Abstract
Objective
To evaluate if weaning from high-frequency oscillatory ventilation (HFOV) directly to a non-invasive mode of respiratory support is feasible and results in successful extubation in extremely low birth weight (ELBW) infants.
Design
Prospective observational study.
Setting
Tertiary neonatal intensive care unit.
Patients
One hundred and eight ELBW infants of 26.2±1.4 weeks of gestational age (GA) directly extubated from HFOV.
Interventions
All infants were managed with elective HFOV and received surfactant after a recruitment HFOV manoeuvre. Extubation was attempted at mean airways pressure (MAP) ≤6 cm H2O with FiO2 ≤0.25. After extubation, all infants were supported by nasal continuous positive airway pressure (6–8 cm H2O).
Main outcome measures
Extubation failure (clinical deterioration requiring reintubation) was defined as shorter than 7 days.
Results
Ninety patients (83%) were successfully extubated and 18 (17%) required reintubation. No significant differences were found between the two groups in terms of birth weight, day of life and weight at the time of extubation. Multivariable analysis showed that GA (OR 1.71; 95% CI 1.04, 2.08) and higher MAP prior to surfactant (OR 1.51; 95% CI 1.06, 2.15) were associated with successful extubation.
Conclusions
In ELBW infants, direct extubation from HFOV at MAP ≤6 cm H2O with FiO2 ≤0.25 is feasible. Our extubation success rate (83%) is higher than conventional mechanical ventilation in this very vulnerable class of infants.
Keywords: HFOV, extubation criteria, ELBW infants, respiratory distress syndrome, mean airway pressure
What is already known on this topic?
Several studies founded the optimal timing of extubation during conventional mechanical ventilation (CMV), but extubation failure in extremely low birth weight (ELBW) infants remains a major problem.
Extubation directly from high-frequency oscillatory ventilation (HFOV) is possible and desirable. In one study, the 90% success rate in preterm infants dropped to 81% in ELBW infants.
In infants with birth weight ≤1000 g, a window of observation of 7 days may be necessary to adequately capture who will require reintubation.
What this study hopes to add?
In ELBW infants electively HFOV ventilated, direct extubation at mean airways pressure ≤6 cm H2O with FiO2 ≤0.25 is feasible.
Our success rate 7 days after the extubation attempt (83%) is higher than that reported for extubation from CMV in ELBW infants.
A recruitment HFOV manoeuvre prior to surfactant administration may be helpful for successful extubation in ELBW infants.
Introduction
Despite the increased use of non-invasive respiratory support, mechanical ventilation may be life-saving in preterm infants with respiratory failure, especially in extremely low birth weight (ELBW) infants (birth weight <1000 g).1 2 A prolonged endotracheal intubation is associated with risks and complications, including bronchopulmonary dysplasia (BPD),1–6 therefore clinicians should wean and extubate ELBW infants as soon as possible.7 Several studies tried to find the optimal timing of extubation of preterm infants treated with conventional mechanical ventilation (CMV).8–14 In these studies, success of extubation in ELBW infants ranged from 52% to 73%,8 14 and this is why extubation failure remains a major problem. In the last years, high-frequency oscillatory ventilation (HFOV) has been increasingly used in preterm infants with respiratory failure, because early HFOV could reduce risk of BPD,15 especially if associated with an open lung strategy.16 17 Despite that, data on weaning and extubation criteria are limited, especially in ELBW infants. Some clinicians are more comfortable in switching from HFOV to CMV to wean and extubate the infants,18 but this combined strategy could reduce the efficacy of HFOV alone to decrease the incidence of BPD.19 Direct extubation from HFOV is possible and may even be desirable.7 16 Van Velzen et al showed that weaning the mean airways pressure (MAP) below 8 cm H2O with a fraction of inspired oxygen (FiO2) below 0.30 is feasible during open lung HFOV and direct extubation at these settings is successful in 90% of preterm infants<37 weeks