Abstract
Background
The outcome of breast cancer treatment largely depends on the timing of detection. The health promotion interventions have an immense contribution to early detection and improved survival. Therefore, this review aimed to provide evidence on the efficacy of the health promotion interventions to increase the uptake of breast cancer screening and to develop effective interventions targeting women.
Methods
Online databases (PubMed/MEDLINE/PubMed Central, Ovid/MEDILINE, EMBASE, Web of Science and Google Scholar) were searched for studies published between January 2005 and January 2017. A quality coding system was assessed using Cochrane checklists for randomized controlled trial (RCT) and Downs and Black checklists for non-RCT. The score was rated for the included articles by each researcher independently and the average score is given accordingly. This study was registered in PROSPERO as [PROSPERO 2017: CRD42017060488].
Results
The review dovetailed 22 studies. Thirteen studies (59.10%) were conducted in the Unite States, 4 in Iran (18.18%), 2 in India (9.09%) and 1 each in Turkey, Saudi Arabia and Israel. The interventions were classified as ‘individual-based’, ‘community-based’, ‘group-based teachings and training’ and ‘behavioral model based’. The majority of the studies showed favorable outcomes after health promotion interventions, including improvements in women’s view of breast screening, breast self-examination and knowledge of breast screening.
Conclusion
The review confirmed that most of the health promotion interventions targeting women boosted the breast screening in one or another way. However, the limited quality of the included studies showed that further research is needed to improve the trials in the next future.
Introduction
The global burden of breast cancer in women is enormous in the developed and the developing world. It is estimated that over 508 000 women were died in 2011 globally due to breast cancer. Its incidence is increasing in the developing world due to increased life expectancy, urbanization and adoption of western lifestyles.1 Although breast cancer is thought to be a disease of the developed world, almost 50% of breast cancer cases and 58% of deaths occur in less developed countries.2 According to the American Cancer Society in 2011, approximately 230 480 females in the United States were diagnosed with breast cancer. The death toll for that same year was estimated at 39 520 deaths.3
Breast cancer survival rate varies in various parts of the world. It is over 80% in North America and around 60% in Sweden and Japan but below 40% in low-income countries.2 The very low survival rate in less developed countries could be marked by a lack of awareness and the lack of early detection programs, which results in a high proportion of women presenting with late-stage disease, as well as by the shortage of adequate diagnosis and treatment facilities.1,2
Various risk factors for breast cancer have been well-documented.4 Prolonged exposure to endogenous estrogens such as early menarche, late menopause and late age at first childbirth and behavior-related factors such as oral contraceptive and hormone replacement therapy lead women to breast cancer.4–6 In fact, the variation of incidence between developed and developing countries can partly be explained by dietary effects combined with later first childbirth, lower parity and shorter breast feeding as well as the effect of globalization.7–9
A holistic approach that integrates prevention of modifiable risk factors for both breast cancer and other non-communicable diseases includes promoting a healthy diet, physical activity, control of alcohol intake, overweight and obesity could eventually have an impact in reducing the incidence of breast cancer in the long term.10,11
Many literatures confirmed the improvement in breast cancer outcome after self-examination, early detection, early diagnosis and mammography screening method.12 Mammography screening is very complex and resource intensive and no research of its effectiveness has been conducted in low resource settings.13
Therefore, this systematic review helps to provide evidence on the efficacy of health promotion interventions on breast cancer screening uptake targeting women in the various parts of the world.
Methods
Data sources, search engines and key words
A comprehensive search was carried out using PubMed/MEDLINE/PubMed Central, EMBASE, Ovid/MEDILINE, Web of Science and Google Scholar. Search terms were ‘breast’ AND ‘cancer’ AND ‘behavioral’ AND ‘intervention’ OR ‘health promotion’ AND ‘mammography’ AND ‘screening’ AND ‘uptake’. Studies published as of January 2005–2017 were searched. Reference lists of included studies were also scanned to identify additional relevant papers. All articles were published in English language. Finally, a total of 22 articles were identified. We limited our review to start from 2005 since the previous review was included the articles up to 2005 in one or another way.14 (((((((health[tiab]) AND promotion[tiab]) OR education[tiab]) OR intervention[tiab]) AND breast[tiab]) AND cancer[tiab]) AND screening[tiab]) AND uptake[tiab]
Study selection
Inclusion and exclusion criteria
All published eligible research articles in past 12 years (as of January 2005–2017) were included. Criteria for the inclusion of articles were: (i) articles that provided behavioral intervention or health promotion and/or education intervention to increase uptake of breast cancer screening were included; (ii) eligible participants were women of any age groups; (iii) the study involved experimental or quasi-experimental designs. The study sought to improve breast cancer screening rates and/or breast cancer knowledge and screening intentions and/or self-examinations. Exclusion criteria (i) focused on survivors of breast cancer (biomedical treatment and rehabilitation). (ii) Studies that focused on assessment/descriptive research, non-intervention studies, drugs research and studies that did not report valid outcome measures. All age groups were included in this study review since the recommendation of cancer screening test varies in developing countries to developed countries; even there is even no guideline in some countries. Two investigators then independently reviewed all located articles to confirm whether inclusion criteria were met. The rest investigators also reviewed to check its consistency.
