Abstract
This randomized controlled trial tested the efficacy of a web-based intervention to increase sexual communication between parents and adolescents. Parent/adolescent dyads (n=660) were recruited from communities in the San Juan area and randomly assigned to the Cuídalos sexual communication or physical activity program. Parent assessments were obtained pre-intervention, and at 3-, 6-, and 12-month follow-up. Parents in the experimental group reported significantly more sexual communication (i.e. peer pressure, sexual prevention, protection, risk) over time than parents in the control group. Results support the efficacy of the Cuídalos web-based format and insight into future web-based sexual health interventions for this population.
Keywords: Hispanics, sexual health, parents, adolescents, Puerto Rico
Introduction
Adolescence is a significant life transition period that offers an opportunity to influence health behaviors - especially sexual behaviors. Latino youth are an important population and particularly vulnerable to the consequences of risky sexual behavior. First, Latinos in general are now the largest minority group in the U.S. with 56.6 million individuals and comprising 17.6% of the population, and by 2060, Latinos will number 119 million, more than 34% of the total U.S. population. [1] Of the current US population, more than 12% or almost 42 million are between the ages of 10 and 19 with Latino adolescents numbering 9.5 million or 22.8%. [2] Second, existing data indicate that Latino youth engage in both early and unprotected sex and are at high risk for HIV/AIDS, other sexually transmitted infections (STIs) - including HIV/AIDS and unintended pregnancies. [3]
Similarly, adolescents in Puerto Rico are a significant yet vulnerable population. Puerto Rican adolescents comprise 15.3% of the total 3.5 million population. According to the High School Youth Risk Behavior Survey, 24% of the Puerto Rican participants, grades 9–12, reported having had sexual intercourse and 16% were currently sexually active. Among those who were sexually active, 50% reported not using condoms during their last sexual intercourse, and 37% did not use any method to prevent pregnancies. [3] Regarding HIV prevention, 85% indicated they had never been tested for HIV. This is significant considering that youth between 15–24 years of age represent 16% of the total HIV cases in Puerto Rico. [4] Teen pregnancy is also high with births among girls and young women aged 10–19 years representing 13% of all births on 2015. [5] It is evident that promoting sexual health among Latinos in general and Puerto Rican youth is an important health priority.
Parent-adolescent approaches in reducing adolescent risky sexual behavior
Parents are one of the most important influences for the prevention of risky sexual behaviors among adolescents. [6,7] Studies indicate that improved communication between parents and adolescents reduces adolescent alcohol and substance use and abuse, which are positively associated with sexual risk behaviors. [8] Recent systematic reviews of the published literature have found that parent-based interventions aiming to reduce sexual risk behaviors or promoting communication about sexual health, have shown to be effective in fostering such communication and increasing condom use skills and self-efficacy among youth. [9–17]
The use of Internet-based or mobile technology-based sexual health interventions for targeting parents and adolescents represents an innovative opportunity to reach large numbers of participants, in comparison with face-to-face facilitated program formats. [18,12] Studies have reported that Latino and African American parents and adolescents are motivated to obtain sexual health information through digital means due to its accessibility. [18,6] Although challenges abound when delivering such interventions (e.g. discomfort with technology among parents, accessibility) the potential benefit of delivering content via online means makes it a promising avenue for impacting parent/adolescent dyads.
While Internet-delivered interventions hold promise for making sexual health information accessible, few studies have tested such interventions with Latinos in general, and none with Puerto Ricans in particular. One study in particular, tested a computer-based parent-adolescent sexual communication intervention, Cuídalos (take care of them) with Spanish language dominant parents in the Midwest. Results from this study documented the intervention’s efficacy in increasing parent-adolescent communication related to sex. [6, 19] The lack of internet based intervention is concerning as studies have shown that Latinos have fewer resources available to obtain information about sexuality and contraception in comparison to young people from other populations. [6, 19, 20] To address this gap, we adapted the Cuídalos (Take Care of Them) intervention from a computer-based to a web-based format and tested its efficacy in increasing parent-adolescent communication (general communication; sexual risk, prevention, protection, and peer pressure communication; comfort with communication) and reducing stigma related to HIV/AIDS among Puerto Rican parents via a randomized controlled trial. [6, 19]
Methods
The Institutional Review Boards at the University of Puerto Rico, University of Michigan, and University of Pennsylvania approved the study. Dyads that agreed to participate signed a consent (parents) and assent (youth) form before completing a pre-test questionnaire. Youth assent was obtained separate from parents in order to avoid coercion. Our team provided each parent with a unique identifier code that allowed them to log into the Cuídalos website.
Recruitment
We established collaborations with community serving entities, including afterschool clubs, sports clubs, and community centers throughout the San Juan, Puerto Rico metropolitan area. We also received the approval of the local Department of Education to recruit dyads throughout Puerto Rico’s public schools. A total of 18 community organizations and 38 public schools participated in this study. Once the partnerships with the organizations and schools were established, our team organized meetings with directors, community leaders or social workers to explain the nature of the study. These leaders served as liaisons between the sites and our team. Afterwards, our team visited the sites to explain and invite potential participants to engage in the study.
Recruitment sites met the following criteria: 1) provided services to youth between the ages of 13–17 years and/or their parents; 2) had available computers where participants could go to engage in the study; 3) were able to provide space for our team to deploy laptop computers for participants’ use; and 4) had flexible schedules in order to facilitate participation in the study. For sites where computers were not available, project staff supplied laptop computers, tablets, and Wi-Fi hotspots to facilitate access to the intervention.
Procedure
Once consent and assent were obtained, the project team assisted first-time participants in creating a password to access the Cuidalos website and to ensure they felt comfortable navigating aspects of the program. We also provided participants with written instructions to log into the site, troubleshooting tips, and the phone numbers/e-mails of our project team in case they encountered problems. Participants could access the website from our recruitment sites, their homes, or any other convenient location. Upon first logging into the Cuídalos website, the system randomly assigned participants to either the sexual risk communication intervention (experimental group) or a health promotion intervention addressing physical activity (control group). Both programs had the theme Cuidalos, and consisted of 6 modules to be completed over two separate days. This was purposefully designed, as parents were asked to complete a set of interactive activities with their sons or daughters after completion of the 3rd module. Parents were asked complete the entire program within one week, either by accessing the remaining program remotely, or by returning to the site where they began the study.
Participants in both the experimental and control conditions had unlimited access to the program via website for three months. We monitored access to the program (i.e., when was it accessed, progress throughout the intervention, and time spent completing it). We made phone calls and sent text-messages on a weekly basis to encourage completion of the program. We also visited the sites regularly to meet with participants that had restricted access to the Internet. After completing the intervention, parents completed secure web-based follow-up measures at 3, 6, and 12 months. Adolescents completed follow-up measures at 6 and 12 months. Adolescents were exempted from completing the 3 month follow-up measures in order to provide time for the sexual behaviors of interest to our study to be manifested, as our previous experience with this population has shown that these may take time to occur among those that have not initiated their sexual activity. Parents and adolescents received economic incentives to cover transportation costs and the invested time in the study. Parents received a total of $80 throughout the one-year period of participation ($10 at pre-test; $10 upon completing the intervention; and $20 at the 3, 6 and 12 month follow-ups). Youth received a total of $50 ($10 at pre-test and $20 at the 6 and 12 month follow-ups).