of gestational age (GA). However, the success rate dropped to 81% in 68 ELBW studied infants.20 Compared with the experience of van Velzen et al, our study is aimed at: the extubation process from HFOV in ELBW infants only (ie, the population at greater risk of ventilator-induced lung injury); evaluating the success or failure of the extubation attempt over a longer period of time (7 days instead of 48 hours after extubation) and the safety of lower pre-extubation MAP values (≤6 cm H2O instead of 8 cm H2O) as the most appropriate ventilatory set for ELBW neonates. The aim of the present study is therefore to evaluate in a cohort of ELBW infants treated with elective open lung HFOV if MAP ≤6 cm H2O and FiO2 ≤0.25 are feasible and successfully associated with direct HFOV extubation during a 7-day observation window, as longer periods may be needed to adequately capture this outcome in ELBW infants.13 14
Methods
Patients
This study was approved by the Ethics Committee of the Department of Pediatrics of Fondazione Policlinico Universitario A. Gemelli IRCCS, Roma—Università Cattolica del Sacro Cuore, which waived the need for parental consent. Between June 2011 and June 2014, inborn ELBW infants were included in this prospective observational study if they met the following conditions: a diagnosis of respiratory distress syndrome (RDS), requiring endotracheal intubation at birth or failing nasal continuous positive airway pressure (CPAP) within 24 hours of life; electively HFOV ventilated and receiving surfactant treatment and directly extubated from HFOV.
HFOV strategy
HFOV is actually the elective modality of ventilation in preterm newborns with GA ≤27 weeks and/or ELBW infants in our NICU, as a result of our previous randomised controlled trial comparing the effects of HFOV versus CMV.21 HFOV was delivered by a Dräger Babylog 8000 plus ventilator (Dräger, Lubeck, Germany) with an ‘optimum lung volume strategy’ prior to surfactant administration, recruiting collapsed alveoli using oxygenation with a FiO2 target ≤0.25 as an indirect parameter for lung volume.17
Ventilation was started at a MAP of 10 cm H2O, a frequency of 10 Hz, and an amplitude of 30%, increased if necessary until the infant’s chest was seen to be visibly vibrating. The FiO2 was initially set to ensure adequate oxygen saturation (SpO2 90%–95%). If the FiO2 was >0.25, the MAP was increased by 1–2 cm H2O every 2–5 min until FiO2 reached ≤0.25. The recruitment was stopped if oxygenation no longer improved or there were signs of lung hyperinflation (capillary refill time >3 s and/or hypotension). This approach provides a more effective means to recruit and protect acutely injured lungs.17 Surfactant was administered at the end of the recruitment procedure. Transcutaneous PaO2 of CO2 (TcPCO2) and/or PaCO2 were managed by adjustment of the oscillatory amplitude and then of the frequency. The goals of respiratory management were to maintain blood gas values of: pH 7.30–7.45, PaCO2 and/or TcPCO245–55 mm Hg, PaO2 and/or transcutaneous PaO2 of O2 (TcPO2) 50–70 mm Hg and SpO2 90%–95%. All patients received a loading dose of caffeine (20 mg/kg) immediately after admission to the NICU, then maintenance therapy22 and Remifentanil by continuous intravenous infusion at a dose of 0.075 µg/kg/min to provide analgesia during HFOV while preserving spontaneous respiratory activity.23 Doxapram was not used during the study period as per our departmental protocols.
Weaning and extubation criteria
HFOV ventilation was managed to ensure to patients the lowest possible MAP, amplitude and FiO2 in order to minimise ventilator-induced lung injury. Reduction in MAP was gradually accomplished following oxygenation and lung expansion estimated by chest radiographs. FiO2 was adjusted to maintain adequate oxygenation. Reduction of amplitude was gradually accomplished following TcPCO2 and/or PaCO2 values. Extubation was attempted when the neonate’s condition remained stable for at least 6 hours, receiving ventilation with MAP ≤6 cm H2O and FiO2 ≤0.25. At that point in time a FiO2>0.25 and ≤0.30 was acceptable, to ensure that the extubation was not delayed by small fluctuations in oxygen need.
