Abstract
Statement of problem.
Structural damage may remain even after a tooth is restored. Conventional diagnostic aids do not quantify the severity of structural damage or allow the monitoring of structural changes after restoration.
Purpose.
The purpose of this retrospective clinical study was to provide an in-depth analysis of 9 high-risk sites after restoration. The analysis followed structural defects found upon disassembly, restorative materials used, therapeutic procedures provided, current longevity, and long-term quantitative percussion diagnostics (QPD) to monitor results. The hypothesis was that QPD can be used to quantify positive and negative changes in structural stability.
Material and methods.
Sixty sites requiring restoration were part of an institutional review board-approved clinical study. Each participant was examined comprehensively, including QPD testing, at each follow-up. Long-term changes in normal fit error (NFE) values after restoration were evaluated according to a pathology rating system established in an earlier publication. Nine highly compromised sites were chosen for further analysis and monitored for an additional 6 years.
Results.
Of the 9 high-risk sites (NFE>0.04), 7 sites improved and 2 sites deteriorated. Potential causes for each trend were documented.
Conclusions.
The data support the hypothesis that QPD can be used to monitor changes in structural stability after restoration. Knowledge of changes in advance of any symptoms allows further preventive or therapeutic intervention before serious structural damage can occur. Follow-up QPD indications of site improvement can also assure the clinician of the desired structural outcome.
The optimal structural strength of teeth is a critical factor in long-term oral health and functional longevity. Unfortunately, the structural breakdown of teeth can progress with no diagnostic warning signs.1,2 Quantifying structural stability can be difficult clinically, until breakdown becomes advanced or terminal.
Current visual dental diagnostics give a static, unloaded image of a defect in visually accessible areas. The results are qualitative, subject to different interpretations,3–5 and can be unreliable because of artifacts from radio-opaque restorative materials.6 The most definitive method for diagnosing a root fracture is a flap reflection toreveal a bony defect, but this procedure is invasive and limited to advanced lesions.7
Quantitative percussion diagnostics (QPD) is a mechanics-based clinical methodology used to analyze the structural integrity of teeth and dental implants by measuring micromobility in the structure.8–11 QPD can be performed rapidly, noninvasively, and without pain under conditions consistent with mastication and parafunction to detect cracks and defects of all sizes.11 Resulting QPD data can also be used to accurately assess the severity of tooth damage, whether before or after the restoration or for long-term monitoring.1,2
A previous in vitro study showed QPD to be a highly predictable diagnostic aid for identifying structural defects in teeth, even those hidden under restorations or within the body of the tooth structure.11 The predictive quality of QPD was demonstrated by comparing the degree of instability indicated by micromovement arising from defects such as cracks, caries, loss of cement seal, or bone loss at the site. The normal fit error (NFE) values were compared with the results of a tooth disassembly procedure under the microscope, aided by dye penetrant and the transillumination recorded in video and written documentation. The method of distinguishing NFE from QPD data has been described elsewhere.1 This comparison indicated that QPD provided 100% sensitivity and 96% specificity for the detection of cracks.11
A recent in vivo study demonstrated the effectiveness of QPD in identifying high-risk sites with structural pathologic micromovement.1 In this clinical trial, NFE thresholds were established for sites that possessed no, mild, moderate, or severe structural pathology. Each site was disassembled under a microscope (Global Surgical) at magnifications of ×8 to ×14 by using dye penetrant (Toluidine Blue O Indicator; Taylor Technologies) and a transillumination wand (TI2200; Kerr Corp) as described previously.1 Results obtained before the restoration exhibited a strong correlation between NFE values and 4 levels of pathology (none, mild, moderate, and severe).1 The cutoff NFE values of these levels were determined by using 2 statistical criteria which were in good agreement (Fig. 1). The correlation between the NFE value and the 4 levels of pathology exhibited at least 92% overall specificity (95% confidence interval [CI], 0.911–0.997) and 100% sensitivity (95% CI, 0.940–1.000). For each standard deviation (SD; ±0.0089) increase in the NFE, the tooth site was 12 times more likely to have a higher pathology rating (odds ratio=11.92; 95% CI, 7.58–18.74; P<.001), showing that the NFE values strongly discriminated among sites based on clinical pathology.1
Figure 1.