Sample
A total of 660 parent/adolescent dyads (N=1,320) participated in the study and met the following criteria: 1) agreed to engage in the study as a dyad, and 2) adolescent was between 13 and 17 years of age. This age range was chosen as previous studies have identified that Puerto Rican youth initiate sexual relations between 13 and 14 years of age. [21, 22, 23] We did not exclude parents or adolescents based on their literacy or computer literacy.
Interventions
All parents received an intervention. To minimize differential attrition between conditions, both experimental and control conditions contained the theme Cuídalos. The term captures the responsibility and affection that parents have toward their adolescents. Both conditions emphasized the important role that parents play in the lives of their adolescents. Both conditions were web-based and allowed the same flexibility for accessing the programs (i.e. unlimited, for a period of 3 months).
Based on feedback from the computer-based Cuídalos study and feedback from community leaders, we made several modifications. [6] These included: 1) making the program available through the Internet; 2) providing mechanisms to access and review all or certain sections of the program as needed; 3) adding additional exemplars (e.g., dealing with conflict, dealing with same-sex relationships, addressing HIV/AIDS stigma) and skill building practice opportunities; 4) providing the ability for parents to print handouts and supporting materials; and 5) the addition of on-line parent resources.
Experimental condition –
The parental experimental intervention consisted of a 60-minute web-based intervention with 6 modules. The theoretical framework guiding modifications of the web-based program was Ecodevelopmental Theory [24], the Theory of Reasoned Action/Planned Behavior, and Social Cognitive Theory. [25–29] We emphasized the importance of the family and specifically, parents in supporting their adolescents as it relates to sexual decisions. We focused on providing parents with basic knowledge about pregnancy, HIV/AIDS, and STDs as a basis for effectively communicating with their adolescents. We worked to support attitudes and develop skills to facilitate communication in general and specifically sexual communication. Based on our prior work, we focused on prevention beliefs, reaction beliefs, and communication efficacy. [6, 13] Importantly, we included a component on HIV/AIDS stigma as we conceptualized this to potentially impact attitudes and communication about sex. The program included a variety of media (e.g. animation, videos) to enhance interest and interactivity. The interactivity was key to communication efficacy and skill building.
We programmed the intervention so that parents had to view the Cuídalos program sequentially and in its entirety, although modules could be reviewed once completed. In the first module, we provided basic information about pregnancy and HIV/AIDS. Challenges confronted by adolescents, including decisions regarding sexual behavior and same-sex behavior, were presented. Parents were provided with a mnemonic – based on the Spanish word ¡Cuídate! to outline information their adolescents need to know in order to make healthy decisions related to sexual behavior which include abstinence and consistent condom and/or contraceptive use. In the second module, we provided an opportunity for parents to explore their own attitudes and beliefs about sex, including beliefs about same-sex relationships and persons with HIV/AIDS. In the third module, we added a stigma reduction component, defined as social stigmas related to HIV/AIDS, their consequences for communication with youth and subsequent youth behaviors, and provided examples of non-stigmatizing communication strategies for parents. In the fourth module, parents learned to choose strategies to promote effective communication with adolescents through the use of selected dialog and scenarios. Parents then utilized these strategies in interactive, digitized case studies developed for the program. To address gender differences in communication, we developed separate case studies for male and female adolescents. In this modification, we also addressed communication about same-sex behaviors.
On completion of these modules, parents were directed to a “homework” activity to be completed with their adolescents (e.g., links to specific web pages or program handouts, which could be printed). Activities included discussing dreams and goals of parents and adolescents for the adolescents’ future, reviewing and discussing information about consequences of unsafe sex, including HIV/AIDS, and using case scenarios as a means to discuss parental values regarding sexual behaviors. In the fifth module, we built on general communication skills and focused on developing and strengthening specific skills related to communication about sexual issues. Using computer-generated dialogs, parents identified obstacles and barriers to communication, and were guided to identify ways to overcome communication barriers (e.g., discomfort, unfavorable reactions from adolescents) by developing effective strategies. Specifically, we presented myths and facts of why parents do not talk with their children and shared with parents a framework for effective communication and limit setting, which we call “DIRAS” (e.g., Be direct about decisions; provide explanations for decisions, discuss alternative behaviors/activities, and discuss feelings). Parents viewed digital scenarios that applied these techniques and were provided with on-screen printed and verbal feedback regarding their selection. These scenarios also modeled non-stigmatizing examples of communication. Parents were provided with various responses from adolescents that could serve as barriers to communication, and had an opportunity to select strategies to overcome specific communication barriers. In the sixth module, parents received a review of important information from each module as well as links to potential resources that they might use to support themselves and their adolescents.
Health promotion control condition –
Participants in the control condition were provided with a health promotion intervention aimed at helping parents prevent significant health problems affecting Puerto Rican adolescents that are related, not to sexual behavior, but to other behaviors. These health problems include obesity and related complications such as diabetes and cardiovascular disease. Parents were taught that these health problems can be prevented in their adolescents by changing personal behaviors, primarily exercise, and that parents play a vital role in supporting these important health behaviors. The program provided general knowledge about exercise and ways to overcome barriers to exercise. Similar to the experimental condition, we developed a set of “homework” activities related to exercise that we asked parents to complete with their adolescents.
Measures
Outcome measures –
The primary outcome measures for this study were parent-adolescent communication (general, sexual risk, sexual prevention, sexual protection, sexual peer pressure, comfort) and stigma. [30] There were 10 questions related to general communication, 7 related to parent-adolescent communication on sexual topics, 9 related to comfort with communication, and 14 related to stigma. As shown in Table 1, all 7 items related to parent-adolescent communication on sexual topics were used to calculate the sexual risk communication scale, 2 items were used to derive each of the sexual prevention and protection communication scales, and 3 items were used for the sexual peer pressure communication scale. The final score for each outcome variable was deemed calculable when at least 75% of the original number of items were non-missing. For example, the sexual risk communication scale consisted of 7 individual items, and at least 6 non-missing items were required to compute the scale for each participant. All items were measured with 5-point Likert-type scales, with higher scores indicating more communication and more stigma when talking about sexual topics.
Table 1.
