Abstract
Background:
Despite the increasing incidence of sports-related knee injuries in youth athletes, few studies have reported on the diagnosis and treatment of pediatric and adolescent meniscal root injuries.
Purpose:
To describe traumatic posterior meniscal root injuries in a pediatric and adolescent population and compare the presentation of meniscal root injuries versus that of nonroot injuries.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A study was conducted of all knee arthroscopies performed on consecutive patients treated in a pediatric sports practice from March 2012 through February 2015. All patients who were younger than 20 years at the time of their injury and who underwent an arthroscopy with meniscal injury were included. Patients with discoid lateral meniscus, atraumatic meniscal cysts, partial-thickness meniscal root injuries (LaPrade type 1), and recurrent root tears were excluded. A comparative analysis of root and nonroot injuries was performed.
Results:
A total of 314 patients had surgery for meniscal injury (mean patient age, 16.0 years; range, 10.5-19.6 years). Of these patients, 58 (18.5%) posterior meniscal root injuries were identified. The root injuries were more likely to have joint line tenderness on preliminary physical examination compared with nonroot injuries (96.5% vs 58.6%, respectively; P < .001). Root injuries rarely occurred in isolation compared with nonroot meniscal tears (6.9% vs 17.6%; P = .021) and were frequently treated in combination with anterior cruciate ligament (ACL) injuries (86.2%). Lateral root injuries occurred more often in conjunction with ACL injuries compared with medial root injuries (84.8% vs 22.2%; P < .001). On review of preoperative imaging, meniscal extrusion occurred more often in root injuries than in nonroot injuries (32.8% vs 3.5%; P < .0001) and was uncommonly seen in the skeletally immature patient. Extrusion was seen more often in medial than lateral root tears (66.7% vs 21.7%; P = .008). A majority of patients (57/58) underwent transosseous suture repair of the meniscal root.
Conclusion:
When treating a pediatric or adolescent patient for a traumatic meniscal tear, a surgeon may expect to see a posterior meniscal root injury in as many as 1 in 6 patients. When treated for an ACL, contact, or multiligament injury or meniscal extrusion, a pediatric or adolescent patient may demonstrate a meniscal root avulsion or complex meniscal tear. These data provide practitioners with an improved ability to identify and treat meniscal root injuries that otherwise lead to rapid cartilage degeneration.
Keywords: meniscal tear, meniscus root, pediatric, adolescent, repair
Meniscal root injuries are uncommon; they occur in 0.8% to 15% of knee injuries, with a higher incidence associated with an anterior cruciate ligament (ACL) injury.3,4,7,9,11,20,23 Since the first described case report, published by Pagnani et al21 in 1991 and involving a 20-year-old patient, the majority of reported meniscal root injuries have involved the adult and young adult population, with limited data in the pediatric and adolescent population.14,21 Assessing 1857 knee arthroscopies, Matheny et al20 reported the prevalence of meniscal root injuries to be 7.4% with a mean patient age of 37 years (range, 17-68 years). Shieh et al23 reported on meniscal injuries in pediatric and adolescent patients ranging from 10 to 19 years old, and demonstrated that meniscal root injuries occurred in 2% of surgically treated menisci. Furthermore, fewer than 10 cases of pediatric medial meniscal root injuries have been reported in the literature to date.13,19,24 Prior to recent literature, the identification of meniscal root injuries during knee arthroscopy was uncommon; however, the importance of meniscal root injuries has now been recognized.
A meniscal root injury, with or without meniscal extrusion, is biomechanically equivalent to meniscal loss.1,6,8 Biomechanical studies over the past 2 decades have demonstrated the association of meniscal root injuries with loss of knee stability12 and increase in total contact pressure of the affected compartment.6,8 Loss of function of the meniscus decreases meniscal-cartilage surface contact, reducing biomechanical and shock absorption functions. This increase in cartilage stress accelerates the degeneration of the knee cartilage, leading to long-term functional problems.1,8 Given the increasing participation rates in youth athletics, the diagnosis and treatment of pediatric and adolescent meniscal injury, especially meniscal root injuries, are more important than ever.
The purpose of this study was to describe the prevalence, demographics, clinical presentation, associated injuries, tear patterns, and treatments for historically uncommon meniscal root injuries in the youth population. A secondary purpose was to compare the presentation of meniscal root injuries versus surgically treated meniscal tears without a root injury.
