Abstract
Background:
Floating knee is a condition resulting from high energy trauma usually associated with minor to life threatening injuries making it challanging to treat There are no studies available in literature describing cross leg sitting and squatting after surgical management of floating knee. This study analyzes prognostic factors, plan of management, functional outcomes (special attention to squatting and cross legged sitting), complications.
Materials and Methods:
52 patients with floating knee injuries treated over a period of 3 years were included in this study. The study followed an algorithmic approach for the management. Femur fractures were fixed before fixing the tibia according to fracture type that was classified by Fraser classification after the stabilization of patient. The mean followup duration was 21 ± 6 months. The outcome was assessed using Karlstrom criteria after bony union.
Results:
The study consists of majority (46) of male. Thirty three patients had some types of significantly associated injury. The mean postoperative range of motion of the knee was observed to be 97° ± 27°. Twenty one patients showed excellent results, whereas 17, 8, and 6 patients had good, fair, and poor results, respectively, as per Karlstrom criteria. Knee pain, stiffness, infection, nerve palsy, delayed union, and nonunion were some of the complications observed. Cross legged sitting was possible in 40 patients and squatting in 31.
Conclusion:
The prognosis of floating knee injury is dependent on factors such as type of fracture, soft tissue condition, and management. Excellent outcomes following these injuries can be achieved with individualized plan of management by multidisciplinary team.
Keywords: Femur fracture, tibia fracture, floating knee, cross legged sitting, squatting
MeSH terms: Femoral fractures, tibial fractures, knee injuries, physical activity
Introduction
The term “floating knee” was first described by Blake and McBride in 1975.1 It is an ipsilateral fracture of the femur and tibia that includes diaphyseal, metaphyseal, and intraarticular regions of the bone. Floating knee injuries occur as a result of a very high-velocity trauma. Road traffic accidents are the most common cause of this type of complex injuries.2 The incidence of road traffic accidents are on the rise and are often associated with complex life-threatening conditions and extensive soft tissue damage. Management of these injuries varies according to the type and extent of bony and soft tissue involvement. Bertrand andAndrés-Cano state “although the exact incidence is unknown, this condition is generally rare,” the incidence is on the rise currently due to the increased trend in high-velocity traumas.3 The largest series reported in literature was 222 patients over 11 years.4
In India, cross legged sitting is an essential part of daily routine activities ranging from sitting in this position for meals, meditation, prayer, work, or studying indicating it's importance. There have been no studies available in literature of floating injuries analyzing the possibility of cross legged sitting after management. Squatting is another aspect that is essential in routine activities as it is a requirement for the use of Indian toilets.
This study appraises the radiological, clinical, functional outcomes (cross legged sitting and squatting possibilities), prognostic factors, postoperative complications.
Materials and Methods
This descriptive study was carried out at a tertiary care university hospital, in India, between January 2013 and January 2016, after approval from ethical committee. A total of 72 patients with floating knee injuries were identified, of which twenty patients were excluded, 12 patients of which underwent a primary conservative amputation procedure.
The study population consisted of skeletally mature individuals (15–69 years) who had floating knee injuries. Patients of a pediatric population with periprosthetic fractures that were conservatively managed or had undergone a primary amputation were excluded from the study [Figure 1]. The fracture injuries were classified according to Fraser classification4 [Figure 2], and Gustilo-Anderson classification was also used to classify open or closed fracture sites.5 All patients were managed by a surgical method of treatment.
Figure 1.
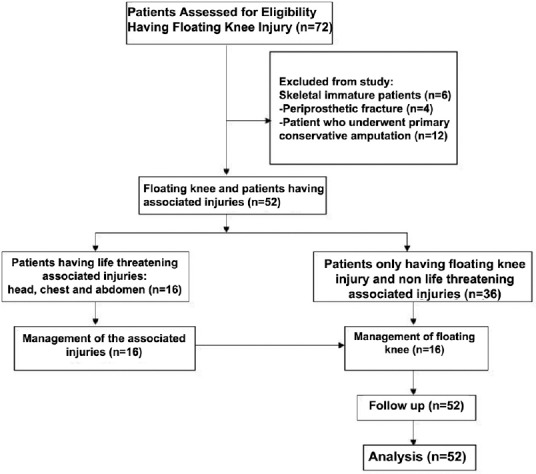
Flow chart of the study design
Figure 2.