Synthesis of results and quality assessment
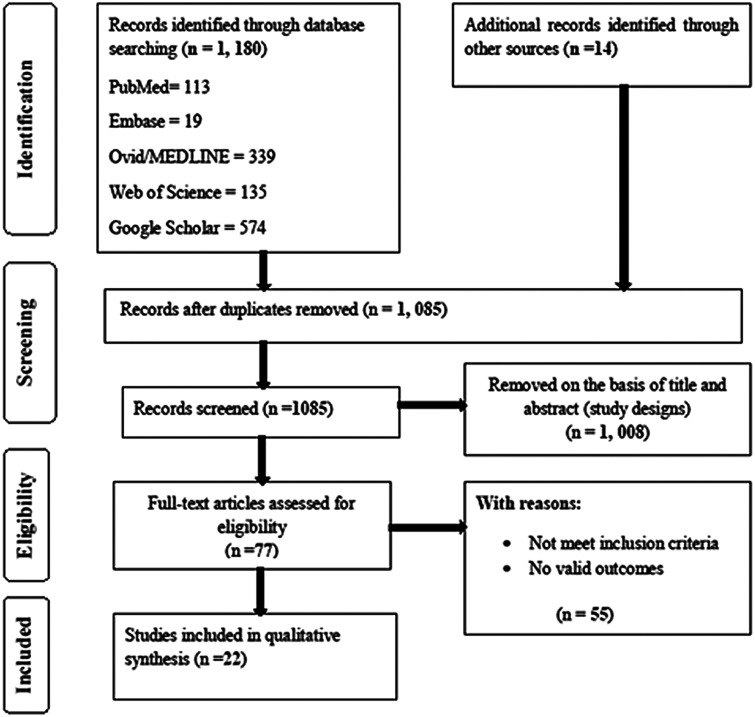
In this systematic review, the authors followed the PRISMA statement rule.15 The authors reviewed all abstracts for inclusion. In cases of doubt based on abstracts, the articles were included for full-text articles review. The authors independently reviewed all full-text articles to confirm whether inclusion criteria were met or not. The data were synthesized in two ways: first, the study design and intervention strategies were presented for all 22 studies that met inclusion criteria. Second, the findings of each study were analyzed. The quality assessment/outcome measure criteria were imposed and the evidence on intervention effectiveness was reported for a subset of studies that reported valid outcome measures as indicated in the PRISMA flow diagram of studies15 (figure 1). Study designs were classified into randomized controlled trials (RCTs; including cluster RCT and randomized controlled crossover trial), quasi-experimental study or non-equivalent control group. In order to present reliable evidence on intervention effectiveness, quality assessments were conducted following the criteria Data Collection Checklist from the Cochrane EPOC guidelines.16 The Jadad scoring system was applied to the assessment of the quality of the included RCTs17 and the feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomized studies of health care interventions to non-RCTs.18 Finally, the interventions were classified as ‘individual-based’, ‘community-based’, ‘group-based teachings and training’ and ‘behavioral model based.’
Figure 1.
PRISMA flow diagram for breast cancer screening articles’ selection and evaluation
Results
The initial literature search resulted in 1194 records through database searching for a total of 1085 unique citations. Of the 77 abstracts, 22 studies were included in this review. Ten were RCTs and 12 Quasi-RCT and non-RCT. A systematic search was detailed in PRISMA flow diagram as indicated in figure 1. The majority of the study (59.10%) were conducted in the United States (13/22), 4 in Iran (18.18%), 2 in India (9.09%) and 1 each in Turkey, Saudi Arabia and Israel (13.64%). Half of the studies were conducted at the community level and one at a religious institution. Majority of study populations were migrant women. The intervention period ranges from 3 months to 8 years with a total sample size of 16 231. The individual sample ranges from 67 to 5144. Diverse intervention strategies were used including phone calls, framed messages, training, lectures, self-test instructions, videos, DVD, pamphlets, booklets, flip charts, demonstrations, group discussions, audiovisuals, education by lay health workers, home-based education and home visits, cultural promoters education, social workers workshops, model-based personal education and screening campaigns. Most studies used multiple strategies (table 1). The quality of RCTs was assessed using Jadad method17 and Downs and Black checklists18 were used non-RCT. The rate was given using the scores 1–5. However, the RCTs scored 2 or 3, pointing that the RCTs included in this review, but, cannot be classified as being of the highest quality and are therefore subject to some degree of bias (table 2) and low quality was reported for non-RCT in table 3.