Methods
An institutional review board–approved assessment was conducted of all knee arthroscopies performed on consecutive patients treated in a pediatric sports practice from March 2012 through February 2015. We performed an electronic medical records search for all patients treated arthroscopically by 1 of 2 surgeons (P.L.W. and H.B.E.) for a medial or lateral meniscal tear. Billing records were reviewed for arthroscopic meniscectomy or meniscal repair codes used within this period. All patients younger than 20 years at the time of their injury or who underwent an arthroscopy with meniscal injury were included in the study. Discoid lateral menisci were excluded owing to the disorganization of the collagen and unclear biomechanical properties compared with normal meniscal tissue. Atraumatic meniscal cysts and partial-thickness injuries (LaPrade type 1 tears) were also excluded. Additional exclusion criteria included recurrent root tears.
Demographic data and presenting complaints were extracted from a chart review. Symptoms of instability, pain, popping, catching, locking, swelling, numbness, and limitations in range of motion were recorded, and mechanism of injury and sport participation at the time of injury were noted. Injuries were classified as either contact or noncontact; injuries resulting from high-energy mechanisms, such as those occurring in motocross, cycling, skateboard, scooter, playground, football, gymnastics, and wrestling, were considered contact injuries.
Standard 3-view knee radiographs were performed and reviewed. Preoperative advanced imaging such as magnetic resonance imaging (MRI) or computed tomography (CT) was also reviewed. A single patient with a concomitant tibial spine fracture had a CT scan as opposed to an MRI. The presence of a distinct separate posterior bony avulsion not associated with a tibial spine avulsion injury in the sagittal plan was considered a posterior meniscal root avulsion (LaPrade type 5). On MRI, the presence of grade 2 or 3 signal within 9 mm of the posteromedial or posterolateral root attachment on coronal or sagittal sequences was considered a posterior meniscal root tear. MRI identification of a posterior lateral meniscofemoral ligament was recorded. Additionally, meniscal extrusion (Figure 1) was identified and defined as 3 mm or greater distance of the peripheral margin of the meniscal body from the peripheral margin of the tibial plateau on MRI coronal sequences.2 The prevalence of meniscal root tears was calculated based on the proportion of patients with identified meniscal root injury compared with meniscal surgeries performed.
Figure 1.
Drawing of meniscal extrusion compared with a normal meniscus. Images courtesy of Texas Scottish Rite Hospital for Children, Dallas, Texas. © 2017. All rights reserved.
Arthroscopic description and tear classification were recorded as well as treatment of the meniscal root injury and any other meniscal body injuries. Treatment of meniscal root tears was similar to previously described techniques.3,5 Suture fixation of the meniscal root tear was performed followed by interosseous tunnel fixation through the meniscal root bed to the anterior cortex of the tibia by use of an ACL drill guide. Fixation over the tibial cortex was performed over a button or a suture anchor, with the patient’s knee in terminal extension. Treatments of additional or associated meniscal injury were as follows: partial body meniscectomy, all-inside meniscal body repair, inside-out meniscal body repair, outside-in meniscal body repair, or a combination of these. Treatment decisions by the individual surgeons were based on tear pattern, tear location, and posterior horn or meniscal body stability. Medial and lateral meniscal tears were classified by location (anterior, middle third, or posterior horn) and by tear pattern (longitudinal, horizontal, bucket handle, radial, or complex, the latter of which was defined as a combination of tear types of the body or horn or a posterior meniscal root tear).
The posteromedial and posterolateral meniscal root tears were retrospectively graded according to the LaPrade classification16 using the arthroscopic images. Two of the authors (J.R. and C.W.W.) reviewed all images and, by consensus, assigned tear types to the meniscal root injuries. The posterior meniscal root tears were classified as type 2, complete radial; type 3, bucket handle with root detachment; type 4, complex, oblique; or type 5, avulsion fracture of the meniscal root attachment. LaPrade type 1 tears (partial stable posterior meniscal root tears), which are believed to be of low clinical significance, were not included or identified in this study.
Comparisons were made between the nonposterior meniscal root tear and posterior meniscal root tear groups. Additional comparisons were made between medial and lateral meniscal root injuries, with bicondylar meniscal root injuries excluded from this comparison. A chi-square test was used to compare categorical variables. When the sample was small, a Fisher exact test was performed. Continuous variables were first examined for normality, and the nonparametric test, Mann-Whitney, was used. Statistical significance was set at P < .05.
