Abstract
Aims
Coronary computed tomography angiography (CTA) has emerged as a non-invasive diagnostic method for patients with suspected coronary artery disease, but its usefulness in patients with complex coronary artery disease remains to be investigated. The present study sought to determine the agreement between separate heart teams on treatment decision-making based on either coronary CTA or conventional angiography.
Methods and results
Separate heart teams composed of an interventional cardiologist, a cardiac surgeon, and a radiologist were randomized to assess the coronary artery disease with either coronary CTA or conventional angiography in patients with de novo left main or three-vessel coronary artery disease. Each heart team, blinded for the other imaging modality, quantified the anatomical complexity using the SYNTAX score and integrated clinical information using the SYNTAX Score II to provide a treatment recommendations based on mortality prediction at 4 years: coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), or equipoise between CABG and PCI. The primary endpoint was the agreement between heart teams on the revascularization strategy. The secondary endpoint was the impact of fractional flow reserve derived from coronary CTA (FFRCT) on treatment decision and procedural planning. Overall, 223 patients were included. A treatment recommendation of CABG was made in 28% of the cases with coronary CTA and in 26% with conventional angiography. The agreement concerning treatment decision between coronary CTA and conventional angiography was high (Cohen’s kappa 0.82, 95% confidence interval 0.74–0.91). The heart teams agreed on the coronary segments to be revascularized in 80% of the cases. FFRCT was available for 869/1108 lesions (196/223 patients). Fractional flow reserve derived from coronary CTA changed the treatment decision in 7% of the patients.
Conclusion
In patients with left main or three-vessel coronary artery disease, a heart team treatment decision-making based on coronary CTA showed high agreement with the decision derived from conventional coronary angiography suggesting the potential feasibility of a treatment decision-making and planning based solely on this non-invasive imaging modality and clinical information.
Trial registration number
Keywords: SYNTAX, Percutaneous coronary intervention, Coronary artery bypass grafting, Computed tomography angiography
Introduction
Myocardial revascularization improves survival in patients with multivessel coronary artery disease.1 The selection of a surgical or catheter-based therapy relies on patient’s preference, clinical comorbidities, and complexity of coronary artery disease. The American and European guidelines support a heart team approach for the decision-making process regarding the revascularization strategy and recommend the evaluation of the anatomical complexity using the SYNTAX score.2,3
Invasive coronary angiography has been the preferred diagnostic modality to assess the extent and severity of the coronary artery disease. Coronary computed tomography angiography (CTA) has emerged as a non-invasive method able to assess the degree of epicardial coronary narrowing, and its physiological repercussion by means of fractional flow reserve derived from computed tomography (FFRCT).4–6 Moreover, the calculation of the SYNTAX score derived from coronary CTA has been shown to be accurate with respect to the one derived from invasive angiographic assessment.7 The integration of the anatomical SYNTAX score with patient’s clinical characteristics and comorbidities using the SYNTAX Score II, provides a treatment recommendation based on the predicted 4-year mortality in patients undergoing coronary artery bypass grafting surgery (CABG) or percutaneous coronary intervention (PCI).8,9
Technological advancements in the field of coronary computed tomography (CT) allowed for expanding its use to patients with known coronary artery disease. However, the diagnostic performance of the latest generation of CT scanners and the agreement on treatment decision in patients with multivessel coronary artery disease remains to be investigated. The present study sought to determine the agreement between separate heart teams on treatment recommendation based either on coronary CTA or conventional angiography in patients with left main or three-vessel coronary artery disease.
Methods
Study design
The design of the SYNTAX III REVOLUTION Trial: A Randomized Study Investigating the Use of CT Scan and Angiography of the Heart to Help the Doctors Decide Which Method is the Best to Improve Blood Supply to the Heart in Patients With Complex Coronary Artery Disease has been reported previously.10 The trial was an international, multicentre study, randomizing separate heart teams to make a treatment decision between CABG and PCI, using either coronary CTA or conventional angiography, while blinded to the other imaging modality. Details of the organization of the study and protocol are provided in the Supplementary material online, Appendix. The trial was approved by the investigational review board or ethics committee at each participating centre. The study was sponsored by the European Cardiovascular Research Institute (ECRI, Rotterdam, the Netherlands) with unrestricted grants from GE Healthcare (Chicago, IL, USA) and Heart Flow Inc. (Redwood City, CA, USA). The principal investigators (the first two authors and the corresponding authors) had unrestricted access to the data, were involved in the analysis and interpretation of the data. The principal investigators guarantee the completeness and accuracy of the data and analyses and the fidelity of the trial to the protocol.
Enrolment and randomization
Patients with left main or three-vessel coronary artery disease, diagnosed with either coronary CTA or conventional angiography and candidates for either CABG or PCI were assessed for eligibility. Patients were consented to participate in a randomized trial of decision making between CABG and PCI performed by the local heart team. In addition to the diagnostic method used for assessment of eligibility, patients underwent evaluation with the alternative imaging modality. Separate heart teams constituted by an interventional cardiologist, a cardiac surgeon, and a radiologist specialized in cardiac imaging were randomized to either assess the coronary anatomy with coronary CTA or conventional angiography in addition to the patient’s clinical information. Randomization was performed by a web-based system. Each heart team calculated the anatomical SYNTAX score based solely on their allocated imaging modality and subsequently integrated the clinical information to compute the SYNTAX Score II risk prediction model providing a treatment recommendation, i.e. CABG, PCI, or equipoise between CABG and PCI. The SYNTAX Score II is a validated tool predicting patient-specific 4-year mortality based on age, gender, kidney function, left ventricular ejection fraction, presence of chronic obstructive pulmonary disease, and peripheral vascular disease.9,11 Angiographic characteristics such as the presence of left main stem disease and the anatomical SYNTAX score are also accounted for in the calculation.11 Finally, the heart team selected the revascularization strategy and planned the procedure (i.e. CABG or PCI). Any anatomical SYNTAX score was eligible for screening and patients with anatomical SYNTAX score >33 were not excluded.12 Patients with prior revascularization were excluded. Complete details of the inclusion and exclusion criteria are provided in the Supplementary material online, Table S1.