Table 1.
Characteristics of health promotion intervention studies and summary of findings
| First author & year | Country | Setting | Study population | Study design and sample size | Intervention and its descriptions | Outcome (Intervention vs. control, if applicable) |
|---|---|---|---|---|---|---|
| Abood et al. (2005)19 | USA | Population based | Women | Nonequivalent experimental design; 1104 | Phone calls and framed messages for intervention groups (Two female staff members on site who received all phone inquiries at the experimental public health unit and delivered the scripted loss-framed message telephonically.) | Odds ratio [OR] = 1.914, χ2 = 7.48 [95%CI 1.20–3.05], P = 0.0063 |
| Rao et al. (2005)24 | India | Community based | Rural women | Non-randomized intervention study; 360 | Health education on breast cancer and BSE by trained health workers. | Self-examination of the breast increased from 0 to 93% (z = −15.807; P< 0.001) |
| Fry et al. (2005)34 | USA | School based | Female students | Randomized education intervention study; 197 | 90 min intervention consisted of an essay, lecture, video portraying of breast cancer, group discussions, self-test and instructions on performing BSEs for a total of 48 h. | BSE a part of a regular routine (r = 0.57, P = 0.001) |
| Consedine et al. (2007)21 | USA | Community based | Black and white women | Intervention study; 5144 | Telephone intervention, education and training | Intervention vs. Control = 65.6% vs. 48.9% |
| Vernon et al. (2008)50 | USA | Population based | women veterans | RCT; 184 | A folder containing (1) a set of four educational booklets, (2) a letter for the woman to discuss mammography with health-care provider, and (3) a pamphlet about mammography screening through the Veterans Administration | No significant difference between intervention group and control group (P>0.05) |
| Gupta et al. (2009)35 | India | Community based | Women | Pre-post Intervention study; 1000 | Lecture, pamphlets, flip charts and demonstration of the five step method of BSE using audio-visual aids were administrated. | 90.7% practiced (BSE) compared with 0% pre-test. and over all 53% vs. 43% of BSE practice |
| Nguyen et.al. (2009)25 | USA | population based | Vietnamese-American women | RCT; 1100 | The intervention group received two LHW educational sessions and two telephone calls. Both groups received targeted Media education. | Mammography use OR = 3.14 (95% CI = 1.98, 5.01) P < 0.001) |
| Kim et al. (2009)30 | USA | Community based | Korean women | Quasi-experimental study; 300 | Stage model based 45-min interactive breast cancer early screening health education session (GO EARLY) in mammography use. | No statistically significant intervention effect was noted on upward shift in stage of readiness for mammography use post intervention (P > 0.05) |
| Lindberg et al. (2009)20 | USA | Health care setting | Women | RCT, 616 | A 30–45 min individual counseling session featuring BSE instruction, training and practice with silicon models, identification of barriers to BSE, and problem-solving. This intervention was followed by two brief follow-up telephone calls. | BSE intervention (0–59% vs. 0–12.2%, P< 0.001) |
| Akhtar et al. (2010)26 | Saudi Arabia | Health care setting | Arabic women | Quasi-experimental study; 1766 | Breast screening program/campaigns via media channels, newspapers, exhibitions, lectures, information stalls, and posters. Awareness with interactive educational sessions. | 18% of the total population participated in mammogram screening, with high recall rate (31.6 %) |
| Arshad et al. (2011)37 | USA | Community based | American-Arabic women | Quasi-experimental study; 100 | Educational interventions are delivered by community health workers at their home together with their adult female family members | BSE and mammogram use regardless of their language preference [OR = 0.15; 95% CI = 0.04–0.50; (OR = 0.15; 95% CI = 0.04, 0.54, P < 0.05)] |
| Cohen et al. (2010)38 | Israel | Community based | Israeli-Arabic Women | Quazi experimental controlled before and after design; 67 | A religious and cultural promoter’s involved training was given for six months by trained social worker on culture-specific barriers and misconceptions. | Intervention group vs. control group (48 % vs. 12.5%) |
