Abstract
Background
Retrobulbar block is one of the chosen methods for local anesthesia in cataract surgery. Since it is a painful procedure, using analgesic and sedative drugs is recommended. Current medications have side effects and evaluating of new drugs or new uses of existing safer drugs is necessary.
Objectives
The aim of this study was to compare the administration of melatonin and acetaminophen on pain and hemodynamic changes during retrobulbar block.
Methods
In a double-blinded randomized trial, 180 patients undergoing cataract surgery were randomly divided into three groups: Melatonin group (received melatonin 6 mg), acetaminophen group (received acetaminophen 500 mg), and control group (received placebo). All drugs were administered orally 60 min before arrival to the operating room by nurses blinded to the drugs administered. All patients received fentanyl 0.5 μg/kg before retrobulbar block intravenously. Hemodynamic variables and pain score in each patient were evaluated on arrival in the operating room, during retrobulbar block, during surgery, 20 min after operation, at the end of surgery, and in the recovery room. In case of pain score more than three, additional fentanyl was administered. All data were recorded in structured data sheets.
Results
Data analysis indicated no significant differences among the groups at baseline on any of the demographic variables. Both acetaminophen and melatonin reduced the pain score significantly compared with control during retrobulbar block (P < 0.05 and P < 0.01, respectively). Administration of additional fentanyl was significantly lower in the melatonin group than the control group (P < 0.05). Hemodynamic changes were not significantly different among all groups.
Conclusions
For the first time, as far as we have studied, the analgesic effect of acetaminophen on the retrobulbar block was indicated. We also showed that melatonin can reduce pain during retrobulbar block leading to reduction of additional fentanyl during operation. It seems that both melatonin and acetaminophen may have a beneficial effect on pain control in the retrobulbar block.
Keywords: Pain, Acetaminophen, Cataract, Melatonin
1. Background
Cataract is the turbidity in the lens of the eyes that may impair contrast sensitivity, glare sensitivity, and perception of light (1). Surgery is the only treatment that can affect visual impairment due to cataract (2). The vast majority of patients undergoing cataract surgery are older people with high CAD or IHD risk factors, such as atherosclerosis, high blood pressure, and diabetes mellitus (3). They face more ischemic events, hemodynamic instability, and changes in heart rate and plasma glucose during general anesthesia. Local anesthesia seems to have many advantages over general anesthesia and cause better analgesia after surgery (4). Among the local anesthesia techniques, retrobulbar, and topical block are more preferred among anesthesiologists and eye surgeons due to the fact that they are safer, more affordable, and less expensive (5).
The retrobulbar block is a painful process and use of analgesic and sedative medications may be helpful. These premeditations are administered to keep the patients painless, calm, and immobile (6). Opioids, benzodiazepines, propofol, fentanyl, and dexmedetomidine were frequently used alone or in combination during cataract surgery. Since all of these drugs have unwanted side effects (7), the evaluation of new drugs that are potentially clinically relevant in this regard is necessary.
Melatonin or N-acetyl methoxytryptamine is a neurohormone produced by the pineal gland and the retina (8). The major physiological role of melatonin is the regulation of sleep and awakening rhythm (9). Several studies revealed that the use of melatonin as premedication reduced perioperative anxiety without cognitive impairment such as memory impairment (10). In addition, analgesic, antioxidant, and inflammatory effects of melatonin have been reported. Therefore, with these characteristics as well as being harmless, melatonin is considered as a potential drug to reduce pain and anxiety during cataract surgery (9).
Acetaminophen is a widely-used drug to relieve mild to moderate pain. After years of its use, its efficacy and harmlessness have been proven and is described as a standard analgesic drug (11).
2. Objectives
The purpose of this study was to compare the administration of melatonin and acetaminophen on pain and hemodynamic changes in retrobulbar block, which was performed in patients undergoing cataract surgery.
