Summary:
Objective:
Epilepsy is a common neurological condition that is often associated with stigmatizing attitudes and negative stereotypes among the general public. This randomized controlled trial (RCT) tested two new communication approaches targeting epilepsy stigma vs. an education-alone approach
Methods:
Two brief stigma-reduction videos were developed, informed by community stakeholder input; one highlighted role competency in people with epilepsy; the other, social inclusion of people with epilepsy. A control video was also developed. A web-based survey using a prospective RCT design compared effects of experimental videos and control on acceptability, perceived impact, epilepsy knowledge, and epilepsy stigma. Epilepsy knowledge and stigma were measured with the Epilepsy Knowledge Questionnaire (EKQ) and Attitudes and Beliefs about Living with Epilepsy (ABLE) respectively.
Results:
295 participants completed the study. Mean age was 23.1 (SD 3.27) years, 59.0% male, 71.4% white. Overall, respondents felt videos impacted their epilepsy attitudes. EKQ scores were similar across videos, with a trend for higher knowledge in experimental videos versus control (p = 0.06). The role competency and control videos were associated with slightly better perceived impact on attitudes. There were no differences between videos on ABLE scores (p=0.568). There were sub-group differences suggesting that men, younger individuals, whites, and those with personal epilepsy experience had more stigmatizing attitudes.
Significance:
This RCT tested communication strategies to improve knowledge and attitudes about epilepsy. While this initial effort will require follow-up, we have demonstrated the acceptability, feasibility and potential of novel communication strategies to target epilepsy stigma, and a web-based approach for assessing them.
Keywords: seizures, stereotypes, discrimination
Introduction:
Epilepsy is a common neurological condition that causes stress and burden for people with epilepsy. In addition to the challenges related to seizures and to having a chronic health condition, people with epilepsy often experience stigmatizing attitudes and negative stereotypes among the general public.1 An overarching goal of the U.S. Healthy People 2020 health promotion initiative is to create social and physical environments that promote good health for all.2 This is especially relevant for people with epilepsy; a recent systematic review on epilepsy stigma suggests that stigma remains pervasive and encompasses a number of differing negative attitudes and beliefs.3 In the U.S., decades of public awareness and education campaigns have sought to increase knowledge about the disorder, and stress the competence, success and “normality” of people with epilepsy.4; 5 National efforts to increase knowledge and to emphasize inclusion might explain why some of the most blatant historically stigmatizing beliefs, such as the notion that epilepsy is due to witchcraft or is contagious, are no longer widely prevalent among the general population in Western and industrialized countries.6
However, subtle forms of stigma rooted in basic negative emotional reactions rather than knowledge may be more resistant to change. Stigma can continue to cause difficulties and burden for people with epilepsy.3 People report expecting to feel distressed when seeing a person having a seizure which may cause them to avoid a person with epilepsy.3; 6 How to best identify and ameliorate stigma by targeting misperceptions and emotional reactions of the public remains unclear.
Because mental health conditions are generally stigmatizing and socially excluding, research in this area, which stresses social inclusion, can help inform how epilepsy stigma might be targeted and further reduced.7 Somewhat counter-intuitively, protest against stigma, which involves identifying instances of incorrect ideas or discrimination and speaking out against them, can potentially exacerbate discrimination against stigmatized people because they are singled out as different from members of general society.7
Additionally, the health communications literature7–10 provides insight into how public messaging can help influence attitudes and decision- making. Decision Theory posits that people may have difficulty resisting and refuting negative information. In an alternative approach, correct positive information can be provided.11 For example, simply stating “people with epilepsy aren’t stupid” can plant the connection of epilepsy with stupidity in a listener’s mind. A preferred approach is to remain positive, avoid negative connections entirely, and stress the role competence of people with epilepsy, such as the statement “Most people with epilepsy are bright, engaged, and living full lives.” Finally, thinking about long-term, population-level benefits, targeting young people may be a way to help reduce epilepsy-related stigma for decades to come.
This randomized controlled trial (RCT) tested two new experimental communication approaches that targeted epilepsy stigma vs. a knowledge-alone approach. We hypothesized that 1.) Viewers of the experimental and control videos would have similar levels of epilepsy knowledge , 2) Viewers of a video that targets role competencies would have lower stigma on the corresponding domain of a standardized epilepsy stigma scale compared to viewers that watched a control video or video targeting social inclusion, and 3.) Viewers of a video that targets social inclusion would score lower on the corresponding stigma domain compared to viewers that watched a control video or a video targeting role competencies.