After extubation, all the patients were supported by nasal CPAP at 6–8 cm H2O using short binasal prongs of appropriate size while nasal ventilation was not administered. Extubation failure was defined as clinical deterioration requiring reintubation during the following 7 days.13 14 All data refer only to the first extubation attempt in the studied neonates.
The indications for reintubation were: (1) repeated episodes of apnoea defined as >4 episodes of apnoea per hour (or >2 episodes of apnoea per hour when ventilation with bag and mask was required); (2) hypoxia defined as FiO2>0.50 to maintain SpO2 90%–95% for more than 2 hours despite 8 cm H2O of CPAP; (3) development of respiratory acidosis indicated by two consecutive blood gases with PaCO2 ≥65 mm Hg and pH <7.20.
Data collection
Demographic data on patient and maternal characteristics were collected from each patient. Data were collected on MAP, FiO2, amplitude, frequency, DCO2, tidal volume HFOV (VT), TcPO2, TcPCO2 at start of ventilation and at the time of extubation attempt. Finally, data on MAP and FiO2 were collected at the end of HFOV recruitment procedure, immediately prior to surfactant administration. The number of patients failing extubation was collected, including the main reason for failure and the time of reintubation. Weight and day of life at extubation, duration of mechanical ventilation and O2-therapy during the hospital stay, requirement of additional doses of surfactant and development of BPD (O2-dependence at 36 weeks of postmenstrual age) were also reported for each patient.
Statistical analysis
Values were expressed as mean and SD or median and range for continuous variables or absolute frequency and percentages for categorical variables. Continuous variables were compared with parametric (Student’s t test) or non-parametric (Mann Whitney U test) tests as appropriate. Categorical variables were compared by using a two-tailed Fisher’s exact test. A 2-tailed value of p<0.05 was considered significant. Data were analysed using commercial statistical software (Graphpad Prism V.5.0a; Chicago, Illinois, USA).
In order to evaluate the association between the successful extubation and each explanatory variable, a univariable analysis was performed using a logistic regression model by including one variable at a time. The independent variables found to be significant in the univariable analyses (p≤0.05) were included in the multivariable model. A likelihood ratio test was used to compare the suitability of the models and to select the most appropriate model. Statistical analyses were done with Stata V.2013 software (Stata Statistical Software: Release 13, College Station, Texas, USA).
Results
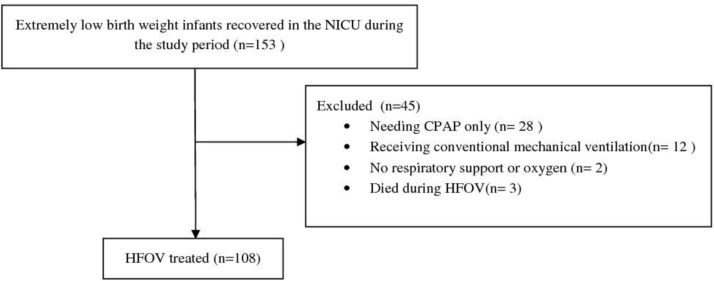
During the study period, 108 ELBW infants with RDS required elective HFOV within 24 hours of life and were directly extubated from HFOV (figure 1). Extubation was attempted at a median (range) age of 4 (1–53) days (table 1). All the comparisons were made between newborns successfully extubated (Extubation Success Group) and newborns failing the extubation attempt (Extubation Failure Group). The percentage of newborns successfully extubated was 83%. The only significant differences between the two groups were the higher percentage of males in the neonates who failed extubation and their lower GA (table 1).
Figure 1.
Infant flow diagram during the study period. CPAP, continuous positive airway pressure; HFOV, high-frequency oscillatory ventilation.
Table 1.