3. Methods
This double-blind, randomized, clinical trial was approved by the University Ethics Committee (Code of Ethics 1930474206) and registered at the Iranian Registry of Clinical Trials (IRCT2015012315963N4). The study was conducted from Mar 2014 to Nov 2014 in Amir Al-Momenin Hospital of Rasht, Iran. The protocols of this study were performed in accordance with ethical guidelines of the 1975 Helsinki Declaration. After obtaining the informed consent, a total of 180 patients of both genders scheduled for cataract surgery (aged 50 to 90) with The American Society of Anesthesiologists (ASA) I-III were included. The exclusion criteria included: coagulation disorders, using anticoagulant drugs, cognitive impairment, Alzheimer's disease, history of allergy to local anesthetic drugs, claustrophobia, spontaneous chronic cough, addiction, and chronic analgesics. In addition, individuals were excluded from the analysis if they had extended surgical time, block failure, and trigeminocardiac reflex. Patients were randomized by random allocation method divided into three groups, each containing 60 patients. Group M received 6 mg melatonin tablets (made by nature-made United States), group A received acetaminophen 500 mg (manufactured by the Arya Pharmaceuticals Co, Iran) and the control group (C) received placebo. All drugs were given orally with 10 mL of water 60 minutes before entering the operating room. The medications were taken by the nurse blinded to the type of drug used. In the operating room and under standard monitoring, all patients were given fentanyl 0.5 μg/kg and midazolam 0.03 mg/kg intravenously (12).
3.1. Retrobulbar Block
A 3 cm length 23-gauge retrobulbar needle inserted through the lower eyelid at the junction between lateral and inferior orbital edge. The needle is advanced posteriorly until it was felt to be within the muscle cone. At this point; 2 to 3 mL of anesthetic mixture solution (lidocaine 2% and hyaluronidase) was slowly injected. Cardiac and respiratory systems were monitored and supplemental oxygen was given via nasal cannula at 5 L/min.
Hemodynamic changes including heart rate (HR), oxygen saturation (O2 Sat), systolic blood pressure (SBP), and diastolic blood pressure (DBP) were noted and the mean arterial pressure (MAP) was calculated. Score of pain at the entrance to the operating room (T1), during retrobulbar block (1 minute after block) (T2), during surgery (5 minutes after the start of operation) (T3), 20 minutes after the start of operation (T4), at the end of surgery (T5), and in the recovery room (T6) were also recorded. The pain score was evaluated by a numerical rating scale (NRS), in which the patient selects a number from zero to 10, which is a reflection of the severity of the pain. In addition, pain was classified as no pain (0), mild (1 - 2), moderate (3 - 4), severe (5 - 6), very severe (7 - 8), and extremely severe (9 - 10). Before surgery, all patients were instructed to describe pain on NRS. Complications during the block, surgery, and recovery including nausea, vomiting, and reduction of oxygen saturation were reported. The nausea, vomiting, and reduction of oxygen saturation were treated by administration of ondansetron (0.08 mg/kg IV) and oxygen via face mask, respectively.
Additional fentanyl would be administered if pain score was more than three during the surgery.
3.2. Statistical Analysis
Kolmogorov-Smirnov test was used to evaluate the normality of the data. One way ANOVA or Kruskal-Wallis test was used to compare the pain score and hemodynamic changes. Tukey's post Hoc test was used to compare the two groups. To compare qualitative variables, the χ2 and Fisher's exact test were used. P < 0.05 was considered as significant difference.
4. Results
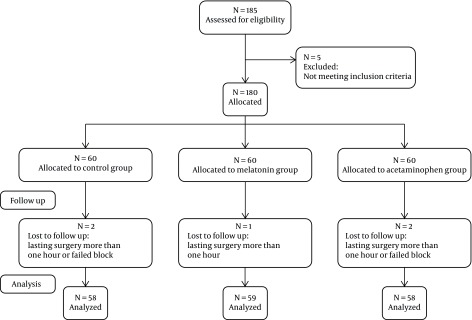
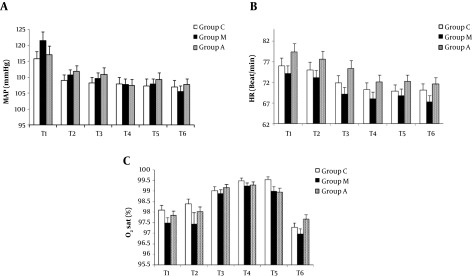
Out of 180 patients, 5 were excluded due to the fact that the surgery lasted for more than one hour or failing block (Figure 1). Demographic features including sex and ASA were not statistically different among all three groups (Table 1). In the case of age, Turkey's post Hoc analysis demonstrated no significant differences among each two groups. MAP, HR, and O2 Sat did not show significant differences before surgery, during retrobulbar block, as well as during and after surgery in the control group with melatonin and acetaminophen groups (Figure 2).