Image acquisition and analysis
Coronary CTA was performed with the GE Revolution CT scanner that has a nominal spatial resolution of 230 microns along the X–Y planes, a rotational speed of 0.28 s, and a Z-plane coverage of 16 cm enabling to image the heart in one heartbeat.13 A proprietary post-processing algorithm allowed for the correction of motion artefacts.13 The imaging acquisition guidelines are detailed in the Supplementary material online, Table S2. The protocol mandated the use of nitrates prior to CT acquisition and beta-blockers in cases of heart rate higher than 65 b.p.m. Image quality was assessed using the five-point Likert scale at the patient level.14 Severity and extension of coronary artery disease were assessed using the anatomical SYNTAX score, coronary segments with narrowing with visual diameter stenosis >50% using coronary CTA, or conventional angiography and weighted according to their location in the coronary tree were included in the calculation.15–18 For the primary endpoint, the two local heart teams made their decision on the choice of revascularization mode based on their clinical and anatomical assessment.
For the secondary endpoint, the FFRCT was used to calculate the non-invasive functional SYNTAX score, which was computed by the core laboratory (Cardialysis BV, Rotterdam, the Netherlands) subtracting non-flow limiting stenosis (FFRCT >0.80) from the coronary CTA-derived anatomical SYNTAX score.17 Finally, the non-invasive functional SYNTAX score was used to calculate the SYNTAX Score III, which is conceptually a combination of coronary anatomical complexity with its physiological repercussion and patient’s clinical characteristics and comorbidities.
Objectives and endpoints
The trial was designed to determine the agreement between separate heart teams on treatment recommendation and planning based either on coronary CTA (with and without FFRCT) or conventional angiography. The primary endpoint based on anatomical assessment was the agreement, assessed by Cohen’s kappa, on the revascularization strategy between separate heart teams.
For the secondary endpoints, the heart team allocated to coronary CTA received the FFRCT and made a second treatment recommendation integrating the functional assessment. Finally, both heart teams were unblinded to all imaging modalities and made a final clinical decision on the revascularization strategy. Definitions of the endpoints are provided in Supplementary material online, Table S3in the Appendix.
Statistical analysis
For both diagnostic imaging strategies, the heart team’s treatment recommendation led to one of three decisions according to the SYNTAX Score II: (i) CABG, patients should be treated by CABG due to a higher 4-year mortality with PCI, (ii) PCI, patients should be treated by PCI due to a higher 4-year mortality with CABG, and (iii) equipoise between CABG and PCI, patients could be treated by either approach, considering that the 4-year mortality prediction is similar between the two revascularization modalities.
The primary endpoint was the agreement upon two treatment recommendations of CABG or PCI/equipoise. The SYNTAX III REVOLUTION Trial was powered to show a substantial agreement (Cohen’s kappa 0.60–0.80) between the separate heart team’s treatment recommendations based on the allocated imaging modality.10,19 Given the assumption that both coronary CTA and conventional angiography diagnostic algorithms will result in a CABG treatment recommendation in 30% of patients, we estimated that a random heart team assignment of 223 patients would provide a 90% power to show at least substantial agreement (at a two-sided alpha level of 0.05), assuming an attrition rate of 10%.17,19 The agreement on the SYNTAX score between the two imaging modalities was assessed by the Bland–Altman and Passing Bablok method.20,21 Categorical variables were compared with the use of the McNemar. Continuous variables were compared with the use of Student’s t-test or the Wilcoxon rank-sum test for non-normally distributed data. A two-sided P-value of 0.05 or less was considered to indicate statistical significance. All statistical analyses were performed with the use of SAS software, version 9.4 (SAS Institute).
Results
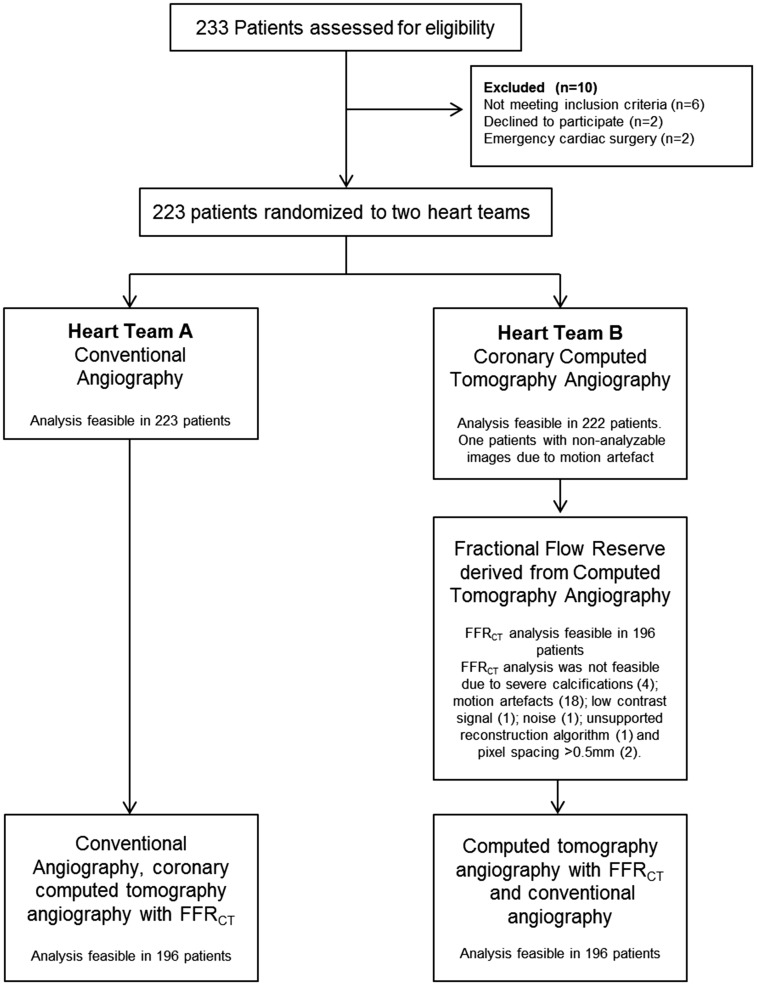
From 29 June 2016 to 8 February 2018, 223 patients with left main or three-vessel coronary artery disease were enrolled in six centres from five European countries. Figure 1 shows the study flow chart and Supplementary material online, Table S4 in the Appendix shows the method used for screening.
