Abstract
Background:
The preoperative diagnosis of hip microinstability is challenging. Although physical examination maneuvers and magnetic resonance imaging findings associated with microinstability have been described, there are limited reports of radiographic features. In patients with microinstability, we observed a high incidence of a steep drop-off on the lateral edge of the femoral head, which we have named the “cliff sign.”
Purpose:
(1) To determine the relationship of the cliff sign and associated measurements with intraoperative microinstability and (2) to determine the interobserver reliability of these measurements.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
A total of 115 consecutive patients who underwent hip arthroscopy were identified. Patients with prior hip surgery, Legg-Calve-Perthes disease, fractures, pigmented villonodular synovitis, or synovial chondromatosis were excluded, resulting in the inclusion of 96 patients in the study. A perfect circle around the femoral head was created on anteroposterior pelvis radiographs. If the lateral femoral head did not completely fill the perfect circle, it was considered a positive cliff sign. Five additional measurements relating to the cliff sign were calculated. The diagnosis of microinstability was made intraoperatively by the (1) amount of traction required to distract the hip, (2) lack of hip reduction after initial traction release following joint venting, or (3) intraoperative findings consistent with hip microinstability. Continuous variables were analyzed through use of unpaired t tests and discrete variables with Fisher exact tests. Interobserver reliability (n = 3) was determined for each measurement.
Results:
Overall, 89% (39/44) of patients with microinstability had a cliff sign, compared with 27% of patients (14/52) without instability (P < .0001). Conversely, 74% of patients with a cliff sign had microinstability, while only 12% of patients without a cliff sign had instability (P < .0001). In women younger than 32 years with a cliff sign, 100% (20/20) were diagnosed with instability. No differences were found in any of the 5 additional measurements. Excellent interobserver reliability was found for the presence of a cliff sign and the cliff angle measurement.
Conclusion:
We have identified a radiographic finding, the cliff sign, that is associated with the intraoperative diagnosis of hip microinstability and has excellent interobserver reliability. Results showed that 100% of young women with a cliff sign had intraoperative microinstability. The cliff sign may be useful in the preoperative diagnosis of hip microinstability.
Keywords: hip, arthroscopy, microinstability, radiographs, cliff sign
Hip microinstability has become an increasingly recognized cause of nonarthritic hip pain and disability in young patients.4–6,9–12,18,23,25,29–31 Known causes of hip microinstability include acetabular dysplasia, connective tissue disorders, macrotrauma, microtrauma, iatrogenic (postsurgical) factors, and idiopathic factors.12,13,16,19,20,25,29 Pathologic capsular laxity can lead to intra-articular injury and pain.23 Although several physical examination tests and magnetic resonance imaging (MRI) findings of microinstability have been described,9,12,14,17 the preoperative diagnosis remains challenging. Intraoperative assessment is a common method of confirming the diagnosis of hip microinstability.11,22,23 As good outcomes have been reported with arthroscopic treatment of hip microinstability,1,4–6,11,13,31 it would be beneficial to identify microinstability patients prior to surgery.
Radiographs are typically included in the preoperative evaluation of patients with hip pain. Acetabular dysplasia is a known cause of microinstability and can be diagnosed with anteroposterior (AP) radiographic measurements of the lateral center-edge angle (LCEA) of Wiberg (less than 20°-25°) and/or the acetabular roof inclination (Tönnis) angle greater than 10° as well as measurement of the anterior center-edge angle on the false profile view of Lequesne (less than 20°-25°).28 However, these radiographic angles have not been shown to effectively predict pathologic hip instability, especially in borderline dysplasia. The femoro-epiphyseal acetabular roof (FEAR) index was recently described to help distinguish between instability and femoroacetabular impingement as causes of pain in patients with borderline dysplasia.30 Other radiographic findings of hip microinstability are femoral head subluxation, broken Shenton line, and distal femoral neck sclerosis. However, none of these radiographic findings have been shown to be a reliable, independent predictor of pathologic hip microinstability.
We observed that many of our patients with hip microinstability had a common preoperative AP pelvis radiographic finding—a steep drop-off from a perfect circle (loss of sphericity) in the lateral femoral head (Figure 1). We termed this finding a “cliff sign.”
Figure 1.
