Abstract
In the current clinical scenario, restenosis following the primary surgical procedure for lumbar canal stenosis is being frequently noticed. A number of studies have evaluated the reoperation rates following different surgical procedures for lumbar canal stenosis. However, a dilemma still exists about the surgical procedures, associated comorbidities and reoperation rates. In this study, we have reviewed the existing literature for lumbar canal stenosis surgery and their reoperation rates. A PubMed search for all papers stating “reoperation after spinal stenosis,” “revision surgery after spinal stenosis,” and “reoperations and lumbar canal stenosis” were explored. A total of 440 publications were found, of which 23 publications were shortlisted. The existing literature on reoperation rates after surgery for lumbar canal stenosis was reviewed and analyzed. From the literature search, 29680 patients who underwent surgeries for spinal stenosis have been included in the review. 11.65% ± 4.25% of them underwent reoperations following the primary procedure with a followup period of 6.80 ± 3.90 years. Fenestration surgeries showed an average reoperation rate of 7.58% ± 5.29% in 8.28 ± 6.26 years followup as compared to laminectomy alone (12.70% ± 7.49%, 6.50 ± 2.12 years followup). Laminectomy with or without fusion showed a reoperation rate of 11.22% ± 4.25% in 6.00 ± 2.60 years followup period. The comparative results of these studies were however not significant. The causes of reoperation were multifactorial ranging from the type of procedure performed, associated comorbidities or smoking. Statistical data do not indicate the superiority of any particular type of surgery, which reduces the rate of reoperation. The causes for reoperation are inadequate decompression or instability. The literature does not give statistics for these complications in the papers. Smoking is an independent risk factor for revision surgery. Diabetes reduces the time interval between the initial surgery and the revision surgery. This review highlights the causes of reoperations in various lumbar stenosis surgeries, associated comorbidities and expected outcome.
Keywords: Comorbidities, fenestration, fusion, laminectomy, lumbar canal stenosis, reoperations
MeSH terms: Lumbar vertebrae, spinal stenosis, laminectomy, reoperation
Introduction
Symptomatic stenosis in lumbar spine often requires decompression with or without fusion if conservative treatment fails. Although laminectomy stays as a traditional decompression technique, minimally invasive decompression procedures such as laminoplasty, laminoforaminoplasty, and unilateral laminotomy for bilateral decompression (ULBD) have been evolved over the past decade to reduce associated complications and reoperations.1,2 As the majority of lumbar stenosis is caused by hypertrophy of ligamentum flavum or facet joints resulting into narrowing of spinal canal, decompression procedures that directly target such structures with the preservation of lamina and bony structures help in maintaining the stability of the spine.3 Reoperations in such cases often result from progressive stenosis or instability at the index or adjacent levels.4 However, reoperations due to perioperative complications such as wound infections, epidural fibrosis, pseudomeningocele, or dural leak are also reported in the literature.5,6 Reoperations after previously operated lumbar surgery tend to result in less favorable outcomes;7,8 however, there are few reports published in the literature that specifically evaluated risk factors regarding reoperations after lumbar stenosis surgery. In this review, we aimed to evaluate the existing PubMed literature on revision surgeries following the primary procedure for lumbar canal stenosis. The risk factors and associated comorbidities have also been discussed in details.
Materials and Methods
The authors independently assessed the methodological quality of each study selected for review. Internal validity scores of methodological quality were assessed based on the operational criteria recommended by the Cochrane Back Review Group. Studies that met six or more of the 11 criteria by scoring a “yes” were considered to be studies of high quality. Blinding of the selected trials with regard to authors, institution, or journal did not seem practical because several authors are familiar with the reported literature in this field.
The data were independently extracted from each study utilizing a predesignated data extraction sheet. Core data entailed study characteristics, the presence of funding, ethical approval, operative characteristics, study population, interventions, and outcomes. If the above data were not available, the corresponding author of the selected study was contacted to provide the necessary information. In the event, the lead study author could not be contacted or is nonresponsive, only the published data parameters were noted. Pooling of the data was completed when it was clinically sensible to do so. Pooling of the data was performed if trials were regarded homogenous (i.e., study design, population, intervention, comparisons, and outcomes).
