Abstract
Chronic suppurative otitis media is an inflammatory condition characterized by disruption of tympanic membrane and aural discharge. It is one of the most incidental conditions in head and neck. There has been a substantial debate about the therapeutic approach for some decades now. From review of past medical literature, it was evident that culture and sensitivity is essential in eradicating the causative organism. However, the cost-effectiveness is a major concern for low-income population. Due to such concern, empirical therapy has proved to be a suitable therapeutic approach since commonly found organisms are highly sensitive to routine antibiotics.
Keywords: Chronic suppurative otitis media, otoscopy, empirical therapy
Short Commentary
Chronic suppurative otitis media (CSOM) is a chronic inflammation of middle ear cavity mucosa with a perforated tympanic membrane and discharge.1 Different regions display significant variations in the prevalence of CSOM. Its prevalence is highest among Inuit, South Pacific Islands and African region however lowest in the United States, United Kingdom, and Denmark.2
The classification of CSOM mainly depends on complete clinical history along with a detailed otoscopic examination of diseased ear. It is mainly classified into six categories which are (1) solitary perforation of the tympanic membrane with no other symptoms; (2) intact membrane with hearing loss (conductive type); (3) tympanic membrane perforation with disease confined to the middle ear and tympanum; (4) cholesteatoma (attico-antral); (5) disease involving the middle ear, epitympanum, and mastoid without cholesteatoma; (6) disease involving the middle ear, epitympanum, and mastoid with cholesteatoma.3
Bacteria are commonly causative agents of CSOM which includes Pseudomonas aeruginosa, Staphylococcus aureus, Diphtheroids, Proteus species, and Klebsiella pneumoniae. Most frequently isolated organism (in 48%-98% cases) is P. aeruginosa followed by S. aureus (in 15%-30% cases). Sometimes, superimposed fungal or an anaerobic infection is concurrently present with these organisms.4 In most instances, culture results show mixed bacteriology which includes the contribution from environmental, bacterial, host, and genetic makeup factors. This is why the treatment approach toward CSOM is no single standardize therapy. It is a multi-modal approach to eradicate all the present organisms in suppuration.5
Diagnosis of CSOM depends on detailed history of sign and symptoms like hearing loss, aural discharge, headache, itching in auditory canal, and so on and complete otoscopic examination. Sometimes, otalgia and rhinitis are also associated with CSOM but mostly present in acute settings. Things that need to be focused on otoscopic examination are the integrity of tympanic membrane and the attic for exclusion of cholesteatoma.6 Next step in the diagnostic evaluation includes culture and sensitivity which is done in two steps. First step is the direct examination of smear in which pathogens are collected with swab and prepared on a glass slide which is then inoculated on different culture media which includes MacConkey agar plate, blood agar plate, chocolate agar plate, and nutrient agar plate. Suspected fungal species are isolated on Sabouraud agar plate. The next step is the determination of sensitivity of organisms to available antibiotics which is done by Kirbay-Bauer disk diffusion method.7
However, the cost affectivity is major concern for a person who belongs to low socio-economic background. A study in developing country like Nigeria indicated that an average cost on the diagnosis, treatment, and follow-up of CSOM is around US$462.7. The initial treatment cost is around US$51.3 and the average monthly wages of a Nigerian worker is around US$47.5 which is not even sufficient to cover initial treatment cost.8 Which is why, the idea of empiric therapy without obtaining culture and sensitivity profile is effective since the most commonly isolated organism is Pseudomonas.4
Regarding the sensitivity profile, most of the organisms are sensitive to commonly available antibiotics like Quinolones, Amikacin, Cephalosporin, and so on. A study from a developing country showed that S. aureus is highly sensitive to Linezolid (100%) and Vancomycin (100%). Pseudomonas is 76.9% sensitive to Tobramycin, 69.2% sensitive to Ciprofloxacin and Meropenem. However, most of the gram-negative isolates (Escherichia coli, Klebsiella, Citrobacter) were sensitive to Amikacin and Piperacillin/Tazobactam.9 Similarly, in another study, most effective agents against Pseudomonas are Piperacillin (97.3%) followed by Tobramycin and Ciprofloxacin (83.8% each). But Cephalosporins, Doxycycline, and Amoxiclav showed 100% affectivity against S. aureus. This study is another example of low-socioeconomic status.10 Another study conducted in India showed that Pseudomonas is 100% sensitive to Imipenem, Meropenem, and Polymyxin B however; S. aureus is 100% sensitive to Linezolid and Vancomycin.11 Similar research conducted in Nepal showed that Pseudomonas is 100% sensitive to Ciprofloxacin, 99% to Amikacin, and 87% Ofloxacin. For S. aureus, it is 87% sensitive to Cloxacillin and 81% to Ofloxacin.12 Summary of all these studies is given in Table 1. Above evidence prove that commonly extracted organisms are highly sensitive to common antibiotics. An empiric therapy can be a good approach in low socioeconomic settings.
Table 1.