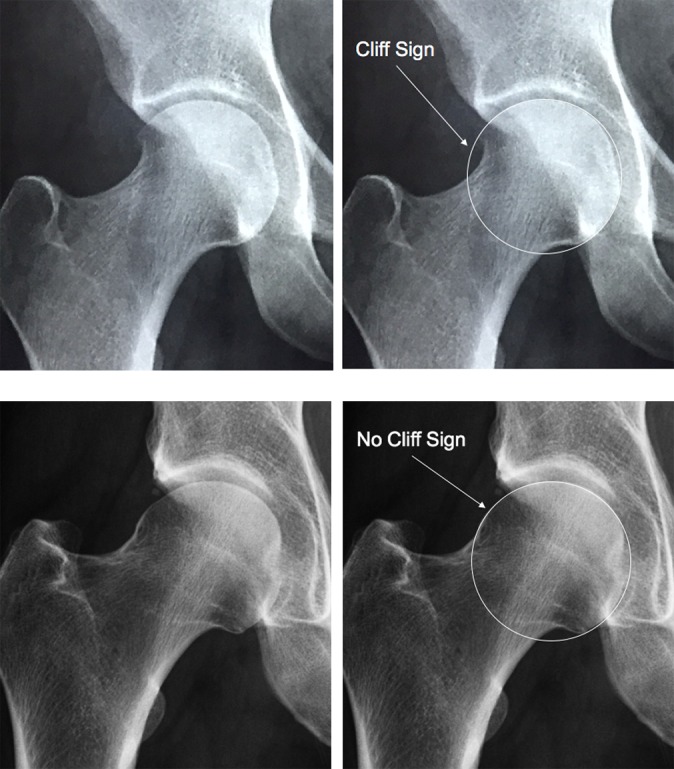
The cliff sign. A perfect circle is created around the femoral head. If the lateral femoral head does not completely fill the perfect circle, it is considered a positive cliff sign (top row). Also shown is a femoral head that does completely fill the perfect circle laterally and is considered a negative cliff sign (bottom row).
The primary objective of this study was to determine the relationship between the presence of a cliff sign and intraoperative confirmation of hip microinstability in a cohort of patients who underwent hip arthroscopy. A second objective was to quantify a cliff sign and determine the relationship between several measurements related to the cliff sign and hip microinstability. A third objective was to determine the interobserver reliability of the cliff sign and all associated measurements.
Methods
We identified 115 consecutive hip arthroscopy patients from the senior author’s (M.R.S.) practice between January 1, 2014, and November 15, 2014. All patients with a history of prior hip surgery, hip fracture, Legg-Calve-Perthes disease, pigmented villonodular synovitis, and synovial chondromatosis were excluded (n = 19). All patients who had hip arthroscopy had undergone a course of failed nonoperative treatment that included physical therapy and/or nonsteroidal anti-inflammatory drugs. Surgical indications included an acetabular labral tear (MRI), cartilage defect (MRI), femoroacetabular impingement (radiographs or MRI), and/or hip microinstability (based on the 6 provocative hip instability tests). An intra-articular diagnostic injection was performed in the majority of patients to confirm an intra-articular cause of the hip pain.
Therefore, 96 patients (47 women and 49 men) were included in the study (age range, 14-62 years; mean, 33 years). All patients had an LCEA greater than 20°. This study was approved by an institutional review board.
Standardized, preoperative AP pelvis radiographs were obtained for each patient and used for all measurements. Blinded, independent measurements were performed by 3 sports medicine fellowship–trained orthopaedic surgeons (J.D.P., J.B.C., B.J.R.). The operative hip was evaluated for the presence of a cliff sign by use of the following method: A perfect circle around the femoral head was created, and if the lateral femoral head did not completely fill the perfect circle, it was considered a positive cliff sign (Figure 1).