Figure 1. CONSORT flow diagram of this study.
Table 1. Demographic Features Including Age, Sex and ASA.
| Variable | Group C | Group M | Group A | P Value |
|---|---|---|---|---|
| N | 58 | 59 | 58 | |
| Age, y | 68.3 ± 1.6 | 63.59 ± 1.38 | 67.9 ± 1.3 | 0.035 |
| Female/Male | 29/29 | 33/26 | 31/27 | 0.222 |
| ASA (I/II/III) | 3/37/18 | 10/35/14 | 4/36/18 | 0.812 |
Abbreviations: A, acetaminophen; C, control; M, melatonin.
Figure 2. Changes in mean arterial pressure (MAP) (A), heart rate (HR) (B), and oxygen saturation (O2 Sat) (C) during assessment. All data are expressed as mean ± SEM (abbreviations: A, acetaminophen; C, control; M, melatonin; T1, entering to the operating room; T2, during retrobulbar block; T3, during operation; T4, 20 minutes after operation; T5, end of operation; T6, recovery room).
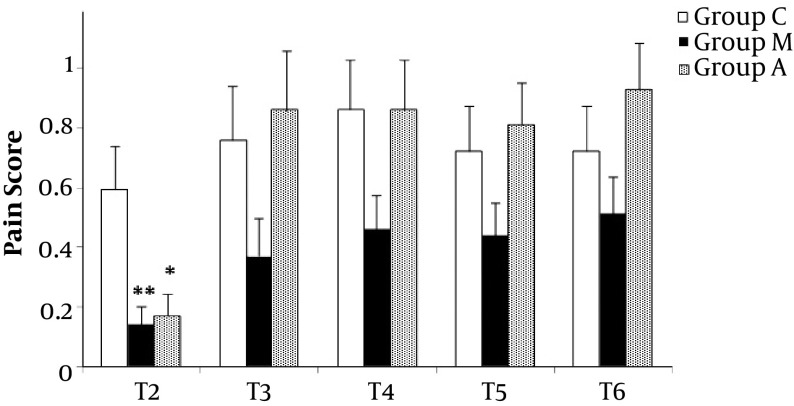
Distribution of pain severity in different stages of surgery was shown in Table 2. All patients were evaluated for pain before entering the operating room; their pain score was zero. None of the patients experienced very severe or extremely severe pain. We found that in the T2 stage, the number of patients in the no pain class significantly increased in either melatonin or acetaminophen groups compared to the control group (P < 0.05). In the rest of the stages, the distribution of painless subjects in the studied groups did not show any significant difference. Compared to control group, melatonin and acetaminophen groups were able to significantly reduce pain score during retrobulbar block (P < 0.01 and P < 0.05, respectively) (Figure 3). In respect to classification of pain score, no significant difference was found during surgery, at the end of surgery, and in the recovery stages in all groups. The amount of additional fentanyl in the control group was 5.6 ± 1.74 μg/dL and in acetaminophen and melatonin groups were 1.72 ± 0.84 μg/dL and 1.27 ± 0.72 μg/dL, respectively. The amount of fentanyl in the melatonin group, however, not acetaminophen group, decreased compared with the control group, significantly (P < 0.05). Only one patient showed complications in the melatonin group.