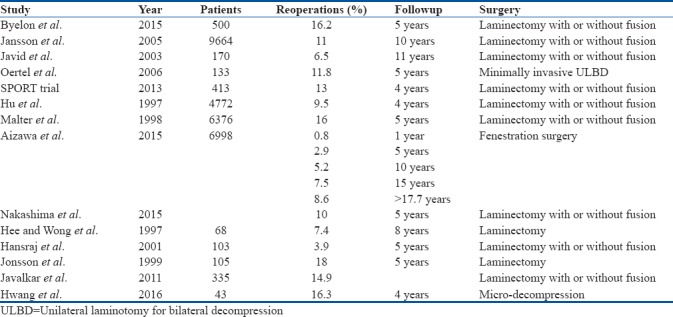
In this review, a PubMed search for all papers stating “reoperation rates after spinal stenosis,” “revision surgery after spinal stenosis,” “reoperations, and lumbar canal stenosis” were explored. A total of 440 publications were found, out of which 140 were related to spine surgery. The literatures on human surgeries with full-text availability were selected for the review [Figure 1]. Only English language publications were included which were listed on PubMed. Although there were a few studies, no review article compiling them was found. A total of 23 studies were shortlisted after internal validation scoring. These were further divided as per the surgeries performed as follows: followup periods and reoperation rates [Table 1].
Figure 1.
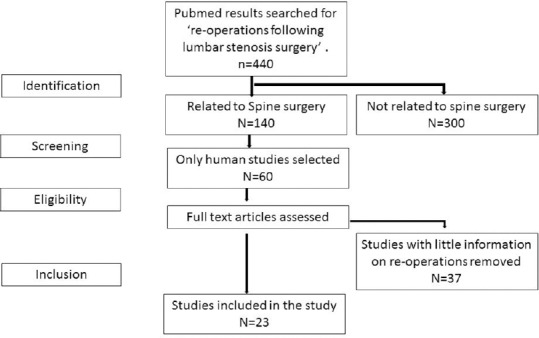
A flow chart showing method of selection of studies for reoperations after spinal stenosis surgery
Table 1.
Existing studies for reoperations following the primary surgery: Lumbar canal stenosis
Results
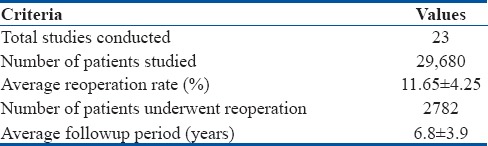
Out of 23 studies conducted, 29680 patients have undergone surgeries for spinal stenosis. 11.65% ± 4.25% (3458 out of 29680) of them underwent reoperations following the primary procedure within a followup period of 6.80 ± 3.90 years [Table 2]. The causes of reoperation were multifactorial ranging from the type of procedure performed, duration of surgery, associated comorbidities, or smoking.
Table 2.
Cumulative results
Further comparing the studies for associated risk factors for restenosis, smoking was found to be the most significant.9 Out of 500 chronic smokers who underwent surgery for spinal stenosis, 81 (16.2%) were found to have undergone revision surgeries. The odds ratio for revision surgery in smokers versus nonsmokers was 2.15 (P = 0.01) indicating that smokers were two times more vulnerable to revision spine surgery after the primary procedure.
Diabetic patients were found to have a higher incidence of revision surgeries compared to nondiabetic group (DG). Although this difference was not statistically significant (P > 0.05), the time interval for revision spine surgery in diabetic patients was significantly low (P = 0.04). The diabetics had more pain (P = 0.04) and neurogenic claudication (P = 0.006) than the control group (CG). The nondiabetics were found to be more satisfied (P = 0.006) and had fewer postoperative complication rates (P = 0.0001).
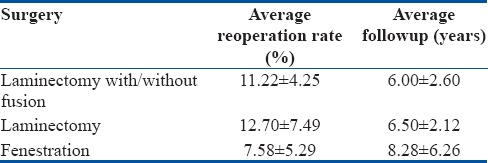
The comparison between the various studies conducted for laminectomy with or without fusion and fenestration surgeries showed that the reoperation rates were higher in isolated decompression procedures. Fenestration surgeries showed an average reoperation rate of 7.58% ± 5.29% in 8.28 ± 6.26 years followup as compared to laminectomy alone (12.70% ± 7.49%, 6.50 ± 2.12 years followup). Laminectomy with or without fusion showed a reoperation rate of 11.22% ± 4.25% in 6.00 ± 2.60 years followup period. The comparative analysis of any of these studies was not significant [Table 3].
Table 3.