| Bowen et al. (2011)23 | USA | Population- based | women | RCT; 1354 | Telephone calls.; Web/Internet intervention | Mammography in the last year intervention (69–82% vs. 71% as it is) and BSE Intervention (40–62% vs. 41–41%) |
| Engelman et al. (2011)22 | USA | Health care setting | Women | RCT, N = 290 | One to one education delivered in person by community health workers. Follow-up telephone calls. | Intervention group vs. control (25–30% vs. 15% to no change ) |
| Hajian et al. (2011)31 | Iran | Community based | Women | RCT; 100 | HBM constructs based intervention (well-known psychological theories health education for breast cancer screening) | Intervention group vs. control [41–82%; vs. 31–62%; P = 0.021 and (x2= 5.6, P = 0.12)] |
| Ayash et al. (2011)27 | USA | Community based | Women | Quasi-experimental study; 597 | Workshops, community-based participatory approach and cultural responsiveness trainings sticking to individual level risks in Arabic language. | 68% reported increased understanding of cancer screening, and 29% increase in screening |
| Dallo et al. (2011)38 | USA | Health care setting | Women | Quasi-experimental study, 866 | Bilingual educational intervention along with physical examination and screening | Cancer knowledge increased after intervention compared with prior to the intervention (P<0.05) |
| Eskandari-Torbaghan et al. (2014)28 | Iran | University | Female Staffs | Randomized controlled trial; 130 | Educational intervention and training based on health belief model (perceived susceptibility, perceived benefits, and perceived barriers as well as in practice) | Behavior scores increased by 18% [1.21 (±2.54) vs. 0.15(±2.94), P < 0.05] |
| Khalili et al. (2014)39 | Iran | Community based | Women | Quasi experimental study, 144 | Three sessions of training were held for case group and every session contained 1 h training. | Cases to control mean score of knowledge improved (11.7–21.81; P < 0.001) |
| Rahman et al. (2014)33 | USA | Religious institutions | Korean Americans Women couple | RCT; 428 | The intervention group slogan was ‘Healthy Family, Healthy Wife’ and the control group slogan was ‘Healthy Family, Healthy Diet’ emphasize on breast screening or healthy diet. The intervention group 30-minute Korean-language DVD on breast screening, group discussion immediately after the video; couple to complete a discussion activity at home | There is no significant difference between the two groups (P > 0.05). Both intervention groups have significantly increased (P<0.05) |
| Taymoori, et al. (2015)32 | Iran | Community based | Iranian women | RCT; 184 | Health belief model and theory of planned behavior based health education | A significant intervention effect was identified (P < 0.0001) |
| Tuzcu et al. (2016)29 | Turkey | Community based | Migrant women | Quasi-experimental study; 200 | Health behavior models based training in BSE and mammography was displayed visually in the film. TRAINING: demonstrated proper palpation using the breast model. Two different reminder cards BSE card, breast cancer screening methods card) and an invitation card and demonstrated proper palpation using the breast model | Increased the rate of BSE 0.8 times and the rate of mammography 0.7 times. An increase of each unit in health motivation increased the rate of clinical breast examination 1.3 times and the rate of mammography 1.5 times |
Table 2.
Jadad assessment criteria for quality assessment of RCTs
| Articles | Jadad quality criteria | Total scores | ||||
|---|---|---|---|---|---|---|
| Randomization | Method of Randomization described | Double blinded | Method of double blinded described | Withdrawals and dropouts described | ||
| Bowen et al. (2011)23 | 1 | 1 | NR | NR | 1 | 3 |
| Engelman et al. (2011)22 | 1 | 1 | NR | NR | 1 | 3 |
| Eskandari-Torbaghan et al. (2014)28 | 1 | NR | NR | NR | 1 | 2 |
| Fry (2005)34 | 1 | 1 | NR | NR | 1 | 3 |
| Hajian et al. (2011)31 | 1 | NR | NR | NR | 1 | 2 |
| Lindberg et al. (2009)20 | 1 | 1 | NR | NR | 1 | 3 |
| Rahman et al. (2014)33 | 1 | 1 | NR | NR | 1 | 3 |
| Vernon et al. (2008)50 | 1 | NR | NR | NR | 1 | 2 |
| Taymoori et al. (2015)32 | 1 | 1 | NR | NR | 1 | 3 |
| Nguyen et al. (2009)25 | 1 | 1 | NR | NR | 1 | 3 |
Note: 1= Yes; 0 = No; NR, not reported.
Table 3.
