemental Program for Women and Children (WIC) (U.S. Department of Agriculture Food and Nutrition Service, 2014) which is based on income and family size and on source of payment for health care. Women are asked whether they have previously experienced, either during or before the pregnancy, symptoms of depression and/or anxiety and if they are currently receiving treatment.
Edinburgh Postnatal Depression Scale
At each of the four data collection points, the Edinburgh Postnatal Depression Scale (EPDS) is administered as the primary outcome measure. The EPDS (Cox, Holden, & Sagovsky, 1987) is a widely-used, well-validated screening instrument to measure symptoms of postpartum depression with demonstrated excellent psychometrics (Hanusa, Scholle, Haskett, Spadaro, & Wisner, 2008) in various samples in the United States as well as many other countries. It consists of 10 items in Likert format, with total scores ranging from 0-30. It is written at a third grade reading level (Logsdon & Hutti, 2006) and has been used extensively among various cultures and in different countries (Schumacher & Zubaran, 2008) with good specificity and sensitivity. As there are many cultural dimensions to the experience of depression, this instrument should be validated in the population under study (Di Florio et al., 2017).
The EPDS is not intended to be diagnostic, but a score of 13 or above has been demonstrated to indicate a high probability for major depressive disorder (Matthey et al., 2006) and scores between 10 and 12 may indicate that a woman is experiencing minor depression (Cox et al., 1987) and further assessment and follow-up may be necessary. As it is not a diagnostic instrument, it can only be used as a measure of symptomatology.
While the administration of the EPDS is intended to be an outcome measure, the follow-up surveys ensure that each participant is screened for postpartum depression three times during the first six months postpartum. The protocol (see ethical considerations below) ensures that women whose scores indicate a high likelihood of major depression are evaluated for safety and referred for treatment when indicated.
Parenting Stress Index-Short Form
The Parenting Stress Index Short Form (PSI-SF) is a widely-used, validated instrument to measure stresses related to child characteristics, parental characteristics and situational and demographic factors (American Psychological Association (APA), 2015). It is written at a fifth grade reading level and includes 36 items, divided into three domains: Parental Distress, Parent-Child Dysfunctional Interaction and Difficult Child (Abidin, 2012). A Total Stress score is also calculated. It has been used in a variety of populations for both screening and diagnosis of stress in the parent-child system. The PSI has been evaluated for United States and transcultural research (Abidin, 2012) and has been used with parents of children ranging from 1 month to 1 year of age. Test-retest reliability was established up to one year with reliability coefficients ranging from .65 to .88 for the Total Stress Score, indicating it is a reliable for use at the 3-weeks, 3-month and 6-month data collection points. The PSI has been found to be correlated with maternal anxiety, bonding and attachment and risk for child abuse (Abidin, 2012). The PSI-SF has been used as an outcome measure for parenting intervention studies (Abidin, 2012) and will be evaluated in this study for utility as an outcome measure of the intervention.
Update on mother and baby
At each of the follow-up surveys, participants are asked to describe any health changes for mother and baby, including whether they have been treated for depression and/or anxiety. Mothers report any life changes such as outside employment or a change in partner status, as well as their infant feeding pattern.
Patient satisfaction/acceptability
Patient satisfaction with the follow-up care is measured by an investigator-developed instrument designed in collaboration with the Patient Satisfaction Committee of the maternity unit at the study site. The satisfaction survey addresses how well expectations are met, including the timeliness of a requested response as well as the quality of communication and the knowledge of the nurse (Senti & LeMire, 2011)., with modifications based on the treatment allocation. For all groups, participants respond to questions about the acceptability and appropriateness of the timing and method of screening/follow-up. The intervention groups respond to questions about the frequency and content of the messages and the Intervention II group is also queried about the amount of time until a nurse phone call was received if requested and about their perception of the communication with the nurse, particularly knowledge, caring and the ability to facilitate follow-up care as needed. Intervention l and II participants are invited to address how they experienced the messages, whether they shared them with others and whether they would choose to receive them again with another child.
Nurse-centered outcomes
Data is being collected on the frequency of requests for phone calls, the content of these calls and the length of time spent on the phone with participants. Any interventions required for the safety of participants is documented, such as scores >13 on the EPDS or any indication of thoughts of self-harm. The number of referrals to follow-up care is also documented.