Figure 1.
A flow chart of the study. FFRCT, fractional flow reserve derived from coronary computed tomography angiography.
Baseline clinical and angiographic characteristics
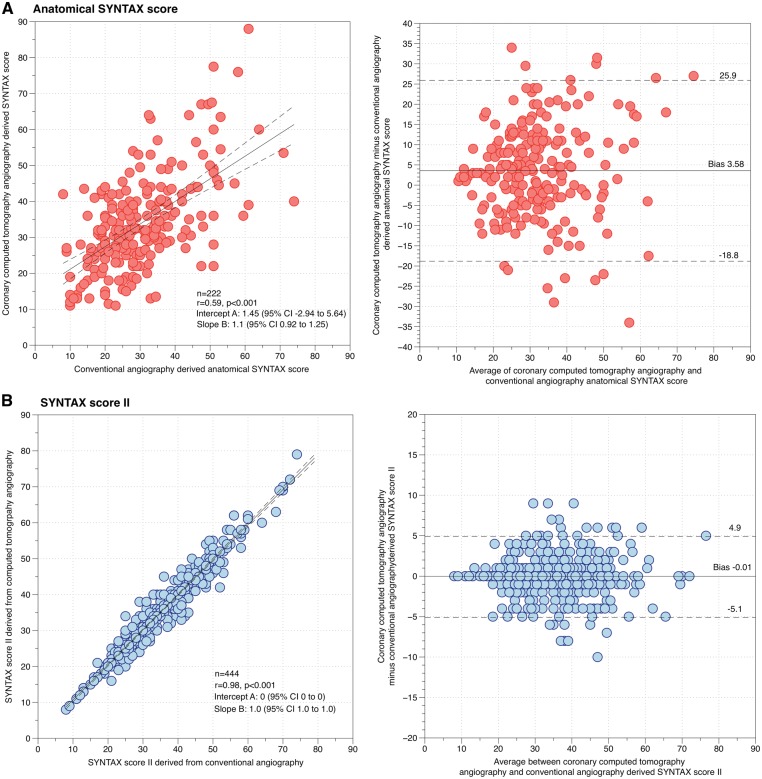
Baseline clinical characteristics are shown in Table 1. The five-point Likert score was 3.15 ± 0.95. The radiation dose (effective dose) was significantly lower with CTA compared with conventional angiography (5.0 ± 3.0 mSv vs. 10.1 ± 16 mSv, P < 0.0001). Using coronary CTA, 1108 stenoses (5.0 ± 1.7 per patient) were detected. The mean anatomical SYNTAX score derived from coronary CTA was 33.9 ± 13.0. Conventional coronary angiography identified 1073 stenoses (4.8 ± 1.7 per patient) with a mean SYNTAX score of 30.3 ± 12.2. Details of the SYNTAX score, its components and differences between the diagnostic imaging modalities are shown in Table 2 and Take home figure shows a case example. The mean difference between coronary CTA and conventional angiography-derived SYNTAX score was 3.58 (limits of agreement −18.8 to 25.9) with a correlation coefficient of 0.59 (P < 0.0001) without systematic or proportional differences (Figure 2A). The agreement on diseased segments between imaging modalities was observed in 85% of the cases.
Table 1.
Baseline clinical characteristics
| Characteristics | N = 223 patients |
|---|---|
| Demographics | |
| Age (years), mean ± SD | 67.6 ± 8.9 |
| Male (%, n) | 84.3 (188/223) |
| Coronary artery disease risk factors | |
| Current smoking (%, n) | 22.6 (48/212) |
| Diabetes mellitus (%, n) | 37.7 (84/223) |
| Treatment for diabetes (%, n) | |
| Insulin | 10.3 (23/223) |
| Medication | 25.6 (57/223) |
| Diet | 0.9 (2/223) |
| Hypertension (%, n) | 74.9 (167/223) |
| Hyperlipidaemia (%, n) | 70.0 (154/220) |
| Family history of CAD (%, n) | 35.6 (67/188) |
| Medical history | |
| Previous stroke (%, n) | 8.1 (18/223) |
| Previous myocardial infarction (%, n) | 0.9 (2/220) |
| COPD (%, n) | 13.0 (29/223) |
| PVD (%, n) | 17.5 (39/223) |
| Clinical presentation | |
| Silent ischaemia (%, n) | 42.2 (94/223) |
| Stable angina (%, n) | 48.9 (109/223) |
| CCS class (%, n) | |
| I | 15.6 (17/109) |
| II | 56.0 (61/109) |
| III | 25.7 (28/109) |
| IV | 2.8 (3/109) |
| Unstable angina (%, n) | 9.0 (20/223) |
| BMI (kg/m2), mean ± SD | 26.5 ± 3.7 |
| Creatinine clearance (mL/min) mean ± SD | 81.6 ± 27.5 |
| LVEF (%), mean ± SD | 54.6 ± 11.0 |
| Heart rate during CT acquisition, mean ± SD | 54.6 ± 11.0 |
BMI, body mass index; CAD, coronary artery disease; CCS, Canadian Cardiovascular Society; COPD, chronic obstructive pulmonary disease; LVEF, left ventricle ejection fraction; SD, standard deviation.