Shows downs and black checklist for assessing the quality of non-randomized trials and quazi-experimental studies
| Articles | Downs and black criteria for non-RCT | Total score (Total points/27) | ||||
|---|---|---|---|---|---|---|
| Reporting (10 points) | External validity (3 points) | Bias (7 points) | Confounding (6 points) | Power (1 point) | ||
| Abood et al. (2005)19 | 8 | 1 | 3 | 3 | 0 | 0.56 |
| Akhta et al. (2010)26 | 4 | 2 | 2 | 3 | 0 | 0.41 |
| Arshad et al. (2011)37 | 6 | 1 | 4 | 2 | 0 | 0.48 |
| Ayash et al. (2011)27 | 7 | 1 | 2 | 2 | 0 | 0.44 |
| Cohen (2010)36 | 6 | 1 | 3 | 2 | 0 | 0.44 |
| Consedine et al. (2007)21 | 5 | 1 | 3 | 1 | 0 | 0.37 |
| Dallo et al. (2011)38 | 7 | 3 | 3 | 4 | 0 | 0.63 |
| Gupta et al. (2009)35 | 7 | 3 | 4 | 4 | 0 | 0.67 |
| Khalili et al. (2014)39 | 7 | 1 | 3 | 2 | 0 | 0.48 |
| Kim (2009)30 | 6 | 1 | 3 | 2 | 0 | 0.44 |
| Rao et al. (2005)24 | 7 | 2 | 4 | 2 | 0 | 0.52 |
| Tuzcu et al. (2016)29 | 7 | 1 | 3 | 2 | 0 | 0.48 |
Note: 1= Yes; 0 = No; 0 = unable to determine.
In this review, multiple and highly diversified interventions were included. Thus, explaining or estimating the effects of each intervention strategy might be difficult in such cases. Therefore, evidence that supports the overall effectiveness of the intervention programs and strategies were reported instead of individual interventions. The highlight of each intervention was discussed as follows.
Individual-based interventions
Phone calls and message-framed interventions
A study from USA found that there was dramatically significant increase in mammography use among medically un- or underinsured women to support the evidence of loss-framed message and phone calls ([OR] = 1.914 [95%CI 1.20–3.05], P =0 .0063).19 Similarly, the studies from Portland Oregon and Iran, indicated that phone calls with lay health advisors and phone call with education intervention had significantly increased in interventional group and correlated with making breast self-examination (BSE) as a part of a regular schedule (r = 0.57, P = 0.001) and with performing BSEs on an irregular basis (r = 0.38, P = 0.02).20,21 Health education delivered in person (one to one education) by community health worker through follow up telephone calls and web based intervention had significantly increased the screening uptake.22,23
Community-based interventions
A community-based educational intervention through demonstration of BSE stressing on thoroughness and the recommended technique significantly increased the overall awareness regarding breast cancer screening (z = −15.807; P < 0.001) as well as in the performance of self-examination of the breast increased from 0% to93% in Indian women.24 In contrast, an intervention through the targeted component consisted of a folder containing educational booklets, a letter for the woman from health-care provider, and a pamphlet about mammography screening services had resulted in no significant difference between intervention group and control group by Cox modeling; however, analysis using logistic regression produced odds ratios (ORs) that were consistently higher than the corresponding hazard rate ratios for both coverage and compliance (ORs = 1.15–1.29).21
Integrating multiple methods to convey breast cancer screening campaign such as newspapers, exhibitions, lectures, information stalls and posters had significantly increased mammography use in 2009 study (OR= 3.14 (95% CI = 1.98, 5.01) and in numerical screening values.25–27
Group-based teachings and training
Health education model-based interventions
Health belief model and theory of planned behavior based health education on BSE and mammography displayed visually in the film and demonstrated proper palpation using the breast model increased behavior scores by 18% (1.21 (+ 2.54) vs. 0.15(+2.94), P < 0.05).28,29 However, stage model based interactive breast cancer early screening health education session (GO EARLY) in mammography use had no statistically significant effect on the upward shift in stage of readiness for mammography use post intervention (P > 0.05) in Korean women, USA and other countries like Iran.28,30–32
Interventions using video, visuals and audio-visuals
The intervention including couples vs. diet emphasizing the importance of the husband’s support in promoting family health by encouraging breast cancer screening or healthy diet through mass media plus DVD plus late group discussions at home did not show significant effect in screening (P > 0.05).33,34 An Indian study revealed the use of lecture, pamphlets, flip charts and demonstration of the five-step method of BSE using audio-visual increased BSE practice by 90.7% compared to 0% pre-test and the BSE practice overall increment was 53–43%.35
Religious, cultural promoters and lay workers
A study from Israel on Arabic women found that culture-based interventions increased the rate of attending for clinical examination and mammography [intervention group vs. the control group (48% vs. 12.5%)].36 The training involving both religious and cultural health promoters by trained social and community health workers at home together with adult female members had a significant effect on BSE and mammography use [OR = 0.15; 95% CI = 0.04–0.50; (OR = 0.15; 95% CI = 0.04, 0.54, P < 0.05)].37–39
Thus, the overall aim of the interventions to increase the uptake of screening through a variety of health promotion strategies by integrating and increasing the awareness of health care professionals, community, lay health workers and community stakeholders was almost successful.
Discussion
The review confirmed that the most common health promotion interventions in breast cancer initiatives targeting women boosted the breast cancer screening in one or another way. However, heterogeneity between the trials limited the statistical pooling of data. Evidence regarding the effectiveness of other interventions such as behavioral interventions, counseling and risk factor assessment was limited by the number of included trials and their moderate or high risk of bias.
