Abstract
Background:
Careful preoperative planning in revision cases with complex acetabular defects is crucial for optimal surgery outcome. However, in many cases, computed tomography (CT) scans cannot give a clear understanding of the pelvic destruction. Three-dimensional (3D) models-based on CT data can help surgeon in planning of complex acetabular reconstruction.
Materials and Methods:
We used 3D plaster pelvic models in 17 revision cases. There were 5 patients with Paprosky II C acetabular defects, 2 patients with Paprosky IIIA defects, and 10 patients with Paprosky IIIB defects (3 patients among them with pelvic discontinuity). We used 3D printer and digital 3D models based on CT scan data for 3D models printing. In 3 cases with Paprosky IIIB defects, we implanted custom-made acetabular components with the porous coating, also printed on the 3D printer.
Results:
In 14 cases, we used trabecular metal (TM) augments with TM cups. In 100% of cases, number and type of planned and used augments were same. In 9 (64.3%) cases, size of planned and used cups was same. In other cases, the difference was not >2 mm.
Conclusions:
Use of 3D plaster models for the revision hip arthroplasty planning with complex acetabular defects has shown high accuracy in the clear understanding of acetabular bone deficiency.
Keywords: Complex acetabular defects, pelvic discontinuity, preoperative planning, revision hip arthroplasty, three-dimensional models
MeSH terms: Hip, acetabulum, arthroplasty, replacement hip, pelvis
Introduction
Total hip arthroplasty is the most successful method of treatment for the patients with serious diseases and traumas of the hip joint. However, in complex acetabular defects, stable fixation of the acetabular component may be a very difficult problem. In primary hip arthroplasty, complex acetabular defects found in patients with dysplasia, posttraumatic arthritis, and protrusion arthritis. In revision cases, massive acetabular osteolysis with Paprosky IIC, IIIA, and IIIB defects usually can be found. Perhaps, one of the most difficult problems is the pelvic discontinuity, which have no standardized solutions for treatment.1,2,3
Careful preoperative planning in these cases is crucial for the optimal outcome of the surgery. Computed tomography (CT) is necessary to understand the acetabular defect. However, in many cases, CT scans cannot give a clear understanding of the pelvic destruction. Three-dimensional (3D) models based on CT data can help surgeon in planning of complex acetabular reconstruction.
Furthermore, in some cases of massive bone loss, standard decisions, such as augments, bone grafting, and cages, do not allow achieving good fixation and function of the hip endoprosthesis. There are some data about large acetabular deficiency treatment with custom-made acetabular components.4,5,6
In this study, we have analyzed our experience of revision hip arthroplasty planning with 3D models.
Materials and Methods
We used 3D models in planning of 17 revision cases with complex acetabular defects since November 2015. The inclusion criteria were: Presence of signed informed consent, Severe acetabular defects (Paprosky IIC, IIIA, IIIB) after primary or revision hip arthroplasty Age ≥18 years.
The exclusion criteria were: Any acetabular defects without primary or revision hip arthroplasty in the anamnesis, Untreated hip periprosthetic infection.
3D models were produced in the following steps:
1. Multispiral CT scans with slice thickness no more 1 mm were performed. 2. CT scans in digital imaging and communications in medicine were sent to engineers 3. Engineers processed image, purify from interferences and create digital 3D model of the acetabulum. They also separated implant and soft tissues from model. For these goals, they used Materialise Mimics software (Belgium). 4. Engineers send digital 3D model in PDF format to us. 5. After agreement, they print 3D model from plaster [Figure 1] on Z printer 650 (USA). Then, they send this model to us.
Figure 1.

Plaster model of the acetabulum. Female, 74-year old. Pelvic discontinuity
As a result, we received plaster 3D model of the acetabulumin real size with all defects. These models help understand pelvic destruction clearer.
Among our patients, there were 11 females (64.7%) and 6 males (35.3%). Mean age was 64.9 ± 11.7 years (range 38-78 years).
Preoperative bone deficiency was defined according to Paprosky classification of acetabular bone loss.3,7 Five patients (29.4%) had Paprosky IIC defects (migration of the acetabular component medial to Kohler's line and intact acetabular rim). Two patients (11.8%) had Paprosky IIIA defects (superior and lateral migration of the acetabular component, intact posterior, and anterior columns, but hemispherical shell will have <50% patients’ bone contact). Ten patients (58.8%) had Paprosky III B defects (superior and medial migration of the acetabular component, <40% of patients’ bone available for ingrowth, rim defect is >1/2 circumference). Among patients with Paprosky IIIB defects, 3 patients (30%) had pelvic discontinuity with disruption of anterior and posterior columns).