Table 2. Distribution of Patients Based on the Severity of Pain in the Different Stages of Operation.
| Variable | Number of Patients | ||||
|---|---|---|---|---|---|
| T2 | T3 | T4 | T5 | T6 | |
| Control (n = 58) | |||||
| No pain (0) | 44 | 42 | 37 | 40 | 40 |
| Mild pain (1 - 2) | 11 | 10 | 17 | 15 | 15 |
| Moderate pain (3 - 4) | 3 | 0 | 0 | 0 | 0 |
| Severe pain (5 - 6) | 0 | 0 | 4 | 3 | 3 |
| Acetaminophen (n = 58) | |||||
| No pain (0) | 53a | 41 | 38 | 36 | 34 |
| Mild pain (1 - 2) | 5 | 10 | 14 | 20 | 20 |
| Moderate pain (3 - 4) | 0 | 6 | 2 | 1 | 2 |
| Severe pain (5 - 6) | 0 | 1 | 4 | 1 | 2 |
| Melatonin (n = 59) | |||||
| No pain (0) | 55b | 50 | 46 | 45 | 44 |
| Mild pain (1 - 2) | 4 | 7 | 12 | 14 | 14 |
| Moderate pain (3 - 4) | 0 | 2 | 1 | 0 | 0 |
| Severe pain (5 - 6) | 0 | 0 | 0 | 0 | 1 |
Abbreviations: A, acetaminophen; C, control; M, melatonin.
aP < 0.05 compared to the control group.
bP < 0.01 compared to the control group.
Figure 3. Pain score in different stages of operation (abbreviations: A, acetaminophen; C, control; M, melatonin; T1, entering to the operating room; T2, during retrobulbar block; T3, during operation; T4, 20 minutes after operation; T5, end of operation; T6, recovery room). *P < 0.05 and **P < 0.01 compared to the control group.
5. Discussion
Our findings showed that administration of acetaminophen and melatonin reduced the pain in the retrobulbar block, however, not during and after surgery. In addition, melatonin was able to reduce the need for additional analgesic therapy during the operation.
In the present study, melatonin was able to reduce the pain score during retrobulbar block. Although pain score decreased during and after operation, the differences were not significant. The effect of melatonin on pain was reported in several studies (13-19). In the only study on retrobulbar block, melatonin had no effect on pain during the block and during and after surgery (18). A systematic study has shown that the effects of melatonin in the various stages of the surgical process are limited and there are contradictory results. This contradiction may be due to the dosage, sex, anxiety levels, and also high risks of bias based on the small sample size used in various studies. Nevertheless, the evidence available from clinical trials suggests that melatonin, as an anxiolytic and analgesic agent, can be an alternative candidate for drugs prescribed before surgery (13). Reducing the amount of pain during retrobulbar block by melatonin in this study is contrary to the findings of Khezri et al. (18). This contradiction may be associated with the quality of melatonin, and how and when it was taken. They used sublingual route 90 min before entering the operation room whereas oral melatonin was applied in our study 60 min before operation. Both sublingual and oral melatonin showed a positive analgesic effect in human experimental studies. Time to maximal plasma concentration value and elimination half-life for sublingual and oral melatonin were approximately 50 min and 45 min, respectively (19). Therefore, it seems that administration of melatonin, 90 min before operation, may reduce its analgesic effect.
Applying additional fentanyl during surgery was reduced by melatonin. This decrease occurred despite no significant reduction of pain score during or after operation in the melatonin group compared to the control group. The reason was that we compared pain score in each stage of operation, however, fentanyl consumption was compared in overall stages. In addition, applying more fentanyl itself led to a reduction of pain score in the control group. In a review article, three out of five studies reported a reduction in requirement of additional fentanyl during operation when the effect of melatonin with placebo was compared (20). In the only study conducted in retrobulbar block, no significant difference in the use of fentanyl in the melatonin and control groups was found (18).
In our study, melatonin had no effect on pain relief during and after operation. Our findings are consistent with the results of the study by Khezri et al (18). In addition, melatonin was not able to change the hemodynamic parameters during retrobulbar block and in all operative and postoperative stages. Three studies reported the effect of melatonin on arterial pressure and heart rate and showed no significant changes in different stages of operation (14, 16, 18). In all the mentioned studies, the percentage of oxygen saturation has not been evaluated.
To evaluate the effect of acetaminophen on pain, a single dose of 500 mg of acetaminophen was administered one hour before surgery. The time of administration was determined based on three parameters: Previous studies, giving the medications at the same time, and the peak concentration of acetaminophen after oral administration (approximately 45 to 60 minutes) (21).
