Abstract
Background:
Magnetic resonance imaging (MRI) has been gold standard investigation for diagnosing anterior cruciate ligament (ACL) tear. Availability and cost are two main factors limiting the universal use of MRI in all those patients in whom ligament injury is suspected. We compared the outcome of functional USG with gold standard MRI scan in this prospective study.
Materials and Methods:
In this study, we included the patients coming to orthopedics outpatient department with sign and symptoms of ACL injury. We performed functional USG of the injured and uninjured knee and noted the difference in translation, measured by USG. More than 1 mm of difference in translation of tibia on the affected side as compared to uninjured side is taken as significant. We compared our result with the findings of MRI. The study result of 130 patients revealed high sensitivity (81.65%) and high specificity (89%) in diagnosing ACL injury. The positive predictive value of the test was 97.8%, and the negative predictive value was 44%. The P value of the difference of translation as 0.0001 was also statistically significant.
Conclusions:
We can safely conclude from the study that the functional USG can be used as a primary tool to diagnose ACL tears. USG's ubiquitous availability and simple technique of the procedure can bring a revolution in the future for diagnosing and managing ACL injury.
Keywords: Knee, anterior cruciate ligament, ligament injury, functional ultrasonography, magnetic resonance imaging
MeSH terms: Anterior cruciate ligament, magnetic resonance imaging, ultrasonography
Introduction
Anterior cruciate ligament (ACL) is one of the most common ligament injuries of the knee. Although there are no registries in India to give an exact number of patients, there is a huge burden of patients of ACL tear and a large number of them undergo ACL reconstruction every year. It involves a huge cost in diagnosing and managing these injuries. At our tertiary care hospital, we see 5–10 patients with ACL injury every week. Lack of awareness, unavailability of diagnosing modality, and treatment facility leads to neglect and delayed presentation of these injuries.
Diagnosing ACL tear accurately and early has always been the goal of treating physician.1
Investigation of choice for suspected ACL tear is magnetic resonance imaging (MRI). It is a costly investigation and is also not readily available in the majority of hospitals in India. Thus, cheaper options have been explored in the past2,3 The very purpose of utilizing ultrasonography (USG) as a diagnostic tool is its availability and cost. It is easy to perform and takes less time. It can be used in acute scenarios and remote locations away from the hospital (field scenario) as well. Sonographic examination has been widely used for detecting musculoskeletal disorders in recent decades. It has the advantages of being noninvasive, readily available, dynamic, and allows for good visualization of superficial structures.2,4
We at our center seldom get acute injuries and our patients present very late to us. Palm et al.3 (2009) conducted their study in acute injury scenario, we decided to carry it out in our patient cohort, to see whether we could reproduce their result or not. We also wanted to find whether their results in acute scenario be replicated in late presented cases of ACL tear.
Materials and Methods
The present study was approved by the Institute Review Committee of our institute. In this prospective clinical study, patients presenting to the outpatient department with complaints of instability and/or locking of knee joint were evaluated and recruited as per the inclusion and exclusion criteria [Table 1]. Informed consent was taken from the patients for their participation in the study and willingness to undergo ultrasound examination and MRI (if not already done). We included 182 patients between May 2014 and August 2016. Of these 182, only 130 patients underwent all three examinations, that is clinical examination findings, functional USG, and MRI scan. Data of these 130 patients were finally evaluated for the purpose of this study.
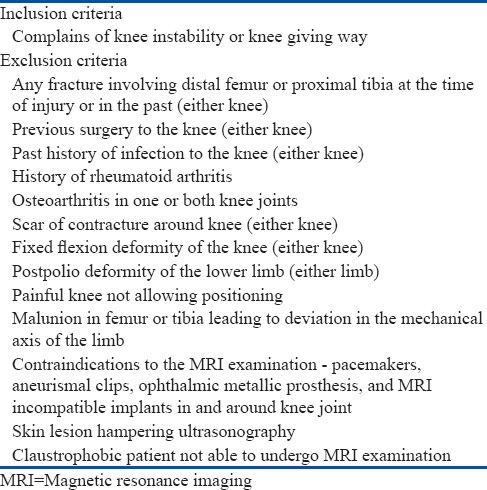
Table 1.