With 3D models, we could not only verify the acetabular defects and classify it but very clearly plan the way of the acetabular reconstruction and stable fixation of revision components.
Acetabular reconstruction
Paprosky IIC defects
In these cases, we used the cage from two trabecular metal (TM) tantalum augments. We fixed augments together by bone cement and put this cage into the medial acetabular defect. Trabecular structure of this cage contacted with the patient's bone. The concave surface of this cage was coated with bone cement and we implanted the cup with TM surface (TM or Continuum, Zimmer Biomet, USA). The central part of the cup was fixed to cage with the bone cement and peripherally contacted with the patient's bone. Therefore, we created monolithic acetabular component with the large contacted area between TM surface and the bone.
Paprosky IIIA defects
In these cases, we used buttress TM augment for the anterior or posterior column defects substitution. Furthermore, we used one shim augment between the buttress and the bone. We fixed augments to the ilium with three or four 6.5 mm screws. Then we implanted the cup with TM surface. Between the cup and the augment, we put the bone cement.
Paprosky IIIB defects without pelvic discontinuity
We used different solutions in these cases. In 6 cases, cage from two augments into the superomedial defect with TM cups. In one case, we used custom triflange acetabular component printed on the 3D printer from the pure titanium powder. We used digital acetabular 3D model. We require following properties of the component:
Three flanges with holes for screws and maximal contact with ilium, ischium, and pubis
Holes orientation for optimal direction of the screws into the bone
Maximal substitution of all defects
A porous surface for contact with the bone
Big hemispherical part with possibilities of using large-diameter heads or dual mobility
Optimal angles orientation of hemispherical part (anteversion 15°, abduction 40°).
Engineers created digital 3D model of the acetabular component. After agreement, they printed custom-made acetabular component from the pure titanium powder Rematitan (Deutschland) on 3D printer Concept Laser M2 Cusing (USA).
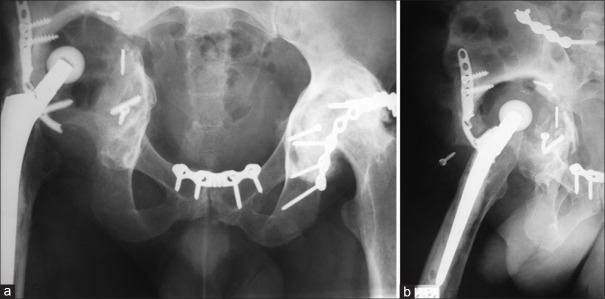
Before the surgery, this triflange acetabular component was sterilized. During the surgery, we removed the spacer and cleaned acetabular bone for the custom-made component. After that, we implanted triflange cup and fixed it by 6.5 mm screws to ilium, ischium and pubis. We implant the dual-mobility cup into the custom-made cup with the cement fixation. For the femoral reconstruction, we used Wagner SL Revision stem with bipolar head [Figure 2].
Figure 2.
Postoperative X-ray (L) hip with thigh anteroposterior view showing custom made triflange acetabular component printed on the three-dimensional printer
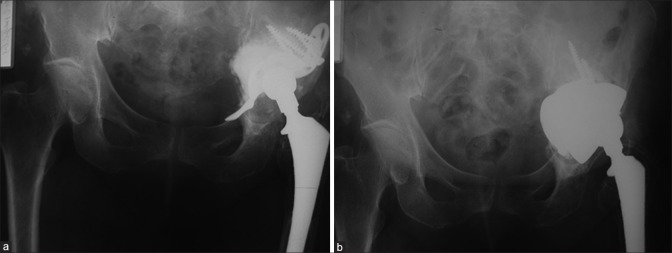
Paprosky IIIB defects with pelvic discontinuity. For these patients, we also used two different strategies. For one patient, we used cage from two TM augments. We impacted this cage to the defect and distracted two parts of the pelvis. After that, we implanted jumbo cup with TM surface (>68 mm). Between the cage and the cup, we used the bone cement [Figure 3].
Figure 3.
