Abstract
Suspected urinary tract infection is a common indication for antimicrobial therapy in long-term care residents. We sought to characterize antimicrobial susceptibilities among urine isolates collected from women long-term care residents enrolled in a clinical trial across 21 long-term care facilities in Connecticut, United States of America between August 2012 and October 2015. Among 967 urine cultures collected from 175 women long-term care residents with and without suspected urinary tract infection, we identified 456 bacterial isolates. Escherichia coli (55.3%), Klebsiella (13.8%) and Enterococcus (8.3%) species were the predominant organisms identified. Among all 456 urine isolates, 68.1% were ciprofloxacin-susceptible, 77.2% were trimethoprim/sulfamethoxazole-susceptible, 86.3% were cefazolin-susceptible, and 72.6% were nitrofurantoin-susceptible. Among 252 Escherichia coli urine isolates, 60.2% were ciprofloxacin-susceptible, 73.7% were trimethoprim/ sulfamethoxazole-susceptible, 84.5% were cefazolin-susceptible, and 86.5% were nitrofurantoin-susceptible. These findings suggest that trimethoprim/sulfamethoxazole may be favorable empiric therapy while the urinary isolate is unknown, and nitrofurantoin may be optimal therapy for uncomplicated urinary tract infection due to Escherichia coli in women long-term care residents.
Keywords: Urinary Tract Infection, Long-Term Care Residents, Escherichia coli, Nitrofurantoin, Antibiotic Susceptibility
Background
Antimicrobial use among long-term care residents is common. The annual prevalence of antimicrobial use among long-term care residents ranges from 47–79% [1] and antimicrobial stewardship programs are needed in long-term care facilities in the United States [2]. The most common indication for antimicrobials among long-term care residents is urinary tract infection [3]. Data suggest that antimicrobial prescribing practices may impact antimicrobial susceptibility of uropathogens among long-term care residents in the Netherlands [4]. Among long-term care residents in Connecticut, we previously showed that Escherichia coli, Proteus, and Klebsiella species were the most common uropathogens identified in patients with suspected urinary tract infection from 2005–2007, and 40% and 93% of Escherichia coli isolates were fluoroquinolone-susceptible and nitrofurantoin- susceptible, respectively [5]. Our current study characterized antimicrobial susceptibilities among urine isolates from long-term care residents in the same region from 2012–2015.
Materials and Methods
We evaluated urine cultures collected from women long-term care residents enrolled in a clinical trial evaluating cranberry capsules to reduce bacteriuria plus pyuria across 21 facilities between August 2012 and October 2015 [6]. Participating facilities had at least 90 beds and were within a 50-mile radius of New Haven, CT. Residents were excluded if they were expected to be in the facility for ≤ 1 month, received suppressive antimicrobials, had an indwelling bladder catheter or prior nephrolithiasis, or were undergoing dialysis. Further enrollment criteria have been reported previously [6]. The Yale Human Investigation Committee approved this study. All nursing home administrators signed letters of participation and signed consent was obtained from participants or their surrogates.
Urine cultures were collected during screening encounters of the clinical trial and during adverse events representing suspected urinary tract infection. Screening urine specimens were obtained by clean catch whereas adverse event urine specimens may have also been obtained by catheterization. All specimens were processed at Yale New Haven Health per hospital microbiology laboratory protocols. Antimicrobial susceptibilities were determined per Clinical and Laboratory Standards Institute M100, Performance Standards for Antimicrobial Susceptibility Testing.
For all cultures, we assessed the number of colony-forming units (cfu) of bacteria per milliliter (ml) and type of organism identified. Isolates with <1,000 cfu/ml were not speciated per laboratory protocol. Cultures with growth of up to two organisms were included in analyses. Cultures with no growth, mixed flora (three or more organisms) or unspecified growth were excluded. Antimicrobial susceptibilities were assessed across all remaining cultures. We recorded demographics, comorbidities, number of urinary tract infections, and antimicrobial courses in the prior year for all residents. Analyses were conducted using SAS, version 9.4.
Results
Overall, we evaluated 967 urine cultures from 175 women long-term care residents collected from 723 screening encounters and 244 adverse event encounters. Among residents, median age was 87 years (range, 65–101 years). Most (90.3%, N=158) were white, 78.9% (N=138) had dementia, 30.9% (N=54) had bladder incontinence, 26.3% (N=46) had diabetes, and 21.7% (N=38) had renal disease. In the prior year, 31.4% (N=55) had ≥1 and urinary tract infection, and 29.7% (N=52) received ≥2 antimicrobial courses.