Analytic procedures
All survey responses will be downloaded from the Qualtrics online survey platform by the PI into an Excel file and de-identified prior to analysis by the statistician. Demographic characteristics of the sample, risk factors for depression, infant feeding data and access to electronic devices will be analyzed using descriptive statistics combined with the data visualization techniques such as box plots and quantile-quantile (q-q) plots. Any statistically significant differences in demographic information between the groups will be assessed by statistical hypothesis testing such as t-test or two-way ANOVA. The primary outcome measure is change in EPDS scores over the six-month follow-up period. Methods of univariate and multivariate statistical analysis will be applied to detect the relationship of other factors, such as socio-economic factors, partner status, history of depression/anxiety, breastfeeding patterns and employment, with the dynamic of the EPDS score over time. Analysis of the differences in EPDS between the three groups will be conducted using t-test with preliminary assessment of the normal distribution using q-q plots. The public-domain statistical package R will be used to analyze the EPDS data. Additionally, groups will be analyzed for differences in the Total Stress Scores of the PSI-SF, using methods outlined above. The relationship between the EPDS and the PSI will be addressed by correlation analysis. Other factors known to be associated with depression such as socioeconomic status, partner status, history of depression/anxiety, breastfeeding patterns and employment will be controlled for in the analysis as well. Data from women who requested a nurse phone call will be analyzed to determine if there are factors which might predict the need for follow-up care.
Groups will be compared based on their experience of and satisfaction with each of the interventions and the amount of nursing time and expertise to respond to requests will be determined. These results will to help inform future clinical practice.
ETHICAL CONSIDERATIONS
The protocol was approved by the hospital on 12 May 2015 and approved annually without substantial revisions. Participants are informed during the consent process that study results will be reported in the aggregate without any identifying information. Consideration will be given for making de-identified data available to other researchers if there appears to be scientific merit in doing so. Because this study involves minimal risk, a Data Safety Monitoring Board was not indicated nor recommended by the IRB.
EPDS follow-up
During the consent process, the participant is informed that should the researcher determine that she may be at immediate risk of harming herself or her baby, we may inform their care provider (whose name and number they provide at enrollment) or refer them to an emergency room. At each of the three follow-up points, if a participant scores ≥ 13 on the EPDS, indicating a high risk for depression (Matthey et al., 2006), or has a positive response to question 10 (thoughts of self-harm), an alert is sent automatically via a Qualtrics email trigger to the principal investigator (PI). The participant is then contacted and evaluated for safety and referred as necessary.
Response time
Participants are also instructed during consent that they should not use the study intervention tools for urgent requests for a nurse, to be certain there are no delays in receiving urgent or emergency care. When a participant in the Intervention II group responds with a request for a nurse phone call, an automated response is generated, informing them that a nurse will call within the week and to seek emergency care or contact their care provider if their request is urgent. A daily morning report from Televox technology is generated and emailed to the PI when a “yes” response to the message indicates a request for a nurse call, but the timing of this report is influenced by the time the participant chooses to respond to the text, allowing for the potential delays of up to 24 hours before the request is known. Despite this variable, nurse response times will be examined.
Validity and reliability
The validity and reliability of the instruments is described above (see Instruments). Any differences in baseline characteristics between groups will be accounted for in the statistical analysis.
DISCUSSION
Preliminary results
Phase 1 & 2
Phase 1 enrolled 75 women and 55 women enrolled in Phase 2. In Phase 3, 547 women were enrolled and randomized to one of the three groups (Figure 1). Phase 1 results were used to make needed modifications in the technology and protocol prior to Phases 2 and 3.
Figure 1.