Inclusion and exclusion criteria
The patients were clinically evaluated by the senior orthopedic surgeon (SK/AK) and the clinical findings were recorded. The clinical findings were not revealed to the sonologist.
The patients were then sent to Department of Radiodiagnosis, who performed the functional USG examination and recorded the findings in a separate Proforma. The procedure was performed on portable ultrasound machine (m-Turbo, Fujifilm Sonosite, USA) using a high-resolution linear probe (6–13 MHz). The procedure was performed as described by Palm et al.3 The patients were made to lie prone with a towel rolled under the lower leg to make the knee flexed by 20° [Figure 1]. The probe was kept in a sagittal plane in the popliteal fossa to obtain a longitudinal image of the medial femoral and tibial condyles in a line [Figure 2]. Reference lines are drawn tangent to the femoral condyle and the posterior aspect of the tibia would be used for further evaluation. Distance D1 as shown by Palm et al.3 was obtained. Maximum pressure was then applied to the tibia [Figure 3] to produce a maximum anterior translation of tibia over femur, and distance D2 [Figures 4–7] was obtained. The measurement was done thrice, and average distance was taken into final calculation. The distance D2-D1 would be D as the distance of translation of tibia. The process was repeated in the other knee also to obtain D, D1, and D2 values.
Figure 1.

A clinical photograph showing position of lower limb for the procedure. Patient is lying prone and a rolled sheet is kept under the ankle to flex the knee around 20°
Figure 2.

Clinical photograph showing position of ultrasound probe. The ultrasound probe is put longitudinally over the popliteal fossa along the longitudinal axis of the lower limb perpendicular to the joint line
Figure 3.

Clinical photograph showing pressure over the limb. The tibia is pushed anteriorly with one hand of the examiner while the probe is kept in the same position with other hand
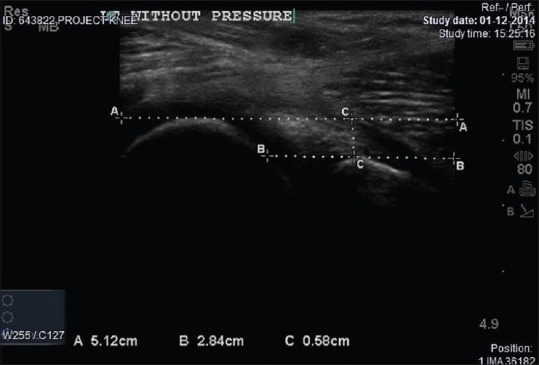
Figure 4.
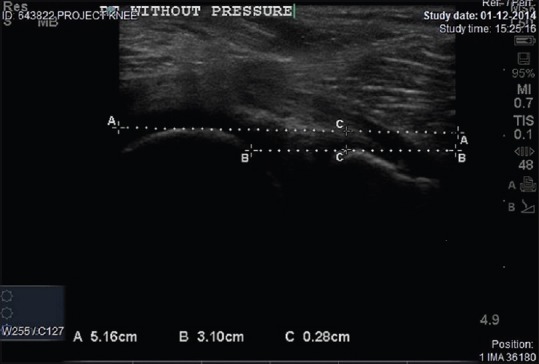
Sonograph of right knee without pressure. Line A is a tangent drawn from the highest point of femoral condyle. Line B is a tangent drawn from the highest point of the tibial condyle. CC is the distance between femoral and tibial condyle
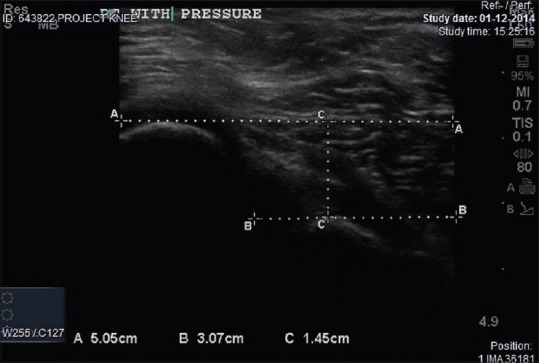
Figure 7.