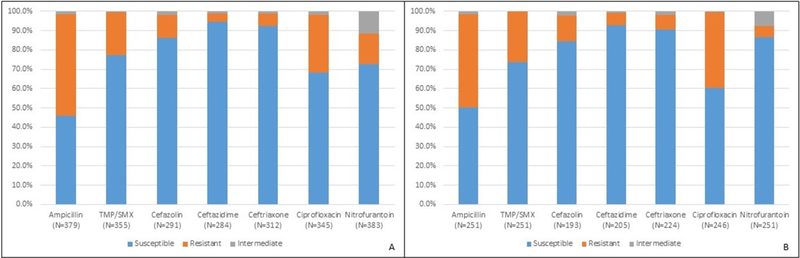
Among 967 urine cultures, 456 isolates were identified (Table 1). The most common organisms were Escherichia coli (55.3%), Klebsiella species (13.8%), and Enterococcus species (8.3%). Figure 1 shows antimicrobial susceptibilities for all cultures and the subset with Escherichia coli. Among all urine isolates, 68.1% were ciprofloxacin-susceptible, 77.2% were trimethoprim/ sulfamethoxazole-susceptible, 86.3% were cefazolin- susceptible, and 72.6% were nitrofurantoin-susceptible. Among Escherichia coli isolates, 60.2% were ciprofloxacin- susceptible, 73.7% were trimethoprim/sulfamethoxazole- susceptible, 84.5% were cefazolin-susceptible, and 86.5% were nitrofurantoin-susceptible. Antimicrobial susceptibilities were similar regardless of whether urine cultures were obtained for clinical trial screening purposes or for suspected urinary tract infection.
Table 1:
Distribution of organisms identified from 456 urine bacterial isolates collected from women long-term care residents
| Organism | N | % |
|---|---|---|
| Escherichia coli | 252 | 55.3 |
| Klebsiella species | 63 | 13.8 |
| Enterococcus species | 38 | 8.3 |
| Proteus species | 26 | 5.7 |
| Group B Streptococcus | 19 | 4.2 |
| Aerococcus species | 14 | 3.1 |
| Lactobacillus | 9 | 2.0 |
| Coagulase negative Staphylococcus | 9 | 2.0 |
| Streptococcus, viridans group | 7 | 1.5 |
| Corynebacterium | 4 | 0.9 |
| Enterobacter species | 4 | 0.9 |
| Pseudomonas aeruginosa | 3 | 0.7 |
| Providencia stuartii | 2 | 0.4 |
| Candida albicans | 2 | 0.4 |
| Group D. Streptococcus | 2 | 0.4 |
| Staphylococcus aureus | 1 | 0.2 |
| Gemella species | 1 | 0.2 |
Figure 1:
Antimicrobial susceptibilities of bacterial isolates from August 2012 to October 2015. A total of 456 bacterial isolates were identified from 175 women long-term care residents during encounters with and without suspected urinary tract infection. Susceptibility patterns of all bacterial isolates (A) and the subset with Escherichia coli (B) are shown. The number of bacterial isolates associated with each tested antimicrobial is noted at the bottom of each bar. The total number of bacterial isolates and the subset with Escherichia coli is less than 456 because some isolates were not tested against each antimicrobial.
Discussion
Our study suggests change in the microbiology and antimicrobial susceptibility of urinary isolates among women long-term care residents compared to prior data from the same region [5]. While Escherichia coli remains the dominant organism, the relative proportion of Enterococcus species has increased (8.3% versus 4.5%) whereas Proteus (5.7% versus 14.6%) and Providencia (0.4% versus 3.7%) have decreased. Additionally, Escherichia coli fluoroquinolone-susceptibility increased during our study period which coincided with the Food and Drug Administration restricting fluoroquinolone use for uncomplicated urinary tract infection in 2015 [7]. These results have implications for empiric antimicrobial therapy for suspected urinary tract infection in women long-term care residents and the potential role of public policy in reducing antimicrobial resistance.
Although trimethoprim/sulfamethoxazole and cephalexin are often used as empiric therapy for uncomplicated urinary tract infection, trimethoprim/sulfamethoxazole-susceptibility and cefazolin-susceptibility was 77.2% and 86.3% across all isolates and 73.7% and 84.5% in Escherichia coli isolates, respectively. In contrast, nitrofurantoin had the most consistent susceptibility among Escherichia coli with 86.5% susceptibility. This susceptibility to nitrofurantoin appears stable when compared to prior urine Escherichia coli data from 2002–2005. While 21.7% of participants had renal disease in our study, nitrofurantoin achieves satisfactory cure rates and remains well-tolerated for urinary tract infection in patients with an estimated glomerular filtration rate of 50 ml/min or less [8]. Collectively, these data support recent findings from a multinational randomized clinical trial in women [9] and indicate empiric nitrofurantoin use may be preferred for uncomplicated Escherichia coli urinary tract infection in long-term care residents [10].