Description and Reliability Coefficients
| Instrument | Number of Items | Reliability (Alpha) | |||
|---|---|---|---|---|---|
| Baseline | 3 Months | 6 Months | 12 Months | ||
| Communication Variables | |||||
| General Communication | 10 | 0.758 | 0.735 | 0.779 | 0.744 |
| Sexual Risk Communication | 7 | 0.938 | 0.939 | 0.946 | 0.947 |
| Sexual Prevention Communication | 2 | 0.854 | 0.872 | 0.858 | 0.872 |
| Sexual Protection Communication | 2 | 0.879 | 0.882 | 0.872 | 0.899 |
| Sexual Peer Pressure Communication | 3 | 0.883 | 0.883 | 0.917 | 0.910 |
| Comfort with Communication | 9 | 0.940 | 0.950 | 0.951 | 0.949 |
| Mediator Variables | |||||
| Sexual Communication Attitudes | 8 | 0.735 | 0.679 | 0.705 | 0.714 |
| Subjective Norms | 3 | 0.862 | 0.886 | 0.903 | 0.898 |
| Self-Efficacy | 5 | 0.891 | 0.912 | 0.919 | 0.916 |
| Sexual Communication Intentions | 3 | 0.897 | 0.853 | 0.871 | 0.896 |
Note: All instruments have a 5-point, Likert-type response scale.
Mediator variables –
Consistent with the theoretical framework used in this study, the mediators included parent-adolescent sexual communication attitudes, subjective norms, perceived self-efficacy, and sexual communication intentions. Eight items were related to attitudes towards communicating with adolescents about condoms and contraceptives (e.g., “I have sufficient knowledge to talk with my son/daughter about sex”). There were 3 items related to subjective norms (e.g., “Would the majority of people most important to you approve or disapprove of you talking to your son/daughter about sex?”), 5 items related to self-efficacy (e.g., “How easy or difficult would it be for you to talk with your son/daughter about sex?”), and 3 items related to intentions to communicate with adolescents about sex, contraceptives, and condoms (e.g., “How likely is it that you’ll talk with your son/daughter in the next 3 months about sex?”). As with communication and stigma outcomes, all mediator variables were calculated when at least 75% of the original items were non-missing. All items were measured with 5-point Likert-type scales, with higher scores indicative of better attitudes, more approval, easier time communicating with adolescent about sex, and higher intentions to talk with adolescent about sex, condoms, and contraceptives.
Demographic and computer access variables –
Demographic variables were obtained through a self-report web-based questionnaire at baseline, and included age (in years), sex (male, female), race (White, Black, American Indian, Asian/Pacific Islander, more than one race, other race), ethnicity (Puerto Rican/Other Hispanic, Latino or Spanish origin/Not of Hispanic, Latino or Spanish origin), marital status (single, married, separated, divorced, widowed, live in partner), partner status (yes, no), education level (did not complete high school, completed high school, did not complete college, completed college), employment outside of home (yes, no), number of hours worked per week, average monthly income (<$300, $300–799, $800–1699, ≥$1700, Unknown), whether they received government assistance (Yes, No), monthly government assistance income (US$), number of children in their household, and location where the Cuídalos program was completed (community agency, school, home, other location (library, other, house of family/friend). Participants were also asked to provide information about their comfort using a computer (very comfortable, somewhat comfortable, somewhat uncomfortable, very uncomfortable), and ease/difficulty in computer access (very easy, easy, difficult, very difficult).
Statistical Analysis
Descriptive statistics were used to characterize demographic variables, parent-adolescent communication and stigma outcomes, as well as the mediators. Chi-square or Fisher’s exact tests were used to examine differences in demographic and computer access variables between parents in the experimental and control groups. Two-sample t-tests were used to examine differences between groups for continuous variables. Additionally, univariate logistic regression modeling was used to determine whether intervention group was a significant predictor of dropping out of the study at any time point. Internal consistency and reliability of our measurement scales were assessed using Cronbach’s alpha estimates at each time point (T1=Baseline, T2=3 months, T3=6 months, T4=12 months) for all mediators and outcomes of interest (Table 1). Scales with an alpha of at least 0.70 were considered acceptable.
In all the analyses, generalized estimating equation (GEE) methodology was used to fit regression models to seven continuous parent-adolescent communication and stigma outcome variables. [31, 32] This methodology allows for modeling of the marginal distribution of each outcome variable as a function of the covariates at each follow-up time point, and accounts for the likely correlations of the repeated outcome measures for each participant. Predictor variables included intervention group, assessment time (treated as a continuous variable where baseline, 3 months, 6 months, and 12 months were coded as 0, 3, 6, and 12, respectively), and the interaction of intervention group and time (predictor of interest), controlling for baseline outcome measures and categorized average monthly income. All analyses relied on an intent–to–treat approach.
Mediation analyses were performed using a modified Baron and Kenny method to correctly account for the group by time (group x time) interaction effects. [33] According to this approach, three separate GEE models were generated to demonstrate mediation. In Model 1, the outcomes were regressed on group, time, and the group x time effect. In Model 2, the mediator of interest was regressed on group, time, and the group x time effect. Lastly, in Model 3, the outcomes were regressed on group, time, the group x time effect, the mediator of interest, and the mediator by time (mediator x time) interaction effect. All models were adjusted for baseline outcome and average monthly income.
Full or partial mediation was determined using three conditions. First, the group x time interaction effect was statistically significant in Model 1. Next, both the group x time effect in Model 2 and the main effect of mediator in Model 3 demonstrated statistical significance. Lastly, for full mediation, there was a reduction in magnitude in the group x time estimate in Model 3 (compared to Model 1), and the group x time effect was not statistically significant. For partial mediation, there was a reduction in magnitude in the group x time estimate in Model 3 (compared to Model 1), and the group x time effect was statistically significant. Standardized effect sizes for the reduction of the intervention effect on the outcome variables were calculated and categorized as small (0-.30), medium (.30-.60), and large (>0.60) using Cohen’s guidelines for interpreting the magnitude of standardized mean differences. [34]
Missing values for the outcome variables of interest at baseline, 3, 6, and 12 month follow-ups were multiply imputed using the fully conditional specification (FCS) method with ten imputation sets. [35] Outcomes were imputed sequentially by fitting on average monthly income and the outcomes in preceding months using linear regression. There were negligible differences in the results after imputing, thus results of this study reflect the original, non-imputed data. Statistical significance was taken at the 0.05 level. All analyses were conducted using SAS Version 9.4 (SAS Institute, Cary, NC).
Results
Attrition
As shown in Figure 1, there was little attrition. For parents in the Cuídalos intervention group (n=330), participation rates at 3-month, 6–month, and 12–month follow–up were 78% (n=257), 80% (n=265), and 74% (n=243), respectively. For parents in the health promotion control group (n=330), participation rates at 3-month, 6–month, and 12–month follow–up were 79% (n=259), 79% (n=259), and 77% (n=254), respectively. Logistic regression analyses of parent participants indicated there were no statistically significant differences in attrition between the two intervention groups (data not shown; p=0.3211).
Figure 1.