Table 2.
Comparison of the anatomical SYNTAX score and SYNTAX score II and its components
| Characteristics | Heart team assessment based on conventional angiography | Heart team assessment based on coronary CTA | P-value |
|---|---|---|---|
| Anatomical SYNTAX score, per patient | 30.3 ± 12.2 | 33.9 ± 13.0 | <0.001 |
| Diseased vessels | |||
| Left main | 28.7% (64/223) | 36.0% (80/222) | 0.10 |
| RCA | 92.4% (206/223) | 95.5% (212/222) | 0.54 |
| LAD | 96.4% (215/223) | 99.5% (221/222) | 0.021 |
| LCX | 95.1% (212/223) | 95.0% (211/222) | 0.96 |
| Components anatomical SYNTAX score | |||
| Total occlusion | 14.0% (150/1073) | 12.0% (133/1108) | 0.17 |
| Bifurcation | 22.0% (236/1073) | 23.4% (259/1108) | 0.44 |
| Medina 1,0,0 | 1.7% (18/1073) | 1.1% (12/1108) | — |
| Medina 0,1,0 | 2.6% (28/1073) | 0.8% (9/1108) | — |
| Medina 1,1,0 | 4.4% (47/1073) | 6.9% (77/1108) | — |
| Medina 1,1,1 | 6.8% (73/1073) | 8.6% (95/1108) | — |
| Medina 0,0,1 | 2.4% (26/1073) | 1.8% (20/1108) | — |
| Medina 1,0,1 | 2.2% (24/1073) | 1.9% (21/1108) | — |
| Medina 0,1,1 | 1.9% (20/1073) | 2.3% (25/1108) | — |
| Aorto ostial lesion | 3.3% (35/1073) | 3.6% (40/1108) | 0.70 |
| Severe tortuositya | 2.2% (24/1073) | 0.9% (10/1108) | 0.014 |
| Length >20 mm | 29.1% (269/923) | 30.4% (296/975) | 0.51 |
| Heavy calcificationb | 13.0% (140/1073) | 28.9% (320/1108) | <0.001 |
| Thrombus | 0.3% (3/1073) | 0.3% (3/1108) | 1.0 |
| SYNTAX score II for PCI | 35.9 ± 10.8 | 36.8 ± 10.9 | 0.38 |
| PCI 4-year mortality (%) | 14.9 ± 14.7 | 16.0 ± 15.8 | <0.001 |
| SYNTAX score II for CABG | 32.0 ± 11.7 | 32.2 ± 11.6 | 0.86 |
| CABG 4-year mortality (%) | 11.8 ± 12.8 | 12.0 ± 12.8 | 0.87 |
CABG, coronary bypass graft; LAD, left anterior descending; LCX, left circumflex; PCI, percutaneous coronary intervention; RCA, right coronary artery.
One or more bends of 90° or more, or three or more bends of 45° to 90° proximal of the diseased segment.
For computed tomography angiography defined as presence of calcium that encompasses more than 50% of the cross-sectional area of the vessel at any location within the specific lesion. For invasive angiography defined as multiple persisting opacifications of the coronary wall visible in more than one projection surrounding the complete lumen of the coronary artery at the site of the lesion.
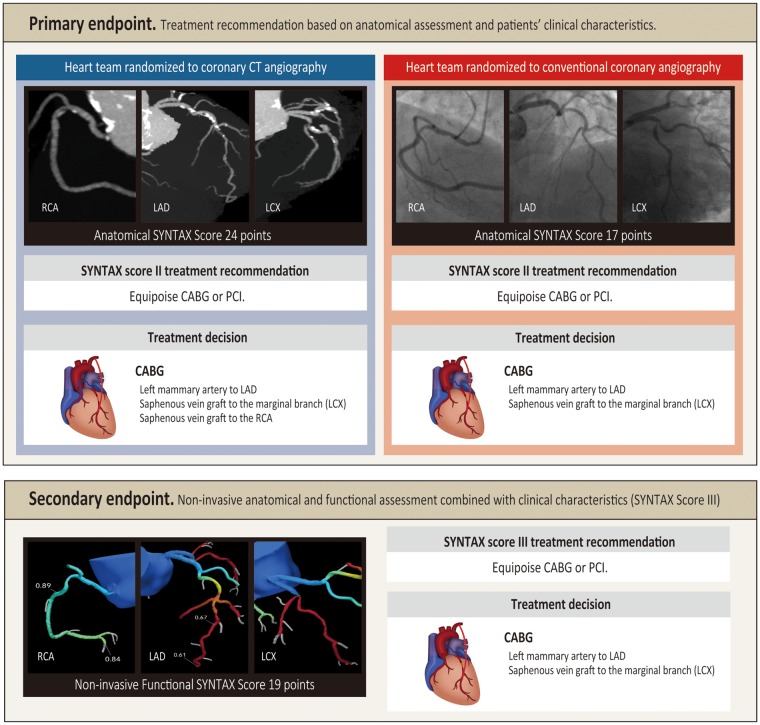
Take home figure.