Sensitivity profile of Pseudomonas aeruginosa and Staphylococcus aureus.
| P. aeruginosa | S. aureus | References | |
|---|---|---|---|
| Antibiotics and their sensitivity profile | Linezolid (100%) Vancomycin (100%) |
Tobramycin (76.9%) Ciprofloxacin (69.2%) Meropenem (69.2%) |
Kumar et al9 |
| Piperacillin (97.3%) Tobramycin (83.8%) Ciprofloxacin (83.8%) |
Cephalosporins (100%) Doxycycline (100%) Amoxiclav (100%) |
Vishwanath et al10 | |
| Imipenem (100%) Meropenem (100%) Polymyxin B (100%) |
Linezolid (100%) Vancomycin (100%) |
Agrawal et al11 | |
| Ciprofloxacin (100%) Amikacin (99%) Ofloxacin (87%) |
Cloxacillin (87%) Ofloxacin (81%) |
Sharma et al12 |
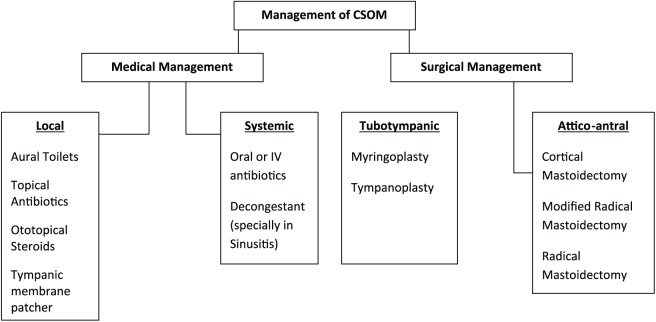
Initial standardize therapeutic approach for CSOM is aural toilets and topical antibiotic drops.13 The most commonly followed approach for treatment of CSOM is given in Figure 1. After eradication of organism, the next step is to repair the tympanic membrane.13
Figure 1.
Therapeutic approach in the management of chronic suppurative otitis media (CSOM).
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: SBB: Principal idea, conception of work, literature search, paper writing, final proving of manuscript. SIA: Literature search, paper writing.
ORCID iD: Syeda Beenish Bareeqa  https://orcid.org/0000-0001-5579-4141
https://orcid.org/0000-0001-5579-4141
References
- 1. Verhoeff M, van der Veen EL, Rovers MM, Sanders EAM, Schilder AGM. Chronic suppurative otitis media: a review. Int J Pediatr Otorhinolaryngol. 2006;70:1–12. [DOI] [PubMed] [Google Scholar]
- 2. Bluestone CD. Epidemiology and pathogenesis of chronic suppurative otitis media: implications for prevention and treatment1. Int J Pediatr Otorhinolaryngol. 1998;42:207–223. [DOI] [PubMed] [Google Scholar]
- 3. Pulec JL, Deguine C. Classification of chronic suppurative otitis media. Oper Tech Otolaryngol Head Neck Surg. 1995;6:2–4. [Google Scholar]
- 4. Roland NJ, McRae RDR, McCombe AW. Chronic suppurative otitis media. In: McCombe AW, Roland NJ, MCRae RDR, eds. Key Topics in Otolaryngology and Head and Neck Surgery. 2nd ed. Abingdon, UK: BIOS Scientific Publishers; 2001:38–41. [Google Scholar]
- 5. Mittal R, Lisi CV, Gerring R, et al. Current concepts in the pathogenesis and treatment of chronic suppurative otitis media. J Med Microbiol. 2015;64:1103–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ramakrishnan K, Sparks RA, Berryhill WE. Diagnosis and treatment of otitis media. Am Fam Physician. 2007;76:1650–1658. [PubMed] [Google Scholar]
- 7. Shyamala R, Reddy PS. The study of bacteriological agents of chronic suppurative otitis media-aerobic culture and evaluation. J Microbiol Biotechnol Res. 2017;2:152–162. [Google Scholar]
- 8. Adoga A, Nimkur T, Silas O. Chronic suppurative otitis media: socio-economic implications in a tertiary hospital in Northern Nigeria. Pan Afr Med J. 2010;4:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kumar R, Srivastava P, Sharma M, Rishi S, Nirwan S, Hemwaniand K. Isolation and antimicrobial sensitivity profile of bacterial agents in chronic suppurative otitis media patients at NIMS Hospital, Jaipur. IJPBS. 2013;3:265–269. [Google Scholar]
- 10. Vishwanath S, Mukhopadhyay C, Prakash R, Pillai S, Pujary K, Pujary P. Chronic suppurative otitis media: optimizing initial antibiotic therapy in a tertiary care setup. Indian J Otolaryngol Head Neck Surg. 2012;64:285–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Agrawal A, Kumar D, Goyal A, Goyal S, Singh N, Khandelwal G. Microbiological profile and their antimicrobial sensitivity pattern in patients of otitis media with ear discharge. Indian J Otology. 2013;19:5. [Google Scholar]
- 12. Sharma S, Rehan HS, Goyal A, Jha AK, Upadhyaya S, Mishra SC. Bacteriological profile in chronic suppurative otitis media in Eastern Nepal. Tropical Doctor. 2004;34:102–104. [DOI] [PubMed] [Google Scholar]
- 13. Prunty S, Ha J, Vijayasekaran S. Management of chronic suppurative otitis media. In: Preciado D, ed. Otitis Media: State of the Art Concepts and Treatment. London, England: Springer; 2015:117–122. [Google Scholar]