Supplemental Digital Content is available in the text
Keywords: acupuncture, dry needling, efficacy, low back pain, meta-analysis, myofascial trigger points
Abstract
Background:
To evaluate the efficacy and safety of dry needling (DN) for treating low back pain (LBP).
Methods:
Nine databases were searched from inception to October 2017. Eligible randomized controlled trials (RCTs) involving DN for treating LBP were retrieved. Two reviewers independently screened the articles, extracted data, and evaluated the risk of bias among the included studies using the risk of bias assessment tool by Cochrane Collaboration.
Results:
Sixteen RCTs were included and the risk of bias assessment of them was “high” or “unclear” for most domains. Meta-analysis results suggested that DN was more effective than acupuncture in alleviating pain intensity and functional disability at postintervention, while its efficacy on pain and disability at follow-up was only equal to acupuncture. Besides, DN was superior to sham needling for alleviating pain intensity at postintervention/follow-up and functional disability at postintervention. Additionally, qualitative review revealed that DN combined with acupuncture had more significant effect on alleviating pain intensity at postintervention and achieved higher response rate than DN alone. However, compared with other treatments (laser, physical therapy, other combined treatments, etc.), it remained uncertain whether the efficacy of DN was superior or equal because the results of included studies were mixed.
Conclusions:
Compared with acupuncture and sham needling, DN is more effective for alleviating pain and disability at postintervention in LBP, while its effectiveness on pain and disability at follow-up was equal to acupuncture. Besides, it remains uncertain whether the efficacy of DN is superior to other treatments. Nevertheless, considering the overall “high” or “unclear” risk of bias of studies, all current evidence is not robust to draw a firm conclusion regarding the efficacy and safety of DN for LBP. Future RCTs with rigorous methodologies are required to confirm our findings.
Details of ethics approval:
No ethical approval was required for this systematic review and meta-analysis.
1. Introduction
With an estimated point prevalence of 23%,[1] low back pain (LBP) has been a major public health challenge in the world, contributing great medical burden. It is also becoming one of the leading specific causes of disability worldwide.[1,2]
To treat LBP, numerous approaches have been explored. Pharmacological treatment remains a mainstream therapy for LBP but it is still not satisfactory, considering the potential harms caused by medication such as non-steroidal anti-inflammatory drugs and opioids in the management of LBP.[3] Clinicians have been seeking for beneficial non-drug therapies including acupuncture, exercise, and multidisciplinary and behavioral treatment.[4]
Dry needling (DN), as a relatively new treatment modality practised by physicians worldwide, is often used to treat musculoskeletal pain (including LBP) and has attracted more and more interest.[5] It involves a minimally invasive procedure in which an acupuncture needle is inserted directly into myofascial trigger points (MTrPs).[6] Although an acupuncture needle is used, unlike conventional acupuncture that is based on the theory of traditional Chinese medicine, DN is developed along with the theory of MTrPs.[6] It is generally accepted that DN no longer involves traditional Chinese medicine concepts and belongs to a subcategory of western medical acupuncture.[5,7] In recent years, an increasing number of trials have been performed to explore the efficacy of DN for treating pain; however, the conclusions were conflicting.[7] The real effectiveness of DN remains controversial. So, it is urgent to seek for the evidence of this therapy for treating pain.
Several related systematic reviews (SRs)[8–13] have been conducted in this field. To our knowledge, however, there were some concerns in previous studies. Firstly, for the region of pain, all previous SRs about DN did not assess its efficacy for managing pain in the region of low back except for 1 SR.[12] However, this review[12] failed to include several eligible RCTs[14–18] and did not compare the efficacy of DN with acupuncture by performing meta-analysis, which was of great interest to most clinicians and physicians. Secondly, considering acupuncture as a generally acknowledged therapy for treating LBP,[19] most previously published SRs did not include RCTs that adopted acupuncture as controls and compare the effectiveness of DN with acupuncture. Thirdly, new related RCTs[20] in the past few years were not included in most published SRs. Therefore, it was essential to integrate subsequently published studies into a new SR to update the conclusion.