Methods:
Community Advisory Board (CAB):
Building upon prior work on epilepsy stigma with funding from the Centers for Disease Control and Prevention (CDC), we developed two novel health communication strategies intended to reduce epilepsy stigma among young people, ages 18–29.3; 12; 13 A local CAB representing people with epilepsy, epilepsy caregivers and providers, and members of the Epilepsy Association of Cleveland provided critical input and oversight to this project. The study team agreed upon two distinct messaging themes that would target and elicit a positive emotional response and hopefully lead to favorable attitudes. The first theme, operationalized in the video entitled, “Different – Just Like You,” focused on the competence of a person with epilepsy in fulfilling typical life roles such as staying physically healthy or working. The second theme, “Be Fearless, Be a Friend,” focused on social inclusion, and included a scenario of four young friends interacting. When two of the friends mock a person having a seizure, the friend with epilepsy withdraws from her social circle.
The CAB included two young adults with epilepsy, three young adults without epilepsy, one young adult family member of a person with epilepsy, one epilepsy care clinician, one older person with epilepsy, and one representative from the Case Western Reserve University (CWRU) Prevention Research Center Network of Community Advisors (NOCA). The NOCA is a community group which provides guidance to CWRU researchers conducting public health research in local neighborhoods. Five of the CAB members were white, three African-American, and one “other” ethnicity. The CAB identified top “key messages” to communicate to the general public about epilepsy. As a frame of reference, the study team shared the Institute of Medicine’s Key Messages about Epilepsy14 with the CAB. The CAB key messages were: 1.) Epilepsy is common; 2.) There are simple guidelines on what to do when witnessing a seizure; 3.) There are different types of seizures in addition to the generalized convulsions often portrayed in the media; and 4.) People with epilepsy should be treated like “normal” people rather than being protected or avoided. This last message emphasizes the competency of people with epilepsy as well as the need for social inclusion.
Additional CAB recommendations included the need to be brief, readily accessible, use platforms widely used by young people (YouTube, social media), be credible, be relatable, and emphasize the normality of people with epilepsy. Additionally, the CAB recommended recognizing the abilities of many successful, happy, and independent people with epilepsy.
Video Development:
Regarding video development, we refined the messages developed with CAB input, then brainstormed a variety of story ideas, keeping in mind video format, story elements, and communication scripting. Six ideas were developed into storyboards, using the free online comic strip creator platform Pixton (https://pixton.com). Through iterative review, scoring on a number of key dimensions, and consensus-goal discussion, four story ideas were retained. The CAB provided feedback via online survey using Survey Monkey. Preferences leaned toward a single person narrative, and the team derived two final experimental videos. An in-house university-based media production source assisted with video editing.
Recruitment of non-professional actors using Institutional Review Board (IRB)-approved advertising targeted local university/college campuses, other community locations, and a northeast Ohio actor and theatre list. To address representativeness and inclusion, we specifically recruited and hired 3 actors with epilepsy. The same cast performed in both videos to focus the differences on video content rather than the actual actors. Video duration was 281 seconds for the “Different Just Like You” (role competency) video, 418 seconds for the “Be Fearless, Be a Friend” (social inclusion) video, and 93 seconds for the control video (e.g., PowerPoint presentation describing the key epilepsy messages). The “Different Just Like You” video is a narrated monologue providing a glimpse into the daily life of a successful young adult with epilepsy (https://youtu.be/G21vZ35yPFk). The “Be Fearless, Be a Friend” video presents dialogue between a group of young friends and emphasizes how stigmatizing words and behaviors hurt a person with epilepsy (http://youtu.be/vdg1zoZsbRM).
For study recruitment, study flyers and postings referenced a short, custom URL that redirected participants to the informed consent document, videos, and surveys. Participants were informed that they would be eligible to receive a U.S. $5 gift card electronically delivered to their email. Those who provided consent completed a brief pre-video survey of demographics (age, gender, ethnicity, race, educational attainment), and experience with epilepsy (personal experience with epilepsy and people with epilepsy). The following assessments were conducted post-video viewing:
Measures:
Acceptability, Usefulness and Perceived Attitudinal Change:
Survey respondents answered a short series of questions on perceived attitudinal impact of the videos, perceived usefulness of videos and perceived acceptability of the videos. This assessment was adapted from an existing video evaluation used in a large multinational study of social media and participatory video.15 Survey respondents also rated how well they understood the provided information, and their likelihood of recommending the site to others as used in a virtual community study by Cheung and Lee.16
The Attitudes and Beliefs about Living with Epilepsy (ABLE) Scale:
The ABLE scale, developed by the CDC17; 18 examines epilepsy stigma in the general public. Four sub-scales address Negative Stereotypes (7 questions), Risk and Safety Concerns (3 items), Work and Social Role Expectations (8 items) and Fear and Social Avoidance (7 items). DiIorio et al. 19 demonstrated validity via hypothesized (a-priori) known groups-testing; associations with epilepsy knowledge; construct validity with scale subdomains; and test-retest reliability. Scale reliability scores (Cronbach’s alpha ≥ 0.7) and test rest-reliability were both acceptable (alpha= 0.6). The ABLE scale subdomains were later found to be valid and reliable (alpha =0.8)6; 17 by confirmatory factory analysis in two independent population-based samples. ABLE items are scored by subscale and overall, where higher scores reflect more negative attitudes.