Patient and maternal demographics, neonatal characteristics at the time of extubation
| All infants n=108 |
Extubation Success Group, n=90 (83%) |
Extubation Failure Group, n=18 (17%) |
P values | |
| Gestational age, weeks | 26.2±1.4 | 26.3±1.3 | 25.5±1.4 | 0.02 |
| Birth weight, g | 742±166 | 750±168 | 703±159 | 0.29 |
| Complete course of antenatal steroids* | 50 (46) | 42 (47) | 8 (44) | 1 |
| 5 min Apgar Score | 8 (2-9) | 7 (2-9) | 8 (4-9) | 0.50 |
| SGA | 31 (29) | 27 (30) | 4 (22) | 0.58 |
| Male | 47 (44) | 35 (39) | 12 (67) | 0.04 |
| Premature rupture of membranes>12 hours | 38 (35) | 29 (32) | 9 (50) | 0.18 |
| Delivery by caesarean section | 82 (76) | 69 (77) | 13 (72) | 0.76 |
| Extubation weight, g | 739±149 | 741±154 | 732±142 | 0.82 |
| Extubation attempt, days | 4 (1–53) | 4 (1–53) | 5 (1–19) | 0.95 |
| Postnatal age at extubation, weeks | 27.2 (24–32) | 27.2 (24–32) | 26.3 (25–30) | 0.31 |
Values expressed as mean±SD, median (range) and number (per cent).
*A complete course of antenatal steroids was defined as two doses of betamethasone administered more than 24 hours but no more than 7 days before delivery.
SGA, small for gestational age.
Thirteen infants failed extubation within 72 hours and were reintubated at a median (range) time of 24 (2–48) hours for hypoxia (n=3), hypercapnia (n=5) and apnoea (n=5). Another five newborns who failed extubation after 72 hours and within 7 days were reintubated at a median (range) time of 120 (96–160) hours for hypoxia (n=3), and apnoea (n=2). Of the 18 infants who met failure criteria within 7 days after extubation: 7 (39%) failed due to apnoea; 6 (33%) due to hypoxia and 5 (28%) due to hypercapnia. No newborn who failed extubation had an episode of suspected or confirmed sepsis during the 7-day period after extubation.
Regarding the ventilator setting at the baseline, no significant differences were observed between the two groups (table 2). Prior to surfactant administration, the neonates of the Extubation Success Group received ventilation with a significantly higher MAP and lower FiO2 (p=0.02 and p<0.001, respectively) in comparison to the newborns of the Extubation Failure Group (table 2). At extubation, there were no differences in MAP, FiO2, amplitude or frequency between infants who were successfully extubated and those who failed extubation (table 2).
Table 2.
Ventilator settings, ventilation and transcutaneous blood gas values at baseline, presurfactant and at extubation time
| Extubation Success Group | Extubation Failure Group | P values | |
| Baseline | |||
| MAP (cm H2O) | 10.2±1.1 | 10.2±1.0 | 0.94 |
| FiO2 | 0.40±0.17 | 0.48±0.24 | 0.08 |
| Amplitude (%) | 59±33 | 56±32 | 0.72 |
| Frequency (Hz) | 9.6±1.0 | 9.7±0.8 | 0.69 |
| VT (mL/kg) | 1.6±0.6 | 1.5±0.5 | 0.51 |
| DCO2 (mL2/kg2/s) | 25±15 | 25±10 | 1 |
| TcPO2 (mm Hg) | 53±12 | 50±8 | 0.31 |
| TcPCO2 (mm Hg) | 52±8 | 54±4 | 0.30 |
| Presurfactant | |||
| MAP (cm H2O) | 13.1±1.6 | 11.9±2.4 | 0.02 |
| FiO2 | 0.25±0.01 | 0.33±0.08 | <0.001 |
| Amplitude (%) | 76±30 | 62±31 | 0.08 |
| Frequency (Hz) | 9.3±1.0 | 9.6±0.9 | 0.30 |
| VT (mL/kg) | 1.9±0.6 | 1.8±0.4 | 0.52 |
| DCO2 (mL2/kg2/s) | 29±15 | 29±10 | 1 |
| TcPO2 (mm Hg) | 59±16 | 54±11 | 0.23 |
| TcPCO2 (mm Hg) | 46±9 | 50±4 | 0.08 |
| Extubation | |||
| MAP (cm H2O) | 6.1±0.9 | 6.1±1.2 | 0.97 |
| FiO2 | 0.22±0.03 | 0.23±0.02 | 0.30 |
| Amplitude (%) | 43±24 | 39±12 | 0.46 |
| Frequency (Hz) | 9.3±1.2 | 9.3±0.7 | 0.88 |
| VT (mL/kg) | 2.1±0.6 | 1.9±0.6 | 0.28 |
| DCO2 (mL2/kg2/s) | 34±11 | 35±15 | 0.70 |
| TcPO2 (mm Hg) | 56±5 | 54±3 | 0.08 |
| TcPCO2 (mm Hg) | 48±3 | 49±2 | 0.18 |
Values expressed as mean±SD.