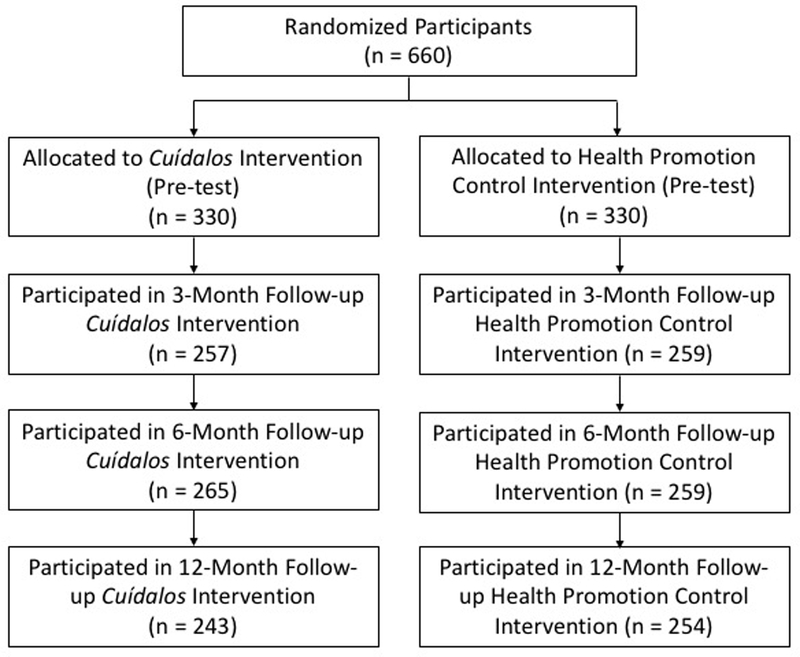
Progress of participants through the trial
Reliability
Cronbach’s alpha estimates for all mediator scales and outcome measures are summarized in Table 1. With the exception of the sexual communication attitudes scale at 3 months (T2 Cronbach’s alpha=0.679), all scales and subscales demonstrated a Cronbach’s alpha value greater than 0.70.
Baseline Characteristics
Baseline characteristics are shown in Table 2. Only parent data (N=660) were included in the analyses. The majority of parents were female (90%, n=591), married (41%, n=269), completed college (44%, n=292), not employed outside of home (61%, n=401), received government assistance (62%, n=412), and had a partner (62%, n=412). There was a near equal percentage of female (52%, n=342) and male (48%, n=316) adolescents participating in this study. Parents ranged in age from 25 to 75 years, with a mean age of 42.5 years (SD = 8.25). In this study, 67% (n=445) of families did not report their average monthly income, 8% (n=51) reported their income less than $300, 7% (n=46) reported between $300 and $799, 10% (n=64) between $800 and $1699, and 8% (n=54) higher than $1700. On average, parents worked 32.5 hours (SD = 13.35) per week, received government assistance income of $553.32 per month (SD = 761.09), and had 1.54 children (SD = 0.74) in their household. Seventy percent (n=459) of parents reported they were very comfortable using computers, and 77% (n=511) did not have difficulty finding a computer. With the exception of average monthly income (p=0.0248), there were no significant differences in demographic characteristics between parents in the Cuídalos intervention and those in the general health promotion control intervention. For communication and stigma variables, only significant differences were found in sexual risk communication between the intervention groups at baseline (p=0.03234). Lastly, no significant differences between the groups were found for any of the mediator variables at baseline (Table 2).
Table 2.
Sample characteristics at baseline (N=660)
| Variable | Total Sample (N=660) | Experiment (N=330) | Control (N=330) | P-value |
|---|---|---|---|---|
| Demographic and Computer Access Variables | ||||
| Parent’s Age [Mean (SD)] | 42.52 (8.25) | 42.41 (8.17) | 42.62 (8.34) | 0.7556 |
| Parent’s Sex [N (%)] | 0.3437 | |||
| Female | 591 (89.55%) | 296 (89.70%) | 295 (89.39%) | |
| Male | 67 (10.15%) | 32 (9.70%) | 35 (10.61%) | |
| Missing | 2 (0.30%) | 2 (0.61%) | 0 (0.00%) | |
| Child’s Sex [N (%)] | 0.3154 | |||
| Female | 342 (51.82%) | 174 (52.73%) | 168 (50.91%) | |
| Male | 316 (47.88%) | 154 (46.67%) | 162 (49.09%) | |
| Missing | 2 (0.30%) | 2 (0.61%) | 0 (0.00%) | |
| Parent’s Race [N (%)] | 0.9083 | |||
| White | 174 (26.36%) | 89 (26.97%) | 85 (25.76%) | |
| Black | 77 (11.67%) | 35 (10.61%) | 42 (12.73%) | |
| American Indian | 16 (2.42%) | 9 (2.73%) | 7 (2.12%) | |
| Asian/Pacific Islander | 5 (0.76%) | 3 (0.91%) | 2 (0.61%) | |
| More than one race | 48 (7.27%) | 24 (7.27%) | 24 (7.27%) | |
| Other race | 29 (4.39%) | 12 (3.64%) | 17 (5.15%) | |
| Missing | 311 (47.12%) | 158 (47.88%) | 153 (46.36%) | |
| Parent’s Ethnicity [N (%)] | 0.6180 | |||
| Puerto Rican | 341 (51.67%) | 171 (51.82%) | 170 (51.52%) | |
| Other Hispanic, Latino or Spanish origin | 22 (3.33%) | 8 (2.42%) | 14 (4.24%) | |
| Not of Hispanic, Latino or Spanish origin | 11 (1.67%) | 6 (1.82%) | 5 (1.52%) | |
| Missing | 286 (43.33%) | 145 (43.94%) | 141 (42.73%) | |
| Marital Status [N (%)] | 0.3439 | |||
| Single | 187 (28.33%) | 98 (29.70%) | 89 (26.97%) | |
| Married | 269 (40.76%) | 127 (38.48%) | 142 (43.03%) | |
| Separated | 22 (3.33%) | 9 (2.73%) | 13 (3.94%) | |
| Divorced | 93 (14.09%) | 51 (15.45%) | 42 (12.73%) | |
| Widowed | 15 (2.27%) | 5 (1.52%) | 10 (3.03%) | |
| Live in Partner | 72 (10.91%) | 38 (11.52%) | 34 (10.30%) | |
| Missing | 2 (0.30%) | 2 (0.61%) | 0 (0.00%) | |
| Partner [N (%)] | 0.1158 | |||
| Yes | 412 (62.42%) | 198 (60.00%) | 214 (64.85%) | |
| No | 245 (37.12%) | 129 (39.09%) | 116 (35.15%) | |
| Missing | 3 (0.45%) | 3 (0.91%) | 0 (0.00%) | |
| Education [N (%)] | 0.8663 | |||
| Did not complete high school | 72 (10.91%) | 32 (9.70%) | 40 (12.12%) | |
| Completed high school | 190 (28.79%) | 95 (28.79%) | 95 (28.79%) | |
| Did not complete college | 102 (15.45%) | 50 (15.15%) | 52 (15.76%) | |