Considering these concerns, we conducted this updated SR to evaluate the efficacy and safety of DN for treating LBP.
2. Methods
2.1. Literature Search
Nine databases were searched to extensively retrieve potentially eligible randomized controlled trials (RCTs) from inception to October, 2017: PubMed; EMBASE; Ovid; Web of Science; Cochrane Library; CINAHL; ScienceDirect; China National Knowledge Infrastructure (CNKI); Chinese Biomedical Literature Database (CBM). No language restrictions were imposed. The following keywords were used individually or jointly to search eligible RCTs: “dry needle,” “dry needling,” “acupuncture,” “low back pain,” “backache,” “myofascial pain syndrome,” “trigger point,” “MTrP,” and “randomized.” References of all eligible papers were scanned to identify additional eligible publications.
2.2. Inclusion criteria
2.2.1. Types of research
RCTs and quasi-RCTs were included in this SR. Quasi-RCTs were defined as trials that allocated participants to treatment groups by using allocation methods such as by alternation, date of birth, or case record number.[21]
2.2.2. Types of participants
Adult patients (>18 years old) with LBP as well as the presence of MTrPs were included. The duration of LBP was not limited. Patients with (sub)acute (≤12 weeks) or chronic low back pain (>12 weeks) were included. Patients with LBP caused by pathologic entities such as infection, metastatic diseases, neoplasm, or fractures were excluded. Patients whose LBP was associated with pregnancy and parturition were also excluded.
2.2.3. Types of intervention
The experiment group received DN and the control interventions included acupuncture, sham needling (i.e., sham acupuncture and sham DN), and other active treatments. Other active treatments included therapies that were generally acknowledged for treating LBP, such as oral drugs, physiotherapy, behavioral therapy, or massage.
In addition, RCTs involving DN combined with another therapy were also included if that adjuvant therapy was the same in both experimental and control groups.
2.2.4. Types of outcome measurements
Primary outcomes included measures used to assess pain intensity, such as visual analogue scale (VAS); measures used to assess functional disability, such as Roland Morris disability questionnaire (RMQ) and Oswestry disability index (ODI). Secondary outcomes included response rate, which was often reported as an important outcome measurement in trials conducted in China and it was calculated based on 3 different levels of VAS reduction at postintervention (markedly effective, effective, inefficacious). Response rate means the percentage of the total number of participants who were categorized in the first 2 levels. Adverse events.
2.3. Exclusion criteria
Repeatedly published papers or non-RCTs; RCTs with no available data to extract; the experimental group in the RCT adopted DN combined with acupuncture; RCTs only comparing the efficacy 2 different types of DN (deep DN vs superficial DN.
2.4. Risk of bias assessment
Risk of bias assessment for included RCTs was evaluated independently by 2 reviewers using the Cochrane risk-of-bias tool,[22] which includes the following items: random sequence generation, allocation concealment, blinding of outcome assessment, blinding of participants and personnel, incomplete outcome data, selective reporting, and other bias. Any disagreements were resolved by discussion.
2.5. Data extraction
After excluding duplicate articles, 2 reviewers independently screened papers by reading titles and abstracts to exclude obviously unrelated papers. Full texts of all potentially eligible papers were screened based on the inclusion/exclusion criteria. After including all eligible RCTs, the same 2 reviewers extracted data regarding author, country, participants, intervention, control types, treatment course, sessions of treatment, primary and secondary outcomes, based on a pre-defined data extraction table. If relevant data were missing, we planned to contact the corresponding authors for further information via email. To note, pain intensity and functional disability measured immediately (measured after the first treatment session), at postintervention (measured at the end of all treatment sessions) and at follow up were extracted respectively, with the aim to evaluate the immediate, postintervention and follow-up effect of DN for treating LBP. Any disagreements during RCT selection and data extraction were resolved by discussion or arbitration by a third reviewer.