Case example of the non-invasive and invasive assessment using the anatomical SYNTAX score and SYNTAX Score II. A 74-year-old man with a creatinine clearance 38 mL/min and left ventricular ejection fraction of 50% without history of chronic obstructive pulmonary disease or peripheral vascular disease. At the top, coronary computed tomography angiography shows three-vessel disease with a coronary narrowings located at the ostium and in the proximal segment of the right coronary artery; two narrowings located in the mid segment of the left anterior descending artery; and one additional narrowing in the proximal segment of the left circumflex artery involving the bifurcation with the first obtuse marginal coronary artery. Conventional angiography revealed also a three-vessel disease with one narrowing located at the proximal segment of the right coronary artery, one narrowing at the mid segment of the left anterior descending artery, and a bifurcation lesion involving the proximal segment of the left circumflex artery and the first obtuse marginal coronary artery. Each coronary narrowing was scored according to the anatomical SYNTAX score and the final anatomical SYNTAX score derived from each modality is shown. With both imaging modalities, the SYNTAX score II recommended either coronary artery bypass graft surgery or percutaneous coronary intervention based on a comparable predicted 4-year mortality. At the bottom, the non-invasive fractional flow reserve derived from coronary computed tomography angiography (FFRCT) is presented. The FFRCT showed that the lesions in the right coronary artery are not haemodynamically relevant, whereas the left anterior descending artery and left circumflex artery have haemodynamically relevant lesions. The treatment recommendation based on coronary computed tomography angiography with FFRCT remained equipoise between coronary artery bypass graft surgery and percutaneous coronary intervention but the treatment planning changed based on the negative FFRCT results in the right coronary artery. CABG, coronary artery bypass graft surgery; LAD, left anterior descending artery; LCX, left circumflex artery; PCI, percutaneous coronary intervention; RCA, right coronary artery.
Figure 2.
Correlation and agreement on the anatomical SYNTAX score (A) and SYNTAX score II (B) between coronary computed tomography angiography and conventional angiography.
Primary endpoint
The SYNTAX Score II provided a treatment recommendation of CABG in 28% of patients with the coronary CTA and in 26% with conventional angiography (Table 3). Patient’s characteristics according to the SYNTAX Score II treatment recommendation are shown in Table 4. The agreement on the anatomical SYNTAX score tertiles was fair [Kappa 0.33, 95% confidence interval (CI) 0.23–0.42; Supplementary material online, Table S5 in the Appendix]. The agreement concerning revascularization treatment recommendation between imaging modalities was almost perfect, according to the statistical nomenclature of Cohens’ kappa, with a coefficient of 0.82 (95% CI 0.73–0.90; Table 2). The mean difference between coronary CTA and conventional angiography-derived SYNTAX Score II was −0.01 (limits of agreement −5.1 to 4.9) with a correlation coefficient of 0.98 (P < 0.001) without systematic or proportional differences (Figure 2B),
Table 3.
Agreement on treatment recommendation between coronary computed tomography and conventional angiography
| Heart team treatment recommendation based on coronary computed tomography angiography |
||
|---|---|---|
| Heart team treatment recommendation based on conventional angiography | CABG | PCI/equipoise CABG and PCI |
| CABG | 23.4% (52/222) | 2.7% (6/222) |
| PCI/Equipoise CABG and PCI | 4.5% (10/222) | 69.4% (154/222) |
| Cohen’s kappa 0.82 (95% CI 0.73–0.910) | ||
| Agreement in 93% of the heart team’s treatment recommendation. | ||
CABG, coronary bypass graft; PCI, percutaneous coronary intervention.
Table 4.
Patients characteristics according to the SYNTAX score II treatment recommendation
| Characteristics | Treatment Recommendation PCI only or Equipoise PCI and CABGa (n = 165) | Treatment Recommendation CABG onlya (n = 58) | P-value |
|---|---|---|---|
| Age (years), mean ± SD | 68.5 ± 8.5 | 65.0 ± 9.5 | 0.009 |
| Male (%, n) | 95.8% (158/165) | 51.7% (30/58) | <0.001 |
| Current smoking (%, n) | 21.0% (33/157) | 27.3% (15/55) | 0.02 |
| Diabetes mellitus (%, n) | 34.5% (57/164) | 48.3% (28/58) | 0.004 |
| Hypertension (%, n) | 73.9% (122/165) | 77.6% (45/58) | 0.581 |
| Hyperlipidaemia (%, n) | 67.1% (110/164) | 78.6% (44/56) | 0.105 |
| Family history of CAD (%, n) | 31.7% (44/139) | 46.9% (23/49) | 0.055 |
| Previous stroke (%, n) | 8.5% (14/165) | 6.9% (4/58) | 1.0 |
| Previous myocardial infarction (%, n) | 1.2% (2/163) | 0.0% (0/57) | 1.0 |
| COPD (%, n) | 17.6% (29/165) | 0.0% (0/58) | <0.001 |
| PVD (%, n) | 18.8% (31/165) | 13.8% (8/58) | 0.389 |
| Creatinine clearance (mL/min), mean ± SD | 81.6 ± 24.5 | 81.8 ± 34.8 | 0.960 |
| LVEF (%), mean ± SD | 56.7 ± 9.0 | 48.9 ± 13.8 | <0.001 |
| Left main disease (%, n) | 33.9% (56/165) | 13.8% (8/58) | 0.003 |
| Anatomical SYNTAX score, per patient | 29.1 ± 12.0 | 33.8 ± 12.2 | 0.011 |
| SYNTAX score II PCI, mean ± SD | 34.2 ± 9.8 | 40.8 ± 12.0 | <0.001 |
| PCI predicted 4-year mortality (%) | 12.6 ± 11.0 | 21.4 ± 20.9 | 0.003 |
| SYNTAX score II CABG, mean ± SD | 34.1 ± 11.5 | 26.3 ± 10.3 | <0.001 |
| CABG predicted 4-year mortality (%) | 13.4 ± 13.6 | 7.2 ± 8.6 | <0.001 |
CABG, coronary artery bypass grafting; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease.