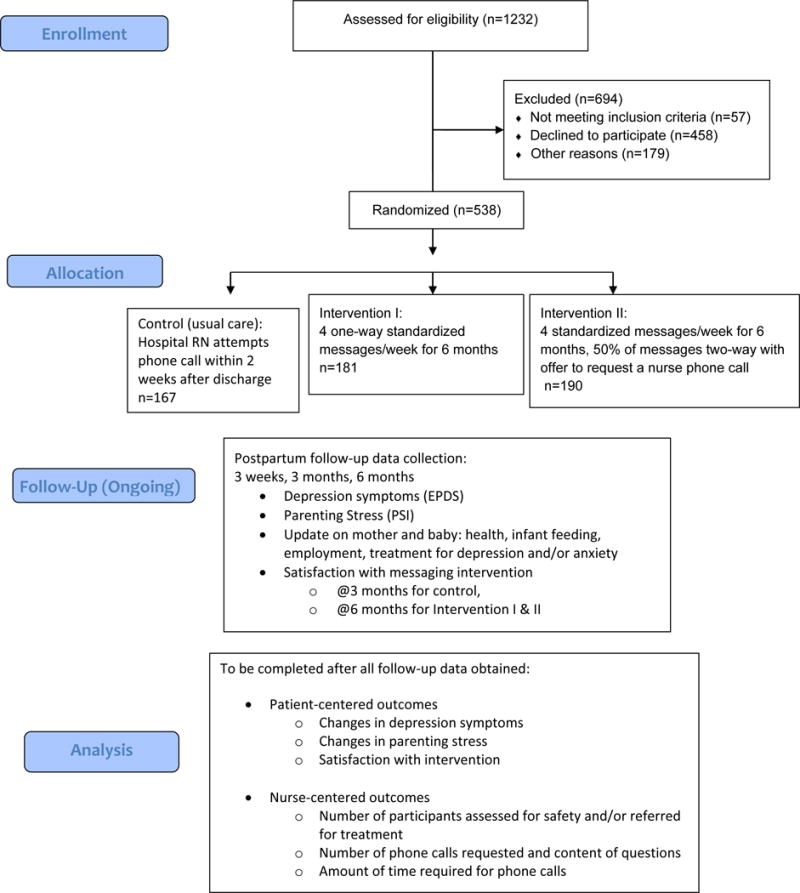
Phase 3: Trial Design
Most participants in Phase 2 (acceptability trial) preferred email (67%) to text for receiving electronic messages. Results of follow-up surveys demonstrated that the majority participants found the intervention to be positive (see Table 1) and that the number of messages was “just right” (83%), with only one person finding the messages to be too frequent. Only 3 participants reported requesting a call back from a nurse (5% of sample). Of these requests, 2 were from the same participant, for a total of 20 minutes of nursing time for the phone calls. It was interesting to note that this participant reported that she wouldn’t have called a nurse on her own, but since it was offered, she made the request. Her concerns were related to normal breastfeeding behaviors. The other person requesting a call stated that she made the request in error.
Table 1.
Phase 2 Satisfaction Data (n=36)
| Question | Disagree/strongly disagree | Neither agree nor disagree | Agree/Strongly agree |
|---|---|---|---|
| The text messages were what I expected | 1 (2.8%) | 14 (38.8%) | 21 (58.3%) |
| I enjoyed receiving text messages/emails from the postpartum nurses | 1 (2.8%) | 10 (27.8%) | 25 (69.4%) |
| It was easy to receive and read the messages | 1 (2.8%) | 4 (11.1%) | 31 (86.1%) |
| The messages were relevant to me personally | 2 (5.6%) | 15 (41.7%) | 19 (52.7%) |
| The messages had a positive influence on my mood | 1 (2.8%) | 12 (33.3%) | 23 (63.9%) |
| I learned something helpful from the messages | 3 (7.9%) | 15 (33.3%) | 18(50%) |
| I liked the option of having a nurse call me back | 0 | 10 (27.8%) | 26 (72.2%) |
| I looked forward to receiving the messages from the postpartum nurses | 2 (5.6%) | 16 (44.4%) | 18 (50%) |
| I used the messages to help me as a mother | 5 (13.9%) | 18 (50%) | 13 (36.1%) |
| I used the messages to help me grow as a person | 7 (19.4%) | 17 (47.2%) | 12 (33.3%) |
| The messages made me feel more connected with [birth hospital] | 2 (5.6%) | 13 (36.1%) | 21 (58.3%) |
| The messages helped me to get to a mother’s group | 16 (44.4%) | 19 (52.8%) | 1 (2.8%) |
| I would recommend the text messages/emails to other new mothers | 2 (5.6%) | 11 (30.5%) | 23 (63.9%) |
| I would sign up for messages again when/if I have another baby at [birth hospital] | 2 (5.6%) | 10 (27.8%) | 24 (66.7%) |
Six phone calls were initiated (11%) due to high scores on the EPDS, as per the safety protocol. Two participants had high scores on two occasions and it was determined that they were in treatment. Two were contacted on only one occasion and referred for treatment after immediate safety was established. These contacts, both phone and email, altogether required a total of 20-30 minutes of nursing time.