Statistical analysis of the existing studies
Discussion
There are a number of enlisted causes that could result in restenosis of a decompressed spinal canal. Some of these are avoidable, and the risk of restenosis can be reduced after lifestyle modification.10 However, a few are genetic, inherited causes and a person has to bear with them and undergo redo surgeries.11,12
Smoking
Overall reoperation rates after lumbar stenosis operation could be multifactorial;1,7,11,13,14 and therefore, there is no particular reason that could be pointed out. However, the presence of recurrence of clinical symptoms must be present to consider the patient as a candidate for revision surgery.10 We define reoperation as a new surgical procedure for spinal stenosis either at the same or another level due to progression or sequel of the previous operation. As per a recent study, smoking has been found to be an independent predictor of reoperation following the lumbar stenosis surgery (odds ratio 2.15, P = 0.01).9 Out of the total patients operated by them, 16.2% had to undergo reoperation within 5 years of surgery.9
Type of surgical procedure
Although it is emphasized in a recent study that surgical decompression gives better symptomatic improvement as compared to nonoperative conservative treatment,15 literature generally described reoperation rates for lumbar stenosis surgery varies between 5% and 23%.1,13,16,17,18,19 Traditional laminectomy has been described as a standard approach for the lumbar stenosis; however, newer minimally invasive approaches have become popular in the past decade. Therefore, it would be interesting to study the revision rates among such population. Jansson et al. reported 11% of revision rate at 10 years after lumbar laminectomy alone or laminectomy with fusion in 9664 patients’ cohort from Sweden, which is the largest cohort available till date.12 However, they have not reported the revision rates in populations who did not have total laminectomy for lumbar stenosis. Similarly, a prospective study by Javid et al. in 170 patients undergoing laminectomy alone or laminectomy with fusion showed that 11 patients (6.5%) underwent reoperations at the end of 11 years followup. On the other hand, Oertel et al.1 have looked up into the clinical results in 133 patients who underwent minimally invasive ULBD for lumbar stenosis, and they found 11.8% reoperation rate with a note of infrequent findings of symptom recurrence and spinal instability in this population.1 Thomé et al. have compared the outcome of 120 consecutive patients who were randomly operated by unilateral laminotomy, bilateral laminotomy or laminectomy; and they found that patients’ satisfaction was superior in the group with bilateral foraminotomy.2 However, comparing the reoperation rates among three groups, it was not statistically different. As per the spine patient outcome research trial in 2013, of the 413 patients who underwent surgical treatment of spinal stenosis, 54 (13%) underwent a reoperation within 4 years.20 Guigui et al. reoperated 38 patients after a primary surgical treatment of lumbar spinal stenosis.21 At a mean followup of 34 months, only 60% had good or very good results. The main causes of failure were postoperative instability and incomplete neurological decompression. According to their report, initial nerve roots decompression was incomplete in 56% of the cases. Therefore, considering the literature review, we can say that reoperation rates may not have direct relation with the type of the surgical procedure.
Decompression without fusion
Decompression with or without fusion may be the factor to consider reoperation. Hu et al. showed 9.5% (n = 449) reoperation rates from 4,722 patients database in the followup period of 4 years.22 They noted that complications from surgery were significantly higher in the fusion and fusion with decompression groups; however, the reoperation rate was not significantly different among individual surgery groups. The incidence of reoperation after back surgery was found to be independent of diagnosis and type of surgery performed. More extensive surgery did not prevent nor predispose a patient to the need for further surgery. On the other hand, Malter et al. have reported their reoperations rates in 6376 patients who underwent lumbar surgery for degenerative conditions in from of decompression alone or decompression with fusions (16%).23 They also noted complications in 18% of fusion patients and 7% of nonfusion patients; however, after adjustment for baseline characteristics, fusion patients had only a slightly greater (and nonsignificant) risk of reoperation (relative risk 1.1) at 5-year followup. Hwang et al. found reoperation rate of 16.3% in individuals undergoing micro-decompression for spinal stenosis in 4 years followup period.24 Deyo et al. in 2011 had concluded that the reoperation rates in patients managed by only decompression procedures are higher than those with arthrodesis. However, these rates were similar at 4 years followup of the patients.25 Aizawa et al. had studied reoperation rates after fenestration surgery in 6998 surgeries with 20-year followup. The overall reoperation rates were 0.8% at 1 year, 2.9% at 5 years, 5.2% at 10 years, 7.5% at 15 years, and 8.6% at >17.7 years. Reoperation rates for those at the same spinal levels were 0.6% at 1 year, 1.7% at 5 years, 2.7% at 10 years, 3.8% at 15 years, and 4.1% at >17 years.26 In another recent study, approximately 10% of individuals had to undergo reoperation after lumbar stenosis surgery.27 About 80% of these revisions were done after 5 years of the primary surgery.27 In this context, we can say that higher rate of perioperative morbidity in fusion group does not correlate with the higher reoperation rates.
