Abstract
Background/aims
Platelet-rich plasma (PRP) injections are used in sports medicine and have been the subject of increased clinical interest. However, there have been very few reports of the composition of initial whole blood and the final PRP product. The objective of this study was to provide technical tools to perform a correct characterisation of platelets, leucocytes and red blood cells (RBCs) from whole blood and PRP.
Methods
Blood and PRP were obtained from 26 healthy volunteers and prepared according to the varying parameters encountered within PRP process preparation and quantification (harvesting method, anticoagulant used, sampling method, counting method). Concentrations were measured at t=0, t=1, t=6 and t=24 hours.
Results
Sampling of blood in Eppendorf tubes significantly decreased platelet concentration over time, whereas sampling in Microvette EDTA-coated tube kept platelet concentration stable until 24 hours. A non-significant difference was observed in platelet counts in PRP with impedance (median (IQR): 521.8 G/L (505.3–524.7)) and fluorescence (591.5 G/L (581.5–595.8)) methods. Other studied parameters did not influence platelet concentrations in blood or PRP samples. Leucocytes and RBC counts were similar whatever the anticoagulant, sampling, harvesting and counting methods used for both blood and PRP samples.
Conclusions
Systematic sampling of blood and PRP in EDTA-coated tubes for quality control is recommended. The use of a validated counter for PRP sample should also be taken into account.
Keywords: platelet-rich plasma, regenerative medicine, quality control
What are the new findings.
Sampling of blood and PRP in microvette EDTA tubes raises to stable concentration over 24 hours, no matter the conditions of harvesting or preparation.
Counting technique influences platelet counts in platelet-rich plasma (PRP).
Validated counters for PRP sample should be taken into account for quality control of PRP in regenerative medicine.
Introduction
Platelet-rich plasma (PRP) is an autologous plasma suspension of platelets, characterised by a higher platelet concentration than in physiological blood.1 In brief, activated platelets release growth factors (GFs) implied in reparative and regenerative processes. High levels of platelet-derived growth factors, transforming growth factor β1, vascular endothelial growth factor, epidermal growth factor, insulin-like growth factor 1 or fibroblast growth factor found in PRP are especially known to play critical role in cell proliferation, chemotaxis, cell differentiation and angiogenesis.2 Described as an easy, fast and safe (because of its autologous origin) product, PRP is becoming more popular and has been the subject of increased clinical interest in the orthopaedic and aesthetic fields.3 However, one of the main weaknesses of the related studies is the lack of a precise biological characterisation of the content of the PRP injected. Recently, Chahla et al reported in a large review that only 17 from 105 studies using PRP in orthopaedic conditions provided quantitative metrics on the composition of the final PRP product.4 However, substantial biological differences exist in the content in platelets, red blood cells (RBCs) and leucocytes produced by the various automated and manual protocols.5 Recent conclusions from a think tank on biological treatments for sports injuries stated that more high-level studies were needed with a consistent attention to the specific components in each study’s PRP preparation.6
Taken together, these elements strongly encourage the introduction of systematic quality control including a precise quantification of platelets, RBCs and leucocytes concentrations in both whole blood and PRP. However, it does exist a large variety of blood harvesting methods (tube or syringe with either anticoagulant citrate dextrose (ACD-A) solution or sodium citrate) and PRP preparation that could influence the results of a complete cell count. The latter is also a source of variation as it can be performed using impedance or fluorescence techniques with different counters and algorithms for platelets’ quantification.
The objective of this study was to provide technical tools to perform a correct characterisation of whole blood and PRP taking into account the varying parameters encountered within PRP process preparation and quantification (harvesting method, anticoagulant used, sampling method, counting method).
Materials and methods
Participant recruitment
Twenty-six healthy volunteers who gave their informed consent were included in the study from June to November 2017. They were free of any medication known to affect platelet functions for 7 days before the study. All donors included in this study had platelet numbers over 150 G/L.
Whole blood collection
A single technician collected a maximum of 56 mL of blood by venipuncture using a 21-gauge needle (BD Vacutainer Safety-Lok Blood Collection Set, Becton Dickinson and Co., Franklin Lakes, New Jersey, USA) connected with a three-way stopcock (reference RO301M;Cair LGL, Civrieux-d’Azergues, France) filling two syringes (containing 18 mL of whole blood and 2 mL of ACD-A or citrate sodium) and three tubes (two containing 8 mL of whole blood with 1 mL of ACD-A or citrate sodium and one 4 mL EDTA-coated tube). Whole blood collected in syringes and tubes was sampled in either plastic eppendorf tube (Dominique Dutscher, Brumath, France) or EDTA microvette 500K2E (ref 20.1339.100, Sarstedt, Numbrecht, Germany). The 4 mL EDTA-coated tube was used as reference for whole blood analysis.