Results
Of 314 pediatric and adolescent patients with meniscal injury who were surgically treated, 58 (18.5%) posterior meniscal root injuries were identified. The mean age of the entire cohort was 16.0 years (range, 10.5-19.6 years), and 61 (19.4%) had open or transitional knee physes at the time of treatment. Three-fourths (75.4%) of surgically treated meniscal injuries had resulted from a noncontact injury; football, soccer, and basketball were the most common sports played during injury. Differences in demographic and clinical presentation between patients with a nonroot meniscal tear and those with a meniscal root tear are listed in Table 1. No demographic differences between the 2 groups were noted. In the meniscal root tear group, 55 of 58 patients (96.5%) had joint line tenderness on preliminary physical examination, compared with 58.6% in the nonroot meniscal tear group (P < .001).
TABLE 1.
Demographic and Clinical Data of Patients With Meniscal Injuries Treated Operativelya
| Nonroot Meniscal Tear (n = 256) |
Meniscal Root Tear (n = 58) |
P Valueb | |
|---|---|---|---|
| Age, y, mean ± SD (range) | 16.03 ± 1.76 (10.45-19.7) | 16.01 ± 1.49 (12.12-18.52) | .762 |
| Male sex | 151 (59) | 34 (58.6) | .960 |
| Body mass index, mean ± SD (range) | 25.35 ± 5.52 (15.19-48.33) | 25.2 ± 5.58 (15.59-42.41) | .839 |
| Physeal status | |||
| Open | 31 (12.1) | 7 (12.1) | .782 |
| Transitional | 20 (7.8) | 3 (5.2) | |
| Closed | 205 (80.1) | 48 (82.8) | |
| Days from injury to surgery, mean ± SD (range) | 114.42 ± 107.06 (0-620) | 150.1 ± 170.29 (5-915) | .136 |
| Mechanism of injury | |||
| Noncontact | 193 (75.4) | 41 (70.7) | .128 |
| Contact | 60 (23.4) | 14 (24.1) | |
| High-velocity (eg, motor vehicle crash, fall) | 3 (1.2) | 3 (5.2) | |
| Sport played during injury | |||
| Football | 77 (30.1) | 15 (25.9) | .052 |
| Basketball | 51 (19.9) | 11 (19) | |
| Soccer | 70 (27.3) | 14 (24.1) | |
| Other | 42 (16.4) | 18 (31) | |
| Physical examination findings | |||
| Joint line tenderness | 150 (58.6) | 55 (96.5) | <.001 |
| Presence of an effusion | 124 (48.4) | 29 (50) | .830 |
| Range of motion loss | 91 (35.5) | 14 (24.1) | .019 |
| Associated injuries | |||
| None | 45 (17.6) | 4 (6.9) | .021 |
| Anterior cruciate ligament tear | 195 (76.2) | 44 (75.9) | |
| Multiligament knee injury | 9 (3.5) | 4 (6.9) | |
| Tibial spine fracture | 3 (1.2) | 2 (3.4) | |
| Anterior cruciate graft tear | 4 (1.6) | 4 (6.9) |
aResults are reported as n (%) unless otherwise indicated.
bStatistical significance of comparison between the groups was noted when P < .05 (boldface).
Meniscal root tears were less likely to occur in isolation than were nonroot meniscal tears (6.9% vs 17.6%, respectively; P = .021). Meniscal root injuries were frequently treated in combination with ACL injuries (n = 50; 86.2%) including ACL reconstruction (n = 44; 75.9%), ACL revision reconstruction (n = 4; 6.9%), or tibial spine injuries (n = 2; 3.4%). Chondral injuries were seen with similar frequency in both cohorts, except for medial femoral condylar chondral injuries (30.5% nonroot tears vs 19% root tears, P = .090) and coexistent multiple chondral injuries (19.5% nonroot tears vs 36.2% root tears, P = .006).
In this series, 11 patients had multiligament knee injuries and a meniscal injury. Three of the 11 patients with multiligament knee injuries and meniscal injuries had medial meniscal root injuries as well. The 3 medial meniscal root injuries seen in multiligament knee injuries occurred with a concomitant posterior cruciate ligament injury and involved meniscal extrusion. One patient had both lateral and medial meniscal root injuries.