Tables 2 and 3 show the evaluation criteria reported from the selected studies. These characteristics must be interpreted with caution, as they by no means give the full picture of indicators used in health promotion interventions. Therefore, it is difficult to arrive at a conclusive and generalizable conclusion on the effectiveness of any particular intervention.17,18
To this end, the evidence shows that effectiveness in boosting screening uptake is greatest for the simple to administer interventions, rather than in depth ones.10 These tend to be the ‘individual-based’ category, e.g. methods of invitation women. Indeed, most interventions were of the individual based category.19,20,22,29–32 This might be, partly, because these interventions are easier to carry out and evaluate than those of the other categories.
The different categories of intervention such as individual-based, community-based and mixed or multi-strategy were taken to conceptualize these interventions in understanding the effectiveness of them and how they fit into the present screening system. A review of interventions to increase breast screening focused on women lifespan and ethnicity issues in the United States studies had shown similar implications.40
Individual level framed message and phone calls are contemporary technologies used in facilitating several interventions and noted in boosting of screening uptake in this review in USA and Indian studies.19,20,22,29–32,37 This is also supported by Lu et al. systematic review of interventions to increase breast and cervical cancer screening uptake among Asian women.10 Behavioral model based behavioral interventions like stage model and health belief model mainly developed to intrapersonal communication in their intention but further explicit implication seen in individual level intervention boosted screening in this review.28–32 and in various findings.41–44
The intervention including couples with diet emphasizing the importance of the husband’s support by encouraging breast cancer screening uptake was more effective than the interventions focusing on healthy diet through mass media at home did not show an effect in screening (Korean women).33 The evidence from the other studies did not support the effectiveness of complex community level interventions.10,41–46 Lecture, pamphlets, flip charts and demonstration of the method of BSE using audio-visuals were increased BSE.35 This evidence was supported by a number of western groups and individual model-based intervention studies though their focus was not only on primary prevention.10,44,47,48
A community level educational intervention emphasizing religious, cultural promoters and lay workers boosted overall awareness regarding breast cancer screening as well as the performance of self-examination (in Indian women, USA migrants).24 For breast cancer screening, evidence was found to support the effectiveness of the following intervention strategies: community-based group education plus culturally sensitive educational materials plus physician consultations.10,40,44,49 In contrast, an intervention based on the targeted component consisted of a folder containing a set of four educational booklets, a letter for the woman to use to discuss mammography with her health-care provider, and a pamphlet about mammography screening services had no significant difference between intervention group and control group.50 However, compared with the literature of screening intervention on general Caucasian population, the patterns of intervention design and results of effectiveness with those observed from the literature targeting general Caucasian population tend to be more heterogeneous. This is in line with the complexity and challenges in interventions targeting ethnic groups.45,49 For sure, many western group and community-based interventions did not show a clear recommendation for further use.10,44,51,52 Surprisingly, almost all studies included were from western countries, but no studies appeared in search engine from African countries. The African studies might focus more on problem definition than recognizing the value of interventions. If so, health promotion researchers should appreciate the value of the interventions rather than giving problem definition and simply assessing the already answered questions.
This review has several limitations. Primarily, it includes only English language published articles and it did not give any room for studies published in other languages and also did not include gray literature that may have overlooked this valuable information. Secondly, the majority of the researches were conducted in the United States on migrant women. This might lead us to refrain from generalizing the specific countries set-up and might be different in permanent residents of the countries linked to cultural differences, access to services and health care system especially issues related to access to breast cancer screening and even affordability of the cost.
In conclusion, although there were noted differences across studies, most studies in this review noted favorable outcomes after health promotion interventions including improvements in participants' view of breast screening, BSE skill, and satisfaction with breast cancer screening educational interventions. Benefits were seen in different resident populations and using both general and specific scenarios. Our results confirmed that the most common health promotion intervention in breast cancer initiatives targeting women boosted the breast cancer screening in one or another way. It is likely that other methods are advantageous, but the evidence is not as strong. Research on breast screening uptake has clearly moved on from the problem definition stage to the next phase of assessing the value of interventions. However, the limited quality of the included studies showed that further research is required to develop simple and effective intervention to improve the trials in the next future.
Conflicts of interest: None declared.
Key points
To provide evidence on the effectiveness of the health promotion interventions.
To find research gap and to improve knowledge in the field of health education.
To develop effective interventions targeting women.
To develop guidelines important for breast screening uptake.
To see professional contribution in the field of health promotion.
Supplementary Material
Acknowledgements
We would like to acknowledge all staff members of department of health education and health promotion, school of public health, International Campus of Tehran University of Medical Sciences for their unreserved administrative support during this manuscript writing. Special thanks go to the Tehran University of Medical Sciences digital library for available search there in the library.