DCO2, coefficient of gas transport; MAP, mean airways pressure; TcPCO2, transcutaneous PaO2 of CO2; TcPO2, transcutaneous PaO2 of O2.VT: tidal volume HFOV.
Finally, the neonates of Extubation Failure Group required treatment with additional doses of surfactant more frequently than infants of Extubation Success Group (p=0.006) and received a significantly longer period of mechanical ventilation (p=0.02) (table 3). Although the neonates of the Extubation Failure Group had a higher percentage of BPD, the difference was not statistically significant (table 3).
Table 3.
Mortality and respiratory outcomes
| Extubation Success Group |
Extubation Failure Group |
P values | |
| Mortality | 11 (12) | 1 (5) | 0.68 |
| >1 dose of surfactant | 19 (21) | 10 (56) | 0.006 |
| Total ventilator, days | 8 (0.3–137) | 16 (0.5–84) | 0.02 |
| Total oxygen, days | 31 (0–200) | 41 (0.4–193) | 0.18 |
| BPD* | 16/79 (20) | 6/17 (35) | 0.20 |
Values expressed as median (range) and number (per cent).
*Data are referred to >36 weeks postmenstrual age survivors babies only.
BPD, bronchopulmonary dysplasia.
Multivariable analysis showed that GA (OR 1.71; 95% CI 1.04 to 2.08) and higher MAP prior to surfactant (OR 1.51; 95% CI 1.06 to 2.15) were associated with successful extubation (table 4).
Table 4.
Risks factors for extubation outcome: multivariable analysis
| Extubation Success Group | OR | 95% CI | P values |
| Gestational age (weeks) | 1.71 | 1.04 to 2.08 | 0.03 |
| Male | 3.08 | 0.85 to 11.2 | 0.09 |
| MAP (cm H2O) presurfactant | 1.51 | 1.06 to 2.15 | 0.02 |
| FiO2 presurfactant | 0.06 | 0.00 to 1.57 | 0.09 |
| >1 dose of surfactant | 0.31 | 0.09 to 1.16 | 0.08 |
FiO2, fraction of inspired oxygen; MAP, mean airways pressure.