Two methods used to determine the cutoff NFE values of four levels of structural pathology: where probability of higher rating exceeds probability of lower rating and based on minimized probability of misdiagnosis across classification tree. NFE, normal fit error.
A recently published follow-up study of this same group of participants examined the ability of the NFE to provide the clinician with information on the structural health of a tooth after restorative treatment.2 Based on the study data, the following conclusions were drawn: QPD is able to provide the clinician with a revised level of structural stability after restorative treatment that could identify high-risk sites requiring further monitoring; and QPD metrics after restoration provide a new risk assessment tool, a patient educational tool, and a motivator for preventive compliance.2 Further research was indicated to test the limits of information provided by this new diagnostic paradigm in follow-up assessments after restorative treatment.
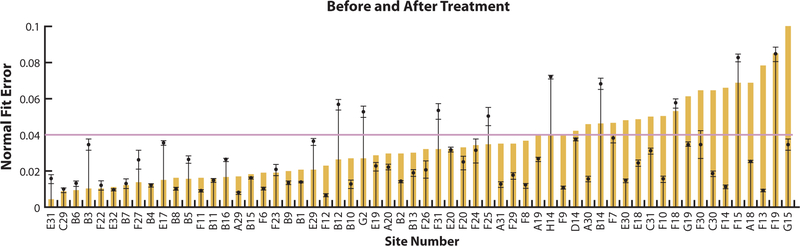
Figure 2 shows the treatment results before NFE as colored bars and the NFE treatment after means as black circles, with an error bar indicating the ±SD values for each of the 60 sites tested. QPD testing after treatment indicated an overall lowering of the average NFE from 0.035 to 0.027. Fifty-one of the 60 sites after restoration (85%) scored below the NFE of 0.04 (greatly stabilized tooth site). Before restoration, 18 sites were classified as severe. After restoration, only 9 sites remained in the NFE severe range of0.04 to 0.099. Although clinically successful, 2 sites had an NFE of [notdef]0.08, indicating very severe structural instability.
Figure 2.
Before treatment NFE results represented by colored bars and after treatment NFE means represented by black circles; error bar indicates standard deviation for 60 sites. The nine sites above red line were participants of present study. NFE, normal fit error.
The purpose of the present study was to analyze in-depth the compromised 9 high-risk sites after restoration to provide additional information on residual structural defects and QPD monitoring results. The hypothesis was that QPD can reveal positive and negative changes in structural stability through monitoring after restoration.
MATERIAL AND METHODS
A sample group of 60 sites was given a QPD complete-mouth evaluation before and immediately after restoration, and the quantitative results have recently been reported.1,2 The selection criteria for the participants, inclusion/exclusion criteria, diagnosis for restorative care, determination of sample size, informed consent, and institutional review board-approved protocol observation and definition of “tooth disassembly” are also detailed elsewhere.1,2 For each site, written and video treatment documentation were reviewed for site-specific structural defects, restorative techniques used to treat the defects, and NFE results found during long-term monitoring. Nine sites remained in the severe classification after restoration and were isolated for further study in a monitoring program that extended over 6 years.