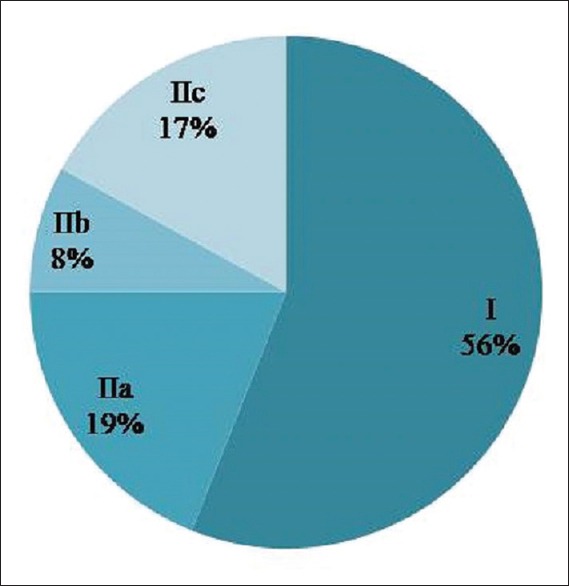
Percentage of cases per Fraser classification
Floating knee injuries resulted from high energy trauma, they were associated with other fractures and a variety of soft tissue injuries. The initial management involved the resuscitation of patients, splinting of fractures, management of open injuries, and traction immobilization by a Bohler Braun splint. Initial wound management, tetanus prophylaxis, and tetanus immunoglobulin were also administered to the patient. A secondary survey was done to rule out other associated injuries. Furthermore, plain radiographs of the chest, pelvis, and affected limbs were taken. In addition, portable ultrasonography of the abdomen and chest was carried out in all the patients to rule out any intraabdominal and chest traumas. In suspected cases of head injury, computed tomography of the brain was done. Patients who had an associated chest injury, head injury, or abdominal injury were managed according to the extent of their injuries before surgical stabilization of any fracture. Immobilization of these patients was done to stabilize the fracture site until definitive fixation could be done. The methods used in these cases include skeletal traction by calcaneal Steinmann pin, posterior stabilization by above knee plaster of Paris slab, and external fixation. Patients treated with initial external fixation were taken into surgery for definitive fixation within 7–10 days of stabilization. In addition, patients were closely monitored for symptoms of fat embolism and suspected patients were referred to and managed by the surgical intensive care unit. Fracture fixation was done once patients were hemodynamically stable. This study followed an algorithmic approach for the management of floating knee injury [Figure 3]. The femur fracture fixation was done before fixation of the tibia.
Figure 3.
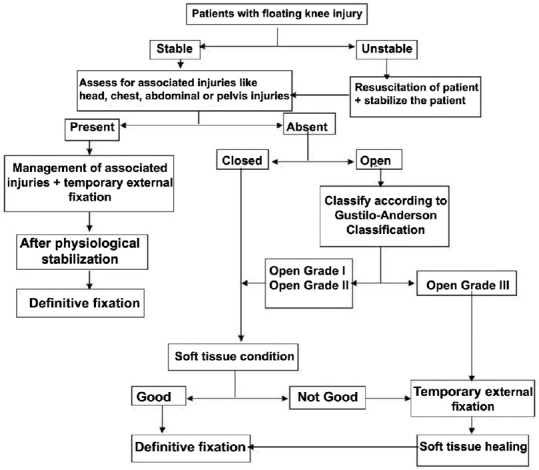
Algorithm for floating knee management
Physiotherapy and mobilization were started as early as possible after surgery depending on the stability of the fracture fixation and stage of wound healing. On the affected limb, patients were kept nonweight bearing for 2–3 months and were followed up until clinical and radiological bony union occurred. Patients with noncomminuted or diaphyseal fractures treated with intramedullary nailing were allowed partial weight bearing with walker at 6 weeks of postoperative period. Fracture union was identified clinically by patient not having pain on palpation at the fracture site and no pain on full weight bearing on affected limb. Union was also determined radiologically when three out of the four cortices were found to be united, and a good amount of callus formation occurred at the fracture site seen on a plain X-ray. Functional assessment and final outcome were measured using the Karlstrom criteria6 after bony union. The final evaluation was based anatomically on when the bony union occurred; however, followups of the patients were taken until the end of the study period to take into account any delayed complications or patient complaints. Data were collected, and significance or association between positive predictive variables and clinical outcomes were analyzed using the Chi-square method within a 95% confidence interval.