2.6. Statistical analysis
In terms of continuous data and dichotomous data, effect sizes were measured using standardized mean difference (SMD) and 95% confidence interval (CI), or risk ratio (RR) with 95% CI, respectively. Heterogeneity within RCTs was examined base on the I2 test, considering I2 ≥50% as a sign of substantial heterogeneity.[23] Once there were >2 homogeneous studies, RevMan 5.3 (Cochran Collaboration, London, UK) software was used to perform meta-analyses. Sensitivity analyses were conducted for the robustness of the result of meta-analyses. If there were >10 trials included in meta-analysis, publication bias was assessed through funnel plot.[24]
2.7. Ethical statement
As all analyses were grounded on previously published studies, ethical approval was not necessary.
3. Results
3.1. Search results
The process of eligible RCT selection was displayed in the flowchart (Fig. 1). Finally, 16 RCTs [14–18,20,25–34] involving 1233 patients were included in this SR.
Figure 1.
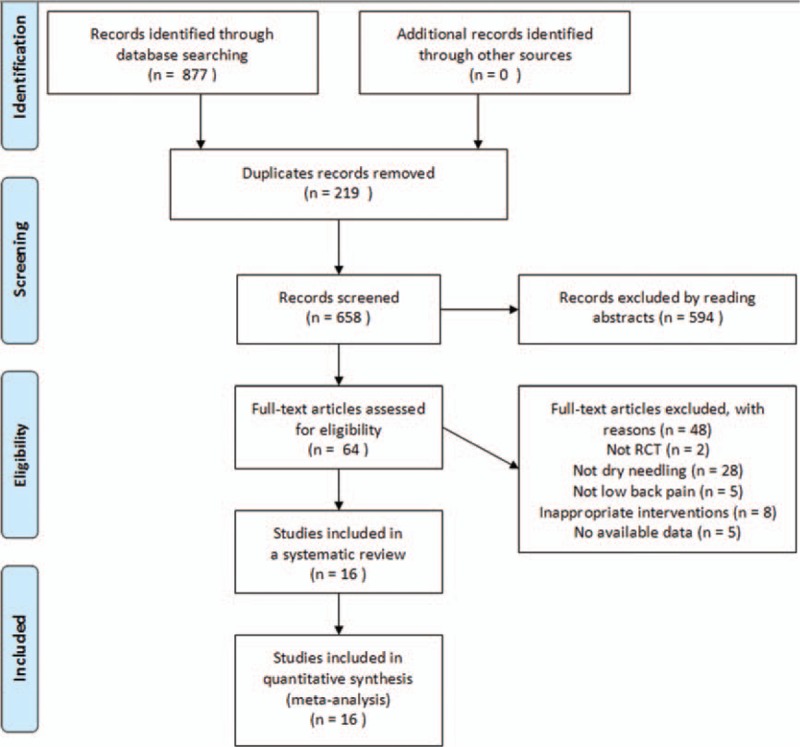
Flowchart of the trial selection process.
3.2. Study characteristics
Characteristics of included studies were summarized in Table 1. Overall, 9 RCTs[15–18,30–34] were conducted in China, 4[25–27,29] in Japan, 1 [28] in Spain, and 1[14] in the United States, 1 [20] in Iran. Only 6 trials [15,20,25–27,29] introduced the background of the DN manipulators. All but 2 RCTs[14,16] described the detailed manipulation method of DN. The mean treatment sessions and total treatment courses ranged from 1 to 20 times, 1 to 140 days; respectively. The mean duration of follow-up ranged from 1 to 12 weeks.
Table 1.
Characteristics and main outcomes of included RCTs.