(a) preoperative X-ray (migration of Burch/Schneider cage). (b) postoperative X-ray after reconstruction of Paprosky IIIB defect with pelvic discontinuity
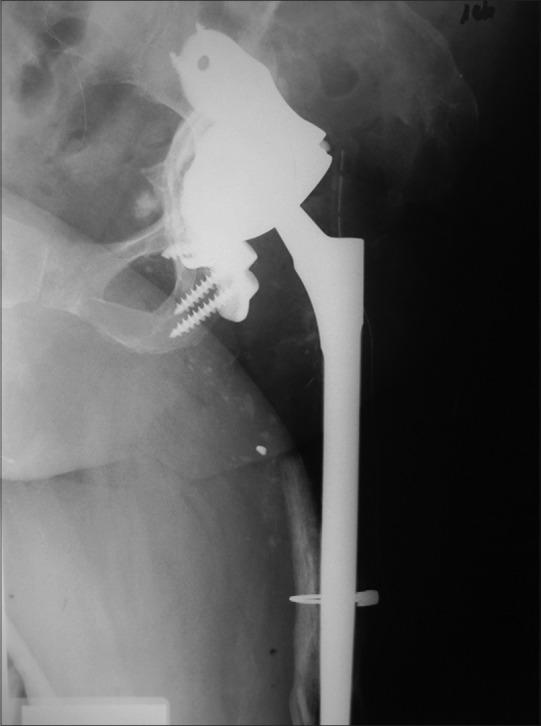
For two patients we used custom-made triflange acetabular components. One patient was 38-year-old male after car accident in 2010 with bilateral unstable pelvic fractures and fractures of both acetabula. After open reposition and internal fixation avascular necrosis of both femoral heads developed. In 2011 the total cemented hip arthroplasty on the right side was performed. In 2013, due to cup instability, revision hip arthroplasty with the cemented cup was performed. In November 2015, due to loosening of the acetabular component, the next attempt of revision hip arthroplasty was performed. However, after removal of the unstable cup, there was massive bleeding (about 12 l of blood). Surgery was stopped and the patient was treated in intensive care department. In February 2016, this patient was admitted to our clinic with an extensive acetabular defect and complete absence of the acetabular walls [Figure 4].
Figure 4.
Preoperative X-ray anteroposterior view of the pelvis (a) and lateral view of the right hip (b) showing large acetabular defects
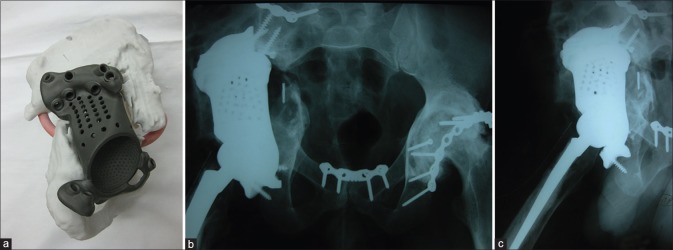
By the procedure described above, we made the plaster pelvic model and custom-made triflange cup. In March 2016, we implanted this acetabular component with pelvic distraction and set the polyethylene liner into the cup with the bone cement. We did not change stable femoral component and used 40 mm Biolox head [Figure 5].
Figure 5.
(a) Custom-made implant with the plaster model (b) postoperative X-ray pelvis anteroposterior view showing acetabular reconstructions (c) X-ray lateral view of the hip showing reconstructed acetabular defect
We have found the high efficiency of preoperative planning with using of plaster models in 14 cases (in three cases we used custom implants). We compared number and type of planned and used augments and size of planned and used cups.
Statistical analysis
Statistical analysis was performed with Statistica 10 software. Kolmogorov–Smirnov (P < 0.1) and Lilliefors (P < 0.01) tests were used for normality of difference between diameters of planned and used acetabular components. Wilcoxon matched pair test was used to compare planned and used diameter of cups (P = 0.463).
Results
Mean followup was 5.35 ± 2.26 months (range 2-9 months). All 17 patients are alive to this moment. We had no cases of implant loosening, periprosthetic infection and prosthesis dislocation.
Number and type of planned and used augments are shown in Table 1.
Table 1.
Comparison of number and type of planned with plaster model and used augments
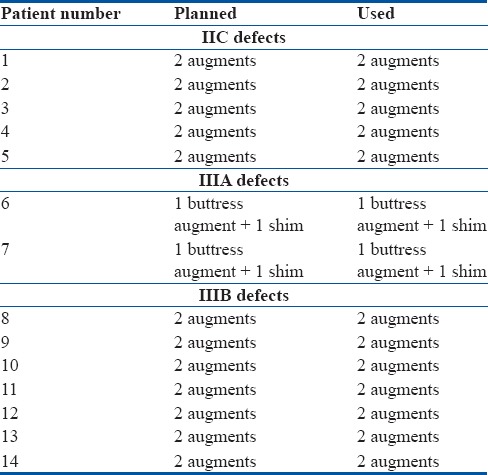
Thus, in 100% of cases number and type of planned and used augments were same.