The Epilepsy Knowledge Questionnaire (EKQ)20–22:
The EKQ measures knowledge of the medical and social aspects of epilepsy. The scale has acceptable measures of internal reliability for medical knowledge (α= 0.62) and social knowledge (α=0.49). The EKG items20; 21 are added to create a total score where higher scores reflect for knowledge. For this study we selected a subset of 8 medical aspect items relevant to our key messages (Table 1).
Table 1:
Subset of Epilepsy Knowledge Profile Questions
| 1. Epilepsy is not infectious |
| 2. Epilepsy is a symptom of mental illness |
| 3. All people with epilepsy have similar symptoms |
| 4. All people with epilepsy lose consciousness during seizures |
| 5. Some seizures may last for a matter of seconds and not be noticed by others |
| 6. For most people, doctors can effectively treat epilepsy with drugs |
| 7. All those who start drugs for their epilepsy have to take them for life |
| 8. Most people’s seizures are well controlled soon after starting regular drug treatment |
Recruitment:
Recruitment of 18–29 year olds was initiated at local university and community college campuses, as well as community locations such as coffee houses, CD/game exchange locations, and libraries, using IRB-approved flyers. While there was no study-specific cultural focus, to help insure diverse inclusion, an email message was sent to a list of African-American college students through the Case Western Reserve University’s office of Multi-Cultural Affairs. To optimize generalizability to future research in the local community, in-person and print-advertising recruitment was conducted exclusively until we reached approximately 40% of our sample, when we began online recruiting. Online recruitment postings were made on social media and news aggregation sites (e.g. Reddit, Buzzfeed). The remainder of the sample was obtained after approximately 30 hours of online recruitment efforts.
Survey Methods:
Data collection was conducted online using REDCap (Research Electronic Data Capture), a secure, web-based application designed to support data capture for research studies.23 Participants who entered the custom URL were redirected to REDCap site where they answered screening questions, affirming they were between the ages of 18 and 29, resided in the U.S. and indicated informed consent. Respondents then provided self-report demographic data and information on their personal epilepsy experience. Several brief validation questions were included (e.g. “Please complete the following series”) to minimize fraudulent responses by anyone using computer programs or algorithms to mass-complete surveys. A computerized system integrated into the web-based form assigned random allocation (one of the 2 experimental videos or the control) in a 1:1:1 ratio. Following randomization, participants viewed the assigned video. After affirming that they viewed the video, participants completed the post-video assessments.
Data analysis:
We compared subject-level variables by group with Kruskal-Wallis, Mann-Whitney or Chi-squared tests. Nonparametric tests were adopted due to their general applicability, and the potential for non-normality with some of the variables being compared. We grouped responses from the two experimental videos and performed a comparison of control vs. experimental videos to determine experimental health communications vs. knowledge. We also compared the two experimental videos to each other on ABLE sub-scales to assess the social inclusion vs. role competency emphasis approaches.
Given the proof-of-concept nature of this study, we conducted several additional post-hoc analyses to guide future research. Based on associations reported in the literature, we conducted sub-group analyses to evaluate potential differences by gender, age, education and ethnicity on epilepsy knowledge and stigma. To adjust for any impact of previous personal knowledge of epilepsy, we also assessed whether knowing someone with epilepsy vs. not knowing anyone with epilepsy was associated with different levels of epilepsy knowledge and stigmatizing attitudes.
Results:
Overall sample description:
As noted in Figure 1, of 394 individuals who agreed to online participation, 390 completed the screening and eligibility questions, 305 were randomized to experimental videos or control, and 300 affirmed that they viewed the videos. Five cases were removed for failing the validation questions. The remaining 295 cases comprised the analytic sample, with a mean age of 23.1 (SD 3.3) years, 59.0% male, and 71.4% white. Over half of respondents were college graduates. Regarding epilepsy experience, 7.8% of respondents had epilepsy, 48.2% had a family member, friend or acquaintance with epilepsy, and 49.2% did not know anyone with epilepsy (multiple answers could be selected). Baseline characteristics were similar between the three arms (Table 2) with only one relatively small gender difference (slightly more women viewed the control video).