| Completed college | 292 (44.24%) | 151 (45.76%) | 141 (42.73%) | |
| Missing | 4 (0.61%) | 2 (0.61%) | 2 (0.61%) | |
| Employment Outside of Home [N (%)] | 0.3667 | |||
| Yes | 257 (38.94%) | 128 (38.79%) | 129 (39.09%) | |
| No | 401 (60.76%) | 200 (60.61%) | 201 (60.91%) | |
| Missing | 2 (0.30%) | 2 (0.61%) | 0 (0.00%) | |
| Number of Work Hours per Week [Mean (SD)] | 32.50 (13.35) | 33.41 (13.35) | 31.62 (13.35) | 0.3124 |
| Average Monthly Income [N (%)] | 0.0248 | |||
| < $300 | 51 (7.73%) | 22 (6.67%) | 29 (8.79%) | |
| $300-$799 | 46 (6.97%) | 22 (6.67%) | 24 (7.27%) | |
| $800-$1699 | 64 (9.70%) | 24 (7.27%) | 40 (12.12%) | |
| ≥ $1700 | 54 (8.18%) | 36 (10.91%) | 18 (5.45%) | |
| Unknown | 445 (67.42%) | 226 (68.48%) | 219 (66.36%) | |
| Government Assistance [N (%)] | 0.2778 | |||
| Yes | 412 (62.42%) | 210 (63.64%) | 202 (61.21%) | |
| No | 246 (37.27%) | 118 (35.76%) | 128 (38.79%) | |
| Missing | 2 (0.30%) | 2 (0.61%) | 0 (0.00%) | |
| Monthly Government Assistance Income (US$) [Mean (SD)] | 553.32 (761.09) | 568.78 (854.96) | 537.16 (650.46) | 0.6750 |
| Number of Children in House [Mean (SD)] | 1.54 (0.74) | 1.53 (0.76) | 1.56 (0.72) | 0.5915 |
| Program Location [N (%)] | 0.7713 | |||
| Community Agency | 120 (18.18%) | 62 (18.79%) | 58 (17.58%) | |
| School | 337 (51.06%) | 172 (52.12%) | 165 (50.00%) | |
| Home | 104 (15.76%) | 46 (13.94%) | 58 (17.58%) | |
| Other Location | 92 (13.94%) | 46 (13.94%) | 46 (13.94%) | |
| Missing | 7 (1.06%) | 4 (1.21%) | 3 (0.91%) | |
| Computer Comfort [N (%)] | 0.7716 | |||
| Very comfortable | 459 (69.55%) | 226 (68.48%) | 233 (70.61%) | |
| Somewhat comfortable | 151 (22.88%) | 78 (23.64%) | 73 (22.12%) | |
| Somewhat uncomfortable | 35 (5.30%) | 20 (6.06%) | 15 (4.55%) | |
| Very uncomfortable | 11 (1.67%) | 4 (1.21%) | 7 (2.12%) | |
| Missing | 4 (0.61%) | 2 (0.61%) | 2 (0.61%) | |
| Ease/Difficulty Finding a Computer [N (%)] | 0.7616 | |||
| Very easy | 271 (41.06%) | 140 (42.42%) | 131 (39.70%) | |
| Easy | 240 (36.36%) | 115 (34.85%) | 125 (37.88%) | |
| Difficult | 109 (16.52%) | 52 (15.76%) | 57 (17.27%) | |
| Very difficult | 35 (5.30%) | 20 (6.06%) | 15 (4.55%) | |
| Missing | 5 (0.76) | 3 (0.91%) | 2 (0.61%) | |
| Communication Variables | ||||
| General Communication [Mean (SD)] | 3.86 (0.60) | 3.84 (0.62) | 3.88 (0.59) | 0.3391 |
| Sexual Risk Communication [Mean (SD)] | 3.22 (1.14) | 3.12 (1.12) | 3.31 (1.16) | 0.0324 |
| Sexual Prevention Communication [Mean (SD)] | 3.16 (1.33) | 3.07 (1.31) | 3.25 (1.35) | 0.0922 |
| Sexual Protection Communication [Mean (SD)] | 2.83 (1.36) | 2.74 (1.36) | 2.93 (1.36) | 0.0664 |
| Sexual Peer Pressure Communication [Mean (SD)] | 3.62 (1.25) | 3.52 (1.21) | 3.71 (1.29) | 0.0574 |
| Comfort with Communication [Mean (SD)] | 3.50 (0.60) | 3.50 (0.61) | 3.51 (0.60) | 0.7967 |
| Mediator Variables | ||||
| Sexual Communication Attitudes [Mean (SD)] | 2.74 (0.49) | 3.71 (0.51) | 3.77 (0.46) | 0.1455 |
| Subjective Norms [Mean (SD)] | 4.16 (0.77) | 4.12 (0.79) | 4.19 (0.75) | 0.2658 |
| Self-Efficacy [Mean (SD)] | 3.83 (0.91) | 3.77 (0.90) | 3.89 (0.91) | 0.1084 |
| Sexual Communication Intentions [Mean (SD)] | 4.01 (0.95) | 4.02 (0.94) | 4.00 (0.96) | 0.7745 |
Note: P-values based on chi-square or Fisher’s Exact tests for categorical variables, and two-sample t-tests for continuous variables
Effect of the Intervention on Outcomes
Results of the GEE analyses indicated that parents who participated in the Cuídalos intervention group reported more sexual peer pressure communication (Table 3, Model 1: mean difference= 0.0167, standard error=0.01, p=0.0393), more sexual prevention communication (Table 4, Model 1: mean difference=0.0184, standard error=0.01, p=0.0311), more sexual protection communication (Table 5 Model 1: mean difference=0.0234, standard error=0.01, p=0.0076), and more sexual risk communication (Table 6, Model 1: mean difference=0.0179, standard error= 0.01, p=0.0099) per month than parents in the control group. GEE model results demonstrated that changes in general communication, comfort with communication, and stigma over time were not significantly associated with the intervention groups; thus, mediation could only be further assessed for sexual peer pressure, sexual prevention, sexual protection, and sexual risk communication variables.
Table 3.