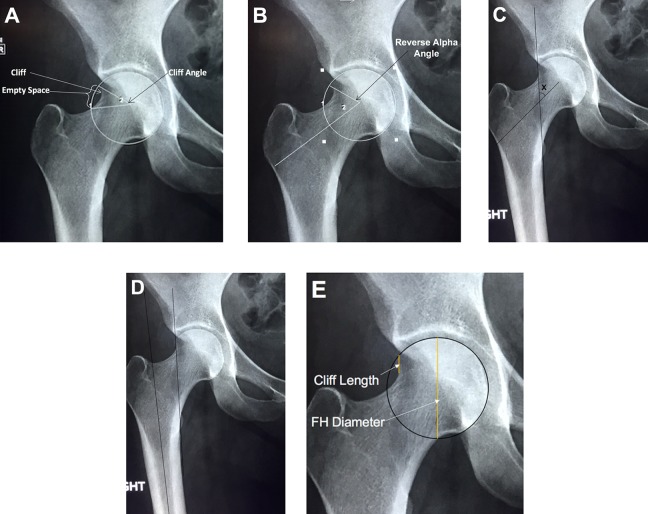
In the hips that had a positive cliff sign, 5 additional measurements were calculated to identify an objective measurement of the cliff (Centricity PACS; GE Healthcare): (1) cliff angle, (2) reverse alpha angle, (3) cliff/femoral neck Cobb angle, (4) cliff/femoral shaft Cobb angle, and (5) ratio of the length of the cliff to the femoral head diameter (Table 1 and Figure 2).
TABLE 1.
Cliff Sign Measurements
| Measurement | Method |
|---|---|
| Cliff angle (Figure 2A) | Angle of the lines formed from the center of the femoral head to the proximal and distal edge of the empty space. |
| Reverse alpha angle (Figure 2B) | Angle of the lines formed between the femoral neck axis and a line from the center of the femoral head to the proximal boundary where the femoral head leaves the perfect circle. |
| Cliff/femoral neck Cobb angle (Figure 2C) | Cobb angle between (1) the line parallel to the slope of the cliff and (2) the line along the axis of the femoral neck. |
| Cliff/femoral shaft Cobb angle (Figure 2D) | Cobb angle between (1) the line parallel to the slope of the cliff and (2) the line parallel to the femoral shaft. |
| Cliff length/femoral head diameter ratio (Figure 2E) | The ratio of the cliff length to the femoral head diameter. |
Figure 2.
Five additional measurements: (A) cliff angle; (B) reverse alpha angle; (C) cliff/femoral neck Cobb angle; (D) cliff/femoral shaft Cobb angle; (E) cliff length/femoral head (FH) diameter ratio.
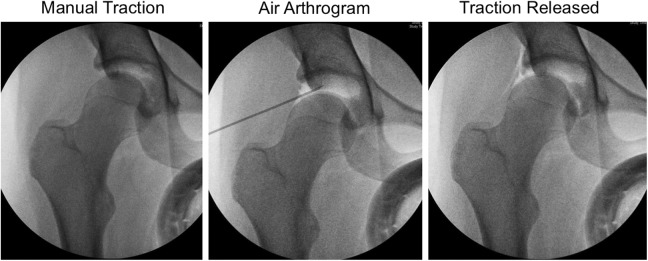
The operative reports were then reviewed for a diagnosis of microinstability, which was indicated by any of the following: (1) minimal traction required to distract the hip (often just manual traction by the senior author) after the administration of general anesthesia and muscular paralysis; (2) lack of hip reduction after release of negative intra-articular pressure and traction prior to the start of hip arthroscopy; or (3) intraoperative findings of microinstability such as straight anterior or straight lateral labral tears23 (Figure 3). A capsular plication was performed in all patients who were intraoperatively diagnosed with hip microinstability (n = 44).
Figure 3.
Intraoperative fluoroscopy images of a patient with microinstability. The hip is distracted with only manual traction (left). After an air arthrogram (middle), the hip remains subluxated after traction is released (right).