Acetaminophen, like melatonin, could reduce the pain score during retrobulbar block, however, not during operation time and postoperative stages. The use of additional fentanyl was not different between acetaminophen and control groups.
Many investigations have reported the effect of postoperative administration of non-opioid medications (22-25), including acetaminophen (26-30), on the postoperative pain, and opioid sparing. However, the efficacy of preoperative administration of acetaminophen on pain after surgery was reported only by limited studies (31). As long as we have studied, the effect of acetaminophen on pain in the retrobulbar block has not been studied yet and the present study, for the first time, shows the analgesic effects of acetaminophen in the retrobulbar block.
The evaluation of hemodynamic parameters in the acetaminophen group did not delineated any significant difference at all stages of surgery. Limited studies have been conducted on the effect of single-dose acetaminophen on hemodynamic parameters in patients (32, 33). Furthermore, none of them are related to retrobulbar block and cataract surgery. It seems that oral administration of acetaminophen does not alter the hemodynamic parameters.
One of the limitations of this study is the difference in pain tolerance in different individuals, which makes it difficult to judge the patient's real pain. We applied NRS-Visual Analogue Scale (VAS) and NRS are two pain assessment tools that are least problematic in most studies (34). Individual differences between surgeons and anesthetists can also cause bias. In this study, all surgeries were performed by the same anesthetist and the same surgeon.
For the first time, in this study, the analgesic effects of acetaminophen were shown in retrobulbar block. Melatonin, in addition to reducing pain during the retrobulbar block, reduced the amount of fentanyl consumption. Considering the doses used in this study and their safety in higher doses, it seems that administration of melatonin and acetaminophen would have a beneficial effect to control the pain in the retrobulbar block.
Footnotes
Authors' Contribution:Soudabeh Hadadi contributed to study conception and design, data acquisition and interpretation and study supervision. Reyhaneh Shahrokhirad participated in data acquisition and helped to draft the manuscript. Malek Moien Ansar involved in study conception, statistical analysis and data interpretation, drafting and critically revising the manuscript. Shideh Marzban and Arman Parvizi were responsible for control of data acquisition and have an advisory function. Mitra Akbari contributed to cataract surgical procedure.
Financial Disclosure:This research was supported by special fund from Guilan University of Medical Sciences, Rasht, Iran.
Ethical Considerations:The study protocol was approved by the University Ethics Committee (Code of Ethics 1930474206) and registered at the Iranian Registry of Clinical Trials (IRCT2015012315963N4).
Contributor Information
Soudabeh Haddadi, Email: so_haddadi@yahoo.com.
Reyhaneh Shahrokhirad, Email: shahrokhireyhaneh@yahoo.com.
Malek Moien Ansar, Email: ansar_moien@yahoo.com.
Shideh Marzban, Email: shideh_42@yahoo.com.
Mitra Akbari, Email: mitra.akbari@gmail.com.
Arman Parvizi, Email: arman_parvizi@yahoo.com.