Discussion
In comparison to the only experience reported on the successful extubation rates directly from HFOV by van Velzen et al,20 referring to a heterogeneous population of 214 preterm infants and including only 68 neonates with a birth weight ≤1000 g, our report provides more detailed data on the extubation process during HFOV in a large cohort of ELBW infants. Moreover, our study evaluated the success or failure of the extubation attempt over a longer period of time (within 7 days), compared with the usually shorter time windows (≤48 or ≤72 hours after extubation). This is particularly important, considering the recent remarks by Giaccone et al,13 which showed that in studies predominately enrolling ELBW infants, rates of extubation success were negatively associated with the duration of observation. By relying on shorter windows of observation, studies enrolling a larger proportion of small infants may therefore underestimate the true rate of reintubation. In fact, the reintubation rate did not appear to plateau even after a week of observation, indicating that longer periods may be necessary to adequately capture this outcome in ELBW infants.13
In our experience, neonates of the Extubation Failure Group prior to surfactant administration received ventilation with a significantly lower MAP (p<0.05) and a significantly higher FiO2 (p<0.001) in comparison respect to the newborns of the Extubation Success Group (table 2). A lower MAP prior surfactant was confirmed by multivariable analysis as an independent risk factor for extubation failure (tables 2 and 4). This occurred despite our protocol of optimal lung volume strategy aiming to fully recruit the lung before surfactant therapy, increasing step-by-step MAP until the target FiO2 of 0.25 had been reached: in case of the neonates who failed extubation, surfactant had been administered before achieving optimal lung recruitment. Even though they were affected by a more severe RDS, as demonstrated by the higher baseline FiO2 in comparison to the neonates who experienced successful extubation, the importance of fully recruiting the lung before surfactant administration should be taken into account, because of the significant association of optimal lung volume strategy with better respiratory outcomes.17 Neonates of the Extubation Failure Group received in fact more frequently additional surfactant doses (table 3).
When compared with the only study reporting the feasibility of weaning and direct extubation from HFOV in ELBW infants,20 our data showed similar rates of successful extubation: 88% within 72 hours and 83% within 7 days after the extubation attempt, versus 81% within 48 hours only, respectively. More importantly, our rates of extubation failure are lower than those recently reported by Giaccone et al in a recent systematic review on the definition of extubation success in very premature infants.13 In the multivariable linear regression analysis, median subject’s birth weight ≤1000 g was found to be an effect modifier (p=0.03) in the association between duration of postextubation observation and rate of reintubation. After stratifying the analysis for this variable, the authors found that in studies of infants with median birth weight ≤1000 g, the reintubation rate increased significantly with longer duration of observation (P=0.001). In particular, the mean reintubation rate in the newborns with median birth weight ≤1000 g increased from 25% at 72 hours to 35% at 168 hours, with the latter result being more than double of that reported in our experience (17%). It is, however, necessary to keep in mind that by prolonging the observation period, the chances of reintubation for a different cause of respiratory failure (ie, sepsis) increase. In our experience, no newborn who failed extubation had an episode of suspected or confirmed sepsis during the 7-day period after extubation.
In our study, the neonates failing extubation had significantly lower GA compared with infants successfully extubated, with the lower GA being an independent risk factor for extubation failure in the multivariable analysis (tables 1 and 4). Apnoea was the main reason for reintubation (39% of cases) stressing the important role of the central inspiratory drive in determining the premature infant’s ability to maintain adequate, independent ventilation. The use of other non-invasive respiratory support, alternatives to CPAP alone in the postextubation period (ie, nasal intermittent mandatory ventilation and/or bilevel CPAP), might be a better strategy to overcome this problem. Recently, Buzzella et al showed that in preterm infants with residual lung disease nasal CPAP in the range of 7–9 cm H2O it was more effective in reducing extubation failure than a range of 4–6 cm H2O.24 These findings suggest: the need for higher distending pressure postextubation to obtain better oxygenation with a more stable lung volume and reduced pulmonary shunt in the more immature infants who are still oxygen-dependent; the improved oxygenation and lung volume stability may have also attenuated central and obstructive apnoea.24 Hypoxia and hypercapnia accounted for most of extubation failure attempts after the first 24 hours (8 out of 13, 61%): a recruitment manoeuvre to try to adequately open the lung could play an important role in preventing extubation failure, as suggested by the results of multivariable analysis. Importantly, we used MAP ≤6 cm H2O and FiO2 ≤0.25 as criteria to attempt extubation. Using these lower setting in comparison to those adopted by van Velzen20 may improve the success rate of extubation but it may also prolong the time on the ventilator. Future studies could evaluate if extubation at higher HFOV settings in ELBW infants could result in similar rates of extubation failure while reducing the ventilation time.