Sonograph of left knee pressure. After giving pressure, on the tibial condyle, line A is a tangent drawn from the highest point of femoral condyle. Line B is a tangent drawn from the highest point of the tibial condyle. CC is the distance between femoral and tibial condyle, also denotes the translation on pressure
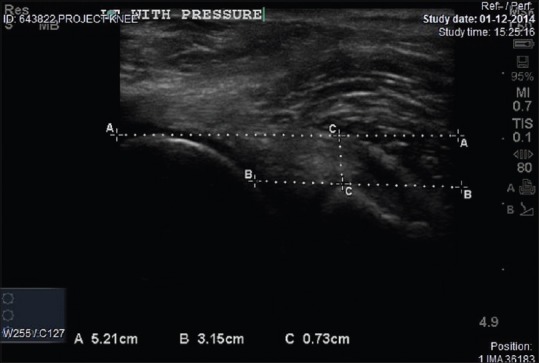
Figure 5.
Sonograph of right knee with pressure. After giving pressure, on the tibial condyle, line A is a tangent drawn from the highest point of the femoral condyle. Line B is a tangent drawn from the highest point of the tibial condyle. CC is the distance between femoral and tibial condyle, also denotes the translation on pressure
Figure 6.
Sonograph of left knee without pressure. Line A is a tangent drawn from the highest point of the femoral condyle. Line B is a tangent drawn from the highest point of the tibial condyle. CC is the distance between femoral and tibial condyle
The patient who did not have an MRI scan was asked to undergo MRI scan, and its film was evaluated and findings were noted. Films of those who already had an MRI were evaluated and findings were recorded.
We tested the sensitivity, specificity, positive predictive value, and negative predictive value of the results of functional ultrasound with respect to the result obtained from MRI. We also measured the 95% confidence interval of our result. Paired t-test was applied to test the translation difference (ΔD) between two knee joints.
Results
We recruited 130 patients (n-130) in this study. Of 130, 122 were male and eight were female. The average age of our study population was 28.26 (range 14-52 years). The patients presented to us at an average lapse of 16.19 months following injury (range 15 days - 10 years) following injury [Tables 2 and 3]. Of 130 patients, 57 knees were left, and 73 were right. We had kept the difference in translation (injured compared to noninjured side) of 1 mm of the injured knee, on USG examination, as significant. The results are summarized in a 2 × 2 table [Table 3].
Table 2.
Duration of presentation since injury
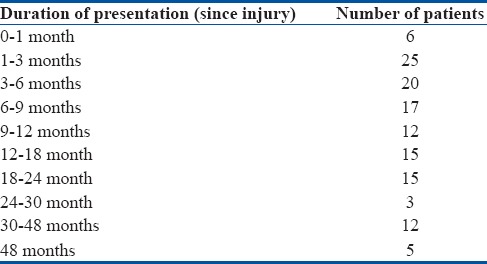
Table 3.
Functional ultrasonography difference in translation between injured and noninjured side
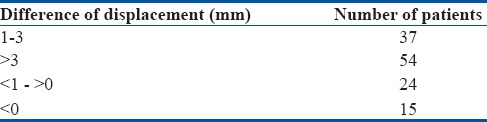
Of 130 patients, 91 of them had positive USG (>1 mm of difference in translation). ACL tear was detected in 89 of those patients in MRI. Thirty-nine patients had negative USG. Of these 39 patients, 22 of them had ACL tear on an MRI.
Of these 39 patients (negative ultrasound), we had 15 patients in which the values of translations were negative which means that there was more translation of tibia on femur on normal side as compared to the injured side.
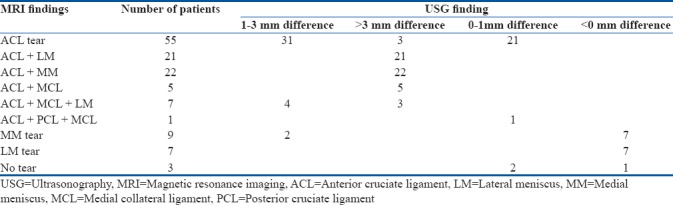
There were patients who also had other associated injuries on MRI [Table 4]. We found in our results that the difference in translation was more in patients who also had either collateral ligament injury or meniscal injury along with ACL tear. Of 48 patients, who had ACL tear and other associated injuries (either medial meniscus, lateral meniscus, or lateral collateral ligament tear), the difference in translation was more than 3 mm in all of them. Of seven patients with combined ACL, medial collateral ligament and lateral meniscus injury, all seven had a significant translation but only three had more than 3 mm of difference in translation. We had one patient with a combination of ACL, posterior cruciate ligament, and medial collateral ligament injury, the translation was not significant (false negative). There were seven patients having only medial meniscus tear. Of these seven patients, two had a significant translation (false positive) and five had an insignificant translation (true negatives). We had seven patients of an isolated lateral meniscus tear, and all of them had an insignificant translation (value < 0 in translation) (true negatives). Three patients who had no injury on MRI had an insignificant translation (true negatives), but one of them had the values in negative [Table 5].