Mediators of the Effect of the Intervention on Sexual Peer Pressure Communication
| Model 1 |
Model 2 |
Model 3 |
Reduction of Intervention Effect on Communication (%) |
Cohen’sd† for Reduction of Intervention Effect on Communication | ||
|---|---|---|---|---|---|---|
| Mediator | Effect* of Intervention on Communication Without Controlling for Mediator | Effect* of Intervention on Mediator | Effect** of Mediator on Communication | Effect* of Intervention on Communication Controlling for Mediator | ||
| Self-Efficacy | .0167 (.0081) p = .0393 |
.0110 (.0056) p = .0494 |
.1577 (0.0272) p <. 0001 |
.0151 (.0080) p = .0614 |
.0016 (10%) | .20 |
| Sexual Communication Attitudes | .0167 (.0081) p = .0393 |
.0074 (.0033) p = .0266 |
.3556 (.0525) p < .0001 |
.0146 (.0080) p = .0679 |
.0021 (13%) | .26 |
| Subjective Norms | .0167 (.0081) p = .0393 |
.0126 (.0056) p = .0255 |
.1491 (.0313) p < .0001 |
.0153 (.0080) p = .0574 |
.0014 (8%) | .17 |
Note. Table covers all time points; [Estimate (Standard Error)]
Group x Time interaction effect
Main effect of mediator
Small (0-.30), Medium (.30-.60), Large (>.60)
Table 4.
Mediators of the Effect of the Intervention on Sexual Prevention Communication
| Model 1 |
Model 2 |
Model 3 |
Reduction of Intervention Effect on Communication (%) |
Cohen’s d† for Reduction of Intervention Effect on Communication |
||
|---|---|---|---|---|---|---|
| Mediator | Effect* of Intervention on Communication Without Controlling for Mediator | Effect* of Intervention on Mediator | Effect** of Mediator on Communication | Effect* of Intervention on Communication Controlling for Mediator | ||
| Self-Efficacy | .0184 (.0085) p = .0311 |
.0134 (.0056) p = .0166 |
.2602 (.0317) p < .0001 |
.0150 (.0083) p = .0695 |
.0034 (18%) | .40 |
|
Sexual Communication Attitudes |
.0184 (.0085) p = .0311 |
.0072 (.0033) p = .0313 |
.4533 (.0576) p < .0001 |
.0155 (.0083) p = .0620 |
.0029 (16%) | .34 |
| Subjective Norms | .0184 (.0085) p = .0311 |
.0125 (.0056) p = .0267 |
.1813 (.0327) p < .0001 |
.0161 (.0084) p = .0557 |
.0023 (13%) | .27 |
Note. Table covers all time points; [Estimate (Standard Error)]
Group x Time interaction effect
Main effect of mediator
Small (0-.30), Medium (.30-.60), Large (>.60)
Table 5.
Mediators of the Effect of the Intervention on Sexual Protection Communication
| Model 1 |
Model 2 |
Model 3 |
Reduction of Intervention Effect on Communication (%) |
Cohen’s d† for Reduction of Intervention Effect on Communication |
||
|---|---|---|---|---|---|---|
| Mediator | Effect* of Intervention on Communication Without Controlling for Mediator | Effect* of Intervention on Mediator | Effect** of Mediator on Communication | Effect* of Intervention on Communication Controlling for Mediator | ||
| Self-Efficacy | .0234 (.0087) p = .0076 |
.0120 (.0056) p = .0327 |
.3137 (.0308) p < .0001 |
.0203 (.0084) p = .0157 |
.0031 (13%) | .36 |
| Sexual Communication Attitudes | .0234 (.0087) p = .0076 |
.0072 (.0033) p = .0299 |
.5780 (.0595) p < .0001 |
.0202 (.0084) p =.0168 |
.0032 (14%) | .37 |
| Subjective Norms | .0234 (.0087) p = .0076 |
.0131 (.0056) p = .0197 |
.1829 (.0351) p < .0001 |
.0213 (.0085) p = .0132 |
.0021 (9%) | .24 |
Note. Table covers all time points; [Estimate (Standard Error)]
Group x Time interaction effect
Main effect of mediator
Small (0-.30), Medium (.30-.60), Large (>.60)
Table 6.
Mediators of the Effect of the Intervention on Sexual Risk Communication
| Model 1 |
Model 2 |
Model 3 |
Reduction of Intervention Effect on Communication (%) |
Cohen’s d† for Reduction of Intervention Effect on Communication |
||
|---|---|---|---|---|---|---|
| Mediator | Effect* of Intervention on Communication Without Controlling for Mediator | Effect* of Intervention on Mediator | Effect** of Mediator on Communication | Effect* of Intervention on Communication Controlling for Mediator | ||
| Self-Efficacy | .0179 (.0069) p = .0099 |
.0123 (.0056) p = .0273 |
.2194 (.0257) p < .0001 |
.0153 (.0067) p = .0229 |
.0026 (15%) | .38 |
| Sexual Communication Attitudes | .0179 (.0069) p = .0099 |
.0074 (.0033) p = .0260 |
.4327 (.0485) p < .0001 |
.0151 (.0067) p = .0249 |
.0028 (16%) | .41 |
| Subjective Norms | .0179 (.0069) p = .0099 |
.0132 (.0056) p = .0181 |
.1658 (.0281) p < .0001 |
.0158 (.0068) p = .0204 |
.0021 (12%) | .30 |
Note. Table covers all time points; [Estimate (Standard Error)]
Group x Time interaction effect
Main effect of mediator
Small (0-.30), Medium (.30-.60), Large (>.60)
Mediation of Intervention Effects on Communication
Mediation analyses demonstrated that self-efficacy, sexual communication attitudes, and subjective norms fully mediated the effect of the intervention on sexual peer pressure communication and sexual prevention communication (Tables 3–4), and partially mediated the the effect of the intervention on sexual protection communication and sexual risk communication (Tables 5–6). Sexual communication intentions was not a significant mediator for any of the outcomes. As seen in Table 3, the effect of intervention on sexual peer pressure communication controlling for self-efficacy (Model 3) is 0.0151 (standard error=0.01, p=0.0614), 10% lower than the effect without controlling for the mediator (Cohen’s d=.20). The effect of intervention on sexual peer pressure communication controlling for sexual communication attitudes (Table 3, Model 3) is 0.0146 (standard error=0.01, p=0.0679), 13% lower than the effect without controlling for the mediator (Cohen’s d=.26). The effect of intervention on sexual peer pressure communication controlling for subjective norms (Table 3, Model 3) is 0.0153 (standard error=0.01, p=0.0574), 8% lower than the effect without controlling for the mediator (Cohen’s d=.17).
The effect of intervention on sexual prevention communication controlling for self-efficacy (Table 4, Model 3) is 0.0150 (standard error=0.01, p=0.0695), 18% lower than the effect without controlling for the mediator (Cohen’s d=.40). The effect of intervention on sexual prevention communication (Table 4, Model 3) controlling for sexual communication attitudes is 0.0155 (standard error=0.01, p=0.0620), 16% lower than the effect without controlling for the mediator (Cohen’s d=.34). The effect of intervention on sexual prevention communication controlling for subjective norms (Table 4, Model 3) is 0.0161(standard error=0.01, p=0.0557), 13% lower than the effect without controlling for the mediator (Cohen’s d=.27).