Figure 1:
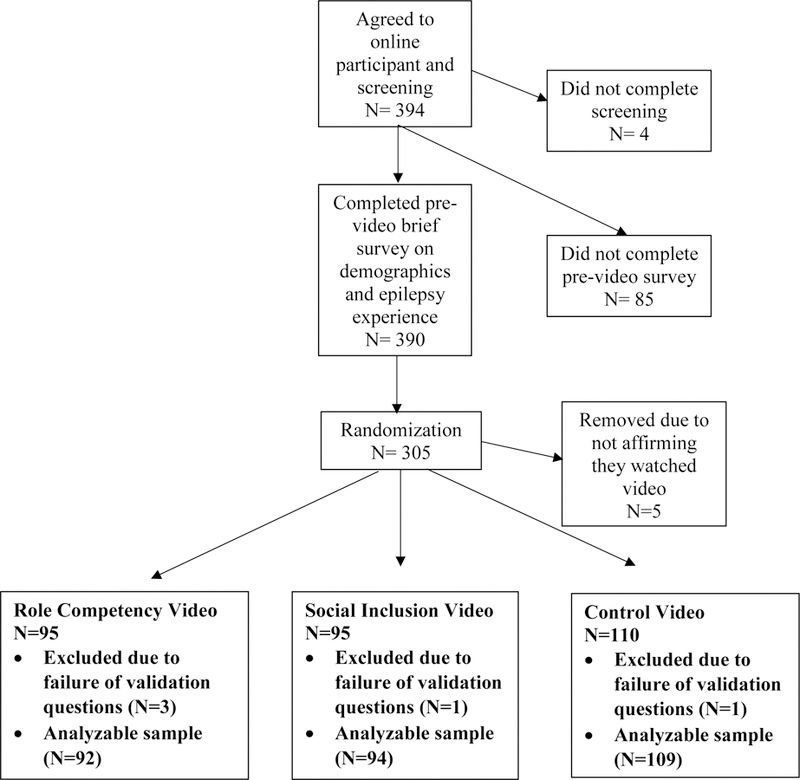
CONSORT Diagram of Study Flow
Table 2:
Baseline demographics of on-line survey respondents participating in a prospective, randomized controlled trial on epilepsy stigma communication
| Variable | All survey respondents N= 295 |
Social Inclusion Video n = 94 |
Role Competency Video n= 92 |
Control Video n= 109 |
Statistic |
|---|---|---|---|---|---|
|
Age in years – Mean (SD) |
23.10 (3.27) | 23.13 (3.37) | 23.10 (3.32) | 23.08 (3.17) | .971 (Kruskal Wallis Test) |
|
Gender – n (%) -Male -Female |
174 (59.0) 121 (41.0) |
60 (63.8) 34 (36.2) |
60 (65.2) 32 (34.8) |
54 (49.5) 55 (50.5) |
.041 (Chi-Square) |
|
Race – n (%) -White -African-American -Asian -Multiracial |
197 (71.4) 37 (13.4) 30 (10.9) 12 (4.3) |
64 (71.9) 11 (12.4) 7 (7.9) 7 (7.9) |
58 (68.2) 14 (16.5) 11 (12.9) 2 (2.4) |
75 (73.5) 12 (11.8) 12 (11.8) 3 (2.9) |
.425 (Chi-Square) |
|
Ethnicity – n (%) -Hispanic -Non-Hispanic |
41 (14.1) 249 (85.9) |
18 (19.8) 73 (80.2) |
9 (9.9) 82 (90.1) |
14 (13.0) 94 (87.0) |
.145 (Chi-Square) |
|
Education – n (%) -Grade 12 (High School Graduate) -Some College / Technical School - College Graduate |
38 (13.1) 92 (31.7) 160 (55.2) |
12 (13.0) 32 (34.8) 48 (52.2) |
9 (10.0) 31 (34.4) 50 (55.6) |
17 (15.7) 29 (26.9) 62 (57.4) |
.596 (Chi-Square) |
|
Epilepsy Experience – n (%) - Does not know anyone with epilepsy -Has epilepsy -Friend or acquaintance with epilepsy -Family member with epilepsy |
145 (49.2) 23 (7.8) 122 (41.4) 20 (6.8) |
45 (47.9) 12 (12.8) 38 (40.4) 8 (8.4) |
47 (51.1) 6 (6.5) 38 (41.3) 5 (5.4) |
53 (48.6) 5 (4.6) 46 (42.2) 7 (6.4) |
.946a (Chi-Square) |
: The categorical variables of epilepsy experience are collapsed into two subgroups: Does not know anyone with epilepsy, and knows someone with epilepsy including self, friend/acquaintance or family member with epilepsy.