Table 4.
Findings on magnetic resonance imaging
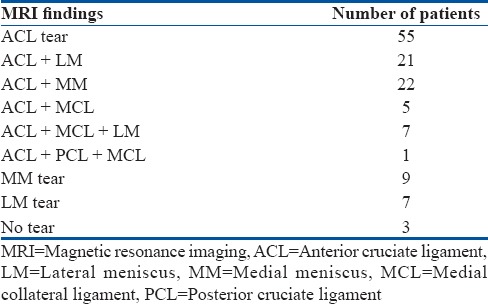
Table 5.
Lesion and difference in translation between injured and noninjured side on ultrasonography
In this study, the percentage of ACL tear correctly diagnosed by USG was 81.65% (sensitivity) with a specificity of 89%. The positive predictive value of the test was 97.8%, and the negative predictive value was 44%.
Statistical analyses were performed using Stata version 10 (Stata Corp, Texas, USA). Paired t-test was applied to test the translation difference (ΔD) between two knee joints. A 2 × 2 contingency table was created to present the result of functional USG and MRI for estimating sensitivity, specificity, positive predictive, and negative predictive values for USG in comparison to MRI [Tables 6 and Table 7].
Table 6.
2×2 contingency table showing the result of magnetic resonance imaging and ultrasonography
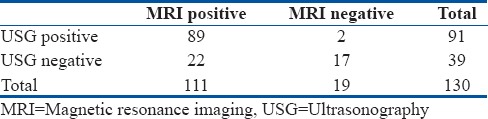
Table 7.
Comparison of the translation difference (ΔD) between two knee joints
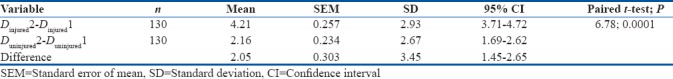
Sensitivity = 80%, 95% confidence Interval = (73%–88%)
Specificity = 89%, 95% confidence interval = (78%–100%)
Positive predictive value = 98%, 95% confidence interval = (95%–100%)
Negative predictive value = 44%, 95% confidence interval = (28%–59%)
The P value of the difference of translation as 0.0001 was also statistically significant.
Two-tailed paired t-test was performed comparing various clinical tests, namely anterior drawer test, Lachman test, and pivot-shift test with anterior displacement on US examination taking 1-mm displacement as cutoff and MRI findings. Following Bonferroni correction, the statistically significant value was kept as - P ≤ 0.017. Comparing the clinical tests with USG anterior drawer test, P value came as 0.018015, Lachman test P value came 0.022758, and pivot-shift test P value was 0.158099. None of these clinical tests were found to be statistically significant (with a significant value of P < 0.017).
On comparing clinical tests with MRI, the P value of anterior drawer test was found to be 0.011996, that of Lachman test was 0.011996, and pivot-shift test was 0.00001. All these tests, the P value was statistically significant (with a significant value of P < 0.017).
Discussion
At present, in our setup, there is no role of USG in suspected cases of ACL (to the best of our knowledge and practice), and MRI is the investigation of choice. This study found a high level of sensitivity, specificity, and positive predictive values in favor of functional USG in diagnosing ACL tears. Thus, in patients who have positive USG, we can justify getting an MRI scan to further evaluate the injury. Those who have a negative clinical examination and negative USG (translation <1 mm as compared to normal side) can be safely suggested not to undergo the MRI scan. Hence, this will not only reduce the cost but also prevent undue delay in getting a proper diagnosis.