References
- 1. Fitzmaurice C, Dicker D, Pain A, et al. The global burden of cancer 2013. JAMA Oncol 2015; 1: 505–27.http://dx.doi.org/10.1001/jamaoncol.2015.0735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coleman MP, Forman D, Bryant H, et al. Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. The Lancet 2011; 377: 127–38.http://dx.doi.org/10.1016/S0140-6736(10)62231-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alteri R, Bandi P, Brinton L, et al. Breast Cancer Facts & Figures 2011–2012. American Cancer Society, Atlanta, Georgia: 2011. [Google Scholar]
- 4. Boyle P, Levin B World Cancer Report 2008. IARC Press, International Agency for Research on Cancer, Lyon, 2008.
- 5. Danaei G, Vander Hoorn S, Lopez AD, et al. Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. The Lancet 2005; 366: 1784–93.http://dx.doi.org/10.1016/S0140-6736(05)67725-2 [DOI] [PubMed] [Google Scholar]
- 6. Lacey JV, Kreimer AR, Buys SS, et al. Breast cancer epidemiology according to recognized breast cancer risk factors in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial Cohort. BMC Cancer 2009; 9: 84.http://dx.doi.org/10.1186/1471-2407-9-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kratzke C, Vilchis H, Amatya A. Breast cancer prevention knowledge, attitudes, and behaviors among college women and mother–daughter communication. J Commun Health 2013; 38: 560–8.http://dx.doi.org/10.1007/s10900-013-9651-7 [DOI] [PubMed] [Google Scholar]
- 8. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA: a cancer journal for clinicians 2015; 65: 5–29. [DOI] [PubMed] [Google Scholar]
- 9. Peto J. Cancer epidemiology in the last century and the next decade. Nature 2001; 411: 390–5.http://dx.doi.org/10.1038/35077256 [DOI] [PubMed] [Google Scholar]
- 10. Lu M, Moritz S, Lorenzetti D, et al. A systematic review of interventions to increase breast and cervical cancer screening uptake among Asian women. BMC public health 2012; 12: 413.http://dx.doi.org/10.1186/1471-2458-12-413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Corkum M, Hayden JA, Kephart G, et al. Screening for new primary cancers in cancer survivors compared to non-cancer controls: a systematic review and meta-analysis. J Cancer Survivorship 2013; 7: 455–63.http://dx.doi.org/10.1007/s11764-013-0278-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sankaranarayanan R, Ramadas K, Thara S, et al. Clinical breast examination: preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst 2011; 103: 1476–80.http://dx.doi.org/10.1093/jnci/djr304 [DOI] [PubMed] [Google Scholar]
- 13. Yip C-H, Cazap E, Anderson BO, et al. Breast cancer management in middle-resource countries (MRCs): consensus statement from the Breast Health Global Initiative. The Breast 2011; 20:S12–9. [DOI] [PubMed] [Google Scholar]
- 14. Masi CM, Blackman DJ, Peek ME. Interventions to enhance breast cancer screening, diagnosis, and treatment among racial and ethnic minority women. Med Care Res Rev 2007;64:195S–242S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mowatt G, Grimshaw JM, Davis DA, et al. Getting evidence into practice: the work of the Cochrane Effective Practice and Organization of Care Group (EPOC). J Contin Educ Health Prof 2001; 21: 55–60.http://dx.doi.org/10.1002/chp.1340210109 [DOI] [PubMed] [Google Scholar]
- 17. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clin Trials 1996; 17: 1–12. [DOI] [PubMed] [Google Scholar]
- 18. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Commun Health 1998; 52: 377–84.http://dx.doi.org/10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Abood DA, Black DR, Coster DC. Loss-framed minimal intervention increases mammography use. Women's Health Issues 2005; 15: 258–64.http://dx.doi.org/10.1016/j.whi.2005.07.005 [DOI] [PubMed] [Google Scholar]
- 20. Lindberg NM, Stevens VJ, Smith KS, et al. A brief intervention designed to increase breast cancer self-screening. Am J Health Promotion 2009; 23: 320–3.http://dx.doi.org/10.4278/ajhp.071009106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Consedine NS, Horton D, Magai C, et al. Breast screening in response to gain, loss, and empowerment framed messages among diverse, low-income women. J Health Care Poor Underserved 2007; 18: 550–66.http://dx.doi.org/10.1353/hpu.2007.0057 [DOI] [PubMed] [Google Scholar]