The surgeries were performed after informed consent and study was carried out after approval by ethical committee.
Results
52 patients were analyzed, 33 (63%) had a type of associated injury, most common of which was head injury 8 (15.3%). Upper limb injuries 7 (13.4%) and pelvic injuries 6 (11.5%) were also frequently associated with floating knee [Figure 4].
Figure 4.
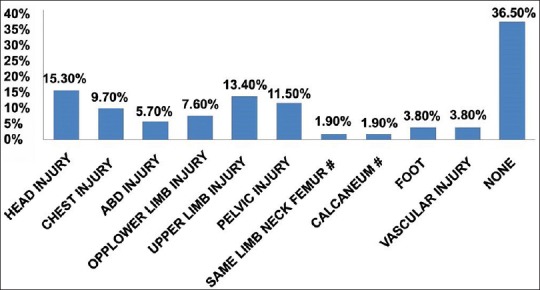
A bar diagram showing percentage of associated injuries in the study (ABD = Abdominal, OPP = Opposite)
The Fraser types were as follows: Type I (n = 29), Type IIa (n = 10), Type IIb (n = 4), and Type IIc (n = 9) [Figure 2]. Out of 52 patients, 46 male and 6 female, with a mean of 31.6 years (range 15-69 years). The right side was involved more frequently as compared to the left in 34 (65%) patients. Forty eight (92%) injuries were due to road traffic accidents and four from a fall.
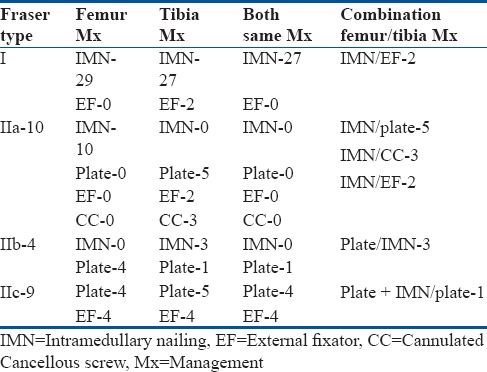
Femur fractures were stabilized using intramedullary nailing in 39 patients, plate fixation in 8 patients, and external fixation in 4 patients. Tibial fractures were stabilized using intramedullary nailing in thirty patients, plate fixation in 11 patients, CC screw in 3 patients, and external fixation in 8 patients. There were 27 patients with intramedullary nailing in both femur and tibia, 5 patients with plating in both, and 4 patients with external fixation in both. Antegrade intramedullary nailing of both bones was the most common technique used in diaphyseal fractures (Fraser Type I). Type I patients were all managed by definitive intramedullary nailing in both the femur and tibia except in two cases where both involved early external fixation and then intramedullary nailing of the femur once patient was stabilized while the tibia external fixation was continued. In fact, all the cases where both femur and tibia were nailed belonged to Type I. In Type IIa, all the combinations for management performed. Most of the fractures of femur were fixed with intramedullary nail, while tibia was fixed with cannulated cancellous screws or plating. There were also two cases involving the nailing of the femur and external fixation of the tibia. In contrast, all the combinations of the femur was plating and tibia nailing were in Type IIb, There was one combination where both femur and tibia were plated. Type IIc fractures involved all the combinations where femur and tibia were both externally fixed and also combinations where both femur and tibia were plated. There was one case in Type IIc that involved not only the plating of the femur but also the nailing of it and the tibia was managed by nailing. This case was seen in a 52-year-old female with an associated intertrochanteric fracture on the same side as the floating knee injury [Table 1].
Table 1.