Based on the SYNTAX score II recommendation using the anatomic SYNTAX score derived from conventional angiography.
Procedural planning
Coronary artery bypass grafting was selected as the revascularization strategy in 164 patients using coronary CTA (58 patients with CABG recommendation and 106 with equipoise CABG or PCI recommendation according to the SYNTAX Score II) and in 155 patients with conventional angiography (62 patients with CABG recommendation and 106 with equipoise CABG or PCI recommendation according to the SYNTAX Score II). Overall, the heart teams agreed on the coronary segments to be revascularized in 81.1% of the cases.
Impact of physiological assessment
Fractional flow reserve derived from CTA was available for 868/1108 lesions. The mean FFRCT value was 0.64 ± 13. Non-flow limiting stenosis (FFRCT >0.80) were observed in 34% (66/196) of the patients (n = 116 lesions). Fractional flow reserve derived from coronary CTA changed the treatment decision in 7% (14/196) of the patients, in 13 patients the surgical procedure was changed to a percutaneous approach. The non-invasive functional assessment score led to a reduction in the anatomical SYNTAX of 2.9 points (95% CI 1.9–3.9) and reduced the proportion of patients with haemodynamically significant three-vessel disease from 92.3% to 78.8%. Furthermore, the use of the non-invasive functional SYNTAX score for the SYNTAX Score II calculation (SYNTAX Score III) corrected for the overestimation of the predicted mortality for PCI at 4 years (Table 2).
Unblinding and outcomes
The unblinding of conventional angiography in the CT arm changed the treatment recommendation in 9% of the cases, whereas the unblinding of CTA with FFRCT modified the treatment recommendation in 6.3% of the patients in the conventional angiography arm. The heart team’s treatment decision was concordant in 91% of the cases after unblinding to all imaging modalities.
The decisions based on coronary CTA and conventional angiography were in agreement with the treatment executed in 71% and 78% of the patients, respectively.
Discussion
By randomizing two heart teams, the present study showed that treatment decision-making based on coronary CTA is in an almost perfect agreement with the treatment decision derived from conventional coronary angiography in patients with left main or three-vessel coronary artery disease. The anatomical SYNTAX scores derived either from coronary CTA or conventional angiography showed a moderate degree of correlation, whereas the SYNTAX Score II demonstrated a high degree of correlation between the two diagnostic strategies. Furthermore, the agreement on the revascularization strategy between coronary CTA and conventional angiography reached 80%.
For patients with multivessel disease, a multidisciplinary heart team approach is currently advocated by the guidelines for treatment decision-making with a Class I recommendation level of evidence ‘C’ in the absence of evidence from randomized trial.2 The SYNTAX III REVOLUTION is the first study to randomize the heart team; the almost perfect agreement upon treatment selection supports the usefulness of coronary CTA in patients with complex coronary artery disease. It should be also recognized that in the current study the heart team routinely included a radiologist in addition to an interventional cardiologist and a cardiac surgeon, which differs from the definition of heart team in the guidelines. The interaction with the radiologist enhanced image interpretation and decision-making process.
In line with previous findings, the anatomical SYNTAX score was higher with coronary CTA compared to conventional angiography; this difference may be related to the higher sensitivity of CT in detecting calcified plaques that due to the blooming artefact may hamper luminal assessment increasing the anatomical SYNTAX score.17,22 In the present study, heavily calcified lesions were identified in 57.7% of patients with coronary computed tomography angiography and in 34.5% using conventional angiography (P < 0.001). Despite the difference observed in the anatomical SYNTAX score, the addition of clinical information mitigated that difference and improved the correlation on the 4-years mortality prediction between imaging strategies (Take home figure), resulting in a similar treatment recommendation in 93% of the cases.8
In patients with multivessel coronary artery disease, physiology-guided revascularization reduces the rate of major adverse cardiovascular events compared with an angiography guided PCI.23 In the SYNTAX II study, invasive physiological evaluation led to a reduction of 56% in the proportion of patients with haemodynamically significant three-vessel disease. Moreover, comparable proportion of patients were reclassified to a lower risk category using the functional SYNTAX score derived either from invasive pressure-wire or FFRCT assessment.17,24 The extension and severity of coronary artery disease was overestimated by coronary CTA compared with conventional angiography; this influenced the SYNTAX Score II predictions resulting in higher predicted mortality risk with the SYNTAX Score II. However, FFRCT corrected the overestimation of the anatomical SYNTAX score and adjusted the SYNTAX Score II, ensuing similar predicted outcome with respect to conventional angiography.
In the present study, the mean FFR value is the lowest reported in the literature (0.63 ± 13) reflecting the severity of coronary artery disease of the patients included in the trial. Use of FFRCT reduced the percentage of patients with significant three-vessel disease from 92.2% to 78.8%, changing treatment recommendation in 7% of patients. Furthermore, by combining anatomical complexity of the coronary artery disease with its physiological repercussion and clinical information the SYNTAX Score III enabled the heart team to refine the decision-making process regarding the optimal revascularization strategy and treatment planning of haemodynamically significant lesions in a non-invasive setting. The unblinding to both imaging modalities changed the heart team’s treatment recommendation in less than 10% of the cases supporting the almost perfect agreement observed in the primary endpoint. Also, the design of the present trial allows us to determine the heart team’s treatment recommendation variability based on multimodality imaging. In 91% of the cases, treatment recommendations were concordant between heart teams.