The regional increase in Escherichia coli fluoroquinolone- susceptibility from 40% in 2005–2007 to 60.2% in our study may reflect evolving prescribing practices. Although we could not evaluate prescription or antimicrobial stewardship data for this cohort, evidence suggests that hospital antimicrobial stewardship programs can reduce fluoroquinolone-resistance in local unaffiliated long-term care facilities [2]. Thus, restricted fluoroquinolone use may have impacted antimicrobial susceptibility patterns in participating facilities.
The main study strength is that we evaluated all organisms and antimicrobial susceptibilities from urine cultures collected from encounters with and without suspected urinary tract infection in women long-term care residents lacking indwelling catheters. Our results may lack generalizability to men, which constituted 16% of our prior study population, or catheterized patients. Nevertheless, the majority of long-term care residents are women, and the microbiology and management of catheter- associated versus non-catheter-associated urinary tract infection differ.
In conclusion, our work suggests a temporal increase in fluoroquinolone-susceptibility and preservation of nitrofurantoin-susceptibility among Escherichia coli urine isolates in women long-term care residents throughout Connecticut. Given susceptibility rates of all uropathogens to trimethoprim/sulfamethoxazole and cephalexin, they remain effective empiric treatment agents for uncomplicated urinary tract infection when the urinary pathogen is unknown. However, given the predominance of Escherichia coli, its preserved susceptibility to nitrofurantoin, and the safety of short-course nitrofurantoin for patients with a reduced glomerular filtration rate, nitrofurantoin deserves further consideration as empiric therapy in this population. Consistent with recent findings from a randomized clinical trial evaluating nitrofurantoin use for uncomplicated urinary tract infection in community women, future research should evaluate nitrofurantoin as empiric therapy for suspected uncomplicated urinary tract infection among women long-term care residents.
Acknowledgement
We thank participating long-term care facilities for their support of this study. This work was supported by 2T32AI007517–16 at the Yale School of Medicine, Section of Infectious Diseases and grants P30 AG021342 Claude D. Pepper Older Americans Independence Center, R01 AG041153, and K07 AG030093 all from the National Institute on Aging, National Institutes of Health. The authors declare that there is no conflict of interest.
References
- 1.Van Buul LW, Van der Steen JT, Veenhuizen RB, Achterberg WP, Schellevis FG, et al. (2012) Antibiotic Use and Resistance in Long Term Care Facilities. J Am Med Dir Assoc 13(6): 561–568. [DOI] [PubMed] [Google Scholar]
- 2.Rahme CLJH, Avery LM (2016) Impact of a hospital’s antibiotic stewardship team on fluoroquinolone use at a long-term care facility. Annals of Long-Term Care: Clinical Care and Aging 24(6): 13–20. [Google Scholar]
- 3.Benoit SR, Nsa W, Richards CL, Bratzler DW, Shefer AM, et al. (2008) Factors associated with antimicrobial use in nursing homes: a multilevel model. J Am Geriatr Soc 56(11): 2039–2044. [DOI] [PubMed] [Google Scholar]
- 4.Vromen M, Van der Ven AJAM, Knols A, Stobberingh MEE (1999) Antimicrobial resistance patterns in urinary isolates from nursing home residents. Fifteen years of data reviewed. J Antimicrob Chemother 44(1): 113–116. [DOI] [PubMed] [Google Scholar]
- 5.Das R, Perrelli E, Towle V, Van Ness PH, Juthani Mehta M (2009) Antimicrobial Susceptibility of Bacteria Isolated from Urine Samples Obtained from Nursing Home Residents. Infect Control Hosp Epidemiol 30(11): 1116–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juthani Mehta M, Van Ness PH, Bianco L (2016) Effect of cranberry capsules on bacteriuria plus pyuria among older women in nursing homes: A randomized clinical trial. JAMA 316(18): 1879–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.FDA (2015) FDA Briefing Document Joint Meeting of the Antimicrobial Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee.
- 8.Bains A, Buna D, Hoag NA (2009) A Retrospective Review Assessing the Efficacy and Safety of Nitrofurantoin in Renal Impairment. Canadian Pharmacists Journal/Revue des Pharmaciens du Canada 142(5): 248–252. [Google Scholar]
- 9.Huttner A, Kowalczyk A, Turjeman A, Babich T, Brossier C, et al. (2018) Effect of 5-Day Nitrofurantoin vs Single-Dose Fosfomycin on Clinical Resolution of Uncomplicated Lower Urinary Tract Infection in Women: A Randomized Clinical Trial. JAMA 319(17): 1781–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Datta R, Juthani Mehta M (2018) Nitrofurantoin vs fosfomycin: Rendering a verdict in a trial of acute uncomplicated cystitis. JAMA 319(17): 1771–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]