Phase 3
Baseline demographic information (Table 2) obtained at enrollment demonstrated that the groups were not significantly different in age, parity, infant health, partner status, education or intended infant feeding plan. The Intervention II group (receiving both text and option for nurse contact) had significantly more women of color (18%) than either the control group (10%) or Intervention I (12%). There were no significant differences in prior history of depression, or history of anxiety and/or depression during the current pregnancy. However, the Intervention II group had a fewer women with clinically significant symptoms of depression at baseline (EPDS<10).
Table 2.
Phase 3 Baseline Patient Characteristics1. (All results noted as Frequency (Percent) unless otherwise noted.)
| Sample Characteristics | All n=538 |
Usual Care n=167 |
Intervention I (text only) n=181 |
Intervention II (text & RN) n=190 |
|---|---|---|---|---|
|
| ||||
| Mean age (SD) | 29.3 (5.3) | 29.3 (5.4) | 28.9 (4.9) | 29.8 (5.4) |
|
| ||||
| Parity: | ||||
| Primipara | 237 (44) | 71 (43) | 81 (45) | 85 (45) |
| Multipara | 301 (56) | 96 (57) | 100 (55) | 105 (55) |
|
| ||||
| * Race: | ||||
| White Women | 465 (86) | 151 (90) | 159 (88) | 155 (82) |
| Women of Color | 73 (14) | 16 (10) | 22 (12) | 35 (18) |
|
| ||||
| Hispanic/Latina: | 38 (7) | 11 (7) | 9 (5) | 18 (9) |
|
| ||||
| Birth: | ||||
| Vaginal | 423 (79) | 133 (80) | 140 (78) | 150 (79) |
| Cesarean | 114 (21) | 34 (20) | 40 (22) | 40 (21) |
|
| ||||
| Infant status: | ||||
| Level 1 nursery | 496 (92) | 150 (90) | 169 (93) | 177 (94) |
| Level 2 or higher | 41 (8) | 17 (10) | 12 (7) | 12 (6) |
|
| ||||
| Education: | ||||
| High school or less | 117 (22) | 34 (20) | 40 (22) | 46 (24) |
| Some college | 188 (35) | 60 (36) | 71 (39) | 57 (30) |
| College degree or higher | 232 (43) | 73 (44) | 70 (39) | 89 (47) |
|
| ||||
| Partner status: | ||||
| Married or cohabitating | 490 (91) | 153 (92) | 164 (91) | 173 (91) |
| In significant relationship | 23 (4) | 8 (5) | 6 (3) | 9 (5) |
| Single | 24 (4) | 6 (4) | 11 (6) | 7 (4) |
|
| ||||
| Intended infant feeding plan2 | ||||
| Breastfeeding only | 392 (73) | 123 (74) | 135 (75) | 134 (71) |
| Formula feeding | 57 (11) | 16 (10) | 23 (13) | 18 (10) |
| Combination breast & formula | 88 (16) | 28 (17) | 23 (13) | 37 (20) |
|
| ||||
| Eligible for WIC benefits | 203 (38) | 64 (39) | 72 (40) | 67 (36) |
|
| ||||
| Depression during this pregnancy2 | 76 (14) | 23 (14) | 30 (17) | 23 (12) |
|
| ||||
| Anxiety during this pregnancy2 | 181 (34) | 62 (37) | 65 (36) | 54 (29) |
|
| ||||
| Depression prior to this pregnancy2 | 198 (37) | 64 (38) | 68 (38) | 66 (35) |
|
| ||||
| * Baseline EPDS (mean, SD) | 4.0 (4.2) | 4.3 (4.5) | 4.5 (4.4) | 3.2 (3.6) |
|
| ||||
| EPDS score <10 (no depression) | 479 (89) | 146 (87) | 154 (85) | 179 (94) |
| EPDS score 10-12 (risk for depression) | 31 (6) | 10 (6) | 14 (8) | 7 (4) |
| EPDS score >12 (high risk for depression) | 28 (5) | 11 (7) | 13 (7) | 4 (2) |
significant difference between groups p<.05
Percentages may sum to greater than 100 based on rounding figures
Based on self-report
To date, there have been 37 participant responses requesting a nurse call from the Intervention II group. Each of these calls has lasted from 2-15 minutes. However, in the total sample (N=538), 60 calls have been initiated based on EPDS scores ≥12. Each of these calls have required from 5-30 minutes of nursing time to assess for safety and refer as necessary.