Previous attempts of using non-invasive coronary CT imaging in patients with three-vessel disease have shown moderate feasibility.17 In this trial, a new CT scanner was selected that could acquire the heart in one beat with high temporal resolution and high-definition spatial resolution. Such technology rendered feasible the conduction of the present study and enabled a high analysability rate along with a robust feasibility for FFRCT processing in this complex population. Moreover, the effective dose was lower with CT compared with conventional angiography, confirming the safety of new scanners in term of radiation dose. These findings support the expansion of coronary CTA to patients with complex coronary artery disease.
The present study must be cautiously interpreted with respect to some limitations. First, in the SYNTAX III REVOLUTION population several subgroups were under-represented such as women, patients with low ejection fraction, and patients with unstable clinical presentation. Second, the unblinding to the alternative imaging modality prior to the final clinical decision precluded the investigation of the safety and feasibility of this strategy solely based on non-invasive imaging. Furthermore, in absence of outcome data a strategy solely based on non-invasive imaging to select patients for surgery cannot be recommended; an outcome trial with treatment selection based on coronary CT is warranted and is currently in design. Third, inherent to the decision-making trial design, treatment selection bias cannot be excluded, but it was reassuring to observe a comparable proportion of agreement between the executed treatment and the coronary CTA or conventional angiography arms. Nevertheless, it should be acknowledged that in 28% with coronary CTA and 21% with conventional angiography the treatment recommendation differed from the treatment executed. Finally, only one type of CT scanner was used in SYNTAX III REVOLUTION, if these results can be extrapolated to other technologies requires further investigation.
Conclusion
In patients with left main or three-vessel coronary artery disease, a heart team treatment decision-making based coronary CTA showed a high agreement with the decision derived from conventional coronary angiography suggesting the potential feasibility of a treatment decision-making based solely on this non-invasive imaging modality and clinical information.
Supplementary Material
Acknowledgments
We acknowledge Hans-Peter Stoll for his contribution and support to the SYNTAX III Revolution trial.
Funding
The European Cardiovascular Research Institute (ECRI) sponsored this study with unrestricted research grants from GE Health Care and Heart Flow Inc.
Conflict of interest: C.C. reports receiving grants from Heartflow Inc and Biosensors. P.W.S. reports consultancy fees from Abbott, Biosensors, Medtronic, Micell, Qualimed, Sinomedical Sciences, St. Jude Medical, Stentys, Svelte Medical Systems, Philips/Volcano, Xeltis, StentIt and HeartFlow. G.P. reports receiving research grant or fee as speaker from GE Helathcare, Bracco, Bayer, Medtronic and Heartflow Inc. The other authors report no conflict of interest.
Footnotes
See page 3699 for the editorial comment on this article (doi: 10.1093/eurheartj/ehy578)
This paper was guest edited by Anthony DeMaria, La Jolla, USA.
References
- 1. Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, Davis K, Killip T, Passamani E, Norris R.. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet 1994;344:563–570. [DOI] [PubMed] [Google Scholar]
- 2. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Juni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A.. 2014 ESC/EACTS Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541–2619. [DOI] [PubMed] [Google Scholar]
- 3. Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, Fonarow GC, Lange RA, Levine GN, Maddox TM, Naidu SS, Ohman EM, Smith PK.. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2014;130:1749–1767. [DOI] [PubMed] [Google Scholar]
- 4. Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, Paul N, Clouse ME, Shapiro EP, Hoe J, Lardo AC, Bush DE, de Roos A, Cox C, Brinker J, Lima JA.. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008;359:2324–2336. [DOI] [PubMed] [Google Scholar]
- 5. Voros S, Rinehart S, Qian Z, Joshi P, Vazquez G, Fischer C, Belur P, Hulten E, Villines TC.. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging 2011;4:537–548. [DOI] [PubMed] [Google Scholar]
- 6. Norgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, Jensen JM, Mauri L, De Bruyne B, Bezerra H, Osawa K, Marwan M, Naber C, Erglis A, Park SJ, Christiansen EH, Kaltoft A, Lassen JF, Botker HE, Achenbach S; Group NXTTS. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63:1145–1155. [DOI] [PubMed] [Google Scholar]
- 7. Papadopoulou SL, Girasis C, Dharampal A, Farooq V, Onuma Y, Rossi A, Morel MA, Krestin GP, Serruys PW, de Feyter PJ, Garcia Garcia HM.. CT-SYNTAX score: a feasibility and reproducibility study. JACC Cardiovasc Imaging 2013;6:413–415. [DOI] [PubMed] [Google Scholar]
- 8. Farooq V, van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, Kappetein AP, Colombo A, Holmes DR Jr, Mack M, Feldman T, Morice MC, Stahle E, Onuma Y, Morel MA, Garcia-Garcia HM, van Es GA, Dawkins KD, Mohr FW, Serruys PW.. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 2013;381:639–650. [DOI] [PubMed] [Google Scholar]
