Abstract
Background:
Cervical pedicle screw fixation through posterior approach has shown greater cervical stability advantage. The cervical pedicle screw fixation technique through posterior approach is demanding. The key to the technique is the choice of point and angle of screw entrance. The angle of screw placement is variable. Morphometric measurements of the cervical pedicle are a prerequisite for individualized screw. CT imaging has become the most reliable and important means to obtain cervical pedicle's measurement data and morphology in vivo. This study explores the feasibility and application of precise in vivo measurements by multi-slice computed tomography (MSCT) for individualized cervical transpedicular screw placement at C3–C7 in Chinese healthy population.
Materials and Methods:
80 adults who underwent cervical examination by enhanced and nonenhanced computed tomography angiography, respectively, were selected and submitted to bone algorithm reconstruction for slice thickness and interval of 0.75 mm to acquire clear images and detailed bone structures. Simulation of individualized screw placement was performed with a 4.0 mm diameter screw with the help of postprocessing workstation. Pedicle transverse angle (PTA) and sagittal angle (PSA) were measured using the single- and double-line methods (analog nailing, 4.0 mm in diameter) in 160 pairs of C3–C7 pedicles, setting positive and negative values for cranial direction and foot side PSAs, respectively. Comparison of the measured change scope in PTA and PSA between the two methods was carried out; the range was defined as the error range.
Results:
Significantly, different results (P < 0.05) were obtained between the single- and double-line methods in the error ranges of PTA and PSA in C3–C7 pedicles. Interestingly, the double-line method was better in simulating the actual needs of individualized nailing. The mean values of PTA and PSA were 42.9°, 45.5°, 42.4°, 37.1°, 29.0° and 8.4°, 5.0°, −4.0°, and −7.8°, −8.1°, respectively, with the double-line method.
Conclusion:
MSCT reconstruction techniques can determine the direction and required parameters for individualized screw placement. In addition, accurate in vivo measurements of PTA and PSA, particularly PSA, provide the orthopedic surgeon with theoretical guidance and reliable basis in screw placement.
Keywords: Cervical spine, pedicle, screw, X-ray, computed tomography, measurement
MeSH terms: Computer tomography, x-rays, cervical vertebrae, bone screws
Introduction
Since Abumi et al.1 first applied the transpedicular screw placement technique for the lower cervical vertebra, cervical pedicle screw fixation through posterior approach has shown greater cervical stability advantage compared with any other cervical fixation system.2,3,4 The indications for cervical pedicle screw have since been extended and now include conditions such as trauma, rheumatoid arthritis, degenerative disease, spondylolysis, and spinal tumor, etc.5,6 It is considered that the cervical pedicle screw placement is most probably going to be the gold standard for cervical spinal fixation.7 The cervical pedicle screw fixation technique through posterior approach is demanding and involves fixation of a steel plate and screw into the vertebral body through the cervical pedicle. Therefore, the key to the technique is the choice of point and angle of screw entrance.5 Abumi and Kaneda8 placed the screw slightly outside the midpoint of the articular process, close to the lower edge of the inferior articular process. The angle of screw placement is variable depending on different segments of vertebral bodies. Due to the interindividual variations of pedicle morphology,9,10,11 application of individualized screw placement should be emphasized.12 It is worthwhile noting that morphometric measurements of the cervical pedicle as well as the correlation between the pedicle and its surrounding structures are a prerequisite for individualized screw placement. Initially, dried bone samples and X-ray images were mainly used for measuring the cervical vertebra. With its development, computed tomography (CT) has been increasingly employed to measure and study the morphology of cervical vertebras; particularly, multislice spiral CT scans can clearly reveal fine structures of the vertebral body, disc, and accessories. Moreover, highly precise three-dimensional (3D) reconstruction images can be naturally obtained in living tissues; this can help keep various tissues and relevant anatomy intact.12 Currently, CT imaging has become the most reliable and important means to obtain cervical pedicle's measurement data and morphology in vivo.10,11,13,14 However, to date, studies assessing preoperative simulation of screw entry using individualized pedicle screw placement are scarce in the measurement with the double-line method. Specifically, a few reports have been published regarding in vivo measurements of the sagittal angle formed between the cervical pedicle and corresponding vertebral body. This study generates 3D reconstruction of in vivo simulation of individualized cervical pedicle screw placement using volumetric CT scanning data, to obtain reliable data of entry angle of the pedicle screw.