There were 3 patients with both medial and lateral meniscal root injuries (1.0% combined meniscus group), 46 patients (14.6%) with an isolated lateral meniscal root injury, and 9 patients (2.9%) with an isolated medial meniscal root injury. Age, height, weight, and physical examination results were not different between patients with lateral versus medial meniscal root injuries; however, a majority of lateral meniscal root injuries occurred as a result of a noncontact mechanism (82.6%). Medial meniscal root injuries more commonly occurred following a contact or high-velocity mechanism (88.9%). As seen in Table 2, lateral meniscal root injuries occurred in conjunction with ACL injuries 84.8% of the time, while only 2 (22.2%) medial meniscal root injuries occurred with an ACL tear (P < .001). Lateral meniscal root injuries were associated with more chondral injuries and multiple chondral injuries (P = .0232).
TABLE 2.
Comparison of Traumatic Root Tears That Occurred in Lateral and Medial Meniscal Tearsa
| Lateral Meniscal Root Injury (n = 46) |
Medial Meniscal Root Injury (n = 9) |
P Valueb | |
|---|---|---|---|
| Mechanism of injury | |||
| Noncontact | 38 (82.6) | 1 (11.1) | .001 |
| Contact | 7 (15.2) | 6 (66.7) | |
| High energy | 1 (2.2) | 2 (22.2) | |
| Associated injuries | |||
| None | 1 (2.2) | 3 (33.3) | |
| Anterior cruciate ligament tear | 39 (84.8) | 2 (22.2) | <.001 |
| Multiligament knee injury | 1 (2.2) | 3 (33.3) | |
| Tibial spine | 1 (2.2) | 1 (11.1) | |
| Anterior cruciate ligament graft tear | 4 (8.7) | 0 (0) | |
| Primary chondral injury | |||
| None | 17 (37) | 7 (77.8) | .3895 |
| Lateral femoral condyle | 16 (34.8) | 1 (11.1) | |
| Medial femoral condyle | 10 (21.7) | 1 (11.1) | |
| Lateral tibial plateau | 0 (0) | 0 (0) | |
| Medial tibial plateau | 1 (2.2) | 0 (0) | |
| Patella | 1 (2.2) | 0 (0) | |
| Trochlea | 1 (2.2) | 0 (0) | |
| Multiple chondral injuries | 18 (39.1) | 0 (0) | .0232 |
aResults are reported as n (%). The 3 patients with bicondylar root tears are excluded from this analysis.
bStatistical significance of comparison between the groups was noted when P < .05 (boldface).
Meniscal extrusion (Figure 2) occurred in 19 of 58 (32.8%) meniscal root injuries on preoperative advanced imaging. In contrast, nonroot meniscal injuries demonstrated extrusion in 9 of 256 injuries, or 3.5% (P < .0001), and 4 of the 9 entailed medial meniscal extrusion with a complex tear pattern. Significantly, a majority of medial meniscal root tears demonstrated preoperative meniscal extrusion (66.7%) as opposed to 21.7% of lateral meniscal root injuries (P = .008). A total of 218 lateral meniscal tears (69.4%) were identified as having a meniscofemoral ligament, and of those posterior lateral meniscal root injuries with extrusion, 61.5% had a meniscofemoral ligament. Characteristic differences in patients who had meniscal extrusion are listed in Table 3.
Figure 2.

A proton density–weighted, fat-suppressed coronal sequence demonstrating meniscal extrusion of the lateral meniscus and indicating loss of hoop stress of the meniscus.
TABLE 3.
Initial Physical Examination Findings, MRI Characteristics, and Arthroscopic Meniscal Root Tear Classification in Pediatric and Adolescent Patients Who Had Meniscal Extrusion on Preliminary MRI Reviewa
| Lateral Meniscal Root Injury With Extrusion (n = 13) |
Medial Meniscal Root Injury With Extrusion (n = 6) |
|
|---|---|---|
| Open physis | 1 | 0 |
| Joint line tenderness | 12 | 5 |
| Effusion upon presentation | 11 | 4 |
| Associated anterior cruciate ligament injury | 11 | 2 |
| Meniscofemoral ligament present | 8 | NA |
| Root tear classification | ||
| Type 1 | 0 | 0 |
| Type 2 | 6 | 1 |
| Type 3 | 2 | 0 |
| Type 4 | 5 | 0 |
| Type 5 | 0 | 5 |
aResults are reported as No. The 3 patients with bicondylar root tears are excluded from this analysis. Due to the differences in incidence, location, and mechanism of injury, categories of lateral meniscal root injury and medial meniscal root injury were reviewed independently. NA, not applicable.