Participant responses on video impact on epilepsy attitudes, perceived acceptability and usefulness:
Mean video time watched was 306 (SD= 77.7), 218 (67.4) and 81 (14.2) seconds for the social inclusion, role competency and control videos respectively. Median viewing times were similar at 304, 234, and 87 seconds for the social inclusion, role competency and control videos. Average proportion of time watched was 73.3%, 77.6%, and 87.1% for the social inclusion, role competency and control videos respectively. For the social inclusion video, 84.3% watched at least 50% of the video while only 32.9% watched at least 75% of the video. For the role competency video, these proportions were 90.1% and 73.2% respectively, while for the control video these were 98.6% and 75.7% respectively. The survey program did not permit being able to link a respondent’s viewing time to their survey responses.
As noted in Figure 2a, nearly all respondents (>90%) rated the videos as understandable. The majority also felt videos impacted their attitudes towards people with epilepsy and were memorable (Figures 2b and 2c). Approximately half of survey respondents stated they would share the videos on their social networking sites. Approximately two-thirds to three-quarters of respondents endorsed having pre-existing beliefs about epilepsy prior to watching the videos. The majority felt the videos made them aware of their own personal beliefs about epilepsy.
Figure 2a:

Perceived effects of videos on epilepsy attitudes
Figure 2b:

Perceived effects of videos on epilepsy usefulness
Figure 2c:
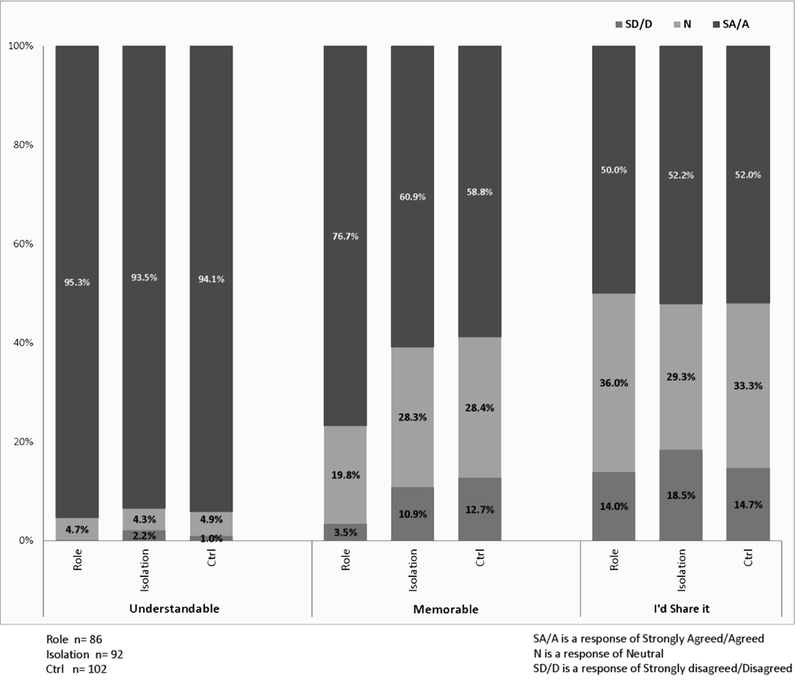
Perceived effects of videos on epilepsy acceptability
Since the specific questions on which videos most impacted attitudes about epilepsy and attitudes toward people with epilepsy mapped onto our original hypotheses, descriptive comparisons (Chi-square analysis) for these two questions were conducted. Because of small cell size, the neutral and disagree/strongly disagree cells were combined. The proportion of respondents who agreed the videos changed their attitudes about epilepsy were slightly but significantly higher in the role competency and control videos compared to the social inclusion video (p=.021). There was a similar trend for respondents to more often agree that their attitudes towards people with epilepsy were changed by the role competency and control videos compared to the social inclusion video (p=.061)
Epilepsy knowledge and stigma:
Table 3 illustrates EKQ and ABLE means and standard deviations in the three video groups. There was a trend for the two experimental videos to be associated with higher knowledge compared to control (Kruskal-Wallis p-value = 0.058). While all except one of the ABLE sub-scale scores were numerically higher (more stigmatizing attitudes) for the control video vs the experimental videos, none was statistically different. There was also no difference on ABLE sub-scale scores between the two experimental videos in role competency or social avoidance domains. The spearman’s rho correlation between the composite ABLE and the EKQ is −.340 (p <.001) indicating that higher knowledge is associated with less stigmatizing attitudes.