Management of floating knee patients as per Fraser classification
Thirty one patients had closed fractures and the rest had open fractures. Open fractures were classified as per the Gustilo-Anderson classification (open Grade I (six), open Grade II (seven), open Grade IIIb (six), and open Grade IIIc (two)). There were 12 patients that were managed with early external fixations. These include all eight of the open Grade IIIb and IIIc fractures, two open Grade II, one open Grade I, and one close fracture. The patient with a close fracture had the only bilateral floating knee injury in this study and had an associated pelvic injury. The outcomes of patients with early external fixations were 50% poor, 33.33% fair, and 16.67% good. All the poor outcomes from the entire study group were from these patients. None had excellent results. In total, there were four cases where the early external fixation of both the tibia and femur was continued as definitive fixation; all of these had poor outcomes. Out of these, two patients had associated vascular injuries that were both classified as IIc under Fraser Classification. The patients were referred for vascular surgery where one of the patients was managed by revascularization by saphenous vein autograft and the other by embolectomy. The other two patients were of open Grade IIIb and had associated injuries of radius-ulna fractures and chest injury, respectively. In the remaining open Grade IIIb injuries, two received definitive fixation of the femur with intramedullary nailing and tibia was externally fixed, whereas two received definitive fixation of both femur and tibia by plating or nailing [Figures 5 and 6].
Figure 5A.
Plain radiograph of knee joint with leg and thigh of a 20-year-old male patient with a history of road traffic accident showing (a) floating knee injury of open Grade II without distal neurovascular deficit (case 1 preoperative x-ray) (b) Immediate postoperative radiograph of surgical management of floating knee
Figure 6A.
Plain radiographs anteroposterior and lateral views of knee joint with leg and thigh of a 21-year-old male patient showing floating knee injury open grade IIIb Gustilo Anderson (preoperative x-ray case 2) (b) Immediate postoperative x-ray of same patient showing surgical management of floating knee
Figure 5B.
(a) Plain radiograph of knee joint anteroposterior and lateral views with leg and thigh at 3 years followup of same patient showing surgical management of floating knee (b) Clinical photographs of same patient at 3 years followup showing range of motion
Figure 6B.
(a) Plain radiograph of knee joint with leg and thigh anteroposterior and lateral views of same patient at 2½-years followup showing fracture well united with implant in situ (b) Clinical photographs of same patient showing range of motion at 2½ years followup
The average time for union was 22 weeks (range 16-32 weeks). Patients were followed up at 1, 3, 6 months, and then a final followup. The average followup was 21 ± 6 months. The mean knee range of motion observed was 97° ± 27° [Table 2].
Table 2.
Mean range of motion of knee observed for each Fraser type

Functional assessment and final outcome were measured according to the Karlstrom criteria [Table 3].6
Table 3.
End result according to Karlstrom criteria

Knee pain was the most common complication experienced by 26 (50%) patients [Figure 7]. Knee stiffness occurred in nine patients. Knee stiffness was considered in patients with the range of motion of knee ≤75°. Knee stiffness was seen more in open grade fractures as compared to closed fracture (P < 0.05). However, knee pain was the most common complication of the study but was not associated with open or closed nature of injury (P > 0.05). Early infection was seen in seven patients of which three had poor outcomes, one had fair, and three had good. Five of these patients were managed by debridement of the wound after the infection was detected initially and antibiotics were intravenously administered, according to the culture and sensitivity of the isolated organism, for 15 days. Afterward, oral antibiotics were continued for 4 weeks. Dry dressings were done regularly until sutures were removed. No patient required implant removal or implant exchange. Common peroneal nerve palsy was seen in four patients. One patient had poor outcome, two had fair, and one good. The patient with the good outcome was a 16-year-old male who had an associated acetabular fracture which was fixed 5 days after his floating knee injury was managed. Complications of the acetabular repair caused his neuropraxia, but patient recovered after 6 months and was able to walk. Delayed union was seen in two patients and nonunion in one patient in this study. Bony union was achieved around 12 months in both patients with delayed union. The patient with nonunion was reoperated with bone grafting (autograft) and intramedullary fixation. In general, complications were seen more in Type II Fraser which was significant (P < 0.05). Complications were also more prominent in open fractures (P < 0.05). The average duration of a hospital stay was 11.32 ± 6.16 days for these patients [Figure 8]. Cross legged sitting was found to be possible in forty patients (76.92%). Out of all patients, majority (27 patients) were from Fraser Type I. However, squatting was possible only in 31 patients (59.62%), in which 25 patients were from Fraser Type I.
Figure 7.