Statistics
Continuous variables were compared with unpaired t tests. Discrete variables were compared with both the chi-square and Fisher exact tests. Interobserver reliability was determined with Fleiss kappa for discrete variables and intraclass correlation (ICC) for continuous variables. ICC values were considered as excellent (>0.75), fair to good (0.40-0.75), and poor (<0.40).7,24
Results
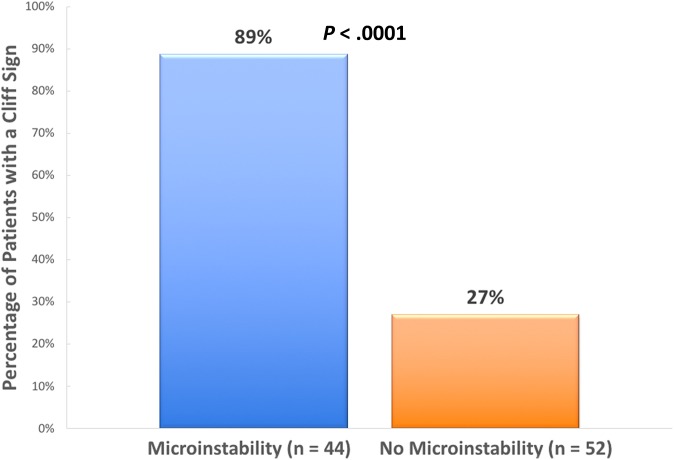
Overall, 44 of 96 (46%) patients were diagnosed intraoperatively with microinstability, and 52 patients did not have microinstability. We found that 89% of patients with microinstability had a cliff sign, whereas only 27% of patients without microinstability had a cliff sign (P < .0001) (Figure 4). When patients with and without a cliff sign were compared, 74% of patients with a cliff sign had microinstability, whereas only 12% of patients without a cliff sign had microinstability (P < .0001) (Table 2 and Figure 5).
Figure 4.
Graph comparing the percentages of patients with a cliff sign for the group of patients with microinstability and the group without microinstability.
TABLE 2.
Cliff Sign Versus Microinstability Resultsa
| Patients With | Microinstability | No Microinstability | Total |
|---|---|---|---|
| Positive cliff sign | 39 (74%) | 14 (26%) | 53 |
| Negative cliff sign | 5 (12%) | 38 (88%) | 43 |
aCliff sign sensitivity = 89% and specificity = 73%.
Figure 5.
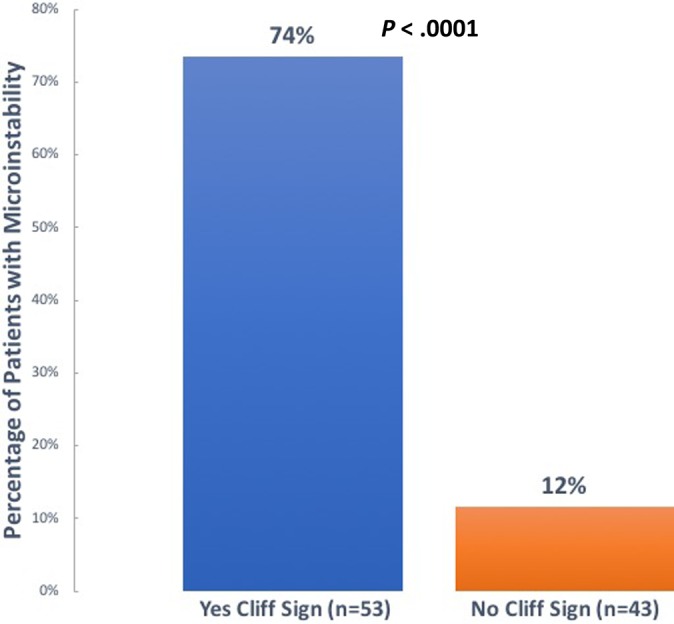
Graph comparing the percentages of patients with microinstability in the groups with positive and negative cliff sign.
The mean age was 31.4 ± 10.9 years for the patients who had microinstability compared with 35.9 ± 12.9 years for the patients without microinstability (P = .066). In the group of women younger than 32 years who had a cliff sign, 20 of 20 (100%) also had microinstability. No significant differences were found between patients with microinstability and those without microinstability in terms of cliff sign measures of cliff angle, reverse alpha angle, cliff/femoral neck Cobb angle, cliff/femoral shaft Cobb angle, and ratio of the length of the cliff to the femoral head diameter (Table 3).
TABLE 3.
Cliff Sign Measurement Results and Interobserver Reliabilitya
| Measurement | Patients With Microinstability | Patients Without Microinstability | P Value | Interobserver Reliability (n = 3) |
|---|---|---|---|---|
| Cliff sign, % | 89 | 27 | <.0001 | 0.81 (excellent) |
| Cliff angle, deg | 37.0 ± 11.7 | 34.8 ± 9.1 | .54 | 0.84 (excellent) |
| Reverse alpha angle, deg | 72.1 ± 12.0 | 73.5 ± 8.5 | .70 | 0.71 (good) |
| Cliff/femoral neck Cobb angle, deg | 45.3 ± 11.0 | 40.5 ± 8.0 | .14 | 0.16 (poor) |
| Cliff/femoral shaft Cobb angle, deg | 5.2 ± 9.7 | 6.4 ± 7.6 | .67 | –0.31 (poor) |
| Cliff length/femoral head diameter ratio | 0.17 ± 0.07 | 0.17 ± 0.09 | .98 | 0.31 (poor) |
aBolded value indicates statistical significance.