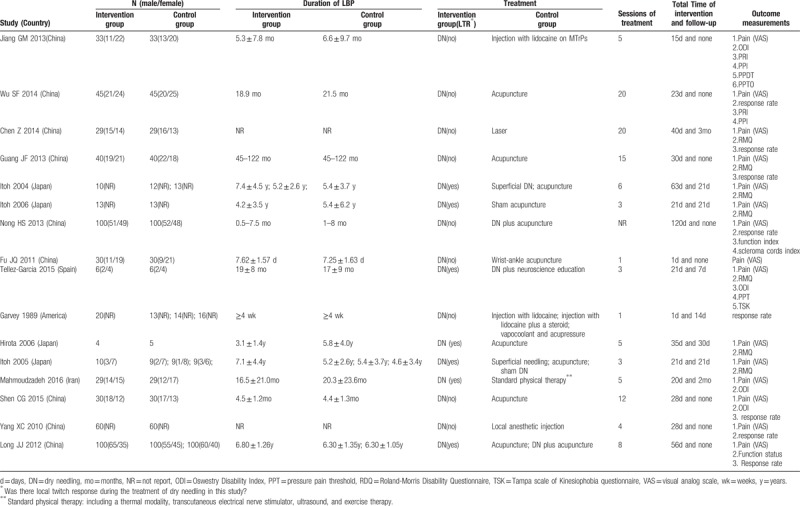
All studies compared the therapeutic effect of DN with other treatments. The control groups included the following types: acupuncture,[15,25,26,29,32–34] wrist-ankle acupuncture,[17] sham needling,[26,27] trigger point injection therapy,[14,18,31] laser irradiation,[30] DN plus neuroscience education,[28] DN in combination with acupuncture,[16,34] and standard physical therapy.[20] Regarding outcome measures, 12 RCTs[15,16,20,25–27,29–34] evaluated pain intensity using VAS. Seven[25–30,33] trials and 4 trials[18,20,28,32] assessed functional disability using RMQ and ODI, respectively. Eight studies used response rate as outcomes.
3.3. Assessment for risk of bias
Risk of bias evaluation for each included RCT was summarized in Fig. 2. All studies had either unclear or high risk of bias on one or more methodological domains. Risk of bias of all included studies with detailed support for each judgement was summarized (see Supplementary Table S1).
Figure 2.
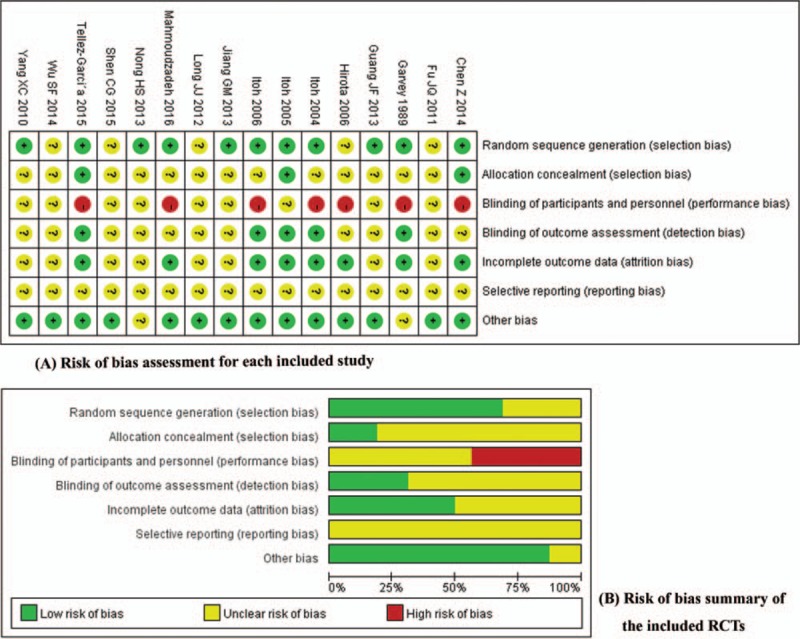
Risk of bias assessment of the included studies. (A) Risk of bias assessment for each included study (B) risk of bias summary of the included RCTs. RCT = randomized controlled trial.
For the majority of included RCTs, random sequence generation and other sources of bias were rated as low risk of bias. Apart from 5 RCTs[15,17,25,32,34] which did not report the method of randomization, the remaining 11 trials adopt computerized randomization, random number table, or coin toss to produce random sequence. With respect to other sources of bias, only 2 trials[14,16] were rated as unclear risk of bias.
