Abstract
A Caucasian 92-year-old female was admitted to hospital with acute epigastric pain associated with vomiting. Initial investigations revealed mildly raised inflammatory markers, normal liver function tests but a markedly distended gallbladder with prominent wall thickening. The patient was managed with intravenous antibiotics for acute cholecystitis but deteriorated significantly on Day 2 of admission. An emergency laparoscopic cholecystectomy was performed and we found a gangrenous gallbladder secondary to gallbladder volvulus. The patient recovered well in the postoperative period and was discharged home 7 days later.
BACKGROUND
Gallbladder volvulus remains a relatively rare diagnosis with only 500 cases reported since the end of the 19th century. There seems to have been an increase in the incidence since the turn of the 21st century, likely due to the condition having a preponderance for older patients and increasing life expectancy around the world [1]. It is reported that a mere 10% of cases are diagnosed preoperatively, thus it is inevitable that there are delays between the onset of the disease process and definitive surgical management. Typically patients are misdiagnosed with acute cholecystitis and there is a delay in proceeding to cholecystectomy. These delays can critically increase the risks of sepsis secondary to gallbladder ischaemia, necrosis and perforation. With prompt diagnosis the mortality is low at 5% [2], highlighting the importance of early surgical intervention.
CASE PRESENTATION
A Caucasian 92-year-old lady attended the emergency department with acute onset epigastric/right hypochondrial pain, waking the patient from sleep. The pain was described as being constant since onset and radiated through to her back. The pain was immediately followed by profuse and intractable vomiting. There had been no previous episodes of similar pain and she had been well in the preceding days. Her past medical history included an open appendicectomy, hypertension, GORD, previous TIA, left carotid endarterectomy, peripheral vascular disease and a L2 crush fracture. The patient denied fevers/rigors and had no recent history of lower urinary tract symptoms or altered bowel habit. The vital signs recorded for the patient were within normal limits and she was afebrile. On examination of the patient’s abdomen it was noted that the abdomen was soft and not distended, with diffuse tenderness down the right side. The gallbladder was also palpable to the right iliac fossa. The white cell count was mildly elevated at 13.2, while there were no electrolyte abnormalities and no renal or liver function derangement evident on blood tests. A CT scan of the abdomen and pelvis (Fig. 1) was arranged with contrast and was reported as showing a ‘distended gallbladder with prominent wall thickening and mild adjacent inflammatory change. The appearances are most consistent with cholecystitis’. An ultrasound was then performed that demonstrated a calculus together with minor gallbladder wall thickening but no evidence of biliary ductal dilatation. Thus, the patient was started on intravenous antibiotic therapy as per local guidelines for a presumed diagnosis of acute cholecystitis and admitted under the care of the general surgeons. The patient was reviewed on rounds the following morning and was noted to have increasing pain despite analgesia associated with tachycardia, tachypnoea and diaphoresis with a peritonitic abdomen. The white cell count was now elevated at 17.6 with a CRP of 198 and the liver function tests remained within normal limits. The patient was reimaged with a further CT abdomen/pelvis with contrast which was reported as showing ‘cholelithiasis and choledocholithiasis with intra and extra bile duct dilatation as well as marked gallbladder distension and pericholecystic fluid’. An emergency laparotomy was performed with findings on entry of a non-viable and gangrenous gallbladder secondary to gallbladder volvulus. The images below show the volvulus as well as the cystic duct and cystic artery after being detorted (Fig. 2). The patient was managed in ICU immediately postoperatively but medically fit for discharge after five nights in hospital.
Figure 1:

CT abdomen with contrast (coronal view).