Excellent interobserver reliability was found for the presence of a cliff sign (κ = 0.81) and the cliff angle measurement (ICC = 0.84). The interobserver reliability was good in the reverse alpha angle measurement (ICC = 0.71) but poor in the cliff/femoral neck Cobb angle (ICC = 0.16), cliff/femoral shaft Cobb angle (ICC = –0.31), and cliff length/femoral head diameter ratio measurements (ICC = 0.31). The results are summarized in Table 3.
Discussion
In recent years, there has been an improved awareness of hip microinstability as a common cause of nonarthritic hip pain in young, active individuals. Many factors are known to cause hip microinstability, including bony abnormalities such as acetabular dysplasia, connective tissue disorders, macrotrauma, microtrauma, and iatrogenic and idiopathic causes.12,13,16,19,20,25,29 Although the bone structure of the femoroacetabular joint is important in stability, soft tissue structures also have a significant stabilizing role.3,12,15,27 Hip capsuloligamentous thickenings make up 60% of the hip capsule, most notably the iliofemoral, pubofemoral, and ischiofemoral ligaments.8,26 When these ligaments and the capsule are stretched or torn, pathologic capsular laxity can lead to excessive femoral head movement within the acetabulum, resulting in intra-articular injury and pain.23
In normal hip range of motion, the center of the femoral head moves relative to the center of the acetabulum. Safran et al21 demonstrated in a cadaveric model that the femoral head translates a mean of 3.4 mm in the medial-lateral plane, 1.5 mm in the anterior-posterior plane, and 1.5 mm in the proximal-distal plane. Additionally, radiographic and MRI studies of asymptomatic professional ballet dancers have demonstrated micromotion of the femoral head on the acetabulum in the splits position.2,18
In the absence of significant dysplasia or connective tissue disorders, the diagnosis of hip microinstability can be challenging because the majority of patients will complain of deep groin pain and not hip instability.12,25 A high degree of suspicion is necessary to make the diagnosis of hip microinstability. Certainly, making the diagnosis of microinstability is critical to formulating an appropriate treatment plan for the patient. Knowledge of the correct diagnosis of microinstability preoperatively will also help in surgical planning. Many believe that the Beighton signs of generalized ligamentous laxity may correlate with the risk of hip microinstability, although this is not proven. In addition to the Beighton signs, the following 6 provocative hip microinstability tests are commonly performed during the physical examination9,12: (1) anterior apprehension test, (2) prone external rotation test, (3) abduction-extension–external rotation test, (4) posterior apprehension test, (5) log roll test, and (6) axial distraction test. In a recent study, we found that if the first 3 of these tests are positive, there is a 95% likelihood that the patient will have intraoperative confirmation of hip microinstability.9
It is important to identify hip microinstability in patients because surgical treatments such as capsular plication can be effective.1,4–6,10,11,13,31 As the history and physical examination may be unreliable in patients who have microinstability, there is a need for objective imaging findings. Several groups have investigated the role of magnetic resonance arthrography in the diagnosis of hip microinstability. Postoperative capsular defects may be present, suggesting an iatrogenic cause of hip microinstability.14,17 Other magnetic resonance arthrography findings that have been associated with microinstability are anterior hip joint recess widening (>5 mm), anterior hip capsular thinning (<3 mm), and a crescent-shaped accumulation of contrast in the posterior-inferior joint on 2 or more planes.14,30
Unfortunately, radiographic findings have not been shown to correlate well with clinical hip microinstability. Acetabular dysplasia can be diagnosed with LCEA, anterior center-edge angle, and Tönnis angles; however, the clinical significance of these measurements has been controversial. Wyatt and colleagues30 investigated a group of patients with borderline dysplasia (LCEA, 20°-25°) to determine whether instability or femoroacetabular impingement was the primary cause of symptoms. The investigators created a radiographic tool called the FEAR index to distinguish between these 2 groups. Wyatt et al30 found that if a patient presented with hip pain and borderline dysplasia, a FEAR index less than 5° indicated an 80% probability that the hip was stable.