- 9. Cavalcante R, Sotomi Y, Lee CW, Ahn JM, Farooq V, Tateishi H, Tenekecioglu E, Zeng Y, Suwannasom P, Collet C, Albuquerque FN, Onuma Y, Park SJ, Serruys PW.. Outcomes after percutaneous coronary intervention or bypass surgery in patients with unprotected left main disease. J Am Coll Cardiol 2016;68:999–1009. [DOI] [PubMed] [Google Scholar]
- 10. Cavalcante R, Onuma Y, Sotomi Y, Collet C, Thomsen B, Rogers C, Zeng Y, Tenekecioglu E, Asano T, Miyasaki Y, Abdelghani M, Morel MA, Serruys PW.. Non-invasive Heart Team assessment of multivessel coronary disease with coronary computed tomography angiography based on SYNTAX score II treatment recommendations: design and rationale of the randomised SYNTAX III Revolution trial. EuroIntervention 2017;12:2001–2008. [DOI] [PubMed] [Google Scholar]
- 11. Sotomi Y, Collet C, Cavalcante R, Morel MA, Suwannasom P, Farooq V, van Gameren M, Onuma Y, Serruys PW.. Tools and techniques—clinical: SYNTAX score II calculator. EuroIntervention 2016;12:120–123. [DOI] [PubMed] [Google Scholar]
- 12. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW.. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961–972. [DOI] [PubMed] [Google Scholar]
- 13. Andreini D, Pontone G, Mushtaq S, Mancini ME, Conte E, Guglielmo M, Volpato V, Annoni A, Baggiano A, Formenti A, Ditali V, Perchinunno M, Fiorentini C, Bartorelli AL, Pepi M.. Image quality and radiation dose of coronary CT angiography performed with whole-heart coverage CT scanner with intra-cycle motion correction algorithm in patients with atrial fibrillation. Eur Radiol 2018;28:1383–1392. [DOI] [PubMed] [Google Scholar]
- 14. Khan MF, Herzog C, Landenberger K, Maataoui A, Martens S, Ackermann H, Moritz A, Vogl TJ.. Visualisation of non-invasive coronary bypass imaging: 4-row vs. 16-row multidetector computed tomography. Eur Radiol 2005;15:118–126. [DOI] [PubMed] [Google Scholar]
- 15. Leaman DM, Brower RW, Meester GT, Serruys P, van den Brand M.. Coronary artery atherosclerosis: severity of the disease, severity of angina pectoris and compromised left ventricular function. Circulation 1981;63:285–299. [DOI] [PubMed] [Google Scholar]
- 16. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, Morice MC, Colombo A, Bass E, Leadley K, Dawkins KD, van Es GA, Morel MA, Mohr FW.. Assessment of the SYNTAX score in the Syntax study. EuroIntervention 2009;5:50–56. [DOI] [PubMed] [Google Scholar]
- 17. Collet C, Miyazaki Y, Ryan N, Asano T, Tenekecioglu E, Sonck J, Andreini D, Sabate M, Brugaletta S, Stables RH, Bartorelli A, de Winter RJ, Katagiri Y, Chichareon P, De Maria GL, Suwannasom P, Cavalcante R, Jonker H, Morel MA, Cosyns B, Kappetein AP, Taggart DT, Farooq V, Escaned J, Banning A, Onuma Y, Serruys PW.. Fractional flow reserve derived from computed tomographic angiography in patients with multivessel CAD. J Am Coll Cardiol 2018;71:2756–2769. [DOI] [PubMed] [Google Scholar]
- 18. Mushtaq S, De Araujo Goncalves P, Garcia-Garcia HM, Pontone G, Bartorelli AL, Bertella E, Campos CM, Pepi M, Serruys PW, Andreini D.. Long-term prognostic effect of coronary atherosclerotic burden: validation of the computed tomography-Leaman score. Circ Cardiovasc Imaging 2015;8:e002332.. [DOI] [PubMed] [Google Scholar]
- 19. Sim J, Wright CC.. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther 2005;85:257–268. [PubMed] [Google Scholar]
- 20. Bland JM, Altman DG.. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 1995;346:1085–1087. [DOI] [PubMed] [Google Scholar]
- 21. Bablok W, Passing H, Bender R, Schneider B.. A general regression procedure for method transformation. Application of linear regression procedures for method comparison studies in clinical chemistry, Part III. J Clin Chem Clin Biochem 1988;26:783–790. [DOI] [PubMed] [Google Scholar]
- 22. Vavere AL, Arbab-Zadeh A, Rochitte CE, Dewey M, Niinuma H, Gottlieb I, Clouse ME, Bush DE, Hoe JW, de Roos A, Cox C, Lima JA, Miller JM.. Coronary artery stenoses: accuracy of 64-detector row CT angiography in segments with mild, moderate, or severe calcification–a subanalysis of the CORE-64 trial. Radiology 2011;261:100–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. De Bruyne B, Pijls NHJ, Kalesan B, Barbato E, Tonino PAL, Piroth Z, Jagic N, Möbius-Winkler S, Mobius-Winckler S, Rioufol G, Witt N, Kala P, MacCarthy P, Engström T, Oldroyd KG, Mavromatis K, Manoharan G, Verlee P, Frobert O, Curzen N, Johnson JB, Jüni P, Fearon WF.. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991–1001. [DOI] [PubMed] [Google Scholar]
- 24. Escaned J, Collet C, Ryan N, Luigi De Maria G, Walsh S, Sabate M, Davies J, Lesiak M, Moreno R, Cruz-Gonzalez I, Hoole SP, Ej West N, Piek JJ, Zaman A, Fath-Ordoubadi F, Stables RH, Appleby C, van Mieghem N, van Geuns RJ, Uren N, Zueco J, Buszman P, Iniguez A, Goicolea J, Hildick-Smith D, Ochala A, Dudek D, Hanratty C, Cavalcante R, Kappetein AP, Taggart DP, van Es GA, Morel MA, de Vries T, Onuma Y, Farooq V, Serruys PW, Banning AP.. Clinical outcomes of state-of-the-art percutaneous coronary revascularization in patients with de novo three vessel disease: 1-year results of the SYNTAX II study. Eur Heart J 2017;38:3124–3134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.