Although our study suggests that direct extubation from HFOV is feasible in ELBW infants, there are some limitations and important questions that remain to be answered. First of all, the small number of ELBW infants failing extubation could limit the power to detect differences between groups and might have affected the accuracy of our estimates. Moreover, higher level of CPAP postextubation (7–9 cm H2O) or other non-invasive respiratory support, such as synchronised nasal IPPV25 or nasal HFOV,26 could be used to improve the success rate of extubation in ELBW infants.
Future randomised controlled trials will be needed to address these questions, also taking into account the possible effects on long-term respiratory outcomes.
In conclusion, this study shows that in ELBW infants electively HFOV ventilated with an open lung strategy, direct extubation from HFOV at MAP ≤6 cm H2O with FiO2 ≤0.25 is feasible. Our extubation success rate (83%) is comparable to and/or higher than success rates reported for extubation from CMV in this very vulnerable class of infants.
Supplementary Material
Acknowledgments
We thank the families of the patients for their understanding and cooperation and the nursing staff for their invaluable support.
Footnotes
Contributors: MT designed the study, collected the data, analysed the data and wrote the first and final drafts of the manuscript. AL carried out the data collection and the literature search, assisted with the analysis and provided significant edits to the manuscript. CT and CA carried out the data collection and drafted the initial manuscript. ET carried out the data collection and the initial analyses, reviewed and revised the manuscript. FS, VP, MC and PC carried out the data collection, the literature search, reviewed and revised the manuscript. VD’A, GB and CR carried out the data collection, the literature search, reviewed and made significant edits to the manuscript. RP carried out statistical analysis GV conceptualised and designed the study and critically reviewed the manuscript. All authors read and approved the submission of this version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: This study was approved by the Ethics Committee of the Department of Pediatrics of Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy—Università Cattolica del Sacro Cuore.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
- 1. Finer NN, Carlo WA, Walsh MC, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med 2010;362:1970–9. 10.1056/NEJMoa0911783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Morley CJ, Davis PG, Doyle LW, et al. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med 2008;358:700–8. 10.1056/NEJMoa072788 [DOI] [PubMed] [Google Scholar]
- 3. Stoll BJ, Hansen NI, Bell EF, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010;126:443–56. 10.1542/peds.2009-2959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miller JD, Carlo WA. Pulmonary complications of mechanical ventilation in neonates. Clin Perinatol 2008;35:273–81. 10.1016/j.clp.2007.11.004 [DOI] [PubMed] [Google Scholar]
- 5. Garland JS. Strategies to prevent ventilator-associated pneumonia in neonates. Clin Perinatol 2010;37:629–43. 10.1016/j.clp.2010.05.003 [DOI] [PubMed] [Google Scholar]
- 6. Walsh MC, Morris BH, Wrage LA, et al. Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr 2005;146:798–804. 10.1016/j.jpeds.2005.01.047 [DOI] [PubMed] [Google Scholar]
- 7. Sant’Anna GM, Keszler M. Weaning infants from mechanical ventilation. Clin Perinatol 2012;39:543–62. 10.1016/j.clp.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 8. Vento G, Tortorolo L, Zecca E, et al. Spontaneous minute ventilation is a predictor of extubation failure in extremely-low-birth-weight infants. J Matern Fetal Neonatal Med 2004;15:147–54. 10.1080/14767050410001668239 [DOI] [PubMed] [Google Scholar]