In the current study, we report a new radiographic finding, the cliff sign, which we found to be associated with the intraoperative confirmation of hip microinstability. Among the patients in our cohort, 74% with a positive cliff sign had microinstability, while 12% with a negative cliff sign had microinstability. All 20 women younger than 32 years who had a cliff sign also had microinstability. The cliff sign can be a valuable tool in the preoperative assessment of hip microinstability. It is a reproducible and easily measured radiographic finding that had excellent interobserver reliability in our cohort of 96 patients. AP pelvis radiographs are routinely included in the outpatient workup of hip pain, so additional images are not necessary. We also studied several other measurements related to the cliff sign; however, we found no significant differences between the measurements in patients with microinstability and those patients without microinstability. It is possible that our study was underpowered to detect any of these differences. The only additional measurement that had an excellent interobserver reliability was the cliff angle.
Our study had several important limitations. The study population consisted of a cohort of a single surgeon’s hip arthroscopy patients, and the diagnosis of hip microinstability was a subjective intraoperative evaluation. However, to our knowledge, this is the most reliable method of diagnosing hip microinstability.11,22,23 The senior author has a large referral source for patients with microinstability and therefore may treat a higher percentage of microinstability patients than is found in the average population. Another limitation is that this was a retrospective study and therefore lacked a control group. It is important to recognize that this study reported on the association of the cliff sign with hip microinstability. Therefore, it is not known whether the femoral head morphologic status of patients with the cliff sign is an independent cause of hip microinstability. Future prospective studies are warranted to determine whether the cliff sign is valuable in predicting microinstability. We attempted to eliminate bias by including 3 independent reviewers who were blinded to the microinstability diagnosis.
Conclusion
The cliff sign is a radiographic finding that is associated with intraoperative hip microinstability. The cliff sign and cliff angle (a measure of the magnitude of the cliff sign) measurements have excellent interobserver reliability. In our surgical cohort, all young women with a cliff sign on preoperative radiographs were diagnosed with hip microinstability. The cliff sign may be useful in the preoperative diagnosis of hip microinstability.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.D.P. has received educational support from Supreme Orthopedic Systems, Smith & Nephew, and Arthrex and has received hospitality payments from Smith & Nephew. J.B.C. has grants/grants pending from Linvatec and has received hospitality payments from Smith & Nephew. B.J.R. has received educational support from Smith & Nephew. M.R.S. receives royalties from Smith & Nephew; is a consultant for Smith & Nephew, Ferring Pharmaceuticals, Linvatec, and Medacta; has received hospitality payments from Smith & Nephew, Ferring Pharmaceuticals, and Medacta; is a paid speaker/presenter for Smith & Nephew; has received educational support from Biomet; and has received honoraria from Medacta. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Stanford University (protocol No. 33119).
References
- 1. Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011;27(12):1720–1731. [DOI] [PubMed] [Google Scholar]
- 2. Charbonnier C, Kolo FC, Duthon VB, et al. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011;39(3):557–566. [DOI] [PubMed] [Google Scholar]
- 3. Domb BG, Martin DE, Botser IB. Risk factors for ligamentum teres tears. Arthroscopy. 2013;29(1):64–73. [DOI] [PubMed] [Google Scholar]
- 4. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29(1):162–173. [DOI] [PubMed] [Google Scholar]
- 5. Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41(11):2591–2598. [DOI] [PubMed] [Google Scholar]
- 6. Ekhtiari S, de Sa D, Haldane CE, et al. Hip arthroscopic capsulotomy techniques and capsular management strategies: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):9–23. [DOI] [PubMed] [Google Scholar]
- 7. Fleiss J. The Design and Analysis of Clinical Experiments. New York, NY: John Wiley & Sons; 1986. [Google Scholar]