Figure 2:
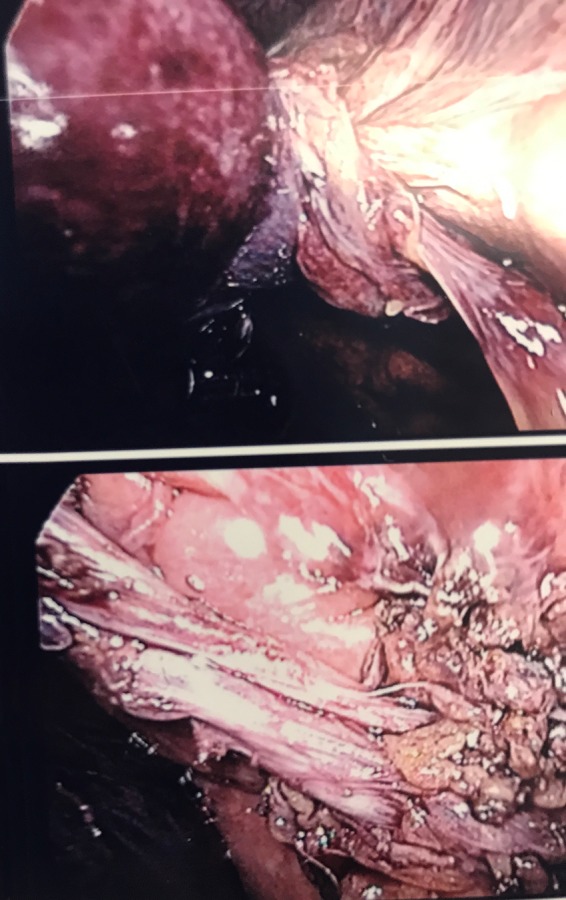
Intraoperative imaging showing gallbladder volvulus and detorsion of the cystic duct and artery.
DISCUSSION
This case splendidly portrays the complexities involved when managing a patient with gallbladder volvulus. Acute cholecystitis was initially suspected and this was supported by radiological findings. Thus medical management for cholecystitis was initiated despite being totally inappropriate in the context of this patient. This resulted in a delay for the patient to proceed to definitive surgical intervention which she ultimately would require. This demonstrates how difficult the diagnosis of gallbladder volvulus is to make preoperatively for both surgeons and radiologists. Lau et al. [3] first described the ‘triad of triads’, involving appearance (elderly, thin, spinal deformities), symptoms (sudden onset, RUQ pain, early emesis) and examination (non-toxic presentation, palpable abdominal mass and pulse–temperature discrepancy). Our patient in this case report satisfied 8 of the 9 features described by Lau, with a normocardia preventing her from fulfilling the ‘triad of triads’ in full. Furthermore, the initial CT scan revealed marked gallbladder distension and wall thickening yet it was not until the patient significantly deteriorated requiring emergency surgical intervention was the diagnosis of gallbladder volvulus made. These delays between presentation and diagnosis can only increase the morbidity and mortality in patients who are commonly elderly. This case is therefore an excellent example of why gallbladder volvulus should be considered as a differential diagnosis in all patients fulfilling the majority of the triad of triads despite equivocal radiological findings.
CONCLUSION
Prompt diagnosis of gallbladder volvulus is undoubtedly challenging yet this case report is an example of how the ‘triad of triads’ can be used to help identify gallbladder volvulus in patients who present like acute cholecystitis. Moreover, there are no radiological signs to diagnose gallbladder volvulus unequivocally thus we must rely on our clinical judgement. We would therefore suggest a low threshold for proceeding to cholecystectomy in patients who satisfy the triad of triads despite radiological evidence that may be non-specific or misleading. This approach may avoid the higher mortality and morbidity associated with gallbladder necrosis, perforation and biliary peritonitis.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Pu TW, Fu CY, Lu HE, Cheng WT. Complete body-neck torsion of the gallbladder: a case report. World J Gastroenterol 2014;20:14068–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nakao A, Matsuda T, Funabiki S, Mori T, Koguchi K, Iwado T, et al. Gallbladder torsion: case report and review of 245 cases reported in the Japanese literature. J Hepatobiliary Pancreat Surg 1999;6:418–21. [DOI] [PubMed] [Google Scholar]
- 3. Lau WY, Fan ST, Wong SH. Acute torsion of the gall bladder in the aged: a re-emphasis on clinical diagnosis. Aust N Z J Surg 1982;52:492–4. [DOI] [PubMed] [Google Scholar]