Materials and Methods
CT imaging data were collected from eighty healthy adult Chinese patients receiving cervical enhanced CT angiography and plain neck imaging examination from January 2012 to April 2015. The informed consent was obtained for every patient before CT examination. They included 44 males and 36 females, average age was 49.7 years (range 18-75 years). Inclusion criteria were as follows: (1) no spinal deformity (except congenital block vertebra), fracture of the vertebral body/accessories, or vertebral dislocation/spondylolisthesis; (2) no reversal of vertebral column's physiological curvature, scoliosis, or vertebral sequence instability; (3) no pathological tumor changes such as bone damage or metastasis of the vertebras or small joints; (4) no obvious lumps or mass surrounding the cervical vertebra.
The study complied with the current laws of our country and regulations of the institute. At the same time, all process was permitted by local ethics committee.
Computed tomography imaging systems and scanning methods
Dual-source spiral 64-slice CT scanner (SIMENS SOMATON, Germany) was used with the patients in supine position. Scanning parameters were 3 mm slice thickness/0.75 mm interval, with a pitch of 1.0–2.0. Reconstruction parameters were 0.75 mm slice thickness/interval and bone reconstruction algorithm (convolution: 80). The tube voltage was 120 kV and the current was auto-regulated. Scanning was performed from the saddle area of the cranial base to the level of the sternal angle.
Postscanning processing and measurement methods
All raw data obtained from patients were stored in postprocessing workstation for 3D reconstructions. Siemens Syngo software workstation was employed for random postscanning imaging processing. Accuracy values of distance and angle measurements were 0.1 mm and 0.1°, respectively. Using the dedicated software (InSpace) of imaging postprocessing workstation, shade surface display, and multi-plane reconstruction (MPR) was carried out to obtain transverse sections perpendicular to the pedicle isthmus [Figure 1]. Initially, morphology, structures, and development of bone cortex in different vertebral bodies and pedicles were observed. Then, in 160 pairs of C3–C7 pedicles, the single-and double-line (Figure 1; diameter of mimicked screw is 4.0 mm) measurement methods were employed to assess the horizontal angle between the pedicle's central axis and the sagittal plane (pedicle transverse angle, [PTA]), and sagittal angle between the pedicle's central axis and the horizontal plane of the corresponding vertebra (pedicle sagittal angle, [PSA]). The PSA values obtained at the cranial and caudal sides were defined as positive and negative values, respectively [Figure 2]. Comparison of the measured change scope in PTA and PSA between the two methods was carried out; the range was defined as the error range.
Figure 1.
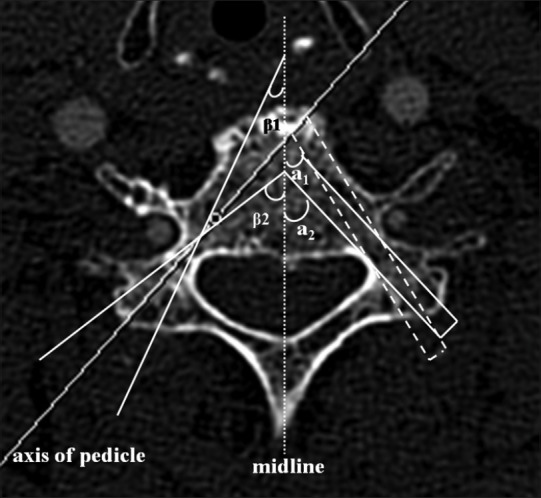
Axial computed tomography images of the third cervical pedicle (C3) in a 74-year-old woman. The image shows the schematic diagram of pedicle transverse angles of C3 measured with the single line method and with the double-line method (analog nailing, 4.0 mm in diameter), respectively. In the diagram, a1 (or β1) and a2 (or β2) mean the minimum and maximum angles, respectively. Pedicle transverse angle values measured with single-line method shows a greater error range, and the accuracy is poor which does not meet the requirements of clinical practice in pedicle screw placement. While pedicle transverse angle values obtained with the parallel double-line measurement approach (i.e., double-line mimics the pathway of screw entry) could be more accurate and reliable, and the error range is significantly reduced, so the technique is more feasible for clinical operation
Figure 2.