References
- 1.Rosenberg EA, Sperazza LC. The visually impaired patient. Am Fam Physician. 2008;77(10):1431–6. [PubMed] [Google Scholar]
- 2.Allen D, Vasavada A. Cataract and surgery for cataract. BMJ. 2006;333(7559):128–32. doi: 10.1136/bmj.333.7559.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong TY. Effect of increasing age on cataract surgery outcomes in very elderly patients. BMJ. 2001;322(7294):1104–6. doi: 10.1136/bmj.322.7294.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glantz L, Drenger B, Gozal Y. Perioperative myocardial ischemia in cataract surgery patients: General versus local anesthesia. Anesth Analg. 2000;91(6):1415–9. doi: 10.1097/00000539-200012000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Navaleza JS, Pendse SJ, Blecher MH. Choosing anesthesia for cataract surgery. Ophthalmol Clin North Am. 2006;19(2):233–7. doi: 10.1016/j.ohc.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Maghsoudi B, Talebnejad MR, Asadipour E. Analgesia for retrobulbar block--comparison of remifentanil, alfentanil and fentanyl. Middle East J Anaesthesiol. 2007;19(3):595–602. [PubMed] [Google Scholar]
- 7.Alhashemi JA. Dexmedetomidine vs midazolam for monitored anaesthesia care during cataract surgery. Br J Anaesth. 2006;96(6):722–6. doi: 10.1093/bja/ael080. [DOI] [PubMed] [Google Scholar]
- 8.[No authors listed] Melatonin monograph. Altern Med Rev. 2005;10(4):326–36. [PubMed] [Google Scholar]
- 9.Khezri MB, Merate H. The effects of melatonin on anxiety and pain scores of patients, intraocular pressure, and operating conditions during cataract surgery under topical anesthesia. Indian J Ophthalmol. 2013;61(7):319–24. doi: 10.4103/0301-4738.99637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andersen LPH, Werner MU, Rosenberg J, Gogenur I. Melatonin in surgery and critical care medicine. J Anesth Clin Res. 2014;5(5) doi: 10.4172/2155-6148.1000407. [DOI] [Google Scholar]
- 11.Macleod AG, Ashford B, Voltz M, Williams B, Cramond T, Gorta L, et al. Paracetamol versus paracetamol-codeine in the treatment of post-operative dental pain: A randomized, double-blind, prospective trial. Aust Dent J. 2002;47(2):147–51. doi: 10.1111/j.1834-7819.2002.tb00319.x. [DOI] [PubMed] [Google Scholar]
- 12.Linebarger EJ, Hardten DR, Shah GK, Lindstrom RL. Phacoemulsification and modern cataract surgery. Survey Ophthalmol. 1999;44(2):123–47. doi: 10.1016/s0039-6257(99)00085-5. [DOI] [PubMed] [Google Scholar]
- 13.Yousaf F, Seet E, Venkatraghavan L, Abrishami A, Chung F. Efficacy and safety of melatonin as an anxiolytic and analgesic in the perioperative period: A qualitative systematic review of randomized trials. Anesthesiology. 2010;113(4):968–76. doi: 10.1097/ALN.0b013e3181e7d626. [DOI] [PubMed] [Google Scholar]
- 14.Ismail SA, Mowafi HA. Melatonin provides anxiolysis, enhances analgesia, decreases intraocular pressure, and promotes better operating conditions during cataract surgery under topical anesthesia. Anesth Analg. 2009;108(4):1146–51. doi: 10.1213/ane.0b013e3181907ebe. [DOI] [PubMed] [Google Scholar]
- 15.Caumo W, Levandovski R, Hidalgo MP. Preoperative anxiolytic effect of melatonin and clonidine on postoperative pain and morphine consumption in patients undergoing abdominal hysterectomy: A double-blind, randomized, placebo-controlled study. J Pain. 2009;10(1):100–8. doi: 10.1016/j.jpain.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Mowafi HA, Ismail SA. Melatonin improves tourniquet tolerance and enhances postoperative analgesia in patients receiving intravenous regional anesthesia. Anesth Analg. 2008;107(4):1422–6. doi: 10.1213/ane.0b013e318181f689. [DOI] [PubMed] [Google Scholar]
- 17.Naguib M, Samarkandi AH. The comparative dose-response effects of melatonin and midazolam for premedication of adult patients: A double-blinded, placebo-controlled study. Anesth Analg. 2000;91(2):473–9. doi: 10.1097/00000539-200008000-00046. [DOI] [PubMed] [Google Scholar]