RESULTS
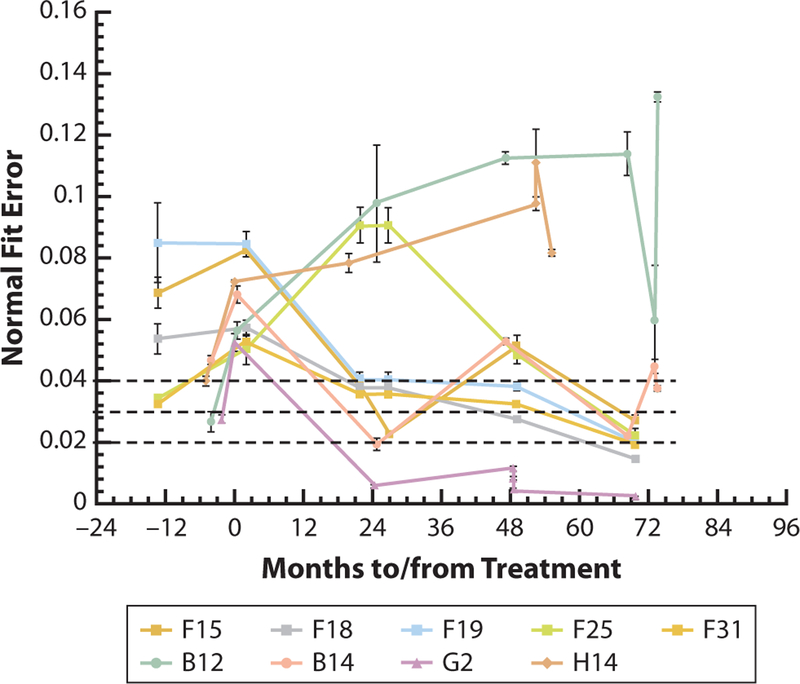
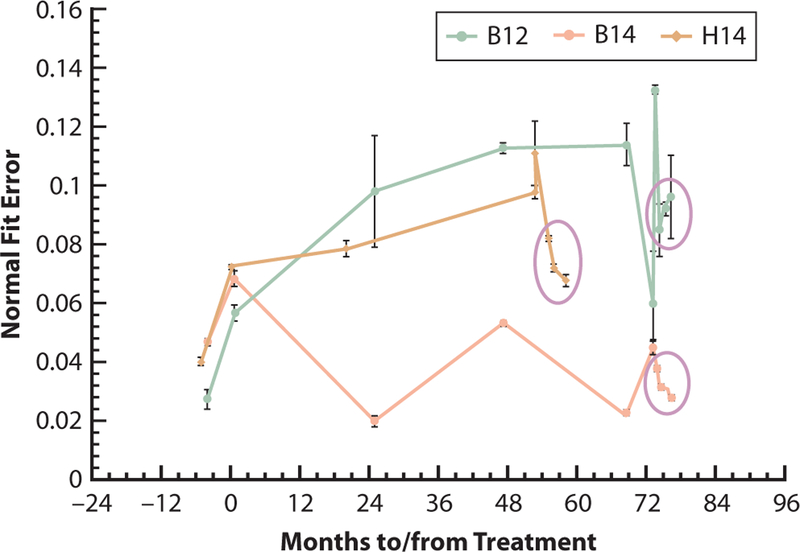
Figure 3 documents the NFE monitoring after restoration of the 9 sites after 7 years from the first examinations in the clinical study. The time of 0 months on this plot corresponds to when the restoration was placed for each site, so that negative values refer to months before restoration and positive values refer to months after restoration. All tooth sites remained clinically asymptomatic and fully functional, with no additional treatment required over the monitoring period. All patients verbally reported 100% compliance with nighttime protective occlusal splint (POS) protocols. During the monitoring, the NFE for 6 sites improved to below the moderate pathology cutoff of 0.03 (Fig. 3).1 The 3 initially highest sites, F15, F18, and F19, all changed over the 6 years after restoration from severe to mild/none (NFE<0.03) (Fig. 2). Site F25 increased significantly in NFE rating at 24 month after restoration, finally stabilizing in the mild range (NFE, 0.02 to <0.03). Site B14 followed an erratic pattern of NFE changes and recently moved into the severe classification for a third time. Two sites, B12 and H14, registered increasing NFE values during the 6 years of monitoring.
Figure 3.
NFE values acquired over 7 years for present in vivo study. Dashed lines indicate cutoff points of 4 pathological classifications identified in earlier work (see Fig. 1).1 Ultimately, 6 of 9 high-risk sites improved to NFE value below 0.03 (mild/none). Two sites, B12 and H14, continued to exhibit NFE>0.04, indicating continuing nonlinear deterioration. Site B14 exhibited positive/negative volatility. NFE, normal fit error; QPD, quantitative percussion diagnostics.