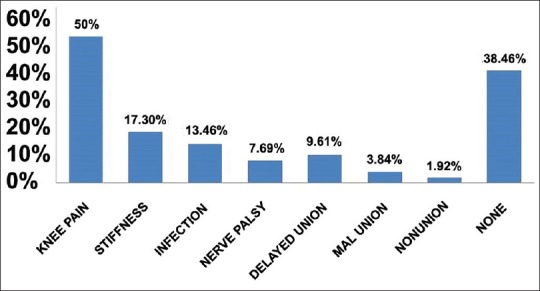
A bar diagram showing percentage of each complication in the study
Figure 8.
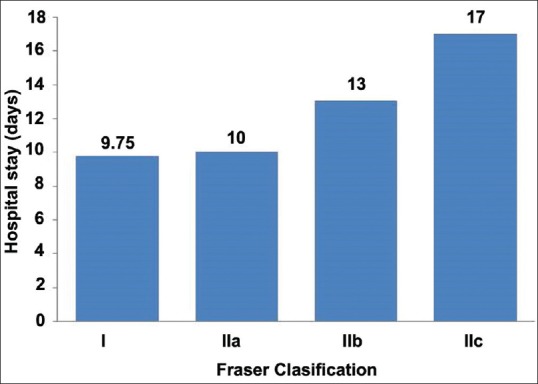
A bar diagram showing mean hospital stay as per Fraser classification
Discussion
Floating knee injuries result from high energy trauma, in which patients sustain significant and occasionally life-threatening injuries. In a recent study by Kao et al.,7 floating knee has been reported to be associated with head injuries in 26% of the study population in contrast to this study where 15.3% had head injuries. Furthermore, Kao et al.'s study reported that 8.8% patients had pelvic injuries and 54.8% had contralateral extremity injury, whereas this study shows about 11.5% and 13.4% of patients with pelvic and contralateral limb injuries, respectively. Currently, the reported mortality rate ranges from 5% to 15% reflecting the impact of associated injuries.8 This study did not report any mortality in patients with floating knee.
A recent study by Goel et al. reports road traffic accidents as the most common cause of lower limb injuries.2 This finding is in accordance with this study. However, they have reported that injury is more common in the left lower limb as compared to right though the value was not significant, whereas this study shows that injuries to right lower limb are more common.
There are many studies in literature suggesting internal fixation of both the fractures of floating knee should be done as early as possible.9,10 Ratliff found that internal fixation of both fractures was less likely to cause the development of knee stiffness and lessen the duration of hospital stay.11 Ostrum treated patients with retrograde femoral nailing and antegrade tibia nailing through 4 cm medial parapatellar incision.12 The average time to union of femoral fracture was 14.7 weeks and for tibial fracture was 23 weeks. This study shows an average union time of 22 weeks. They opined that this method was an excellent treatment option.
In a prospective study by Rethnam et al., 29 patients with floating knee injuries were followed up over a period of 3 years.13 Intramedullary nailing was done in both femur and tibia fractures in 20 patients, whereas, in this study, intramedullary nailing in both was done in 27 patients. Other modalities of treatment were used in the remaining nine patients. Thirty eight associated injuries were noted in 29 patients. Complications noted were knee stiffness in four patients, foot drop in one patient, delayed union of tibia in two patients, and superficial infection in one patient. In comparison, this study had nine patients of knee stiffness, four with foot drop, two with delayed union, and seven had infections. According to the Karlstrom criteria, results were excellent in 15 patients, good in nine, acceptable in two, and poor in three; in contrast, this study had 21, 17, 8, and 6, respectively.
As per Fraser Classification, 71.5% of patients were of Type I, 8.2% of Type IIa, and 11.6% of Type IIc which was in concurrence with the findings of this study. At 12 month followup, of 116 patients, the results were excellent in 20% of the patients, good in 33%, fair in 30%, and poor in 17%. In contrast, this study had 40%, 33%, 15%, and 12%, respectively. Feron et al.14 noted that the Karlstrom score was significantly dependent on the level of femoral fracture. They found that 66.2% of good or excellent results were in diaphyseal fractures while that percentage dropped to 12.5% in distal third femoral fractures. In this study, the management of femur fractures significantly affected the outcomes as per the Karlstrom criteria; femoral intramedullary nailing was associated with excellent outcomes (P < 0.05) as there were more excellent outcomes with intramedullary nailing than compared with other methods of management. In contrast, there was no significant association found between tibial fracture management and outcome (P > 0.05) of the floating knee injuries. Patients with Fraser Type I floating knee injuries were also associated with significant low complication rate (P < 0.05). Furthermore, patients with closed fractures had more excellent outcomes than open fractures (P < 0.05). Squatting in patients managed by intramedullary nailing were significantly more than in other forms of management (P < 0.05). Furthermore, cross legged sitting in patients treated with intramedullary nailing was more than in other management (P < 0.05). The age of the patient did not affect the outcomes of the floating knee injuries (P > 0.05). In addition, there is no significant association found between the associated injury and range of motion of knee observed in patients with floating knee injuries in this study (P > 0.05).