PRP preparation
Syringes (Proteal, Barcelona, Spain) and tubes (Estar Medical, Hamerkava, Israel) harvested were used to prepare the PRP according to the manufacturer’s instructions. Punctually, a second spin was performed to remove the platelet poor plasma and increase the platelet concentrations. The final PRP obtained was sampled in either plastic eppendorf tube or EDTA microvette 500K2E.
Quantification of platelet, white cell count and RBC concentrations
Platelets, leucocytes and RBC concentrations from whole blood and from each PRP preparation were determined with three techniques using automated haematology blood cell analyzers Micros ES (Horiba, Montpellier, France) using impedancemetry or Sysmex XN-10 (Sysmex, Japan) using impedancemetry or fluorescence flow cytometry. Measurements were performed at t=0 h, t=1 h, t=6 h and t=24 h.
Statistical analysis
Statistical analyses were performed using the GraphPad PRISM statistical software, V.5 (GraphPad Prism Software, San Diego, California, USA). A 5% level of significance was used for all statistical tests. Data are presented as median and IQR. Two-way analysis of variance (ANOVA) following Bonferroni post hoc tests were used to analyse the difference according to time, between the two anticoagulants, the two sampling methods, the two harvesting methods and the three counting methods. Regarding the impact of sampling on whole blood analysis, concentrations obtained with 4 mL EDTA-coated tube were considered as reference values. No reference was used for impact of sampling on PRP values.
Results
Demographic characteristics of healthy donors
Donors included in the study presented a median age of 26 years (24–30.75). Median initial platelet concentrations with the reference tube were of 272 G/L (222–298), 280 G/L (220–310) and 270 G/L (228–292) with the impedance and the fluorescence flow cytometry method on Sysmex XN-10 and the Micros ES, respectively. The median initial leucocyte concentrations were 6.45 G/L (5.78–6.99) and 6.40 G/L (5.4–6.7) on Sysmex XN-10 and Micros ES, respectively. The median initial RBC concentrations were 4.72 T/L (4.44–5.41) and 4.99 T/L (4.43–5.33) on Sysmex XN-10 and Micros ES, respectively.
Impact of varying parameters on blood cell count
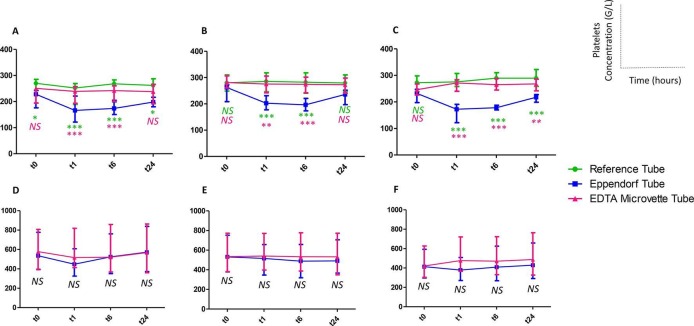
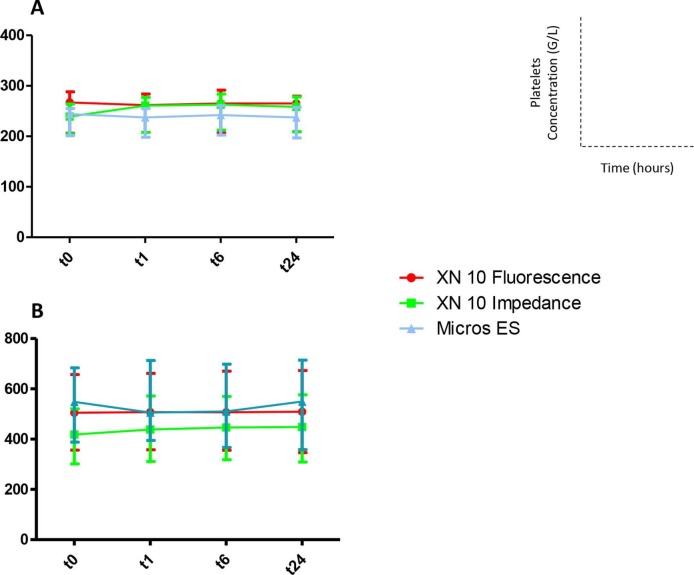
Sampling method significantly modified platelet counts over the time. Indeed, sampling in eppendorf plastic tube decreases the platelet concentrations compared with the reference tube at any time of the kinetic when counts were performed with Micros ES (figure 1A). This difference was observed at t1 h, t6 h and t1 h, t6 h, t24 h when counts were performed with Sysmex XN-10 in fluorescence and impedance techniques, respectively (figure 1B,C). Conversely, no difference was shown between Microvette EDTA and reference tube, whatever the harvesting and counting methods used (figure 2A). Finally, leucocytes and RBCs counts were similar whatever the anticoagulant, sampling, harvesting and counting methods used.