Participant F presented with caries before the restoration with severe restorative breakdown and a 3.5-year history of preprosthetic orthodontic treatment. After restoration, participant F had 5 remaining severe sites with an NFE of 0.04 or greater (severe classification). Site F15 (maxillary left second molar) had a failing class II alloy restoration with extensive caries into the pulp chamber. Additional tooth structure was lost during restoration because of caries and endodontic treatment. The site was restored with a bonded composite resin foundation restoration and a metal-ceramic crown. The NFE increased from an NFE of 0.069 before restoration to an NFE of 0.083 after restoration. Six years later, the NFE had decreased to 0.028.
Site F19 (mandibular left first molar) had a failing metal-ceramic crown with preexisting endodontic treatment and an extensive composite resin foundation restoration. After the foundation restoration and metal-ceramic crown had been replaced, the NFE remained the same after restoration (before, NFE=0.085; after, NFE=0.085), and 6 years later, the NFE had decreased to 0.020.
Site F18 (mandibular left second molar) had micro-leakage under a failing metal-ceramic crown and recurrent caries beneath an amalgam foundation restoration. All damaged tooth structure was replaced with a large composite resin foundation restoration and a new metal-ceramic crown (before, NFE=0.054; after, NFE=0.057). Six years later, the NFE had improved to 0.015 (classification of none).
Site F31 (mandibular right second molar) exhibited mild periodontal bone loss, microleakage, and caries beneath a large composite resin foundation restoration. Beneath the old foundation restoration, the mesial buccal cusp had an incomplete oblique fracture and mesial and distal lingual cusp complete fractures, and 2 preexisting pins were found. The site was restored with an extensive bonded composite resin foundation restoration retained by the stable preexisting pins and a metal-ceramic crown (before, NFE=0.033; after, NFE=0.053). Ultimately, the NFE value for this site decreased to 0.020.
Site F25, (mandibular right central incisor) was included in a lingual wire splint from canine to canine. The tooth showed moderate incisal wear, moderate horizontal bone loss, and a widened periodontal ligament space because of recent orthodontic movement. The definitive restoration was a nonsplinted porcelain veneer to provide function, hygiene, and esthetics (before, NFE=0.035; after, NFE=0.050. As with the other sites for Participant F, the NFE fell into the mild or none classification range over the monitoring period of 6 years (NFE=0.023).
Participant G was a heavy clencher/bruxer who had been provided with gold restorations 25 years earlier. Three teeth had developed some recurrent caries because of leakage through occlusal perforations. Site G2 (maxillary right second molar) showed severe micro-leakage and isolated areas of caries under a mesioocclusal (MO) gold onlay. This site was restored with a bonded composite resin foundation restoration under a more extensive MO gold onlay. The before, NFE was0.031 and the after NFE was 0.053. Six years later the NFE for this site had fallen to the lowest value recorded in the study (NFE=0.003).
Participant B was an attorney with a highly stressed lifestyle and severe loss of tooth structure due to bulimia and caries and recent preprosthetic orthodontic treatment. Site B12 (maxillary left first premolar) had an extensive disto-occlusal (DO) composite resin restoration, with a shell of remaining enamel. The definitive restoration was a bonded composite resin foundation restoration with a metal-ceramic crown. The before NFE was 0.027, and the after NFE was 0.057. Six years later, the NFE was even higher at 0.133.
Site B14 (maxillary left first molar) had a mesial buccal incomplete oblique cuspal fracture under a leaking composite resin restoration with recurrent caries and a metal-ceramic crown. The incompletely fractured cusp was retained under the newly bonded composite resin foundation restoration and metal-ceramic crown (before, NFE=0.047; after, NFE=0.068). Six years later, the NFE was also still elevated at 0.037 with a history of significant swings between improvement and breakdown. After clinical intervention (occlusal adjustment), the NFE started to drop (final NFE=0.027).