Role of USG is well accepted for use in evaluating extraarticular structures of the knee,4,5,6 but has a debatable role in the evaluation of intraarticular structures.6 Although sonographic examination is not perfect for evaluating the internal structure of the knee, it is thought to be accurate for the detection of knee effusion.4,7,8
For ACL injury, researchers have tried diagnosing it with ultrasound using different criteria such as “echo-poor space,”9,10 and “S shape” or “comma shape”11 of the posterior cruciate ligament, but have not shown consistent and reproducible results. These indirect signs are easy to appreciate in acute cases but are not possible in chronic cases of ACL tears.
Another indirect method of revealing ACL tear in acute knee injuries is the USG demonstration of increased tibial translation on femur in injured knee. This was first described by Schricker in 1987.12 It was further developed by Chylarecki in 1995.13 Schwarz et al. in 199714 and Gebhard et al. in 1999,15 who unlike Schricker,12 examined the patients in the prone position from a dorsal approach and performed the tests manually and without assistance. Using this method, it is also easy to examine the posterior cruciate ligament.
In the paper published by Palm et al. in “The Knee” in 2009,3 they revealed the effectiveness of this method in acute setting. They had shown very good outcome with 97% of sensitivity and with a specificity of 87.5%. The positive predictive value was 97%, and the negative predictive value was 87.5%. All their cases were done in acute setting during ski season. Taking the lead from the study by Palm et al.,3 we did our study.
Our result of 130 patients showed 81.65% of sensitivity (95% confidence interval = [73%–88%]) with a specificity of 89% (95% confidence interval = [78%–100%]). The positive predictive value of the test was 97.8% (95% confidence interval = [95%–100%]) and negative predictive value was 44% (95% confidence interval = [28%–59%]). The P value of translation as 0.0001 which was statistically significant.
These results are highly significant because we took 130 patients in our study which is statistically a very good number and we are not aware of any such study with such high number of patients. Most of the studies evaluating the role of USG in diagnosing ACL injury have been done on patients with the acute presentation. Our study thus becomes significant as our patient cohort is of late presenters. There were many patients who underwent some form of physical therapy and continued with their daily activity and job. This might have created some positive feedback and self-protective mechanism by periarticular muscles and ligaments. Thus, in chronic cases, it is important to realize that there can be other knee stabilizers acting to resist the tibial translation and thus we got a low negative predictive value in our study (44% [95% confidence interval = [28%–59%]). This finding is contrary to the results of Palm et al. who showed high negative predictive values as well (87.5%). It is also worth noting that Palm et al. did their study in acute cases, and chances of secondary stabilizer getting strengthened were very less and thus their negative predictive values were high.
We also noticed in our series that those patients who had other injuries along with ACL (medial meniscus, lateral meniscus, and medial collateral ligament) injury had more than 3 mm of difference in translation. If we only had taken patients with these injuries then our sensitivity, specificity, positive predictive value, and negative predictive value will come as 100%. This goes to show that even in chronic cases if other knee stabilizers are injured, then it is difficult to keep the knee stabilized. Thus, we can safely recommend on the basis of our study that if the difference in translation is more than 3 mm, then an MRI is highly recommended to understand the extent of injury and evaluate other associated injuries.
We had 22 patients, where the USG could not detect a significant difference of translation while the MRI reveals ACL injury. Of these 21 patients had only isolated ACL injury. It again goes on to signify that the false-positive results were seen in isolated injury, and this may be due to the stabilizing effect of the periarticular muscles of the knee and other ligaments and menisci.
Single radiology consultant performed the USG in all the patients in this study, we cannot confidently say that the results of the procedure, which is somewhat user dependent, can be reproduced by other sonologists or not. It would have been interesting to see the outcomes if two different sonologists performed the procedure on the same patient.
Another limitation of thi study was that since all the MRIs were not done at one institute, and hence, the standardization in sequence could not be established or guaranteed. Although, all the patients included in this study had T1, T2, and PD sequence in sagittal, axial, and coronal section, and the images were reviewed by the same radiologist before confirming the diagnosis.
Conclusions
The purpose of this study was not to replace MRI in investigating ACL tear but to compare the role of USG. This study showed a high sensitivity, specificity, and positive predictive value of functional USG in diagnosing ACL tear. On this basis, we recommend that functional USG can be used as a first modality of investigation in suspected cases of ACL tear.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. Alok Ranjan and Dr. Sanjay Pandey Department of Community and Family Medicine got their help towards statistical analysis.