Most studies did not provide information about allocation concealment and this domain was classed as “unclear” risk of bias. Selective reporting of all included RCTs was assessed as “unclear” risk of bias because of the inaccessibility to the trial protocol. The majority of the included trials published in Chinese scored “unclear” on allocation concealment, blinding of participants/personnel, blinding of outcome assessment, and incomplete outcome data. By contrast, most foreign RCTs scored “low” on blinding of outcome assessment and incomplete outcome data. Seven trials[14,20,25–27,29,30] reported reasons about dropouts.
3.4. Outcomes and effect estimates
For the purpose of the review, subgroup analysis was performed based on different types of control groups, different assessment times, and different outcome measures.
3.4.1. DN versus sham needling
3.4.1.1. Effect at postintervention
(1) Pain intensity
This group included 2 trials[25,26] and significant difference in postintervention pain intensity between 2 groups was observed, which was in favor of the better effect of DN for alleviating pain (Fig. 3: SMD = –2.74, 95% CI: –3.77 to –1.71, I2 = 26%).
Figure 3.
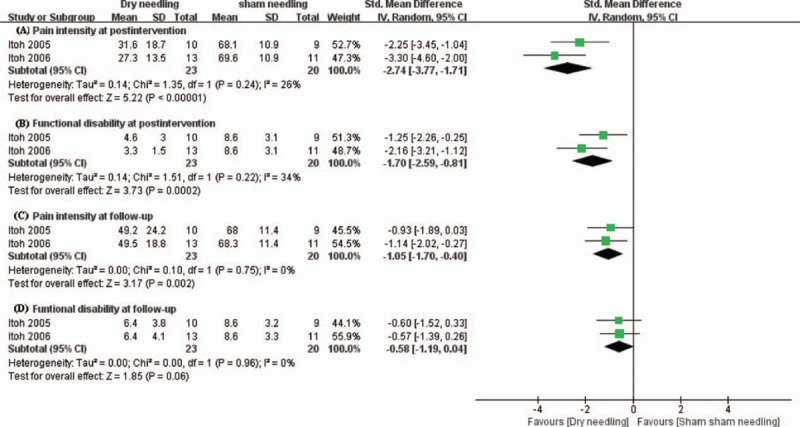
Forest plot for DN compared with sham needling. (A) Pain intensity at postintervention. (B) Functional disability at postintervention. (C) Pain intensity at follow-up. (D) Functional functional disability at follow-up. DN = dry needling.
(2) Functional disability
Meta-analyses of 2 studies[25,26] showed that a better effect on alleviating postintervention functional disability was achieved by DN in contrast to sham needling (Fig. 3: SMD = –1.70, 95% CI: –2.59 to –0.81, I2 = 34%).
3.4.1.2. Effect at follow-up
(1) Pain intensity
Meta-analyses of 2 studies[25,26] demonstrated that the effect of DN was superior to sham needling for alleviating follow-up pain intensity (Fig. 3: SMD = –1.05, 95% CI: –1.70 to –0.40, I2 = 0%).
(2) Functional disability
Meta-analyses of 2 studies[25,26] revealed that there were no statistically significant differences between the 2 groups on follow-up functional disability (Fig. 3: SMD = –0.58, 95% CI: –1.19 to 0.04, I2 = 0%).
3.4.2. DN versus acupuncture
3.4.2.1. Immediate effect
(1) Pain intensity
Only one trial was included in this subgroup. This RCT[17] included 60 patients of acute LBP. The treatment group received DN and the control arm was given wrist-ankle acupuncture. After 1 session of treatment (5 minutes), the DN group scored significantly lower VAS than pretreatment, but no significant reductions in VAS was achieved in the acupuncture group. There were significant statistical differences between the 2 groups, implying that the immediate effect of DN was more beneficial than wrist-ankle acupuncture.