Lessons learned from Phase 1 and 2
Testing of the technology in phase 1 uncovered several challenges, leading to modification of the protocol prior to the RCT (Phase 3). In Phase 1, the electronic messages were used to facilitate the timing of the routine nurse follow-up phone call (the usual care), by sending a message to enrolled participants asking them if they would be available for the phone call the following day. The intent was to establish the control condition for the randomized controlled trial, using the technology to increase the number of patients reached by phone by assuring that women would be available for the call as if they had made an appointment. However, this intervention had no effect on the number of calls completed. Additionally, confirming a day for the call became a challenge as the nurses making calls also have other clinical responsibilities, so that they could not always complete the intended call on the scheduled day, further limiting the utility of the electronic message.
Another challenge with the technology is the timing of receiving reports of when the patient responded “yes” to the message. If they responded immediately after receiving the text, the nurse received the notification of the response the following morning. If they responded after the daily report was generated, the nurse was not notified until the following day, now past the date offered to the patient. It was determined that managing the timing of the nurse phone calls was labor-intensive and not productive. Thus, the planned control condition for the RCT was modified to simply be the usual care. Since the revised control condition no longer included any electronic messaging, the protocol for Phase 3 was modified to have three groups—the usual care group (unscheduled phone call only) and two intervention groups— one that involves only one-way electronic messaging (Intervention I) and one which includes two-way electronic messages to allow for a response requesting nurse contact (Intervention II). The design with two intervention groups is intended to better distinguish the effects of the technology alone from the web-enhanced nursing intervention.
LIMITATIONS
The study is limited to a population of mothers from one hospital in the Northeast United States (i.e., predominantly white and well educated) and thus results cannot be readily generalized to other more diverse populations. In addition, while all eligible women are offered participation, women who have experienced anxiety and depression previously may be more motivated to participate than women who do not expect to be affected. General reasons for declining participation are documented when available, but self-selection cannot be ruled out. Thus, this may be a more psychologically vulnerable sample than would be found in the general population of new mothers. During the six months of follow-up, there is expected to be some attrition from the study which will limit the data available for analysis. All reasons for attrition will not be known. During informed consent, participants learn that if they choose to opt out, they may receive one final survey to inquire as to the reason for this, but to date, no participants choosing to opt out have responded to this survey. Recruitment is planned in anticipation of 60% retention rate, based on previous research with this study population, to ensure there is adequate data to retain statistical power.
The study employs technology designed for another use (appointment reminders) and while economical, is limited in functionality and difficult to modify. If it is determined that the intervention improves maternal mood and decreases parenting stress, it is likely that a more facile technology would be needed for use in clinical practice.
CONCLUSION
Preliminary results
Results analyzed to date have determined that receiving digital messages from nurses at the maternity hospital is acceptable to patients and does not represent a significant burden on nursing time to respond to requests for a return call. In addition, anecdotal evidence from unsolicited patient contact suggests that respondents feel comforted and secure knowing that they have the option to ask for a nurse, even when they did not choose to do so.
Follow-up until six months postpartum was completed in February 2018 and analysis of primary outcomes scheduled. The number of calls initiated based on EPDS scores suggests that there may be benefit to a nursing intervention which screens for depression for at least six months after hospital discharge.
Contribution to nursing knowledge
This study is motivated by assessment of unmet needs of postpartum women and the negative health impact for mothers, fathers and children if such neglect is not addressed. Beyond this however, it is motivated by the need to generate evidence for nurses’ assumed role and expertise in health education, anticipatory guidance, support and triage. While health promotion and disease prevention are recognized competencies of nursing (American Nurses Association, 2015), the outcomes of such nursing interventions are not frequently measured or reported. In addition, there is a growing number of technologies designed for pregnancy and parenting (Wellde & Miller, 2016), but it is not known if technology use improves outcomes. This study seeks to determine if technology can facilitate nursing care and support after discharge from the maternity hospitalization in a manner that will improve patient outcomes. Knowledge gained from this study will help inform nursing interventions that use or recommend digital technologies to improve health. Such interventions could be customized and adapted to meet the needs of many communities of women world-wide. For this reason, results will be disseminated by the authors in research and clinical forums such as nursing journals and professional conferences.