Computed tomography reconstruction of Cervical oblique-sagittal image by multi-plane reconstruction. The dashed and dotted lines represent the corresponding vertebral horizontal level and the pathway of screw entry, respectively. a means the pedicle sagittal angle value of C3 obtained at the cranial side, so it's defined as positive value. -a means the pedicle sagittal angle value of C7 obtained at the caudal side, so it's defined as negative value
Statistical analysis
The SPSS 13.0 software (SPSS for Windows, version 13.0; Chicago, IL, USA) was used for statistical analysis; paired t-test was used to assess values at the same vertebral level, and Kendall test was employed for different vertebral levels. P < 0.01 was considered to be statistically significant.
Results
Congenital vertebral fusion (block vertebra) was found in 2 of the 80 patients and involved fusion of 4 vertebral bodies; one patient had a congenital vertebral cortical bone defect.
Average error ranges of PTA and PSA in C3–C7 using the single- and double-line measurement methods are shown in Table 1. Statistically significant differences were correspondingly found in the two measurements (t- test, P < 0.01). The error range obtained using the single line measurement method was relatively large while double-line measurement mimicked screw placement and was more accurate and suitable for clinical screw placement [Figure 1].
Table 1.
Average error ranges of pedicle transverse angle and pedicle sagittal angle in C3-C7 with different measurement methods (x̄±S°) (n=160)
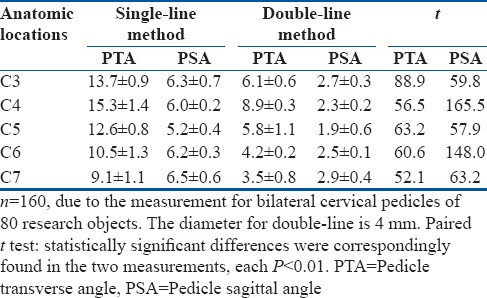
Combination of MPR and InSpace successfully yielded accurate PTA and PSA measurements of C3–C7 cervical pedicles using the double-line method. Mean PTA values were of 42.9°, 45.5°, 42.4°, 37.1°, and 29.0°, respectively [Table 2]; mean PSA values were 8.4°, 5.0°, −4.0°, −7.8° and -8.1°, respectively [Table 2], which were similar to the “negative linear slope” [Figure 3]. No significant differences in gender and other parameters displayed on the right or left side of the x-axis were observed (Paired t-test, P > 0.01); however, a significant difference was found in PTA and PSA measurements at different vertebral levels (Kendall test, P < 0.01) [Table 2].
Table 2.
Pedicle transverse angle and pedicle sagittal angle measurements of cervical pedicles using double-line method in different gender and side (x̄±S°)
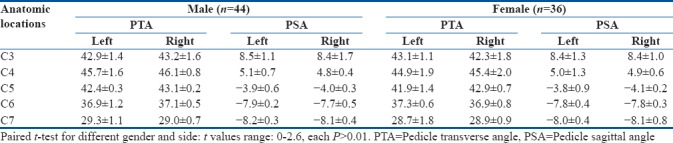
Figure 3.