- 18.Khezri MB, Oladi MR, Atlasbaf A. Effect of melatonin and gabapentin on anxiety and pain associated with retrobulbar eye block for cataract surgery: A randomized double-blind study. Indian J Pharmacol. 2013;45(6):581–6. doi: 10.4103/0253-7613.121368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harpsoe NG, Andersen LP, Gogenur I, Rosenberg J. Clinical pharmacokinetics of melatonin: A systematic review. Eur J Clin Pharmacol. 2015;71(8):901–9. doi: 10.1007/s00228-015-1873-4. [DOI] [PubMed] [Google Scholar]
- 20.Hansen MV, Halladin NL, Rosenberg J, Gogenur I, Moller AM. Melatonin for pre- and postoperative anxiety in adults. Cochrane Database Syst Rev. 2015;(4):CD009861. doi: 10.1002/14651858.CD009861.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bertolini A, Ferrari A, Ottani A, Guerzoni S, Tacchi R, Leone S. Paracetamol: New vistas of an old drug. CNS Drug Rev. 2006;12(3-4):250–75. doi: 10.1111/j.1527-3458.2006.00250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rahimzadeh P, Imani F, Nikoubakht N, Koleini Z, Faiz SHR, Sayarifard A. A comparative study on the efficacy of oral memantine and placebo for acute postoperative pain in patients undergoing dacryocystorhinostomy (DCR). Anesth Pain Med. 2017;7(3):e45297. doi: 10.5812/aapm.45297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Entezary SR, Farshadpour S, Alebouyeh MR, Imani F, Emami Meybodi MK, Yaribeygi H. Effects of preoperative use of oral dextromethorphan on postoperative need for analgesics in patients with knee arthroscopy. Anesth Pain Med. 2014;4(1):e11187. doi: 10.5812/aapm.11187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Imani F, Rahimzadeh P. Gabapentinoids: Gabapentin and pregabalin for postoperative pain management. Anesth Pain Med. 2012;2(2):52–3. doi: 10.5812/aapm.7743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alimian M, Imani F, Hassani V, Rahimzadeh P, Sharifian M, Safari S. Effects of single-dose pregabalin on postoperative pain in dacryocystorhinostomy surgery. Anesth Pain Med. 2012;2(2):72–6. doi: 10.5812/aapm.4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Atef A, Fawaz AA. Intravenous paracetamol is highly effective in pain treatment after tonsillectomy in adults. Eur Arch Otorhinolaryngol. 2008;265(3):351–5. doi: 10.1007/s00405-007-0451-5. [DOI] [PubMed] [Google Scholar]
- 27.Delbos A, Boccard E. The morphine-sparing effect of propacetamol in orthopedic postoperative pain. J Pain Symptom Manage. 1995;10(4):279–86. doi: 10.1016/0885-3924(95)00004-I. [DOI] [PubMed] [Google Scholar]
- 28.Hernandez-Palazon J, Tortosa JA, Martinez-Lage JF, Perez-Flores D. Intravenous administration of propacetamol reduces morphine consumption after spinal fusion surgery. Anesth Analg. 2001;92(6):1473–6. doi: 10.1097/00000539-200106000-00024. [DOI] [PubMed] [Google Scholar]
- 29.Peduto VA, Ballabio M, Stefanini S. Efficacy of propacetamol in the treatment of postoperative pain. Morphine-sparing effect in orthopedic surgery. Italian Collaborative Group on Propacetamol. Acta Anaesthesiol Scand. 1998;42(3):293–8. doi: 10.1111/j.1399-6576.1998.tb04919.x. [DOI] [PubMed] [Google Scholar]
- 30.Imani F, Faiz HR, Sedaghat M, Hajiashrafi M. Effects of adding ketamine to fentanyl plus acetaminophen on postoperative pain by patient controlled analgesia in abdominal surgery. Anesth Pain Med. 2014;4(1):e12162. doi: 10.5812/aapm.12162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moon YE, Lee YK, Lee J, Moon DE. The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet. 2011;284(6):1455–60. doi: 10.1007/s00404-011-1860-7. [DOI] [PubMed] [Google Scholar]
- 32.Kord Valeshabad A, Nabavian O, Nourijelyani K, Kord H, Vafainejad H, Kord Valeshabad R, et al. Attenuation of hemodynamic responses to laryngoscopy and tracheal intubation: Propacetamol versus lidocaine-A Randomized clinical trial. Anesthesiol Res Pract. 2014;2014:170247. doi: 10.1155/2014/170247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Remy C, Marret E, Bonnet F. Effects of acetaminophen on morphine side-effects and consumption after major surgery: Meta-analysis of randomized controlled trials. Br J Anaesth. 2005;94(4):505–13. doi: 10.1093/bja/aei085. [DOI] [PubMed] [Google Scholar]
- 34.Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]