- 22. Engelman KK, Cupertino AP, Daley CM, et al. Engaging diverse underserved communities to bridge the mammography divide. BMC Public Health 2011; 11: 47.http://dx.doi.org/10.1186/1471-2458-11-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bowen DJ, Robbins R, Bush N, et al. Effects of a Web-based intervention on women’s breast health behaviors. Transl Behav Med 2011; 1: 155–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rao R, Nair S, Nair NS,. et al. Acceptability and effectiveness of a breast health awareness programme for rural women in India. Indian J Med Sci 2005; 59: 398.http://dx.doi.org/10.4103/0019-5359.16817 [PubMed] [Google Scholar]
- 25. Nguyen TT, Le G, Nguyen T, et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prevent Med 2009; 37: 306–13.http://dx.doi.org/10.1016/j.amepre.2009.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Akhtar S, Nadrah H, Al-Habdan M, et al. First organized screening mammography programme in Saudi Arabia: preliminary analysis of pilot round/Premier programme de mammographie de depistage en Arabie saoudite: rapport preliminaire de l'operation pilote. East Mediterr Health J 2010; 16: 1025. [PubMed] [Google Scholar]
- 27. Ayash C, Axelrod D, Nejmeh-Khoury S, et al. A community intervention: AMBER: Arab American breast cancer education and referral program. J Immigr Minority Health 2011; 13: 1041.http://dx.doi.org/10.1007/s10903-011-9481-6 [DOI] [PubMed] [Google Scholar]
- 28. Eskandari-Torbaghan A, Kalan-Farmanfarma K, Ansari-Moghaddam A, et al. Improving breast cancer preventive behavior among female medical staff: the use of educational intervention based on health belief model. Malay J Med Sci: MJMS 2014; 21: 44. [PMC free article] [PubMed] [Google Scholar]
- 29. Tuzcu A, Bahar Z, Gözüm S. Effects of interventions based on health behavior models on breast cancer screening behaviors of migrant women in Turkey. Cancer nursing 2016; 39: E40–50. [DOI] [PubMed] [Google Scholar]
- 30. Kim JH, Menon U. Pre-and postintervention differences in acculturation, knowledge, beliefs, and stages of readiness for mammograms among Korean American women. Oncol Nurs Forum 2009, 36:E80–92. [DOI] [PubMed] [Google Scholar]
- 31. Hajian S, Vakilian K, Najabadi KM, et al. Effects of education based on the health belief model on screening behavior in high risk women for breast cancer, Tehran, Iran. Asian Pac J Cancer Prev 2011; 12: 49–54. [PubMed] [Google Scholar]
- 32. Taymoori P, Molina Y, Roshani D. Effects of a randomized controlled trial to increase repeat mammography screening in Iranian women. Cancer Nurs 2015; 38: 288.http://dx.doi.org/10.1097/NCC.0000000000000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rahman SM, Harris CM, Mitchell M, KF Soliman KE. Perceptions related to breast cancer prevention and behavioral practices in underserved women participated in a CBPR intervention. Cancer Research 2014; 74(19 Suppl): 5056–5056. [Google Scholar]
- 34. Fry RB, Prentice-Dunn S. Effects of a psychosocial intervention on breast self-examination attitudes and behaviors. Health Educ Res 2005; 21: 287–95.http://dx.doi.org/10.1093/her/cyh066 [DOI] [PubMed] [Google Scholar]
- 35. Gupta SK, Pal D, Garg R, et al. Impact of a health education intervention program regarding breast self examination by women in a semi-urban area of Madhya Pradesh, India. Asian Pac J Cancer Prev 2009; 10: 1113–7. [PubMed] [Google Scholar]
- 36. Cohen M, Azaiza F. Increasing breast examinations among Arab women using a tailored culture-based intervention. Behav Med 2010; 36: 92–9.http://dx.doi.org/10.1080/08964280903521313 [DOI] [PubMed] [Google Scholar]
- 37. Arshad S, Williams KP, Mabiso A, et al. Evaluating the knowledge of breast cancer screening and prevention among Arab-American women in Michigan. J Cancer Educ 2011; 26: 135–8.http://dx.doi.org/10.1007/s13187-010-0130-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dallo FJ, Zakar T, Borrell LN, et al. Cancer knowledge increases after a brief intervention among Arab Americans in Michigan. J Cancer Educ 2011; 26: 139–46.http://dx.doi.org/10.1007/s13187-010-0179-6 [DOI] [PubMed] [Google Scholar]
- 39. Khalili S, Shojaiezadeh D, Azam K, et al. The effectiveness of education on the health beliefs and practices related to breast cancer screening among women referred to Shahid Behtash Clinic, Lavizan area, Tehran, using health belief model. J Health 2014; 5: 45–58. [Google Scholar]
- 40. Rimer BK. Interventions to increase breast screening: lifespan and ethnicity issues. Cancer 1994; 74: 323–8.http://dx.doi.org/10.1002/cncr.2820741317 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.