Why this study is needed (summary statement).
Postpartum women are at high risk for depression and may not receive needed care and support
Electronic interventions for outreach and continuity of care exist but outcomes are seldom measured.
Maternal-child nursing care facilitated by technology may be able to support vulnerable women during the first six months postpartum, decreasing negative outcomes.
Acknowledgments
FUNDING
Research supported by New Hampshire-INBRE through an Institutional Development Award (IDeA), P20GM103506, from the National Institute of General Medical Sciences of the NIH. Contact: http://nhinbre.org/
Footnotes
DR DEBORAH ELAINE MCCARTER (Orcid ID: 0000-0002-7947-481X)
No CONFLICT OF INTEREST has been declared by the authors.
Trial registration number: ClinicalTrials.gov NCT 02843022
Author Contributions:
All authors have agreed on the final version and meet at least one of the following criteria (recommended by the ICMJE*):
1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
2) drafting the article or revising it critically for important intellectual content.
Contributor Information
Deborah E. MCCARTER, Professor of Nursing, Saint Anselm College, Manchester, NH; Staff Nurse, Catholic Medical Center, Manchester, NH.
Eugene DEMIDENKO, Professor of Biomedical Data Science, Geisel School of Medicine at Dartmouth, Hanover, NH.
Mark T. HEGEL, Professor in Psychiatry, Geisel School of Medicine at Dartmouth, Hanover, NH.
References
- Abdollahi F, Lye MS, Md Zain A, Shariff Ghazali S, Zarghami M. Postnatal depression and its associated factors in women from different cultures. Iranian Journal of Psychiatry and Behavioral Sciences. 2011;5(2):5–11. [PMC free article] [PubMed] [Google Scholar]
- Abidin RR. Parenting Stress Index. 4th. Lutz, Florida: PAR; 2012. [Google Scholar]
- Aguilera A, Berridge C. Qualitative feedback from a text messaging intervention for depression: Drawbacks and cultural differences. JMIR mHealth and uHealth. 2014;2(4) doi: 10.2196/mhealth.3660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists (ACOG) Optimizing postpartum care: Committee opinion no. 666. Obstetrics and Gynecology. 2016;127(6):e187–192. doi: 10.1097/AOG.0000000000001481. [DOI] [PubMed] [Google Scholar]
- American Nurses Association. Nursing Scope and Standards of Practice. 3rd 2015. [Google Scholar]
- American Psychological Association (APA) Parenting Stress Index. 2015 Retrieved from http://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/parenting-stress.aspx.
- Association for Women’s Health, Obstetric and Neonatal Nursing [AWHONN]. Mood and anxiety disorders in pregnant and postpartum women. Journal of Obstetric, Gynecologic and Neonatal Nursing. 2015;44(5):687–689. doi: 10.1111/1552-6909.12734. https://doi.org/10.1111/1552-6909.12734 [DOI] [PubMed] [Google Scholar]
- Brealey SD, Hewitt C, Green JM, Morrell J, Gilbody S. Screening for postnatal depression – is it acceptable to women and healthcare professionals? A systematic review and meta-synthesis. Journal of Reproductive & Infant Psychology. 2010;28(4):328–344. doi: 10.1080/02646838.2010.513045. [DOI] [Google Scholar]
- Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113(6):e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Danaher BG, Milgrom J, Seeley JR, Stuart S, Schembri C, Tyler MS, Lewinsohn P. Web-based intervention for postpartum depression: Formative research and design of the MomMoodBooster program. JMIR Journal of Medical Internet Reserach. 2012;1(2):e18. doi: 10.2196/resprot.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danbjørg DB, Wagner L, Clemensen J. Do families after early postnatal discharge need new ways to communicate with the hospital? A feasibilility study. Midwifery. 2014;30(6):725–732. doi: 10.1016/j.midw.2013.06.006. https://doi.org/10.1016/j.midw.2013.06.006 [DOI] [PubMed] [Google Scholar]
- Davies BR, Howells S, Jenkins M. Early detection and treatment of postnatal depression in primary care. Journal Of Advanced Nursing. 2003;44(3):248–255. doi: 10.1046/j.1365-2648.2003.02799.x. [DOI] [PubMed] [Google Scholar]