As seen in Table 5, the effect of intervention on sexual protection communication controlling for self-efficacy (Model 3) is 0.0203 (standard error=0.01, p=0.0157), 13% lower than the effect without controlling for the mediator (Cohen’s d=.36). The effect of intervention on sexual protection communication controlling for sexual communication attitudes (Table 5, Model 3) is 0.0202 (standard error=0.01, p=0.0168), 14% lower than the effect without controlling for the mediator (Cohen’s d=.37). The effect of intervention on sexual protection communication controlling for subjective norms (Table 5, Model 3) is 0.0213 (standard error=0.01, p=0.0132), 9% lower than the effect without controlling for the mediator (Cohen’s d=.24).
The effect of intervention on sexual risk communication controlling for self-efficacy (Table 6, Model 3) is 0.0153 (standard error=0.01, p=0.0229), 15% lower than the effect without controlling for the mediator (Cohen’s d=.38). The effect of intervention on sexual risk communication controlling for sexual communication attitudes (Table 6, Model 3) is 0.0151 (standard error=0.01, p=0.0249), 16% lower than the effect without controlling for the mediator (Cohen’s d=.41). The effect of intervention on sexual risk communication controlling for subjective norms (Table 6, Model 3) is 0.0158 (standard error=0.01, p=0.0204), 12% lower than the effect without controlling for the mediator (Cohen’s d=.30).
Discussion
The results from our study suggest that the Cuídalos intervention is efficacious tool for increasing sexual related communication between Puerto Rican parents and adolescents. These results add to the growing evidence of the intervention’s efficacy in both its face-to-face and Internet-delivered formats. [6, 19] Parents in the experimental condition reported more sexual communication over time with their adolescents focusing on peer pressure, sexual prevention, sexual protection, and sexual risk than those in the control group.
Just as important, our analysis demonstrated that self-efficacy, sexual communication attitudes, and subjective norms fully mediated the effect of the intervention on sexual peer pressure communication and sexual prevention communication, and partially mediated the effect of the intervention on sexual protection communication and sexual risk communication. The results evidence that when equipped with the right tools and trained appropriately, parents can engage in communication with adolescents on issues that are commonly perceived as difficult for them, such as those related to sexuality. The Cuídalos intervention stands as an important tool that can be used with Spanish-speaking populations to increase parental communicating about sexuality with adolescents.
The testing of this web-based version of the Cuídalos intervention took place in Puerto Rico in the context of concerning health statistics for adolescent sexual health. The Cuídalos intervention can be a promising tool to provide parents with the needed information and skills to engage in communication about sexual health with adolescents in Puerto Rico. The delivery of the intervention via the Internet can allow parents to circumnavigate institutional barriers that have been an obstacle for adolescent education on sexual health on the Island.
Limitations
Although the reported results are promising for fostering parent/adolescent communication on sexual related issues, we are aware that this study is just one part of the many needed efforts to fully impact youth’s sexual health and has its limitations. First, we chose a web-based platform but issues of accessibility and convenience may have affected the results. Certainly, mobile technologies should be considered as another platform for health information. Second, the population and sample in Puerto Rico may limit generalizability to other mainland Puerto Rican and Latino populations as well as to fathers.
Conclusion
The results from our study should be interpreted against the social and cultural backdrop in which Latino youth are embedded. First, there is an urgent need to address the sexual health of Latino youth in general, and Puerto Ricans in particular. As stated in the introduction to this paper Latinos are a growing minority group, and young people engage in early and unprotected sex, which places them at risk for HIV/AIDS, other STIs, and unintended pregnancies. Data shows that Puerto Rican youth in particular are sexually active, avoid condom use, and are rarely tested for HIV. This scenario highlighst the need for intervention targeting Latino youth’s sexual health, and Cuidalos is now part of the existing evidence based tools that families and communities can use for these purposes.
Second, the integration of parents into interventions that aim to foster youth health is vitally important. Latino culture places value on collectivity, and this entails a recognition of the important role of parents in young people’s lives. The Cuidalos intervention recognizes this role and highlights the need to understand youth health as a communal experience, heavily influenced by their immediate family and parents. Furthermore, the deployment of our intervention via local clubs and schools, continues to highlight the importance of communities in reaching adolescents and fostering their sexual health. In summary, the Cuidalos intervention, both due to its implementation approach and its results, is an added resource to the existing scientific literature on the role of family and community in youth health.
Future implementation of Cuidalos, or other interventions aiming to address similar variables of interest, will need to examine how changes in sexual communication between parents and adolescents impact the latter’s sexual behaviors and protective practices. This is an important step for a future research agenda, and one which will help us continue to support youth’s sexual health.
Acknowledgments
Source of Funding: Dr. Nelson Varas-Díaz was supported by the National Institute of Drug Abuse (1K02DA035122) and this study by the National Institutes of Health (R01NRO13505). We are grateful for the support from our communities and the parents and adolescents who participated in the study. For the remaining authors, no funding was declared.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
Contributor Information
Nelson Varas-Díaz, Global and Sociocultural Studies, Florida International University, Miami, FL.
Elba Betancourt-Díaz, Institute for Psychological Research, Universidad del Este, San Juan, PR.
Alicia J. Lozano, University of Pennsylvania School of Nursing, Philadelphia, PA.
Liming Huang, Unviersity of Pennsylvania School of Nursing, Philadelphia, PA.
Lucia DiNapoli, University of Pennsylvania School of Nursing, Philadelphia, PA.
Alexandra Hanlon, University of Pennsylvania School of Nursing, Philadelphia, PA.
Antonia M. Villarruel, University of Pennsylvania School of Nursing, Philadelphia, PA.