Figure 1.
Platelet concentrations (median 25–75th quartile) over the time in whole blood (A–C) and platelet-rich plasma (D–F) measured after different sampling methods with Micros ES (A and D), XN-10 fluorescence (B and E) and XN-10 impedance (C and F). NS: not significant; ***P≤0.001; **P≤0.01; *P≤0.05 (green : comparison between eppendorf tube and reference tube; pink: comparison between eppendorf tube and Microvette tube).
Figure 2.
Platelet concentrations (median, 25–75th quartile) over the time in whole blood (A) and platelet-rich plasma (B) measured after sampling in EDTA Microvette and measured with Micros ES, XN-10 fluorescence and XN-10 impedance (not significant at any time for each pair of counters compared).
Impact of varying parameters on PRP cell count
No difference was observed on platelet concentrations between PRP sampling in Eppendorf or EDTA Microvette (figure 1D–F) no matter the counter used. Type of anticoagulant or harvesting methods did not show any statistical difference on the platelet concentrations. Figure 2B represents the kinetic of platelet concentrations of PRP sampled in EDTA Microvette obtained with the different counters without any differences. Finally, leucocytes and RBC counts were similar whatever the anticoagulant, sampling, harvesting and counting methods used.
Discussion
We provide for the first time the technical tools to perform a basic cell count of whole blood and PRP under the varying harvesting and production conditions that PRP users could encounter. Kaux et al performed a large review of PRP use in gonarthrosis and conclude that ‘a platelet concentration lower than five times the baseline and avoidance of leucocytes should be preferred’ in this specific indication.7 This is particularly relevant as we already described that the platelet content of PRP is positively correlated with the quantity of GFs delivered.5 Recently, we stated that a single injection of very pure PRP (91.4%±4.1% of platelets compared with RBCs and leucocytes) with a mean dose of 2.4 billions of platelets offers a significant clinical improvement in the management of knee osteoarthritis, equivalent to a single hyaluronic acid injection in a randomised clinical trial.8 The presence or absence of leucocytes in PRP, namely neutrophils, is hotly debated. Positive reports have shown that leucocyte-rich PRP could play a valuable antimicrobial role in PRP treatment,9 10 whereas neutrophils, known to contain metalloproteases and to have a very short half-life, could impede healing.11 Finally, removing RBCs and reversing the initial composition of blood (95% of RBCs) remains the essential challenge in PRP preparation.12 Indeed, a high proportion of RBCs in PRP could be clinically detrimental through the release of reactive oxygen species and the deleterious clinical impact of RBCs on joints is clearly established with the model of haemophilic arthropathy.13 These elements largely justify a correct characterisation of PRP and in a second way of whole blood. Our main finding is in relation to blood sampling as the use of Eppendorf tubes significantly decreased platelet concentration over the time, whereas sampling in Microvette EDTA-coated tube raises to stable platelet concentrations until 24 hours whatever anticoagulant, harvesting and counting methods used. Interestingly, the likely aggregation observed in Eppendorf tube seems reversible as platelet concentrations increase slightly at t24 h with the three counters used. The whole blood quantification offers the possibility to describe the recovery rate in platelets corresponding to the percentage of platelets in PRP compared with those present in the initial blood representing a good performance indicator for PRP preparation and used in some classification.14 No statistical difference was shown on PRP where sampling method did not influence significantly the platelet counts. An interesting statement was the apparent difference in platelet counts in PRP with impedance and fluorescence methods from XN-10 counter (521.8 G/L (505.3–524.7) for impedance versus 591.5 G/L (581.5–595.8) for fluorescence). However, this difference was not significant using two-way ANOVA statistical method which could be due to the high variability in platelet concentrations of PRP obtained (from 224 to 1503 G/L with median (IQR): 597.4 G/L (388.5–683.8) at t0 h, fluorescence technique). From a technical point of view, one hypothesis is that the absence of RBCs in the PRP could disrupt platelets’ measurements in some counters. However, results were similar between XN-10 counter in fluorescence and Micros ES (606.6 G/L (599.6–613.9)) validating the use of two different kinds of counters: a large counter used on dedicated platform for outsourced quality control with XN-10 counter and a more compact counter usable as point-of-care just after PRP preparation with Micros ES.