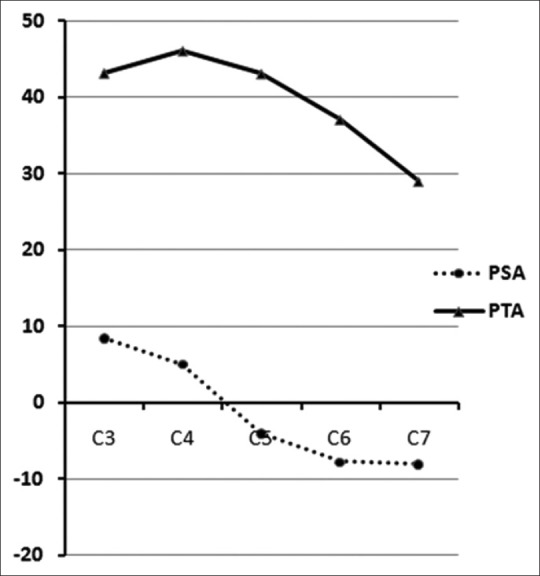
Trend chart for pedicle sagittal angle and pedicle transverse angle of C3–C7. It reveals that the pedicle sagittal angle of C5–C7 shows negative value, suggesting that the nailing direction should be inclined to caudal side. The characteristic trend for pedicle sagittal angle from C3 to C7 demonstrates a large change with a sharply negative linear slope, yielding a probably higher clinical value than that of pedicle transverse angle, which should be more alert in practice
Discussion
Cervical pedicles have greater variations and more complicated anatomical structures than the thoracic and lumbar vertebral arches. Therefore, cervical pedicle screw placement is prone to cause bone cortex perforation and complications. Munusamy et al.11 suggested the individualized screw placement method, that is, preoperative imaging examination should be routinely performed in order to obtain 3D quantitative anatomic data for safety and accuracy of cervical pedicle screw placement; the recorded data include anterior and posterior diameters of the spinal canal, transverse diameter, length, and horizontal angle of the cervical pedicles. Based on these data and the principle of individualized treatment, screws with suitable length and diameter are selected for screw placement. It is widely accepted that imaging measurements are a more accurate initial assessment of suitability for screw insertion in obtaining an effective and reliable data.15,16 Meanwhile, individualized cervical pedicle measurement is a must and a reliable technique for pedicle screw fixation;11 however, how to apply preoperative data to make accurate screw placement intraoperatively remains a problem that needs to be overcome by further quantifying a series of parameters; particularly, the preoperative measurement of screw's entry angle is a critical issue. Theoretically, individualized screw placement is an ideal method to circumvent the problem posed by variations of the cervical pedicles: the entry point and direction of the screw depend on measurement results of each pedicle preoperatively.11,14 Obviously, accurate imaging measurement is advantageous in providing data in a noninvasive, more informative and safer manner compared with those obtained through intraoperative exploration. Based on published reports,14,15,17,18,19,20 successful pedicle screw replacement is mainly dependent on the following three aspects: (1) determination of screw placement's entry point, which is usually easy to select according to anatomical structures; (2) the angle of the screw at 3D level is used for placement, i.e., data obtained using concise PTA and PSA measurements; (3) suitable screw diameter and length. Therefore, the pedicle screw placement technique is feasible for individualization and precision as long as it meets all requirements mentioned above. Up to date, multi-slice CT (MSCT) is the most important and reliable measurement means for preoperative cervical pedicle placement.11,13,14,15,16 In the study, MSCT data revealed that normal variations occurred in 3 cases (congenital block vertebra and unilateral pedicle cortex defect in 2 and 1 cases, respectively), suggesting anatomical variations of the cervical pedicle. Thus, individualized measurements are critical to achieve individualized screw placement.
It should first be mentioned that PTAs of C3–C7 pedicles, the angle between the pedicle's longitudinal axis at the transverse section and midline, has been reported in a few studies.11,18 The measurements results could be slightly variable due to sample size and different methods used. Nevertheless, data from these studies are generally similar; specifically, the rule of angle changes of C3–C7 is basically the same, that is, the largest angle was usually in C4, approximately 45°, with the angle, gradually decreased at lower vertebral levels, and smallest value found at C7 [Figure 3]. Moreover, no evidence was found for an association of the angle change with gender and side (right or left), which is consistent with a previous report.19 However, the C5–C7 pedicle's angle in the present study is smaller than reported values.11,14,20 It is possible that we used the parallel double-line measurement approach (i.e., double-line mimics the pathway of screw entry) instead of the single-line measurement method (i.e., axis of the pedicle), which could effectively avoid impact of human factors on measurement errors caused by the single-line measurement method used for the determination of the pedicle axis. The study data should be more accurate and reliable, and the technique is more feasible for clinical operation because the average error ranges of PTA and PSA in C3–C7 with the double-line method are much less than those with single-line method [Table 1].