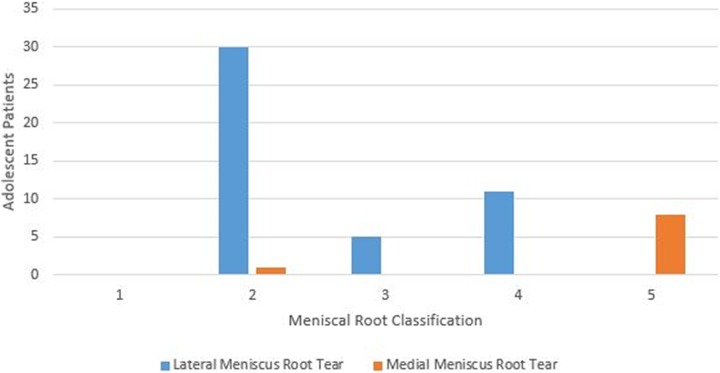
No partial meniscal root tears (type 1) were recorded, as these were not defined as root tears for the purposes of this study. Lateral meniscal root injuries were primarily type 2 (65.2%) or type 4 (23.9%) (Figure 3). No root avulsions occurred in lateral meniscal root injuries. In lateral meniscal root tears, extrusion was seen only in type 4 tears and with closed physes. Extrusion was not seen in patients with open physes. A medial root avulsion, classification type 5, was the predominant medial root tear pattern. It was noted in 8 of 9 (88.9%) medial injuries (Figure 4). A majority of patients underwent an arthroscopic anatomic repair, and all but 1 of the patients were treated with transosseous suture reconstruction.
Figure 3.
Lateral and medial meniscal root classifications in a pediatric and adolescent population.
Figure 4.
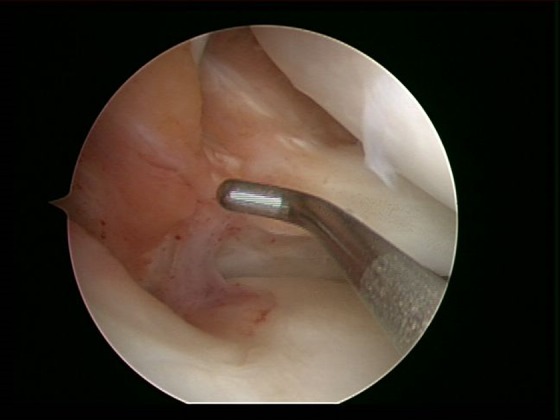
Arthroscopic image of the posterior horn of a medial meniscal root avulsion (LaPrade type 5).
Discussion
The purpose of this study was to describe posterior meniscal root tear patterns, prevalence (defined as the proportion of patients with identified meniscal root injury compared with meniscal surgeries performed), and the presence of extrusion on advanced imaging and then compare these results with those for nonroot meniscal tears. In our pediatric and adolescent cohort, 18.5% of meniscal injuries were meniscal root injuries, which is higher than previously reported in this age group.23 The prevalence of posterior medial meniscal root injuries found in our study (2.9%) was similar to that reported in a comparable series of all arthroscopies performed for meniscal injuries in an adult population (3.4%).20 The prevalence of posterior lateral meniscal root injuries in our cohort, occurring 5 times as frequently as posterior medial root injuries, was higher than previously reported. However, an effort was made to restrict this study group to a traumatic population by excluding discoid menisci and meniscal cysts. Additionally, in this age group, almost all meniscal tears are traumatic in nature, whereas adult patients would likely have a higher proportion of degenerative tears. This resulted in a current cohort that had a coexisting ACL injury rate of 75.2%. These factors likely account for the higher prevalence of posterior lateral meniscal tears in our population compared with reported adult series. In fact, when examining the association of posterior lateral root tears with an ACL injury, previous authors reported that 14% to 15% of ACL injuries involved posterior lateral root tears9,11; a similar proportion (15.3%) of the ACL injuries in our cohort had an associated posterior lateral root tear.