References
- 1.Friemert B, Oberländer Y, Schwarz W, Häberle HJ, Bähren W, Gerngross H, et al. Diagnosis of chondral lesions of the knee joint: Can MRI replace arthroscopy? A prospective study. Knee Surg Sports Traumatol Arthrosc. 2004;12:58–64. doi: 10.1007/s00167-003-0393-4. [DOI] [PubMed] [Google Scholar]
- 2.Khan Z, Faruqui Z, Ogyunbiyi O, Rosset G, Iqbal J. Ultrasound assessment of internal derangement of the knee. Acta Orthop Belg. 2006;72:72–6. [PubMed] [Google Scholar]
- 3.Palm HG, Bergenthal G, Ehry P, Schwarz W, Schmidt R, Friemert B, et al. Functional ultrasonography in the diagnosis of acute anterior cruciate ligament injuries: A field study. Knee. 2009;16:441–6. doi: 10.1016/j.knee.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Friedman L, Finlay K, Jurriaans E. Ultrasound of the knee. Skeletal Radiol. 2001;30:361–77. doi: 10.1007/s002560100380. [DOI] [PubMed] [Google Scholar]
- 5.Bouffard JA, Dhanju J. Ultrasonography of the knee. Semin Musculoskelet Radiol. 1998;2:245–70. doi: 10.1055/s-2008-1080106. [DOI] [PubMed] [Google Scholar]
- 6.Court-Payen M. Sonography of the knee: Intraarticular pathology. J Clin Ultrasound. 2004;32:481–90. doi: 10.1002/jcu.20069. [DOI] [PubMed] [Google Scholar]
- 7.Delaunoy I, Feipel V, Appelboom T, Hauzeur JP. Sonography detection threshold for knee effusion. Clin Rheumatol. 2003;22:391–2. doi: 10.1007/s10067-003-0759-5. [DOI] [PubMed] [Google Scholar]
- 8.Hauzeur JP, Mathy L, De Maertelaer V. Comparison between clinical evaluation and ultrasonography in detecting hydrarthrosis of the knee. J Rheumatol. 1999;26:2681–3. [PubMed] [Google Scholar]
- 9.Suzuki S, Kasahara K, Futami T, Iwasaki R, Ueo T, Yamamuro T, et al. Ultrasound diagnosis of pathology of the anterior and posterior cruciate ligaments of the knee joint. Arch Orthop Trauma Surg. 1991;110:200–3. doi: 10.1007/BF00571059. [DOI] [PubMed] [Google Scholar]
- 10.Ptasznik R, Feller J, Bartlett J, Fitt G, Mitchell A, Hennessy O, et al. The value of sonography in the diagnosis of traumatic rupture of the anterior cruciate ligament of the knee. AJR Am J Roentgenol. 1995;164:1461–3. doi: 10.2214/ajr.164.6.7754893. [DOI] [PubMed] [Google Scholar]
- 11.Hawe W. The S shape of the posterior cruciate ligament in the sonogram. Prakt Sport Traumatol Sportmed. 1990;2:7–8. [Google Scholar]
- 12.Schricker T, Hien NM, Wirth CJ. Clinical results of sonographic functional studies of lesions of the capsule and ligaments of the knee and ankle joint. Ultraschall Med. 1987;8:27–31. doi: 10.1055/s-2007-1011653. [DOI] [PubMed] [Google Scholar]
- 13.Chylarecki C, Hierholzer G, Tabertshofer H. Sonographic features of fresh rupture of the anterior cruciate ligament. Unfallchirurgie. 1995;21:109–17. doi: 10.1007/BF02589947. [DOI] [PubMed] [Google Scholar]
- 14.Schwarz W, Hagelstein J, Minholz R, Schierlinger M, Danz B, Gerngross H, et al. Manual ultrasound of the knee joint. A general practice method for diagnosis of fresh rupture of the anterior cruciate ligament. Unfallchirurg. 1997;100:280–5. doi: 10.1007/s001130050120. [DOI] [PubMed] [Google Scholar]
- 15.Gebhard F, Authenrieth M, Strecker W, Kinzl L, Hehl G. Ultrasound evaluation of gravity induced anterior drawer following anterior cruciate ligament lesion. Knee Surg Sports Traumatol Arthrosc. 1999;7:166–72. doi: 10.1007/s001670050142. [DOI] [PubMed] [Google Scholar]