References
- 1.Hispanic Heritage Month 2016. US Census Bureau. 2017-June-26 URL:https://www.census.gov/content/dam/Census/newsroom/facts-for-features/2016/cb16-ff16.pdf. Accessed: 2017–06-26. (Archived by WebCite® at http://www.webcitation.org/6rVvb6×9C)http://www.webcitation.org/6rVvb6×9C)
- 2.The Changing faces of America’s adolescents. US Department of Health and Human Services. 2017-June-26 URL:https://www.hhs.gov/ash/oah/facts-and-stats/changing-face-of-americas-adolescents/index.html. Accessed: 2017–06-26. (Archived by WebCite® at http://www.webcitation.org/6rVzxUUoF)http://www.webcitation.org/6rVzxUUoF)
- 3.Centers for Disease Control and Prevention (2015). Youth Risk and Behavior Survey Questionnaire. Available at:www.cdc.gov/yrbs. Accessed on November, 2017. (Archived by WebCite® at http://www.webcitation.org/6wFvSI5jr)
- 4.HIV/AIDS Surveillance Program. Puerto Rico HIV (not AIDS) Surveillance Summary Cumulative HIV Cases. 2017. Puerto Rico Health Department. [Google Scholar]
- 5.Mothers, Children, and Adolescents Division. Por cientos y Tasas de Nacimientos a Adolescentes Puerto Rico, 2015. 2017. Puerto Rico Health Department. [Google Scholar]
- 6.Villarruel A, Loveland-Cherry C, Ronis D. Testing the efficacy of a computer-based parent-adolescent sexual communication intervention for Latino Parents, Fam Relat 2010. December 1;59(5):533–543. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guilamo-Ramos V, Bouris A, Lee J, McCarthy K, Michael S, Pitt-Barnes S, Dittus P. Paternal Influences on Adolescent Sexual Risk Behaviors: A Structured Literature Review. Pediatrics 2012. November;130(5):e1313–25. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cervantes R, Goldbach J, Santos S. Familia Adelante: A Multi-Risk Prevention Intervention for Latino Families. J Prim Prev 2011. August;32(3–4):225–34. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santa Maria D, Markham C, Bluethmann S, Mullen P. Parent-Based Adolescent Sexual Health Interventions and Effect on Communication Outcomes: A Systematic Review and Meta-Analyses. Perspect Sex Repro H 2015. March;47(1):37–50. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sutton M, Lasswell S, Lanier Y, Miller K. Impact of Parent-Child Communication Interventions on Sex Behaviors and Cognitive Outcomes for Black/African American and Hispanic/Latino Youth: A Systematic Review, 1988–2012. J Adolesc Health 2014. Apr; 54(4):369–84. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wight D, Fullerton D. A Review Interventions with Parents to Promote Sexual Health of Their Children. J Adolesc Health 2013. January;52(1):4–27. PMID: [DOI] [PubMed] [Google Scholar]
- 12.Wang B, Stanton B, Deveaux L, Li X, Koci V, Lunn S. The impact of parent involvement in an effective adolescent risk reduction intervention on sexual risk communication and adolescent outcomes. AIDS Educ Prev 2014. December;26(6):500–20. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weekes C, Haas B, Gosselin K. Expectations and Self-Efficacy of African American Parents Who Discuss Sexuality with their Adolescent Sons: An Intervention Study. Public Health Nurs 2014. May-Jun;31(3):253–61. PMID: [DOI] [PubMed] [Google Scholar]
- 14.Bogart LM, Skinner D, Thurston IB, Toefy Y, Klein DJ, Hu CH, Schuster MA. Let’s talks!, A south African Worksite-Based HIV Intervention Parenting Program. J Adolesc Health 2013. November; 53(5):602–8. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cupp PK, Atwood KA, Byrnes HF, Miller BA, Fongkaew W, Chamratrithirong A, Rhucharoenpornpanich O, Rosati MJ, Chookhare W. The Impact of Thai Family Matters on Parent/Adolescent Sexual Risk Communication Attitudes and Behavior. J Health Commun 2013;18(11):1384–96. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prado G, Cordova D, Huang S, Estrada Y, Rosen A, Bacio GA, Leon Jimenez G, Pantin H, Brown CH, Velazquez MR, Villamar J, Freitas D, Tapia MI, McCollister K. The efficacy of Familias Unidas on drug and alcohol outcomes for Hispanic delinquent youth: Main effects and interaction effects by parental stress and social support. Drug and Alcohol Depend 2012. September;125 Suppl 1:S18–25. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villarruel A, Cherry CL, Cabriales EG, Zhou Y. A parent-adolescent intervention to increase sexual risk communication: results of a randomized controlled trial. AIDS Educ Prev 2008. October;20(5):371–83. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guilamo-Ramos V, Lee J, Kantor L, Levine D, Baum S, Johnsen J Potential for Using Online and Mobile Education with Parents and Adolescents to Impact Sexual and Reproductive Health. Prev Sci 2015. January;16(1):53–60. PMID: [DOI] [PubMed] [Google Scholar]
- 19.Villarruel AM, Loveland-Cherry C, Gallegos Cabriales EC, Ronis D, Zhou Y (2008). A parent-adolescent intervention to increase sexual risk communication: results of a randomized controlled trial. AIDS Education and Prevention, 20 (5), 371–383. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee YM, Dancy B, Florez E, Holm K. Factors related to sexual practices and successful sexually transmitted infection/HIV intervention programs for Latino adolescents. Public Health Nurs 2013. Sep-Oct;30(5):390–401. PMID: [DOI] [PubMed] [Google Scholar]
- 21.Ortiz AP, Soto-Salgado M, Suárez E, del Carmen Santos-Ortiz M, Tortolero-Luna G, & Pérez CM (2011). Sexual behaviors among adults in Puerto Rico: a population-based study. J Sex Med, 8 (9):2439–49. doi: 10.1111/j.1743-6109.2011.02329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Department of Health PR (2013). Programa Educativo de Responsabilidad Personal para Adolescentes en Puerto Rico (PR-PREP). Division of Mothers, Children and Adolescents, San Juan, Puerto Rico. [Google Scholar]
- 23.Sanjurjo L (2013). “Lamentable” el inicio temprano de la sexualidad. Primera Hora. Accessed on Dec 20, 2017 at http://www.primerahora.com/noticias/puerto-rico/nota/lamentableeliniciotempranodelasexualidad-956944/
- 24.Perrino T, Gonzalez-Soldevilla A, Pantin H, & Szapocznik J (2000). The role of families in adolescent HIV Prevention: A Review. Clinical Child and Family Psychology Review, 3(2), 81–96. PMID: [DOI] [PubMed] [Google Scholar]
- 25.Ajzen I From intentions to actions: A theory of planned behavior In: Kuhl J, Beckmann J, editors. Action control: From cognition to behavior. Heidelberg: Springer; 1985. p. 11–39. [Google Scholar]
- 26.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, N.J.: Prentice-Hall; 1980. [Google Scholar]
- 27.Bandura A Perceived self-efficacy. In: Mays VM, Albee GW, Schneider SF, editors. Primary prevention of AIDS: Psychological approaches. Newbury Park (CA): Sage; 1989. p. 128–141. [Google Scholar]
- 28.Bandura A Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, N.J.: Prentice-Hall; 1986. [Google Scholar]
- 29.Bandura A Self-efficacy mechanism in human agency. Am Psychol. 1982; 37(2):122. [Google Scholar]
- 30.Villarruel, A.M. & Varas-Diaz, N. (2012). Testing a Latino web-based parent-adolescent sexual communication intervention. Co-PI. NIH, NINR.R01NR013505 [DOI] [PMC free article] [PubMed]
- 31.Zeger SL, Liang KY: Longitudinal data analysis for discrete and continuous outcomes. Biometrics 1986, 42(1):121–130. [PubMed] [Google Scholar]
- 32.Liang KY, Zeger SL: Longitudinal data analysis using generalized linear models. Biometrika 1986, 73(1):13–22. [Google Scholar]
- 33.Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology 2005;89(6):852–63. doi: 10.1037/0022-3514.89.6.852 [DOI] [PubMed] [Google Scholar]
- 34.Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 35.Van Buuren S Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007; 16(3):219–42. PMID: [DOI] [PubMed] [Google Scholar]