- Di Florio A, Putnam K, Altemus M, Apter G, Bergink V, Bilszta J, Penninx BW. The impact of education, country, race and ethnicity on the self-report of postpartum depression using the Edinburgh Postnatal Depression Scale. Psychological Medicine. 2017;47(5):787–799. doi: 10.1017/S0033291716002087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake E, Howard E, Kinsey E. Online screening and referral for postpartum depression. Community Mental Health. 2014;50:305–311. doi: 10.1007/s10597-012-9573-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earls MF, The Committee on Psychosocial Aspects of Child and Family Health Clinical report–Incorporating recognition and management of perinatal and postpartum depression Into pediatric practice. Pediatrics. 2010;126(5):1032–1039. doi: 10.1542/peds.2010-2348. [DOI] [PubMed] [Google Scholar]
- Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization. 2012;90(2):139G–149G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra-Reyes L, Christie VM, Prabhakar A, Siek KA. Mind the gap: Assessing the disconnect between postpartum health information desired and health information received. Women’s Health Issues. 2017;27(2):167–173. doi: 10.1016/j.whi.2016.11.004. [DOI] [PubMed] [Google Scholar]
- Hanusa BH, Scholle SH, Haskett RF, Spadaro K, Wisner KL. Screening for depression in the postpartum period: A comparison of three instruments. Journal of Women’s Health. 2008;17(4):585–596. doi: 10.1089/jwh.2006.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes K, McGowan E, O’Donnell M, Tucker R, Vohr B. Social emotional factors increase risk of postpartum depression in mothers of preterm infants. The Journal of Pediatrics. 179:61–67. doi: 10.1016/j.jpeds.2016.07.008. [DOI] [PubMed] [Google Scholar]
- Heneghan AM, Mercer M, DeLeone NL. Will mothers discuss parenting stress and depressive symptoms with their child’s pediatrician? Pediatrics. 2004;113(3):460–467. doi: 10.1542/peds.113.3.460. [DOI] [PubMed] [Google Scholar]
- Hutto HF, Kim-Godwin Y, Pollard D, Kemppainen J. Postpartum depression among White, African American and Hispanic low-income mothers in rural southeastern North Carolina. Journal of Community Health Nursing. 2011;28(1):41–53. doi: 10.1080/07370016.2011.539088. [DOI] [PubMed] [Google Scholar]
- Kanotra S, D’Angelo D, Phares TM, Morrow B, Barfield WD, Lansky A. Challenges faced by new mothers in the early postpartum period: An analysis of comment data from the 2000 Pregnancy Risk Assessment Monitoring System (PRAMS) survey. Maternal & Child Health Journal. 2007;11(6):549–558. doi: 10.1007/s10995-007-0206-3. [DOI] [PubMed] [Google Scholar]
- Kim JJ, La Porte LM, Adams MG, Gordon TEJ, Kuendig JM, Silver RK. Obstetric care provider engagement in a perinatal depression screening program. Archives Of Women’s Mental Health. 2009;12(3):167–172. doi: 10.1007/s00737-009-0057-6. [DOI] [PubMed] [Google Scholar]
- Le H, Perry DF, Sheng X. Using the internet to screen for postpartum depression. Maternal & Child Health Journal. 2009;13(2):213–221. doi: 10.1007/s10995-008-0322-8. [DOI] [PubMed] [Google Scholar]
- Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Archives Of Women’s Mental Health. 2005;8(2):77–87. doi: 10.1007/s00737-005-0080-1. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Hutti MH. Readability: an important issue impacting healthcare for women with postpartum depression. MCN: The American Journal of Maternal Child Nursing. 2006;31(6):350–355. doi: 10.1097/00005721-200611000-00004. [DOI] [PubMed] [Google Scholar]
- Martin A, Horowitz C, Balbierz A, Howell E. Views of women and clinicians on postpartum preparation and recovery. Maternal & Child Health Journal. 2014;18(3):707–713. doi: 10.1007/s10995-013-1297-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthey S, Henshaw C, Elliott S, Barnett B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale: Implications for clinical and research practice. Archives Of Women’s Mental Health. 2006;9(6):309–315. doi: 10.1007/s00737-006-0152-x. [DOI] [PubMed] [Google Scholar]