Size of planned and used cups is shown in Table 2.
Table 2.
Comparison of size of planned with plaster model and used cups
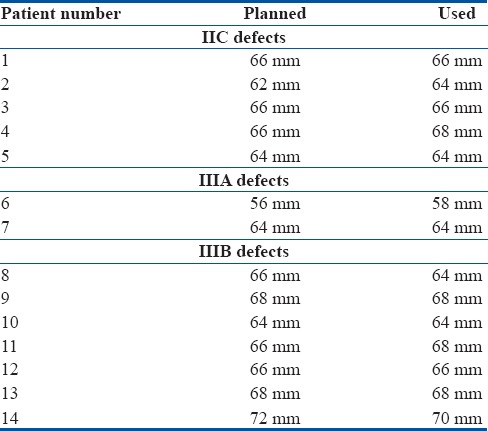
In 9 patients (64.3%), size of planned and used cups was same. In other cases, the difference was not >2 mm.
Discussion
Treatment of patients with complex acetabular defects is a very difficult problem.7,8 In cases of severe bone defects, we should achieve stable fixation of the acetabular component and restore the hip center.9 The most optimal way is the biologic fixation with good primary stability and secondary osteointegration. Many authors report good results of tantalum augments and cups with tantalum coating.8,10,11,12,13,14 Furthermore, there are some publications about custom-made triflange components for complex acetabular revision.4,5,6
The key to success of revision hip arthroplasty is the accurate preoperative planning. 3D technologies can help to solve this problem. Won et al. reported about “Rapid Prototype” (RP) modeling technique. They produced full-sized wax/plaster models of the pelvis based on 3D CT data. They used pelvic RP models in 21 patients with hypoplastic acetabulum, uncontained acetabular defects, or a fused hip.15
Hughes et al. described life-size 3D models, which were manufactured from CT scans of three hip joints in two patients. The first patient had undergone multiple previous hip arthroplasties for bilateral hip infections, resulting in right-sided pelvic discontinuity and a severe left-sided posterosuperior acetabular deficiency. The second patient had a first-stage revision for infection and recurrent dislocations. These models allowed accurate surgical simulation, thus improving anatomical appreciation and preoperative planning.16 Our experience also showed high accuracy of planning with pelvic life-size 3D models in patients with complex acetabular defects.
The goal of our study was to show that 3D models of the acetabulum in real size makes the planning very precise and correct. All the reconstructive methods, planned with plaster models, were accurately reproduced during surgery.
We used our models for revision hip arthroplasty planning with TM augments and cups. However, in three cases, we improved our technology and based on 3D models we produced custom-made acetabular components with porous coating from titanium powder on 3D printer. In these cases usage of tantalum augments was impossible, or more expensive, than the printing of custom-made components.
Berasi et al. formulated indications for the use of custom triflange components in revision hip arthroplasty. There are previous, failed, salvage reconstruction with cage or porous metal construct augments; largely contained defects with possible discontinuity; known pelvic discontinuity and complex hips which have previously undergone repeated total hip arthroplasty (THA) and with insufficient bone stock to reconstruct using other means.6 We agree with these indications and use it in our practice.
Perhaps, the most complex cases in acetabular reconstruction are pelvic discontinuity. Taunton et al. retrospectively identified 57 patients who had pelvic discontinuity treated with a custom Pinnacle TM Triflange Acetabular System.4 Among these patients, twenty (30,3%) had revision for any reason. Only three reoperations (5, 3%) were due to failures of the triflange acetabular components, and only one patient was revised due to aseptic loosening. We used custom-made implants only in two patients with pelvic discontinuity, and we have a very short followup.
We believe that usage of modern 3D printers greatly simplifies production of custom-made cups and this technology may be more common in the future.
There were several limitations in this study. The sample size is small. In addition, we have very short followup and cannot analyze clinical significance of three-dimensional models. In the future, we plan to compare revision groups with or without 3D models.