Posterior medial meniscal root avulsions were associated with high-energy mechanisms (88.9%), consisting of contact or collision injuries, and were seen in isolation or in combination with varied patterns of ligament injury. The mechanisms and coincident ligament injuries were comparable with those in adult patients.20 However, the adult population demonstrated a high number of concurrent cartilage injuries with posterior medial meniscal root tears (74%) and a predominant type 2 injury pattern (78.4%).15,17,20 Significantly, in our young population with these higher energy mechanisms, almost all posterior medial meniscal root tears (89%) were type 5 osteocartilaginous avulsion injuries, but the majority did not have an associated cartilage injury (77.8%).
In contrast, posterior lateral meniscal root injuries were predominantly transverse or oblique tears in the zone of the root (types 2 and 4) and were associated with a high number of noncontact ACL injuries (82.6%). While this tear classification and high association with ACL injury are consistent with adult reports, posterior lateral meniscal root tears in adults have more often been associated with contact mechanisms.6,10,18 High rates of noncontact ACL injuries are known to be present in the youth population, as was demonstrated in this series. It is possible that this accounts for the discrepancy in mechanism compared with an adult population.
Meniscal extrusion was present in 28 (8.9%) of all patients undergoing surgery for meniscal injury in this young population. When meniscal extrusion was present, it was associated with a posterior meniscal root tear 68% of the time. Meniscal extrusion was seen at a higher rate in posterior medial meniscal root tears (66.7%) than in posterior lateral meniscal root tears (28.3%). This is consistent with the adult literature and the theory that the presence of a meniscofemoral ligament may stabilize the meniscus and prevent extrusion in the setting of a posterior meniscal root tear when this meniscofemoral ligament is present.4,6,22 Thus, the majority of posterior medial meniscal root tears would be expected to exhibit extrusion and subsequent loss of meniscal function, strongly indicating the benefit of attempted meniscal root repair. Conversely, posterior lateral meniscal root tears often may be expected to occur in the setting of a meniscofemoral ligament, which may protect function of the meniscus by limiting extrusion. However, we noted extrusion to be present in some cases when a meniscofemoral ligament was present. In 8 of the 13 cases (61.5%) of extrusion of the lateral meniscus in the setting of a posterior lateral meniscal root tear, a meniscofemoral ligament was identified. Because the long-term stabilizing function of an intact meniscofemoral ligament against meniscal extrusion remains unclear, and because our findings suggest that extrusion may occur even in the setting of a meniscofemoral ligament, meniscal root repair may be indicated in posterior lateral meniscal root tears, just as it is believed to be indicated in all posterior medial meniscal root tears. All patients in our study were able to have arthroscopic root repair, with all but 1 undergoing repair with a transosseous suture technique.
We acknowledge some limitations of this study. As a retrospective analysis, it is subject to the inherent flaws of such study types. However, meniscal root injuries and classifications were based on current review of arthroscopic images. This method was believed to be appropriately conservative, identifying only those injuries clearly defined on still images. An additional limitation was that the timing of preoperative MRI was not controlled as related to the date of injury. How this may have affected the presence of meniscal extrusion is unknown. Finally, the population was drawn from a pediatric sports referral center, and the patient mix and complexity of the cases have an unknown effect on the generalizability of the results for other populations.
With increasing youth sport activity, the prevalence of meniscal injury and associated root tears may be expected to increase. Although natural history studies on meniscal root treatment have not been reported, untreated posterior meniscal root injuries may result in loss of chondroprotective and stabilizing meniscal function. Our study provides large-sample data on the infrequently discussed injury of meniscal root tears in the pediatric and adolescent population. Although uncommon, these injuries may occur more frequently than previously expected. Ongoing preoperative joint line pain and the presence of meniscal extrusion may be clues that posterior meniscal root injuries are present. These injuries should be considered in the athletic pediatric or adolescent patient, as they may be amenable to repair and crucial to maintaining to longevity of the joint in the young athlete.