Second, the measurement of the pedicle's PSA (upward or downward angle between the sagittal plane and longitudinal pedicle axis) is rarely reported in the literature.20,21 It is possible that the 3D nature of the pedicle and its irregularity make it difficult to precisely measure at 2D level in wet-dry samples or living subjects.18 In the present study, modern volumetric CT scanning and 3D reconstruction algorithm combined with a special software were applied to successfully measure the sagittal angle with double-line simulation of the screw. Interestingly, we found the change rules of angular measurements for C3–C7; for example, the sagittal angle measured as the longitudinal pedicle axis pointing to the superior vertebral endplate was considered the positive value, whereas that obtained as the longitudinal pedicle axis pointing to the inferior vertebral endplate was considered the negative value. PSA values of C3–C7 were 8.4°, 5.0°, −4.0°, −7.8°, and −8.1°, respectively, similar to the “negative linear slope” [Figure 3]. No similar data and changes have been reported previously; nevertheless, in this study, individualized screw placement was performed taking into account the screw diameters, and PTA and PSA measurements using the double-line method can, respectively, determine transverse and sagittal angles of screw entry. These techniques provide higher reference values and have greater clinical significance: they should become the most likely gold standard of in vivo measurements, which will provide reliable evidence for training orthopedic surgeons to obtain “freehand skills and tactile sensation experience of screw insertion” and 3D computerized image-guided navigation system for screw placement.5,22 For example, the average in vivo measuring error ranges of either PTA or PSA in C3–C7 using double-line method are superior to those with the single-line method, which may provide the orthopedic surgeon with theoretical guidance and reliable basis in screw placement. More importantly, the same CT images will be transmitted to 3D computerized image-guided navigation system, and hence, the same surgeons in vivo trained for CT measuring with the double-line method will be more familiar, skilled, and confident in the operation of 3D navigation system.
In summary, preoperative MSCT reconstruction techniques can determine the direction and required parameters for individualized screw placement; it mimics operation to make precise measurements of key parameters such as PTA and PSA. Precise PTA and PSA measurements using the double-line method provide theoretical guidance for preoperative simulation of individualized pedicle screw placement; particularly, for the first time, in vivo PSA measurement was shown to provide reliable evidence for training orthopedic surgeon to obtain “freehand skills and tactile sensation experience of screw insertion” and 3D computerized image-guided navigation system for screw placement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported by grants from the National Natural Science Foundation of China (No. 81101043), by 333 High-level Talents Training Project of Jiangsu (No. 2016III-0603), Six-one Project of Top Talents in Jiangsu Province (LGY2017015) and by Youth Talents Program of Science-education Rejuvenating Healthy in Jiangsu Provincial Commission of Health and Family Planning (No. QNRC 2016181), National Key R&D Program of China (2017YFC0114300).
Conflicts of interest
There are no conflicts of interest.