Length of postoperative followup
Interestingly, from Sweden database study, it was evident that as the length of postoperative followup increases, reoperation rate also increases to 2%, 5%, 8%, and 11% at 1, 2, 5, and 11 years, respectively.16 However, apart from this study, none of the other study has evaluated reoperation or clinical results periodically. Therefore, although it is predictable that reoperation rate increases on followup; further studies need to focus more on this important issue to reach to definitive conclusion.
Patient's age and comorbidities
Patients’ age or associated comorbidities can also play a major role determining reoperation. A study by Arinzon et al. evaluated their clinical outcome after lumbar stenosis surgery between 62 elderly DG and sex- and age-matched nondiabetic CG at a mean age of 40 months postoperatively.11 Although they found more reoperations in DG group than CG group, it was statistically nonsignificant. However, the time interval for the second intervention was significantly shorter in the DG group. Although, a higher rate of postoperative complication was observed in the DG group, it is concluded that surgical treatment of elderly diabetic patients suffering from spinal stenosis improves quality of life and ameliorates pain. Successful postoperative pain reduction remained the strongest factor associated with patients’ satisfaction. Similarly, another retrospective study by Hee and Wong from Singapore compared clinical outcome and reoperation in 68 patients aged 60 and above who had decompression laminectomy for lumbar spinal stenosis at an average of 8 years after surgery.13 They reported 68% excellent and good, 22% fair and 10% poor results in elderly group with 5 (7.4%) reoperations. They concluded that surgical results of spinal stenosis in the elderly are favorable and comparable to those reported for the general population. An another study by Hansraj et al. in 103 consecutive lumbar spinal stenosis patients with an average age of 65 years showed reoperation rate of 3.9% (n = 4) at 1-year followup which was not changed at 2- to 5-year followup.17 Satisfaction rates for older patients were similar to patients younger than 65 years although physical function scores and severity scores were less. Thus, surgical results or reoperation rates does not depend on age or associated comorbidities of the patient.
Prognostic factors
Risk factors for reoperations in lumbar stenosis surgery were evaluated by Jönsson et al. in their prospective study in 105 consecutive patients who underwent surgical decompression (laminectomy with facet preserving technique).19 During the followup period, 19 patients underwent reoperation; consisting of fusion to treat lumbar pain (n = 4), repeat decompression because of progressive stenosis (n = 13), and repairs in response to surgical complications (n = 2). The results after surgical decompression in patients with central spinal stenosis deteriorated with time. Patients with a preoperative duration of symptoms of <4 years and patients with no preoperative back pain tend to have better surgical outcomes. The reoperation rate was 18% within 5 years. When surgery for spinal stenosis is contemplated, these prognostic factors should be taken into consideration. The “ideal patient” has a pronounced constriction of the spinal canal, insignificant lower back pain, no concomitant disease affecting walking ability, and a symptom duration of <4 years.
Length of postoperative period
Javalkar et al. have retrospectively evaluated several associated factors after the initial lumbar stenosis surgery in 335 patients. They found out 14.9% (n = 50) reoperations after unknown period of followup.28 We believe that over a period of time, reoperation might increase which is similar to the reported literature. In their evaluation, they also reported a higher rate of postoperative complications in patients who underwent decompression with instrumentation (19%) than those with decompression alone (5.5%). However, comparing the reoperation rate between them, it did not show any significant difference (19% vs. 11.8%) which is similar to the published literature. Similarly, they also could not find out any difference in adjacent level disease between these two groups. Moreover, they could not find out any difference in reoperation between patients with single- or multi-level stenosis surgery (13.6% vs. 12.8%). However, their reoperation rate was statistically significantly higher in patients aged 65 years or less (16.9%) than those with 65 years or more (8.9%). In fact, this is a new finding in contrast to previously reported literature that suggested that reoperations are not related with age, sex, or associated comorbidities of patients. We believe further studies should be carried out to reach a conclusion. They have additionally pointed out that around 75% of reoperations were at the index while 25% at adjacent level, which is expected and could be explained by either progression of the disease or instability.