Participant H was also an attorney with a highly stressed lifestyle and minimal dental needs before developing symptoms of a cracked tooth. He reported a history of parafunctional activity and noxious habits (ice and gum chewing). Site H14 (maxillary left first molar) had initial pain on mastication and a fractured occlusal composite resin restoration. The fracture in the restoration was directly over a mesial to distal dentinal fracture on the floor of the preparation. The tooth was provisionally restored with a resin onlay for 3 months, became asymptomatic, and a bonded ceramic onlay was placed. The before NFE was 0.040, the after NFE was0.072, and 6 years later the NFE was 0.082.
DISCUSSION
NFE readings will increase during orthodontic treatment, as in traumatic occlusion, and decrease as bone density and the periodontal ligament return to normal. Participant F had received 3.5 years of orthodontic treatment to eliminate reverse articulation, align midlines, and expand a premolar space to allow implant placement. Participant B also had preprosthetic orthodontic treatment. The ultimate establishment of a mature bone density after orthodontics and a normal periodontal ligament space is partially responsible for the improved NFE scores in many of their tooth sites.
The 2 sites with the highest NFE values after treatment were F15 and F19. For site F15, the NFE increased significantly after restoration (before, NFE=0.069; after, NFE=0.083), which is understandable because of the extensive caries, endodontic access, and loss of tooth structure for the metal-ceramic crown. The pulp chamber and missing tooth structure was replaced with bonded composite resin, increasing the overall damping effect and the NFE (Fig. 3). Site F19 (mandibular left first molar) measured as equally damaged before and after restoration (before, NFE=0.085; after, NFE=0.085) and at the same level after restoration as F15. Site F19 had preexisting endodontic treatment, an extensive older composite resin foundation restoration, and a metal-ceramic crown. Consequently, site F19 was structurally compromised before and after treatment, and minimal measurable change was seen in the structural integrity of the site. The small improvement was potentially due to the increase in stability of the newly bonded foundation restoration and recently cemented crown. The comparison of these 2 sites shows that even precisely executed, necessary therapies involve a structural price for reestablishing the biological and functional health of a tooth site. Both sites improved with time, potentially due to bone stabilization after orthodontic treatment, protective splint use, and the elimination of noxious habits.
For site F18 (before, NFE=0.054; after, NFE=0.057), the change from an alloy to a composite resin foundation restoration material could provide more mobility because of the difference in impact responses of the 2 materials. An increase in mobility, therefore, could have accounted for the slightly higher after NFE. Ultimately, the NFE for F18 fell into the none classification (NFE=0.015). This site had a vital pulp and might have benefitted from secondary dentin formation.10
Site F31 had initial visible structural damage (incomplete and complete cuspal fractures). However, many fractures cannot be identified visually even with ×20 magnification, transillumination, and dye penetrant.7 Site F31 increased in NFE after treatment (before, NFE=0.033; after, NFE=0.053) for no obvious reason. Possible cause include a combination of new crack propagation during tooth preparation and micromovement from the retained pins under the new foundation restoration.
In testing before treatment, site F25 was splinted to the mandibular anteriors with a lingual wire splint. After treatment, site F25 was tested as an independent tooth. Six years later, F25 had increased in bone stability and had a narrower periodontal ligament space as a result of compliance with POS and mandibular retainer use (before, NFE=0.035; after, NFE=0.050. Six years later it is NFE=0.023).
Site G2 had an NFE before-treatment value of 0.028 and an NFE after-treatment value of 0.053. This surprising result is counter to what we would have expected given the minimal pathology. The removal of the very retentive gold onlay may have created or increased a dentinal crack before restoration with a new gold onlay. The site improved significantly during monitoring, perhaps because of secondary dentin formation generated from a vital pulp (NFE=0.003).12
Participant B had 2 sites that showed consistently high NFEs yet reported 100% POS compliance. Upon further discussion, the participant confirmed daytime parafunction, significant work and family stressors, and recurrent upper respiratory infections. Site B12 exhibited a significant increase in the NFE (before, NFE=0.027; after, NFE=0.057). The previous post and composite resin foundation restoration was similar to that of the original restoration, but, the original extensive loss of tooth structure combined with additional tooth structure removal for the metal-ceramic crown, decreased the site’s structural strength. For most of the 73 months after the restoration, this site trended higher at each testing period, with 1 improvement that reversed on the next reading with a very high value of0.133. Clinical intervention was instituted at this point, including occlusal refinement and preventive counseling (Fig. 4). After intervention, the NFE value initially decreased to 0.085 after 1 month but then increased to0.096 over the next 2 months. The participant was placed on a 1-month recall to assess further therapeutic clinical interventions.