Conclusion
When treating a pediatric or adolescent patient for a traumatic meniscal tear, a surgeon may expect a posterior meniscal root injury with significant frequency, occurring in more than 1 in 6 patients in this cohort. The presence of an ACL injury should alert the provider to the possibility of a posterior lateral meniscal root injury, whereas contact and multiligament injuries may demonstrate associated posterior medial meniscal root avulsions. The presence of an extruded meniscus on MRI should alert the practitioner to the high possibility of a posterior meniscal root or a complex meniscal tear. In this cohort, 93% of the cases of MRI-demonstrated meniscal extrusion occurred in conjunction with a posterior meniscal root tear (68%) or a complex meniscal tear (25%). This information can provide the treating physician with improved ability to identify and treat injuries that otherwise may lead to rapid cartilage degenerative change. Treatment of a pediatric or adolescent knee injury should not inhibit the arthroscopist from consideration of a meniscal root injury based on age alone.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: P.L.W. receives royalties from Elsevier and has received educational support and hospitality payments from Pylant Medical. H.B.E. is a consultant for Smith & Nephew, receives royalties from Elsevier, has received educational support from Synthes and Pylant Medical, and has received hospitality payments from Sanofi-Aventis, Arthrex, and Pylant Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from University of Texas Southwestern Medical Center.
References
- 1. Bellisari G, Samora W, Klingele K. Meniscus tears in children. Sports Med Arthrosc. 2011;19(1):50–55. [DOI] [PubMed] [Google Scholar]
- 2. Bergin D, Hochberg H, Zoga AC, Qazi N, Parker L, Morrison WB. Indirect soft-tissue and osseous signs on knee MRI of surgically proven meniscal tears. AJR Am J Roentgenol. 2008;191(1):86–92. [DOI] [PubMed] [Google Scholar]
- 3. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. [DOI] [PubMed] [Google Scholar]
- 4. Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239(3):805–810. [DOI] [PubMed] [Google Scholar]
- 5. Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42–49. [DOI] [PubMed] [Google Scholar]
- 6. Forkel P, Herbort M, Sprenker F, et al. The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthroscopy. 2014;30(7):833–840. [DOI] [PubMed] [Google Scholar]
- 7. De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192(2):480–486. [DOI] [PubMed] [Google Scholar]
- 8. DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14(3):218–224. [DOI] [PubMed] [Google Scholar]
- 9. Feucht MJ, Bigdon S, Mehl J, et al. Risk factors for posterior lateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):140–145. [DOI] [PubMed] [Google Scholar]
- 10. Feucht MJ, Kuhle J, Bode G, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–1816. [DOI] [PubMed] [Google Scholar]
- 11. Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):112–118. [DOI] [PubMed] [Google Scholar]
- 12. Frank JM, Moatshe G, Brady AW, et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sports Med. 2017;5(6):2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Griffith CJ, LaPrade RF, Fritts HM, Morgan PM. Posterior root avulsion fracture of the medial meniscus in an adolescent female patient with surgical reattachment. Am J Sports Med. 2008;36(4):789–792. [DOI] [PubMed] [Google Scholar]
- 14. Hwang BY, Kim SJ, Lee SW, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–1610. [DOI] [PubMed] [Google Scholar]
- 15. LaPrade CM, Foad A, Smith SD, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43(4):912–920. [DOI] [PubMed] [Google Scholar]
- 16. LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. [DOI] [PubMed] [Google Scholar]
- 17. LaPrade CM, LaPrade MD, Turnbull TL, Wijdicks CA, LaPrade RF. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43(4):899–904. [DOI] [PubMed] [Google Scholar]
- 18. Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124–129. [DOI] [PubMed] [Google Scholar]
- 19. Matava MJ, Kim YM. Tibial avulsion fracture of the posterior root of the medial meniscus in a skeletally-immature child—a case report. Knee. 2011;18(1):62–65. [DOI] [PubMed] [Google Scholar]
- 20. Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127–3131. [DOI] [PubMed] [Google Scholar]
- 21. Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7(3):297–300. [DOI] [PubMed] [Google Scholar]
- 22. Pula DA, Femia RE, Marzo JM, Bisson LJ. Are root avulsions of the lateral meniscus associated with extrusion at the time of acute anterior cruciate ligament injury? A case control study. Am J Sports Med. 2014;42(1):173–176. [DOI] [PubMed] [Google Scholar]
- 23. Shieh A, Bastrom T, Roocroft J, Edmonds EW, Pennock AT. Meniscus tear patterns in relation to skeletal immaturity: children versus adolescents. Am J Sports Med. 2013;41(12):2779–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sonnery-Cottet B, Mortati R, Archbold P, Gadea F, Clechet J, Thaunat M. Root avulsion of the posterior horn of the medial meniscus in skeletally immature patients. Knee. 2014;21(6):1291–1296. [DOI] [PubMed] [Google Scholar]