- McCarter-Spaulding D, Shea S. Effectiveness of discharge education on postpartum depression. MCN: The American Journal of Maternal Child Nursing. 2016;41(3):168–172. doi: 10.1097/NMC.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLennan JD, Kotelchuck M. Parental prevention practices for young children in the context of maternal depression. Pediatrics. 2000;105(5):1090–1095. doi: 10.1542/peds.105.5.1090. [DOI] [PubMed] [Google Scholar]
- Myers ER, Aubuchon-Endsley N, Bastian LA, Gierisch JM, Kemper AR, Swamy GK, Sanders GD. Comparative effectiveness review 106. Rockville, MD: 2013. Efficacy and safety of screening for postpartum depression. (Prepared by the Duke Evidence-based Practice Center under Contract No 290-2007-10066-I. (13-EHC064-EF)). Retrieved from. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0056006/ [Google Scholar]
- Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. Mobile fact sheet. 2017 Retrieved from http://www.pewinternet.org/fact-sheet/mobile/
- Piette JD, Schillinger D. Applying interactive health technologies for vulnerable populations. In: King TE, Wheeler MB, editors. Medical management of vulnerable and underserved patients: Principles, practice and populations. New York: McGraw-Hill; 2007. [Google Scholar]
- Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, Waheed W. Interventions for common perinatal mental disorders in women in low- and middle-income countries: a systematic review and meta-analysis. Bulletin of the World Health Organization. 2013;91(8):593–601I. doi: 10.2471/BLT.12.109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher M, Zubaran C. Screening tools for postpartum depression: validity and cultural dimensions. International Journal of Psychiatric Nursing Research. 2008;14(1):1752–1765. [Google Scholar]
- Segre LS, O’Hara MW, Arndt S, Beck CT. Screening and counseling for postpartum depression by nurses: the women’s views. MCN: The American Journal of Maternal Child Nursing. 2010;35(5):280–285. doi: 10.1097/NMC.0b013e3181e62679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senti J, LeMire S. Patient satisfaction with birthing center nursing care and factors associated with likelihood to recommend institution. Journal of Nursing Care Quality. 2011;26(2):178–185. doi: 10.1097/NCQ.0b013e3181fe93e6. [DOI] [PubMed] [Google Scholar]
- Smith MV, Shao L, Howell H, Wang H, Poschman K, Yonkers K. Success of mental health referral among pregnant and postpartum women with psychiatric distress. General Hospital Psychiatry. 2009;31:155–162. doi: 10.1016/j.genhosppsych.2008.10.002. http://dx.doi.org/10.1016%2Fj.genhosppsych.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Pariante CM. Effects of perinatal mental disorders on the fetus and child. Lancet (London, England) 2014;384(9956):1800–1819. doi: 10.1016/S0140-6736(14)61277-0. [DOI] [PubMed] [Google Scholar]
- Sword W, Busser D, Ganann R, McMillan T, Swinton M. Women’s care-seeking experiences after referral for postpartum depression. Qualitative Health Research. 2008;18(9):1161–1173. doi: 10.1177/1049732308321736. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture Food and Nutrition Service. Women, Infants and Children. 2014 Retrieved from http://www.fns.usda.gov/wic/women-infants-and-children-wic.
- Wellde PT, Miller LA. There’s an app for that! New directions using social media in patient education and support. Journal of Perinatal and Neonatal Nursing. 2016;30(3):198–203. doi: 10.1097/JPN.0000000000000177. [DOI] [PubMed] [Google Scholar]
- Wenze SJ, Battle CL, Tezanos KM. Raising multiples: Mental health of mothers and fathers in early parenthood. Archives Of Women’s Mental Health. 2015;18(2):163–176. doi: 10.1007/s00737-014-0484-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. WHO recommendations on postnatal care of the mother and newborn 2013. 2014 Retrieved from http://apps.who.int/iris/bitstream/10665/97603/1/9789241506649_eng.pdf. [PubMed]