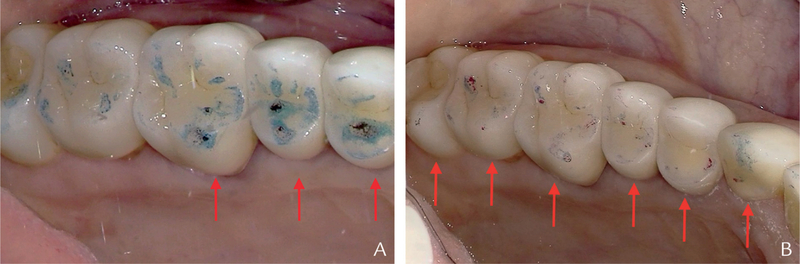
Figure 4.
Intraoral image of occlusal adjustment markings. A, Before adjustment markings (arrows). B, After adjustment markings. POS subsequently adjusted to new occlusal scheme. B12 (first premolar) and B14 (first molar) continued to exhibit relatively high NFE values. B14 opposed well-integrated mandibular left first molar dental implant-supported metal-ceramic crown. Occlusal adjustment distributed occlusal load over 5 teeth rather than 3 teeth as seen in A, and subsequently NFE values improved. NFE, normal fit error; POS, protective occlusal splint.
Site B14 had an incomplete cuspal fracture under the foundation restoration for the crown. The severity of the fracture may have increased, or additional microcracks may have formed during preparation (before, NFE=0.047, after, NFE=0.068, and 73 months NFE=0.045). The site was erratic in the NFE long-term results. Clinical intervention was instituted, including occlusal refinement to protect this site from overload caused by an opposing implant restoration. For this site, the intervention led to an NFE value of 0.027 in 4 months after the occlusal adjustment (Fig. 4).
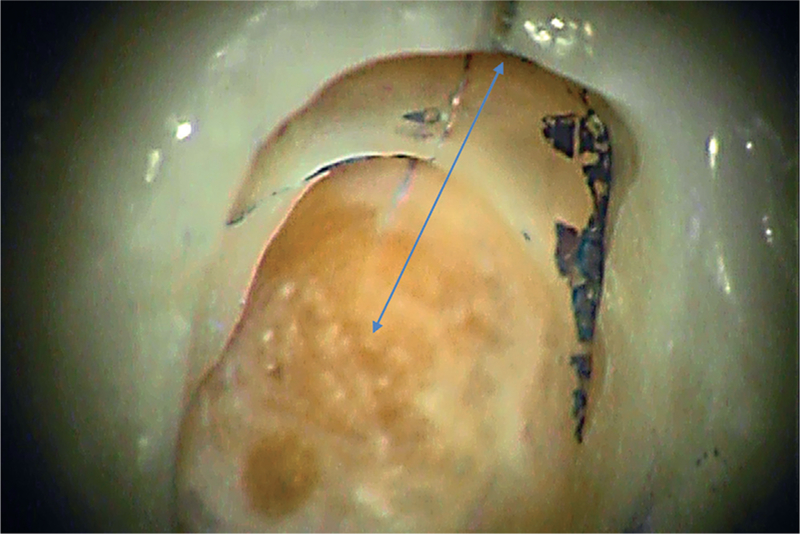
Participant H had an NFE before treatment for site H14 of 0.040, consistent with the dentinal fracture found on the floor of the preparation and symptoms of pain on occluding (Fig. 5). However, the NFE after treatment was 0.072, representing an increase in pathological micromovement, even though the tooth remained asymptomatic. Other microcracks might have developed during the restorative treatment, or the primary crack might have propagated, increasing the NFE to 0.11. At this point, the participant was clinically evaluated and radiographically (2D and 3D) imaged, the occlusion and POS were adjusted, and the participant was given preventive counseling (Figs. 6, 7). The NFE subsequently dropped over the next 2 months (NFE0.081 to NFE 0.072). The participant was then encouraged to wear the POS during workouts. After this change, the subsequent NFE fell to 0.067 (Fig. 8). As with Participant B, participant H has unprotected heavy daytime parafunctional habits due to high professional and personal stressors.