References
- 1.Abumi K, Itoh H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: Description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 2.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976) 1997;22:977–82. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 3.Nakamura C, Kawaguchi Y, Ishihara H, Sainoh H, Kimura T. Upper thoracic myelopathy caused by vertebral collapse and subluxation in rheumatoid arthritis: Report of two cases. J Orthop Sci. 2004;9:629–34. doi: 10.1007/s00776-004-0827-y. [DOI] [PubMed] [Google Scholar]
- 4.Gaines RW., Jr The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82-A:1458–76. doi: 10.2106/00004623-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC. The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: A series of 45 consecutive patients. Spine (Phila Pa 1976) 2014;39:280–5. doi: 10.1097/BRS.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 6.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ, et al. Placement of pedicle screws in the human cadaveric cervical spine: Comparative accuracy of three techniques. Spine (Phila Pa 1976) 2000;25:1655–67. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 7.Yusof MI, Ming LK, Abdullah MS, Yusof AH. Computerized tomographic measurement of the cervical pedicles diameter in a Malaysian population and the feasibility for transpedicular fixation. Spine (Phila Pa 1976) 2006;31:E221–4. doi: 10.1097/01.brs.0000210263.87578.65. [DOI] [PubMed] [Google Scholar]
- 8.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1997;22:1853–63. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Karaikovic EE, Daubs MD, Madsen RW, Gaines RW., Jr Morphologic characteristics of human cervical pedicles. Spine (Phila Pa 1976) 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 10.Kato S, Shoda N, Chikuda H, Seichi A, Takeshita K. Morphological characteristics of cervical spine in patients with athetoid cerebral palsy and the accuracy of pedicle screw placement. Spine (Phila Pa 1976) 2014;39:E508–13. doi: 10.1097/BRS.0000000000000234. [DOI] [PubMed] [Google Scholar]
- 11.Munusamy T, Thien A, Anthony MG, Bakthavachalam R, Dinesh SK. Computed tomographic morphometric analysis of cervical pedicles in a multi-ethnic Asian population and relevance to subaxial cervical pedicle screw fixation. Eur Spine J. 2015;24:120–6. doi: 10.1007/s00586-014-3526-1. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Zhang B, Dai M, Xiong HC, Gao S, Li BH, et al. Anatomic study of individualized and improved pedicle screw implantation in the lower cervical spine. Int Surg. 2015;100:328–33. doi: 10.9738/INTSURG-D-14-00216.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim HS, Heller JG, Hudgins PA, Fountain JA. The accuracy of computed tomography in assessing cervical pedicle screw placement. Spine (Phila Pa 1976) 2003;28:2441–6. doi: 10.1097/01.BRS.0000090830.94641.AE. [DOI] [PubMed] [Google Scholar]
- 14.Mohi Eldin MM. Cervical pedicle screw fixation: Anatomic feasibility of pedicle morphology and radiologic evaluation of the anatomical measurements. Asian Spine J. 2014;8:273–80. doi: 10.4184/asj.2014.8.3.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Onibokun A, Khoo LT, Bistazzoni S, Chen NF, Sassi M. Anatomical considerations for cervical pedicle screw insertion: The use of multiplanar computerized tomography measurements in 122 consecutive clinical cases. Spine J. 2009;9:729–34. doi: 10.1016/j.spinee.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 16.Rao RD, Marawar SV, Stemper BD, Yoganandan N, Shender BS. Computerized tomographic morphometric analysis of subaxial cervical spine pedicles in young asymptomatic volunteers. J Bone Joint Surg Am. 2008;90:1914–21. doi: 10.2106/JBJS.G.01166. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Liu J, Liu Y, Wu Y, Zhu Q. Cervical pedicle screw fixation at C6 and C7: A cadaveric study. Indian J Orthop. 2015;49:465–70. doi: 10.4103/0019-5413.159678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakamoto T, Neo M, Nakamura T. Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine (Phila Pa 1976) 2004;29:2510–4. doi: 10.1097/01.brs.0000144404.68486.85. [DOI] [PubMed] [Google Scholar]
- 19.Koller H, Hempfing A, Acosta F, Fox M, Scheiter A, Tauber M, et al. Cervical anterior transpedicular screw fixation. Part I: Study on morphological feasibility, indications, and technical prerequisites. Eur Spine J. 2008;17:523–38. doi: 10.1007/s00586-007-0572-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oh SH, Min WK. Analysis of cervical pedicle with reconstructed computed tomography imaging in Korean population: Feasibility and surgical anatomy. J Spinal Disord Tech. 2014;27:E99–103. doi: 10.1097/BSD.0b013e318291f560. [DOI] [PubMed] [Google Scholar]
- 21.Ebraheim NA, Xu R, Knight T, Yeasting RA. Morphometric evaluation of lower cervical pedicle and its projection. Spine (Phila Pa 1976) 1997;22:1–6. doi: 10.1097/00007632-199701010-00001. [DOI] [PubMed] [Google Scholar]
- 22.Berry E, Cuppone M, Porada S, Millner PA, Rao A, Chiverton N, et al. Personalised image-based templates for intra-operative guidance. Proc Inst Mech Eng H. 2005;219:111–8. doi: 10.1243/095441105X9273. [DOI] [PubMed] [Google Scholar]