Table 3:
Epilepsy knowledge and stigma scores after viewing a brief video on epilepsy stigma communication
| Variable | Social Inclusion Video n = 94 |
Role Competency Video n= 92 |
Control n= 109 |
Statistic (Kruskal Wallis Test) |
|---|---|---|---|---|
| ABLE– Mean (SD) | ||||
|
-Negative Stereotypes |
2.51 (1.35) |
2.71 (2.08) |
2.88 (2.35) |
p=.873 |
|
-Risk and Safety Concerns |
3.33 (0.74) |
3.61 (3.52) |
3.67 (3.16) |
p=.442 |
|
-Work and Social Role Expectations |
3.85 (0.43) |
4.10 (1.88) |
3.92 (1.28) |
p=.351 |
|
-Fear and Social Avoidance |
2.63 (1.26) |
3.18 (2.59) |
3.21 (2.66) |
p=.537 |
|
Composite Score* |
3.08 (0.79) |
3.40 (1.60) |
3.42 (1.75) |
p=.568 |
|
Epilepsy Knowledge Questionnaire – Mean (SD) |
6.25 (1.70) |
6.33 (1.66) |
6.01 (1.76) |
p=.457 |
ABLE: Attitudes and Beliefs about Living with Epilepsy. Higher scores indicate more stigmatizing attitudes
: Average of 4 ABLE sub-scale scores
EKQ: Epilepsy Knowledge Questionnaire. Higher scores indicate more knowledge
Post-hoc analyses association of epilepsy knowledge and attitudes based on age, gender, ethnicity and prior personal acquaintance with a person with epilepsy:
We conducted a selected set of post-hoc analysis with a focus on sub-groups where stigma may be particularly relevant, specifically individuals with less education, men, younger individuals, minorities, and those who without personal familiarity with epilepsy.3 Overall, age was negatively correlated with epilepsy knowledge (younger people had less knowledge, Spearman correlation −.231, p<.01) and positively correlated with stigma levels (younger people had more stigmatizing attitudes, Spearman correlation .522, p<.01).Women had lower levels of stigma compared to men when videos were assessed separately (p<.01), but in the combined sample there were no gender differences in epilepsy knowledge. Individuals who knew someone with epilepsy had more stigmatizing attitudes (p<.01) and a trend for less epilepsy knowledge (p=.079) compared to those who did not know someone with epilepsy. Respondents who self-identified as white had higher stigmatizing attitudes and lower knowledge compared to individuals of other ethnicities (p <.01 for both). Higher levels of education were associated with higher levels of knowledge (p<.01), but no difference in stigma.
We also compared EKQ and ABLE scores in women vs. men. For all three videos, men had higher stigma scores than women (p<.001). Knowledge scores between men and women were comparable for the role competency (p=.20) and social inclusion videos (p=.81), but in the control video knowledge was lower for men compared to women (p<.05).
Open-ended comments:
There were 59 individuals who provided optional comments. Most comments were on the social inclusion video (N=21), with fewer comments for the role competency (n=16) and control (N=15) videos. Comments were mainly positive (70%) and indicated many respondents did not know much about epilepsy prior to video viewing. Furthermore, respondents reported the social inclusion and competency videos were informative. One respondent noted, “To be honest, I had never heard of epilepsy before. This video makes me want to go learn more”. The control video had the largest proportion of negative comments, and some respondents did not find it engaging or memorable, “It was just a PowerPoint presentation which I see hundreds of times in a classroom and will likely forget”.
Discussion:
To our knowledge, this is a first RCT testing novel health communication strategies intended to reduce epilepsy stigma. The nature and presentation of epilepsy stigma has been widely documented, 3; 24 but evidence-based approaches to reduce epilepsy stigma are limited. Additional novel features of this RCT is that it targeted young people between the ages of 18–29, used stigma-reduction interventions that were informed by a systematic review of the epilepsy stigma literature,3 considered health communication concepts, and was informed by input from a CAB consisting of key stakeholders that included people with epilepsy, family members and a health professional with expertise in epilepsy. Study findings regarding the association of video format as it relates to epilepsy knowledge and stigma are somewhat mixed. We found a trend for epilepsy knowledge to be higher in the experimental video groups vs. the control, but the videos did not appear to differ in their association with composite levels of stigma or on stigma sub-domains using a standardized measure.
Several pragmatic points with respect to this pilot study are worth mention. First, given budget limitations, video production was not of the caliber that might be expected in commercial media programs, and we did not employ full-time professional actors. Second, the average viewer did not view the videos in their entirety, and the proportion of individuals who continued to watch each video decreased over time. Only a third of individuals assigned to the longest video (social inclusion ~7 minutes) viewed at least 75% of the video. This may have limited the potential impact of the experimental communications and suggests that videos used in future research need to be very brief (no more than 4–5 minutes). Omission of a baseline assessment of attitudes also limited the ability to examine changes within individuals. It’s possible that despite randomization, study participants in all three groups who self-selected to participate in the study, had more pro-social attitudes biasing study outcomes. Additionally, this was a relatively well-educated sample, perhaps not surprising given the recruitment methods and web-based format. Additional assessment of the videos’ impact with more diverse study participants is warranted.