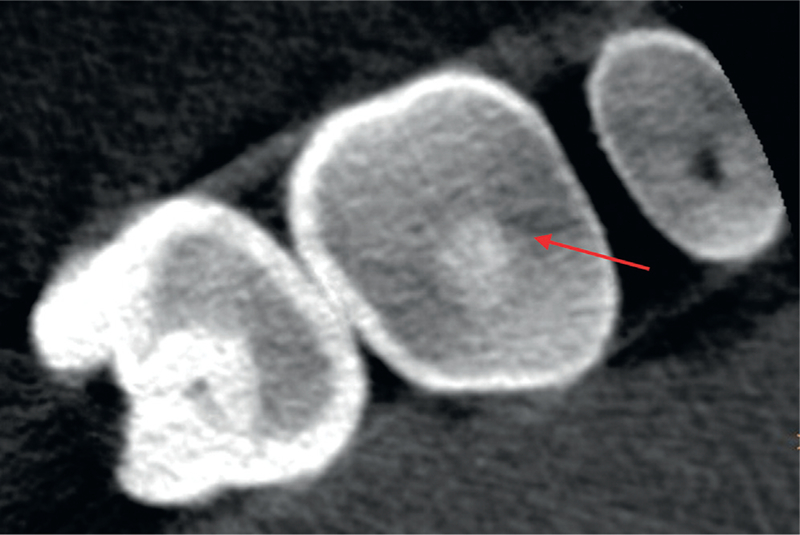
Figure 5.
Site H14 showing crack (arrow) in floor of preparation from mesial marginal ridge to midpoint. Dye penetrant only visible in one third of crack (original magnification ×21) view shows more visible crack length. Smaller cracks may be present but not visible.
Figure 6.
Site H14 cone beam computed tomography image. Possible tooth structure disruption (arrow) at approximate position of documented crack in Figure 5. Crack may also be present on distal or could be radiographic artifact.
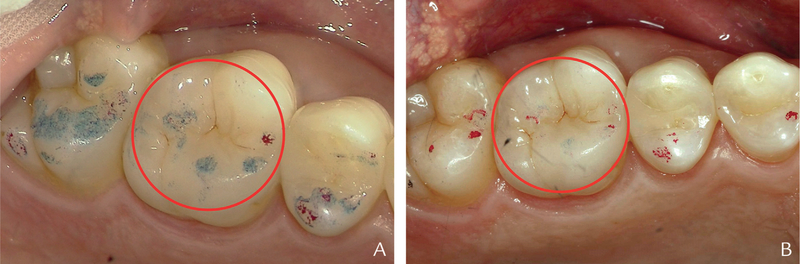
Figure 7.
Site H14 exhibited heavy occlusal contact on mesial marginal ridge directly over original crack as seen in A. Occlusal contacts equilibrated to provide more even contacts on quadrant and lighter occlusal load on maxillary first molar as seen in B. Subsequent improvement indicated by gradual reduction in NFE (Fig. 8, circled data). NFE, normal fit error.
Figure 8.
Chart showing sites B12, B14, and H14 monitoring results. Circles show 3 NFE tests after occlusal adjustments and preventive counseling for each site. Site B12 dropped significantly at first but then slowly increased as patient’s health problems lingered. Site B14 and H14 continued to exhibit lower NFE levels with greater protection. NFE, normal fit error; QPD, quantitative percussion diagnostics.
The high level of structural damage before the restorations in the reviewed sites, combined with needed treatment, did not initially show a postoperative reduction in NFE to a level below 0.04. However, the judicious use of preventive aides such as protective occlusal splints, stress reduction therapies, cessation of harmful parafunctional habits, and other techniques may extend the lifetime of high-risk tooth sites and lower the NFE.