Conclusion
In a nutshell, this is a review on reoperations after surgery for lumbar canal stenosis. Statistical data do not indicate the superiority of a particular type of surgery which reduces the rate of reoperation. The causes for reoperation are inadequate decompression or instability. The literature does not give statistics for these complications in the papers. This is a review analysis of the conducted studies, which is a weak point of the paper. A prospective study shall be able to give a better impression and outcomes of surgery. Smoking is an independent risk factor for revision surgery. Diabetes reduces the time interval between the initial surgery and the revision surgery. Further prospective randomized controlled studies evaluating reoperation and related risk factors after lumbar stenosis surgery are mandatory for this simple but unsolved question.
Financial support and sponsorship
AO Spine Asia Pacific Grant 2017. Modi, Goel, Desai et al. We have been funded by AO spine Asia Pacific in 2017 to carry forward research.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Oertel MF, Ryang YM, Korinth MC, Gilsbach JM, Rohde V. Long term results of microsurgical treatment of lumbar spinal stenosis by unilateral laminotomy for bilateral decompression. Neurosurgery. 2006;59:1264–9. doi: 10.1227/01.NEU.0000245616.32226.58. [DOI] [PubMed] [Google Scholar]
- 2.Thomé C, Zevgaridis D, Leheta O, Bäzner H, Pöckler-Schöniger C, Wöhrle J, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: A randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3:129–41. doi: 10.3171/spi.2005.3.2.0129. [DOI] [PubMed] [Google Scholar]
- 3.Lauryssen C, Berven S, Mimran R, Summa C, Sheinberg M, Miller LE, et al. Facet-sparing lumbar decompression with a minimally invasive flexible MicroBlade shaver® versus traditional decompression: Quantitative radiographic assessment. Clin Interv Aging. 2012;7:257–66. doi: 10.2147/CIA.S32536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang H, Ma L, Yang D, Wang T, Yang S, Wang Y, et al. Incidence and risk factors for the progression of proximal junctional kyphosis in degenerative lumbar scoliosis following long instrumented posterior spinal fusion. Medicine (Baltimore) 2016;95:e4443. doi: 10.1097/MD.0000000000004443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Narverud SF, Ramli NB, Chandran H, Ganesan D. Calcified pseudomeningocele of the lumbar spine: A review. Eur Spine J. 2013;22(Suppl 3):S443–9. doi: 10.1007/s00586-012-2610-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akhaddar A, Boulahroud O, Boucetta M. Nerve root herniation into a calcified pseudomeningocele after lumbar laminectomy. Spine J. 2012;12:273. doi: 10.1016/j.spinee.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Keskimäki I, Seitsalo S, Osterman H, Rissanen P. Reoperations after lumbar disc surgery: A population-based study of regional and interspecialty variations. Spine (Phila Pa 1976) 2000;25:1500–8. doi: 10.1097/00007632-200006150-00008. [DOI] [PubMed] [Google Scholar]
- 8.Waddell G, Kummel EG, Lotto WN, Graham JD, Hall H, McCulloch JA, et al. Failed lumbar disc surgery and repeat surgery following industrial injuries. J Bone Joint Surg Am. 1979;61:201–7. [PubMed] [Google Scholar]
- 9.Bydon M, Macki M, De la Garza-Ramos R, Sciubba DM, Wolinsky JP, Gokaslan ZL, et al. Smoking as an independent predictor of reoperation after lumbar laminectomy: A study of 500 cases. J Neurosurg Spine. 2015;22:288–93. doi: 10.3171/2014.10.SPINE14186. [DOI] [PubMed] [Google Scholar]
- 10.Jönsson B, Strömqvist B. Repeat decompression of lumbar nerve roots. A prospective two-year evaluation. J Bone Joint Surg Br. 1993;75:894–7. doi: 10.1302/0301-620X.75B6.8245078. [DOI] [PubMed] [Google Scholar]