To conclude, we recommend the systematic use of EDTA-coated tube to perform complete cell counts of whole blood and PRP which presents the advantage to give stable platelet counts until 24 hours. The use of Microvette EDTA tube is easy and appropriate for limiting the volume of samples dedicated to quality control. The use of a validated counter for PRP sample should also be taken into account and larger multicenter studies would be appropriate to provide official recommendations for realisation of PRP quality control.
Footnotes
Contributors: HG, AL, ML, YBH and JM performed the analysis and interpretation. PF and MV performed the statistical analysis. FG, JV, FDG and FS reviewed and edited the final manuscript.
Funding: Medical devices used for PRP preparation were given for free by the companies.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data sharing statement: Raw data could be obtained through contacting jeremy.magalon@ap-hm.fr
References
- 1. Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent 2001;10:225–8. 10.1097/00008505-200110000-00002 [DOI] [PubMed] [Google Scholar]
- 2. Sánchez-González DJ, Méndez-Bolaina E, Trejo-Bahena NI. Platelet-rich plasma peptides: key for regeneration. Int J Pept 2012;2012:1–10. 10.1155/2012/532519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rachul C, Rasko JEJ, Caulfield T. Implicit hype? Representations of platelet rich plasma in the news media. PLoS One 2017;12:e0182496 10.1371/journal.pone.0182496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chahla J, Cinque ME, Piuzzi NS, et al. . A call for standardization in platelet-rich plasma preparation protocols and composition reporting: a systematic review of the clinical orthopaedic literature. J Bone Joint Surg Am 2017;99:1769–79. 10.2106/JBJS.16.01374 [DOI] [PubMed] [Google Scholar]
- 5. Magalon J, Bausset O, Serratrice N. Characterization and comparison of 5 platelet-rich plasma preparations in a single-donor model. Arthroscopy 2014;30:629–38. 10.1016/j.arthro.2014.02.020 [DOI] [PubMed] [Google Scholar]
- 6. Zlotnicki JP, Geeslin AG, Murray IR, et al. . Biologic treatments for sports injuries ii think tank-current concepts, future research, and barriers to advancement, part 3: articular cartilage. Orthop J Sports Med 2016;4:232596711664243 10.1177/2325967116642433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Milants C, Bruyère O, Kaux J-F. Responders to platelet-rich plasma in osteoarthritis: a technical analysis. Biomed Res Int 2017;2017:1–11. 10.1155/2017/7538604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Louis ML, Magalon J, Jouve E, et al. . Growth factors levels determine efficacy of platelets rich plasma injection in knee osteoarthritis: a randomized double blind noninferiority trial compared with viscosupplementation. Arthroscopy 2018;34:1530–40. 10.1016/j.arthro.2017.11.035 [DOI] [PubMed] [Google Scholar]
- 9. Saad Setta H, Elshahat A, Elsherbiny K, et al. . Platelet-rich plasma versus platelet-poor plasma in the management of chronic diabetic foot ulcers: a comparative study. Int Wound J 2011;8:307–12. 10.1111/j.1742-481X.2011.00797.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moojen DJ, Everts PA, Schure RM, et al. . Antimicrobial activity of platelet-leukocyte gel against Staphylococcus aureus. J Orthop Res 2008;26:404–10. 10.1002/jor.20519 [DOI] [PubMed] [Google Scholar]
- 11. Borregaard N, Cowland JB. Granules of the human neutrophilic polymorphonuclear leukocyte. Blood 1997;89:3503–21. [PubMed] [Google Scholar]
- 12. Magalon J, Velier M, Francois P, et al. . Comment on “Responders to platelet-rich plasma in osteoarthritis: a technical analysis”. Biomed Res Int 2017;2017:1–3. 10.1155/2017/8620257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Valentino LA. Blood-induced joint disease: the pathophysiology of hemophilic arthropathy. J Thromb Haemost 2010;8:1895–902. 10.1111/j.1538-7836.2010.03962.x [DOI] [PubMed] [Google Scholar]
- 14. Magalon J, Chateau AL, Bertrand B, et al. . DEPA classification: a proposal for standardising PRP use and a retrospective application of available devices. BMJ Open Sport Exerc Med 2016;2:e000060 10.1136/bmjsem-2015-000060 [DOI] [PMC free article] [PubMed] [Google Scholar]