CONCLUSIONS
Based on the findings of this clinical retrospective study, the following conclusions were drawn:
Data support the hypothesis that QPD can reveal positive and negative changes in structural stability during periodic monitoring.
Advanced knowledge of increasing tooth instability before a clinical crisis occurs can lead to preventive or therapeutic intervention.
Even precise evidence-based treatment with positive biological changes can result in a weakened structural system that would benefit from mechanical monitoring.
QPD also provides data for assessing the structural impact of current dental therapies and allows monitoring of tooth stability before and after orthodontic therapy.
Clinical Implications.
Quantitative percussion diagnostics (QPD) can be used as a structural integrity monitoring and patient motivational device to help choose and implement preventive protocols that can increase the longevity of teeth and restorations. Early QPD indications of increasing structural damage provide clinical intervention opportunities prior to catastrophic failure.
Acknowledgments
The authors thank Kassi Bretag, Leila Behnood, and Bryan Gutierrez for their assistance with the data collection, administrative services, and manuscript preparation.
REFERENCES
- 1.Sheets CG, Wu JC, Rashad S, Phelan M, Earthman JC. In vivo study of the effectiveness of quantitative percussion diagnostics as an indicator of the level of the structural pathology of teeth. J Prosthet Dent 2016;116:191–9. [DOI] [PubMed] [Google Scholar]
- 2.Sheets CG, Wu JC, Rashad S, Phelan M, Earthman JC. In vivo study of the effectiveness of quantitative percussion diagnostics as an indicator of the level of structural pathology of teeth after restoration. J Prosthet Dent 2017;117: 218–25. [DOI] [PubMed] [Google Scholar]
- 3.Walton RE. Vertical root fracture. J Amer Dent Assoc 2017;48:100–5. [DOI] [PubMed] [Google Scholar]
- 4.Lubisich EB, Hilton TJ, Ferracane J. Cracked teeth: a review of the literature. J Esthet Restor Dent 2010;22:158–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hilton TJ, Funkhouser E, Ferracane JL, Gilbert GH, Baltuck C, Benjamin P, et al. ; for the National Dental Practice-Based Research Network Collaborative Group. Correlation between symptoms and external characteristics of cracked teeth. Findings from The National Dental Practice-Based Research Network. J Am Dent Assoc 2017;148:246–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chavda R, Mannocci F, Andiappan M, Patel S. Comparing the in vivo diagnostic accuracy of digital periapical radiography with cone-beam computed tomography for the detection of vertical root fracture. J Endod 2014;40:524–9. [DOI] [PubMed] [Google Scholar]
- 7.PradeepKumar AR, Shemesh H, Jothilatha S, Vijayabharathi R, Jayalakshmi S, Kishen A. Diagnosis of vertical root fractures in restored endodontically treated teeth: a time-dependent retrospective cohort study. J Endod 2016;42:1175–80. [DOI] [PubMed] [Google Scholar]
- 8.VanSchoiack LR, Wu JC, Sheets CG, Earthman JC. Effect of bone density on the damping behavior of dental implants: an in vitro method. Mater Sci Eng 2006;26:1307–11. [Google Scholar]
- 9.Dinh A, Sheets CG, Earthman JC. Analysis of percussion response of dental implants in an in vitro study. Mater Sci Eng 2013;33:2657–63. [DOI] [PubMed] [Google Scholar]
- 10.Sheets CG, Hui DD, Bajaj V, Earthman JC. Quantitative percussion diagnostics and bone density analysis of implant bone interfaces in a pre- and post-mortem human subject. Int J Oral Maxillofac Implants 2013;28:1581–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheets CG, Stewart DL, Wu JC, Earthman JC. An in vitro comparison of quantitative percussion diagnostics to standard technique for determining the presence of cracks in natural teeth. J Prosthet Dent 2014;112:267–75. [DOI] [PubMed] [Google Scholar]
- 12.Gronthos S, Mankani M, Brahim J, Gehron Robey P, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A 2000;97:13625–30. [DOI] [PMC free article] [PubMed] [Google Scholar]