Conclusions
The need for revision hip arthroplasty increases every year. Unfortunately, among these patients, many have massive acetabular osteolysis with Paprosky IIC, IIIA, or IIIB defects. 3D plaster models in these cases have shown high accuracy in the clear understanding of acetabular bone deficiency. In 100% of cases number and type of planned and used augments were same. There was no difference in size of planned and used cups ffor > 2 mm. The development of 3D modeling and 3D printing technologies will improve the results of treatment in patients with complex acetabular defects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Villanueva M, Rios-Luna A, Pereiro De Lamo J, Fahandez-Saddi H, Böstrom MP. A review of the treatment of pelvic discontinuity. HSS J. 2008;4:128–37. doi: 10.1007/s11420-008-9075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown NM, Hellman M, Haughom BH, Shah RP, Sporer SM, Paprosky WG, et al. Acetabular distraction: An alternative approach to pelvic discontinuity in failed total hip replacement. Bone Joint J. 2014;96-B:73–7. doi: 10.1302/0301-620X.96B11.34316. [DOI] [PubMed] [Google Scholar]
- 3.Sheth NP, Melnic CM, Paprosky WG. Acetabular distraction: An alternative for severe acetabular bone loss and chronic pelvic discontinuity. Bone Joint J. 2014;96-B:36–42. doi: 10.1302/0301-620X.96B11.34455. [DOI] [PubMed] [Google Scholar]
- 4.Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ, et al. Pelvic discontinuity treated with custom triflange component: A reliable option. Clin Orthop Relat Res. 2012;470:428–34. doi: 10.1007/s11999-011-2126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hogan C, Ries M. Treatment of massive acetabular bone loss and pelvic discontinuity with a custom triflange component and ilio-sacral fixation based on preoperative CT templating. A report of 2 cases. Hip Int. 2015;25:585–8. doi: 10.5301/hipint.5000247. [DOI] [PubMed] [Google Scholar]
- 6.Berasi CC, 4th, Berend KR, Adams JB, Ruh EL, Lombardi AV., Jr Are custom triflange acetabular components effective for reconstruction of catastrophic bone loss? Clin Orthop Relat Res. 2015;473:528–35. doi: 10.1007/s11999-014-3969-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year followup evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 8.Jeong M, Kim HJ, Lim SJ, Moon YW, Park YS. Revision total hip arthroplasty using tantalum augment in patients with paprosky III or IV acetabular bone defects: A minimum 2-year follow up study. Hip Pelvis. 2016;28:98–103. doi: 10.5371/hp.2016.28.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bozic KJ, Rubash HE. The painful total hip replacement. Clin Orthop Relat Res. 2004;420:18–25. doi: 10.1097/00003086-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Del Gaizo DJ, Kancherla V, Sporer SM, Paprosky WG. Tantalum augments for paprosky IIIA defects remain stable at midterm followup. Clin Orthop Relat Res. 2012;470:395–401. doi: 10.1007/s11999-011-2170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siegmeth A, Duncan CP, Masri BA, Kim WY, Garbuz DS. Modular tantalum augments for acetabular defects in revision hip arthroplasty. Clin Orthop Relat Res. 2009;467:199–205. doi: 10.1007/s11999-008-0549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Long WJ, Noiseux NO, Mabry TM, Hanssen AD, Lewallen DG. Uncemented porous tantalum acetabular components: Early followup and failures in 599 revision total hip arthroplasties. Iowa Orthop J. 2015;35:108–13. [PMC free article] [PubMed] [Google Scholar]
- 13.Whitehouse MR, Masri BA, Duncan CP, Garbuz DS. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years. Clin Orthop Relat Res. 2015;473:521–7. doi: 10.1007/s11999-014-3861-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA, et al. Systematic review on outcomes of acetabular revisions with highly-porous metals. Int Orthop. 2014;38:689–702. doi: 10.1007/s00264-013-2145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Won SH, Lee YK, Ha YC, Suh YS, Koo KH. Improving preoperative planning for complex total hip replacement with a rapid prototype model enabling surgical simulation. Bone Joint J. 2013;95-B:1458–63. doi: 10.1302/0301-620X.95B11.31878. [DOI] [PubMed] [Google Scholar]
- 16.Hughes AJ, DeBuitleir C, Soden P, O’Donnchadha B, Tansey A, Abdulkarim A, et al. 3D printing aids acetabular reconstruction in complex revision hip arthroplasty. Adv Orthop. 2017;2017:8925050. doi: 10.1155/2017/8925050. [DOI] [PMC free article] [PubMed] [Google Scholar]