- 11.Arinzon Z, Adunsky A, Fidelman Z, Gepstein R. Outcomes of decompression surgery for lumbar spinal stenosis in elderly diabetic patients. Eur Spine J. 2004;13:32–7. doi: 10.1007/s00586-003-0643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goffin J. Comment with regard to “outcomes of decompression surgery for lumbar spinal stenosis in elderly diabetic patients” (Z. Arinzon et al.) Eur Spine J. 2004;13:38. doi: 10.1007/s00586-003-0644-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hee HT, Wong HK. The long term results of surgical treatment for spinal stenosis in the elderly. Singapore Med J. 2003;44:175–80. [PubMed] [Google Scholar]
- 14.Kelleher MO, Timlin M, Persaud O, Rampersaud YR. Success and failure of minimally invasive decompression for focal lumbar spinal stenosis in patients with and without deformity. Spine (Phila Pa 1976) 2010;35:E981–7. doi: 10.1097/BRS.0b013e3181c46fb4. [DOI] [PubMed] [Google Scholar]
- 15.Malmivaara A, Slätis P, Heliövaara M, Sainio P, Kinnunen H, Kankare J, et al. Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine (Phila Pa 1976) 2007;32:1–8. doi: 10.1097/01.brs.0000251014.81875.6d. [DOI] [PubMed] [Google Scholar]
- 16.Jansson KA, Németh G, Granath F, Blomqvist P. Spinal stenosis re-operation rate in Sweden is 11% at 10 years – A national analysis of 9,664 operations. Eur Spine J. 2005;14:659–63. doi: 10.1007/s00586-004-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hansraj KK, Cammisa FP, Jr, O’Leary PF, Crockett HC, Fras CI, Cohen MS. Decompressive surgery for typical lumbar spinal stenosis. Clin Orthop Relat Res. 2001;384:10–7. doi: 10.1097/00003086-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Herno A, Airaksinen O, Saari T. Long term results of surgical treatment of lumbar spinal stenosis. Spine (Phila Pa 1976) 1993;18:1471–4. [PubMed] [Google Scholar]
- 19.Jönsson B, Annertz M, Sjöberg C, Strömqvist B. A prospective and consecutive study of surgically treated lumbar spinal stenosis. Part II: Five-year followup by an independent observer. Spine (Phila Pa 1976) 1997;22:2938–44. doi: 10.1097/00007632-199712150-00017. [DOI] [PubMed] [Google Scholar]
- 20.Radcliff K, Curry P, Hilibrand A, Kepler C, Lurie J, Zhao W, et al. Risk for adjacent segment and same segment reoperation after surgery for lumbar stenosis: A subgroup analysis of the spine patient outcomes research trial (SPORT) Spine (Phila Pa 1976) 2013;38:531–9. doi: 10.1097/BRS.0b013e31827c99f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guigui P, Ulivieri JM, Lassale B, Deburge A. Reoperations after surgical treatment of lumbar stenosis. Rev Chir Orthop Reparatrice Appar Mot. 1995;81:663–71. [PubMed] [Google Scholar]
- 22.Hu RW, Jaglal S, Axcell T, Anderson G. A population-based study of reoperations after back surgery. Spine (Phila Pa 1976) 1997;22:2265–70. doi: 10.1097/00007632-199710010-00013. [DOI] [PubMed] [Google Scholar]
- 23.Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 1998;23:814–20. doi: 10.1097/00007632-199804010-00015. [DOI] [PubMed] [Google Scholar]
- 24.Hwang HJ, Park HK, Lee GS, Heo JY, Chang JC. Predictors of reoperation after microdecompression in lumbar spinal stenosis. Korean J Spine. 2016;13:183–9. doi: 10.14245/kjs.2016.13.4.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deyo RA, Martin BI, Kreuter W, Jarvik JG, Angier H, Mirza SK, et al. Revision surgery following operations for lumbar stenosis. J Bone Joint Surg Am. 2011;93:1979–86. doi: 10.2106/JBJS.J.01292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aizawa T, Ozawa H, Kusakabe T, Tanaka Y, Sekiguchi A, Hashimoto K, et al. Reoperation rates after fenestration for lumbar spinal canal stenosis: A 20-year period survival function method analysis. Eur Spine J. 2015;24:381–7. doi: 10.1007/s00586-014-3479-4. [DOI] [PubMed] [Google Scholar]
- 27.Nakashima H, Kawakami N, Tsuji T, Ohara T, Suzuki Y, Saito T, et al. Adjacent segment disease after posterior lumbar interbody fusion: Based on cases with a minimum of 10 years of followup. Spine (Phila Pa 1976) 2015;40:E831–41. doi: 10.1097/BRS.0000000000000917. [DOI] [PubMed] [Google Scholar]
- 28.Javalkar V, Cardenas R, Tawfik TA, Khan IR, Bollam P, Banerjee AD, et al. Reoperations after surgery for lumbar spinal stenosis. World Neurosurg. 2011;75:737–42. doi: 10.1016/j.wneu.2010.10.043. [DOI] [PubMed] [Google Scholar]