- 9. Dimitriou G, Greenough A, Endo A, et al. Prediction of extubation failure in preterm infants. Arch Dis Child Fetal Neonatal Ed 2002;86:32F–5. 10.1136/fn.86.1.F32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Szymankiewicz M, Vidyasagar D, Gadzinowski J. Predictors of successful extubation of preterm low-birth-weight infants with respiratory distress syndrome. Pediatr Crit Care Med 2005;6:44–9. 10.1097/01.PCC.0000149136.28598.14 [DOI] [PubMed] [Google Scholar]
- 11. Kamlin CO, Davis PG, Morley CJ. Predicting successful extubation of very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 2006;91:F180–F183. 10.1136/adc.2005.081083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stefanescu BM, Murphy WP, Hansell BJ, et al. A randomized, controlled trial comparing two different continuous positive airway pressure systems for the successful extubation of extremely low birth weight infants. Pediatrics 2003;112:1031–8. 10.1542/peds.112.5.1031 [DOI] [PubMed] [Google Scholar]
- 13. Giaccone A, Jensen E, Davis P, et al. Definitions of extubation success in very premature infants: a systematic review. Arch Dis Child Fetal Neonatal Ed 2014;99:F124–7. 10.1136/archdischild-2013-304896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Manley BJ, Doyle LW, Owen LS, et al. Extubating Extremely Preterm Infants: Predictors of Success and Outcomes following Failure. J Pediatr 2016;173:45–9. 10.1016/j.jpeds.2016.02.016 [DOI] [PubMed] [Google Scholar]
- 15. Cools F, Offringa M, Askie LM. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2015;3:CD000104 10.1002/14651858.CD000104.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Courtney SE, Durand DJ, Asselin JM, et al. High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants. N Engl J Med 2002;347:643–52. 10.1056/NEJMoa012750 [DOI] [PubMed] [Google Scholar]
- 17. Tana M, Zecca E, Tirone C, et al. Target fraction of inspired oxygen during open lung strategy in neonatal high frequency oscillatory ventilation: a retrospective study. Minerva Anestesiol 2012;78:151–9. [PubMed] [Google Scholar]
- 18. Johnson AH, Peacock JL, Greenough A, et al. High-frequency oscillatory ventilation for the prevention of chronic lung disease of prematurity. N Engl J Med 2002;347:633–42. 10.1056/NEJMoa020432 [DOI] [PubMed] [Google Scholar]
- 19. Clark RH, Gerstmann DR, Null DM, et al. Prospective randomized comparison of high-frequency oscillatory and conventional ventilation in respiratory distress syndrome. Pediatrics 1992;89:5–12. [PubMed] [Google Scholar]
- 20. van Velzen A, De Jaegere A, van der Lee J, et al. Feasibility of weaning and direct extubation from open lung high-frequency ventilation in preterm infants. Pediatr Crit Care Med 2009;10:71–5. 10.1097/PCC.0b013e3181936fbe [DOI] [PubMed] [Google Scholar]
- 21. Vento G, Matassa PG, Ameglio F, et al. HFOV in premature neonates: effects on pulmonary mechanics and epithelial lining fluid cytokines. A randomized controlled trial. Intensive Care Med 2005;31:463–70. 10.1007/s00134-005-2556-x [DOI] [PubMed] [Google Scholar]
- 22. Schmidt B, Roberts RS, Davis P, et al. Caffeine therapy for apnea of prematurity. N Engl J Med 2006;354:2112–21. 10.1056/NEJMoa054065 [DOI] [PubMed] [Google Scholar]
- 23. Giannantonio C, Sammartino M, Valente E, et al. Remifentanil analgosedation in preterm newborns during mechanical ventilation. Acta Paediatr 2009;98:1111–5. 10.1111/j.1651-2227.2009.01318.x [DOI] [PubMed] [Google Scholar]
- 24. Buzzella B, Claure N, D’Ugard C, et al. A randomized controlled trial of two nasal continuous positive airway pressure levels after extubation in preterm infants. J Pediatr 2014;164:46–51. 10.1016/j.jpeds.2013.08.040 [DOI] [PubMed] [Google Scholar]
- 25. Gizzi C, Montecchia F, Panetta V, et al. Is synchronised NIPPV more effective than NIPPV and NCPAP in treating apnoea of prematurity (AOP)? A randomised cross-over trial. Arch Dis Child Fetal Neonatal Ed 2015;100:F17–23. 10.1136/archdischild-2013-305892 [DOI] [PubMed] [Google Scholar]
- 26. Zhu XW, Zhao JN, Tang SF, et al. Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with moderate-severe respiratory distress syndrome: A preliminary report. Pediatr Pulmonol 2017;52:1038–42. 10.1002/ppul.23755 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.