All videos performed relatively well, with 60–74% of respondents agreeing that the videos had an impact on their perceived attitudes towards people with epilepsy. Brief, online messages that educate and inform the general population about epilepsy seem that they can improve knowledge about epilepsy and may help to reduce epilepsy stigma. Some other reports have not found a clear association between disease knowledge and stigmatizing attitudes.25 In contrast to our expectations, survey respondents in this study felt that the role competency and control videos most strongly impacted their attitudes towards epilepsy and people with epilepsy compared to the social inclusion video. It is possible that the drop-off in video viewing time may have contributed to the slightly lower impact scores for the social inclusion video. It’s also possible that study participants, by virtue of their age, were biased toward social inclusive attitudes as many came of age when the American with Disabilities Act was already implemented, and attitudes toward social inclusiveness toward people with disabilities have significantly improved.26; 27
Also in contrast to our original hypothesis, there were no differences in composite stigma or stigma sub-scales across the 3 videos. Because findings on the ABLE scale did not consistently mirror self-reported perceived video impact on epilepsy attitudes, it is possible that the ABLE scale may not capture small or short-term differences in epilepsy attitudes that viewers might experience with seeing a single brief video. Alternatively, it is possible that asking individuals to report on their attitudes generally vs. assessing attitudes with the ABLE questionnaire may measure somewhat different constructs. Finally, perhaps the video messages didn’t resonate with the target group, despite CAB input.
Post-hoc analyses revealed some unexpected differences within the sample. In particular, whites and those who knew someone with epilepsy appeared to have the most stigmatizing attitudes. These patterns need to be explored in future studies of misconceptions surrounding epilepsy. Men and women had similar levels of knowledge in the two experimental videos, but men had less knowledge in the control video group. Stigmatizing attitudes were more common in men compared to women in all three videos. However, given the study limitations, repeating assessments with larger and more diverse populations is warranted to determine whether post-hoc findings are robust or due to chance.
There are a number of limitations to this study including a lack of pre-post evaluations, a relatively small and homogeneous sample who self-selected to participate, pooling of individuals with differential personal experience with epilepsy, and the well-documented problems inherent in web-based surveys.28 While the ABLE is a well-validated tool to assess epilepsy stigma at the population level,6; 17 self-reported attitudes and stigma may be imperfectly aligned with real-world behaviors like social avoidance and job hiring. This study sample had a relatively high proportion with personal familiarity with epilepsy by either having epilepsy themselves or having a friend or family member with epilepsy. It seems likely that individuals with personal epilepsy experience would be biased in favor of participating in a study on epilepsy, and findings need to be interpreted in light of this consideration.
In conclusion, this prospective randomized controlled study utilized and tested novel health communication strategies to improve knowledge and attitudes about epilepsy and people with epilepsy. We employed a contemporary, web-based approach, which allowed rapid, efficient recruitment and completion of the study. While this is an initial effort and will require follow-up development, we have demonstrated the acceptability, feasibility and potential of novel communication strategies to target epilepsy stigma and a web-based system for assessing them.
Acknowledgments:
The authors would like to acknowledge the Centers for Disease Control and Prevention (CDC), the Department of Health and Human Services, and also the Clinical and Translational Science Collaborative (CTSC) for the funding support of this study.
Footnotes
Conflicts of Interest:
Author MS has received grant support from Alkermes, Janssen, Pfizer and Merck, royalties from Springer Press, Johns Hopkins University Press and Oxford Press, and served as consultant for Bracket, Otsuka, Sunovion, Supernus, Health Analytics and Neurocrine. Authors LKH, JRVD, CT, EW, ATP, AB, KN, and ATB have no relevant conflicts of interest to disclose.
Ethical statement:
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
References:
- 1.Institute of Medicine. Epilepsy across the spectrum: Promoting health and undesrtanding. In Committee on the public health dimensions of the epilepsies England MJ, Liverman CT, Schultz AM, et al. (Eds)The National Academies Press: Washington, DC; 2012. [PubMed] [Google Scholar]
- 2.Healthy people 2020, 2014. Available at: https://www.healthypeople.gov Accessed 1/24/17.