3.4.2.2. Effect at postintervention
(1) Pain intensity
This subgroup involved 6 trials[15,26,29,32–34] covering 467 participants. Meta-analysis result (Fig. 4) demonstrated that a better effect on alleviating pain intensity was achieved by DN than acupuncture (SMD = –0.96, 95% CI: –1.80 to –0.12).
Figure 4.
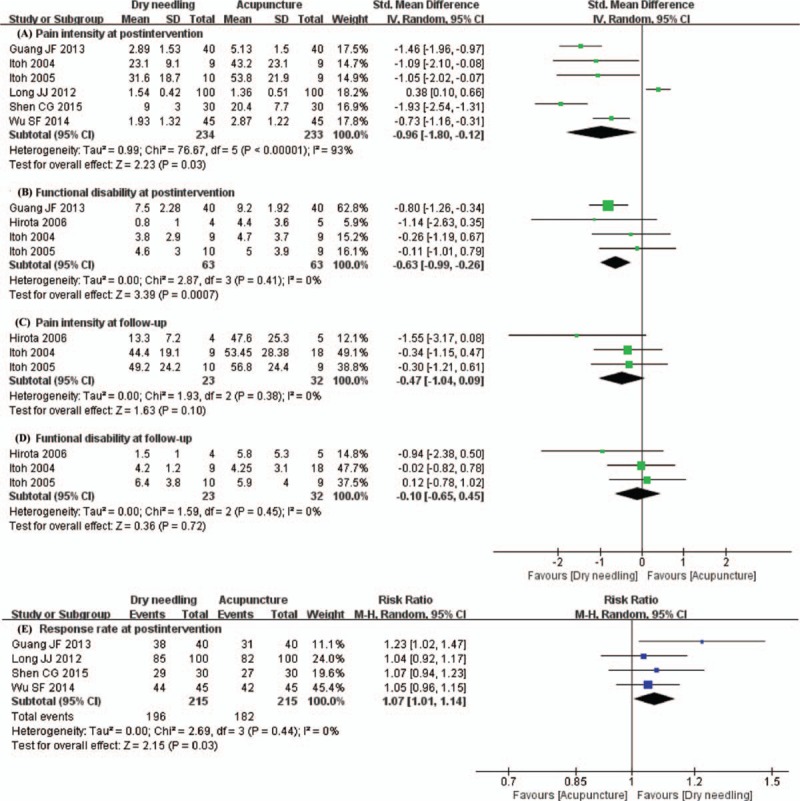
Forest plot for DN compared with acupuncture. (A) Pain intensity at postintervention. (B) Functional disability at postintervention. (C) Pain intensity at follow-up. (D) Functional disability at follow-up. (E) Response rate at postintervention. DN = dry needling.
(2) Functional disability
Four trials[25,26,29,33] were included in this subgroup and meta-analysis result (Fig. 4) proved that DN achieved more significant effect on alleviating functional disability than acupuncture, with low heterogeneity (SMD = –0.63, 95% CI: –0.99 to –0.26, I2 = 0%).
(3)Response rate
Four RCTs[15,32–34] were pooled in this subgroup and meta-analysis outcome (Fig. 4) demonstrated that DN achieve better effect on improving response rate than acupuncture, with no heterogeneity (RR = 1.07, 95% CI: 1.01–1.14, I2 = 0%).
3.4.2.3. Effect at follow-up
(1) Pain intensity
Meta-analyses of 3 studies[25,26,29] showed that the differences were not statistically significant between the 2 groups for alleviating follow-up pain intensity (Fig. 4: SMD = –0.47, 95% CI: –1.04–0.09, I2 = 0%).
(2) Functional disability
Meta-analyses of 3 studies[25,26,29] showed that there were no statistically significant differences between the 2 groups for alleviating follow-up functional disability (Fig. 4: SMD = –0.10, 95% CI: –0.65 to 0.45, I2 = 0%).