Conclusion
Floating knee injury is more than just an ipsilateral fracture of the femur and tibia with associated life-threatening conditions. It should be managed by step wise systemic approach according to patient's associated inuries. Definitive fixation should be delayed until the patient's condition is suitable for surgery. Mobilization should be started as soon as possible keeping the patient nonweight bearing after the fixation of fractures for better functional outcomes. Patients treated with intramedullary nailing have better outcomes with low complications rate compared to other methods of management. Hence, excellent clinical and functional outcomes can be achieved with individualized planning of treatment which is dependent on the patient's general condition, type of fracture, and severity of soft tissue injury by an experienced multidisciplinary team instead of a fixed definite management for all patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Blake R, McBryde A., Jr The floating knee: Ipsilateral fractures of the tibia and femur. South Med J. 1975;68:13–6. [PubMed] [Google Scholar]
- 2.Goel SA, Bhavsar NM, Makwana H, Lil NA, Patel PR. Epidemiology and patterns of lower limb injuries at a tertiary care hospital in Ahmedabad? Int J Med Res Rev. 2015;3(5):490–496. doi: 10.17511/ijmrr.2015.i5.094. [Google Scholar]
- 3.Bertrand ML, Andrés-Cano P. Management of the floating knee in polytrauma patients. Open Orthop J. 2015;9:347–55. doi: 10.2174/1874325001509010347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fraser RD, Hunter GA, Waddell JP. Ipsilateral fracture of the femur and tibia. J Bone Joint Surg Br. 1978;60-B:510–5. doi: 10.1302/0301-620X.60B4.711798. [DOI] [PubMed] [Google Scholar]
- 5.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 6.Karlström G, Olerud S. Ipsilateral fracture of the femur and tibia. J Bone Joint Surg Am. 1977;59:240–3. [PubMed] [Google Scholar]
- 7.Kao FC, Tu YK, Hsu KY, Su JY, Yen CY, Chou MC, et al. Floating knee injuries: A high complication rate. Orthopedics. 2010;33:14. doi: 10.3928/01477447-20091124-04. [DOI] [PubMed] [Google Scholar]
- 8.Adamson GJ, Wiss DA, Lowery GL, Peters CL. Type II floating knee: Ipsilateral femoral and tibial fractures with intraarticular extension into the knee joint. J Orthop Trauma. 1992;6:333–9. [PubMed] [Google Scholar]
- 9.Dwyer AJ, Paul R, Mam MK, Kumar A, Gosselin RA. Floating knee injuries: Long term results of four treatment methods. Int Orthop. 2005;29:314–8. doi: 10.1007/s00264-005-0679-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bansal VP, Singhal V, Mam MK, Gill SS. The floating knee 40 cases of ipsilateral fractures of the femur and the tibia. Int Orthop. 1984;8:183–7. doi: 10.1007/BF00269914. [DOI] [PubMed] [Google Scholar]
- 11.Ratliff AH. Fractures of the shaft of the femur and tibia in the same limb. Proc R Soc Med. 1968;61:906–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Ostrum RF. Treatment of floating knee injuries through a single percutaneous approach. Clin Orthop Relat Res. 2000;(375):43–50. doi: 10.1097/00003086-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Rethnam U, Yesupalan RS, Nair R. The floating knee: epidemiology, prognostic indicators and outcome following surgical management. J Trauma Manag Outcomes. 2007;1:2. doi: 10.1186/1752-2897-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feron JM, Bonnevialle P, Pietu G, Jacquot1 F. Traumatic floating knee: A review of a multi-centric series of 172 cases in adult. Open Orthop J. 2015;Suppl 1 M11:356–60. doi: 10.2174/1874325001509010356. [DOI] [PMC free article] [PubMed] [Google Scholar]