- 3.Herrmann LK, Welter E, Berg AT, et al. Epilepsy misconceptions and stigma reduction: Current status in western countries. Epilepsy & Behavior 2016;60:165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Price P, Kobau R, Buelow J, et al. Improving understanding, promoting social inclusion, and fostering empowerment related to epilepsy: Epilepsy foundation public awareness campaigns-2001 through 2013. Epilepsy & Behavior 2015;44:239–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buelow JM, Gattone P. The epilepsy foundation is the voice of people with epilepsy and their families. Epilepsy Behav 2015;47:72. [DOI] [PubMed] [Google Scholar]
- 6.Cui W, Kobau R, Zack MM, et al. Recent changes in attitudes of us adults toward people with epilepsy - results from the 2005 summerstyles and 2013 fallstyles surveys. Epilepsy Behav 2015;52:108–118. [DOI] [PubMed] [Google Scholar]
- 7.Corrigan PW. Best practices: Strategic stigma change (ssc): Five principles for social marketing campaigns to reduce stigma. Psychiatr Serv 2011;62:824–826. [DOI] [PubMed] [Google Scholar]
- 8.Lewandowsky S, Ecker UKH, Seifert CM, et al. Misinformation and its correction: Continued influence and successful debiasing. Psychological Science in the Public Interest 2012;13:106–131. [DOI] [PubMed] [Google Scholar]
- 9.Loewenstein G, Lerner JS. The role of affect in decision making Oxford University Press; 2003. [Google Scholar]
- 10.Lerner JS, Li Y, Valdesolo P, et al. Emotion and decision making. Annu Rev Psychol 2015;66:799–823. [DOI] [PubMed] [Google Scholar]
- 11.Lewandowsky S, Ecker UK, Seifert CM, et al. Misinformation and its correction: Continued influence and successful debiasing. Psychol Sci Public Interest 2012;13:106–131. [DOI] [PubMed] [Google Scholar]
- 12.Perzynski A RR, Cage J, Colon-Zimmermann K, Welter E, Sajatovic M. Barriers and facilitators to self-management among persons with epilepsy and mental illness. Chronic Illness 2016;October 19:1742395316674540. [Google Scholar]
- 13.Herrmann LK. Development of a technology-based health communication strategy to reduce epilepsy stigma among young adults. Annual Meeting of the American Public Health Association 2016;2 November Colorado Convention Center, Denver, CO: Oral Presentation. [Google Scholar]
- 14.Institute of Medicine. Committee on the public health dimensions of the epilepsies. Epilepsy across the spectrum. Promoting health and understanding The National Academies Press; Washington, DC; 2012. [PubMed] [Google Scholar]
- 15.Underwood C, Jabre B. Arab women speak out: Self-empowerment Sage: New Delhi; 2003. [Google Scholar]
- 16.Cheung CM, Lee MKO. Understanding the sustainability of a virtual community: Model development ad empirical test. Journal of Information Science 2009;35:279–298. [Google Scholar]
- 17.Kobau R, DiIorio CA, Anderson LA, et al. Further validation and reliability testing of the attitudes and beliefs about living with epilepsy (able) components of the CDC epilepsy program instrument on stigma. Epilepsy Behav 2006;8:552–559. [DOI] [PubMed] [Google Scholar]
- 18.DiIorio CA, Kobau R, Holden EW, et al. Developing a measure to assess attitudes toward epilepsy in the US population. Epilepsy & Behavior 2004;5:965–975. [DOI] [PubMed] [Google Scholar]
- 19.Diiorio CA, Kobau R, Holden EW, et al. Developing a measure to assess attitudes toward epilepsy in the us population. Epilepsy Behav 2004;5:965–975. [DOI] [PubMed] [Google Scholar]
- 20.Jarvie S, Espie CA, Brodie MJ. The development of a questionnaire to assess knowledge of epilepsy: 1--general knowledge of epilepsy. Seizure 1993;2:179–185. [DOI] [PubMed] [Google Scholar]
- 21.Jarvie S, Espie CA, Brodie MJ. The development of a questionnaire to assess knowledge of epilepsy: 2--knowledge of own condition. Seizure 1993;2:187–193. [DOI] [PubMed] [Google Scholar]
- 22.Doughty J, Baker Gus A, Jacoby A, et al. Cross-cultural differences in levels of knowledge about epilepsy. Epilepsia 2003;44:115–123. [DOI] [PubMed] [Google Scholar]
- 23.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (redcap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kate Collins TB, Camfield PR, Camfield CS, et al. People with epilepsy are often perceived as violent. Epilepsy Behav 2007;10:69–76. [DOI] [PubMed] [Google Scholar]
- 25.Chan SK, Lee KW, Hui CL, et al. Gender effect on public stigma changes towards psychosis in the hong kong chinese population: A comparison between population surveys of 2009 and 2014. Soc Psychiatry Psychiatr Epidemiol 2016. [DOI] [PubMed]
- 26.Siperstein G, Romano N, Mohler A, & Parker R. A national survey of consumer attitudes towards companies that hire people with disabilities. Journal of Vocational Rehabilitation 2006;24:3–9. [Google Scholar]
- 27.Goreczny A, Bender EE, Caruso G, & Feinstein CS. Attitudes towards individuals with disabilities: Results of a recent survey and implications of those results. Res Dev Disabil 2011;32:1596–1609. [DOI] [PubMed] [Google Scholar]
- 28.Wyatt JC. When to use web-based surveys. J Am Med Inform Assoc 2000;7:426–429. [DOI] [PMC free article] [PubMed] [Google Scholar]