3.4.3. DN versus other treatments
Other treatments were defined as active treatments apart from acupuncture. And they also included combined treatments, such as DN combined with acupuncture and DN combined with neuroscience education. Considering the clinical heterogeneity, data were not pooled and meta-analyses were not performed in this subgroup. Instead, quantitative review was adopted to summarize the results of the included studies.
3.4.3.1. Effect at postintervention
(1) Pain intensity
Seven[16,18,20,28,30,31,34] studies reported outcomes of pain intensity at postintervention, which was assessed using VAS. Two[20,31] of them revealed that DN was more effective for alleviating pain intensity at postintervention, compared with injection therapy and standard physical therapy, respectively. Besides, 2[18,28] trials demonstrated that there was no significant difference between DN and other treatments, one[18] of which used local injection as control and the other trial[28] adopted DN plus neuroscience education in the control group.
By contrast, 1 study conducted by Chen[30] showed a statistically significant effect in favor of laser over DN. The remaining 2[16,34] trials adopts DN combined with acupuncture as control, and both of them revealed that showed a statistically significant difference in favor of DN + acupuncture over DN alone.
(2) Functional disability
Three[18,28,30] trials provided outcomes of functional disability at postintervention. Two[18,28] of them assessed it using ODI and 1[30] used RMQ. No significant difference was observed in functional disability at postintervention between DN and other treatments in 2[18,28] trials, 1[18] of which used local injection as control and the other one[28] adopted DN combined with neuroscience education in the control group. However, the remaining one trial conducted by Chen[30] showed a statistically significant effect in favor of laser over DN.
(3) Response rate
Four[14,16,30,31] studies reported outcomes of response rate at postintervention. In 2[14,31] studies that compare DN with trigger point injection, DN achieved a more favorable effect for improving the response rate. However, the trial by Chen[30] demonstrated a statistically significant effect in favor of laser over DN and the trial by Nong[16] revealed that the group of DN plus acupuncture had a more significant improvement than the DN group.
3.4.3.2. Effect at follow-up
(1) Pain intensity
Two studies[20,30]reported pain intensity at the end of follow-up. The study conducted by Mahmoudzadeh et al[20] revealed that DN achieved a more favorable effect than physical therapy for improving follow-up VAS. By contrast, the other trial[30] showed a statistically significant effect in favor of laser over DN.
(2) Functional disability
Two studies[20,30] reported functional disability at follow-up. Mahmoudzadeh et al[20] employed ODI to assess functional disability at follow-up and the results revealed a statistically significant effect in favor of DN over physical therapy, while Chen[30] used RMQ to evaluated functional disability at follow-up and the results showed a statistically significant effect in favor of laser over DN.
3.5. Sensitivity analyses
Sensitivity analyses via alteration of effect modes (fixed or random) were performed. The effect estimates in each subgroup did not differ significantly, implying that small sample effect did not influence the pooled effect estimate. Thus, the results of meta-analyses above were robust.
3.6. Publication bias
Publication bias was not evaluated due to the insufficient numbers (n < 10) of RCTs included in meta-analyses.
3.7. Safety evaluation
Only 3[14,18,27] RCTs reported adverse events. One RCT[18] reported sticking of the needle occurring in 1 participant of the treatment group and 1 study[27] mentioned occurrence of deterioration of symptoms in 1 patient, who was dropped out later. Two participants in Garvey's trial[14] had dry needle-sticks, which led to increasing pain; and another patient was sent to the emergency room with complaints of fever and chills.
4. Discussion
4.1. Summary of evidence
This SR evaluated the efficacy of DN for treating LBP by extensively retrieving eligible RCTs. Finally, 16 RCTs were included and based on the meta-analysis results, it appeared that the effect of DN on alleviating pain intensity and functional disability at postintervention was more significant than acupuncture. However, the effectiveness of DN on pain intensity and functional disability at follow-up was equal to acupuncture. And DN had more significant effect than sham needling on alleviating postintervention pain intensity, postintervention functional disability, and follow-up pain intensity, but its effect on alleviating follow-up functional disability was not superior to sham needling.