- 8. Hewitt JD, Glisson RR, Guilak F, Vail TP. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002;17(1):82–89. [DOI] [PubMed] [Google Scholar]
- 9. Hoppe DJ, Truntzer JN, Shapiro LM, Abrams GD, Safran MR. Diagnostic accuracy of 3 physical examination tests in the assessment of hip microinstability. Orthop J Sports Med. 2017;5(11):2325967117740121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jackson TJ, Peterson AB, Akeda M, et al. Biomechanical effects of capsular shift in the treatment of hip microinstability: creation and testing of a novel hip instability model. Am J Sports Med. 2016;44(3):689–695. [DOI] [PubMed] [Google Scholar]
- 11. Kalisvaart MM, Safran MR. Hip instability treated with arthroscopic capsular plication. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):24–30. [DOI] [PubMed] [Google Scholar]
- 12. Kalisvaart MM, Safran MR. Microinstability of the hip—it does exist: etiology, diagnosis and treatment. J Hip Preserv Surg. 2015;2(2):123–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Larson CM, Stone RM, Grossi EF, Giveans MR, Cornelsen GD. Ehlers-Danlos syndrome: arthroscopic management for extreme soft-tissue hip instability. Arthroscopy. 2015;31(12):2287–2294. [DOI] [PubMed] [Google Scholar]
- 14. Magerkurth O, Jacobson JA, Morag Y, Caoili E, Fessell D, Sekiya JK. Capsular laxity of the hip: findings at magnetic resonance arthrography. Arthroscopy. 2013;29(10):1615–1622. [DOI] [PubMed] [Google Scholar]
- 15. Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24(2):188–195. [DOI] [PubMed] [Google Scholar]
- 16. Martin RL, Kivlan BR, Clemente FR. A cadaveric model for ligamentum teres function: a pilot study. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1689–1693. [DOI] [PubMed] [Google Scholar]
- 17. McCormick F, Slikker W III, Harris JD, et al. Evidence of capsular defect following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):902–905. [DOI] [PubMed] [Google Scholar]
- 18. Mitchell RJ, Gerrie BJ, McCulloch PC, et al. Radiographic evidence of hip microinstability in elite ballet. Arthroscopy. 2016;32(6):1038–1044. [DOI] [PubMed] [Google Scholar]
- 19. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(suppl):85S–91S. [DOI] [PubMed] [Google Scholar]
- 20. Philippon MJ, Rasmussen MT, Turnbull TL, et al. Structural properties of the native ligamentum teres. Orthop J Sports Med. 2014;2(12):2325967114561962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Safran MR, Lopomo N, Zaffagnini S, et al. In vitro analysis of peri-articular soft tissues passive constraining effect on hip kinematics and joint stability. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1655–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shibata KR, Matsuda S, Safran MR. Arthroscopic hip surgery in the elite athlete: comparison of female and male competitive athletes. Am J Sports Med. 2017;45(8):1730–1739. [DOI] [PubMed] [Google Scholar]
- 23. Shibata KR, Matsuda S, Safran MR. Is there a distinct pattern to the acetabular labrum and articular cartilage damage in the non-dysplastic hip with instability? Knee Surg Sports Traumatol Arthrosc. 2017;25(1):84–93. [DOI] [PubMed] [Google Scholar]
- 24. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. [DOI] [PubMed] [Google Scholar]
- 25. Shu B, Safran MR. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30(2):349–367. [DOI] [PubMed] [Google Scholar]
- 26. Telleria JJ, Lindsey DP, Giori NJ, Safran MR. An anatomic arthroscopic description of the hip capsular ligaments for the hip arthroscopist. Arthroscopy. 2011;27(5):628–636. [DOI] [PubMed] [Google Scholar]
- 27. van Arkel RJ, Amis AA, Cobb JP, Jeffers JR. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres: an experimental study. Bone Joint J. 2015;97(4):484–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wilkin GP, Ibrahim MM, Smit KM, Beaule PE. A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplasty. 2017;32(suppl 9):S20–S27. [DOI] [PubMed] [Google Scholar]
- 29. Wuerz TH, Song SH, Grzybowski JS, et al. Capsulotomy size affects hip joint kinematic stability. Arthroscopy. 2016;32(8):1571–1580. [DOI] [PubMed] [Google Scholar]
- 30. Wyatt M, Weidner J, Pfluger D, Beck M. The femoro-epiphyseal acetabular roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia? Clin Orthop Relat Res. 2017;475(3):861–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wylie JD, Beckmann JT, Maak TG, Aoki SK. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44(1):39–45. [DOI] [PubMed] [Google Scholar]