In addition, according to qualitative review results, it seems that DN combined with acupuncture was more effective in alleviating pain intensity and achieved higher response rate than DN alone. However, when compared with trigger point injection or laser or standard physical therapy, it remained uncertain whether DN was superior to these other treatments or had equal efficacy because results of the included studies were mixed. It should be pointed out that evidence based on qualitative method should be interpreted cautiously due to the limitation and small power of qualitative review.
In regard to safety evaluation, a conclusion for the safety of DN still could not be drawn because a majority of the included trials did not have adequate reporting of adverse events associate with DN,
Nevertheless, due to the overall “high” or “unclear” risk of bias of most included studies, all current evidences above were not robust to permit a firm conclusion regarding the efficacy and safety of DN for LBP.
4.2. Comparison with previous SRs
Two similar SRs[8,12] in this field were published previously. The SR by Tough et al[8] investigated the effectiveness of acupuncture and DN in the management of myofascial trigger point pain (MTrPs located in multiple body regions, including the upper quarter, low back, and lower extremity) in 2009, but only 2 out of the 7 included RCTs involved DN for treating LBP. The latest SR published by Liu et al[12] also evaluated the current evidence of the effectiveness of DN for treating LBP associated with MTrPs. However, this review[12] failed to include several eligible RCTs[14–18] and did not compare the efficacy of DN with acupuncture by performing meta-analysis, which was of great interest to most clinicians.
Compared with these SRs, our study aimed to evaluate the efficacy of DN for treating LBP and integrate subsequently published studies as well as all eligible RCTs to update the current evidence. Moreover, we compared the efficacy of DN with traditional acupuncture/sham needling for treating LBP in our meta-analysis, which was of absence in all previously published SRs. Thus, this study adds new value to the current evidence and updates the conclusions.
4.3. Implications for clinical trials
In contrast to acupuncture, in which needles are inserted in meridian points, extra points and Ah-shi points (painful points), points for DN are chosen by palpation of the muscle and the needles are inserted into MTrPs. MTrPs are defined as points with excessive strain that, when palpated, can cause symptoms as localized/referred pain and a muscle twitch response.[35–37] Along with the increased use of DN, some physicians had been debating about whether dry needling belonged to traditional acupuncture. Especially, for the treatment of musculskeletal pain, DN and acupuncture overlapped greatly in their origin, techniques and theories.[38,39] Previous studies[40,41] also found that MTrPs were significantly correlated to meridian points and Ah-shi points. Although this therapy had roots in traditional acupuncture, current mainstream view still tended to regard DN as an adaption of traditional acupuncture which provided mechanistic underpinnings from contemporary scientific-based medicine including anatomy, physiology, and pathology.[42] It was (seemingly) different from traditional acupuncture.[43] Our study revealed that DN was more effective than acupuncture for alleviating pain intensity and functional disability at postintervention, but during follow-up period, its efficacy was only equal to acupuncture. However, before recommending this therapy to more physicians, we should be concerned about the manipulation method of DN.
In our review, most studies specified the manipulation method of DN in details. However, the applied manipulation method varied across studies, especially for trials conducted in China. As a dynamic needling technique, DN generally involves a relatively slow, but deliberate, steady lancing motion in and out of the muscle.[44] One of key points during the manipulation of DN is to elicit a local twitch response (LTR),[45] which is an involuntary spinal cord reflex contraction of the muscle fibers in a taut band following palpation or needling of the band or MTP.[46] Previous studies had shown a positive relationship between the presence of a LTR during treatment with positive clinical outcomes.[47] Out of the 16 studies included in this review, only 7 studies[20,25–29,34] reported LTR during treatment. The “fast-in and fast-out” technique put forward by Hong[47] to produce LTR has been generally accepted by most clinicians in the west.[38] But in real-world practice, especially in China, the manipulation method of DN has not been uniformed and varies greatly. No agreement has been reached on the best form of DN manipulation method, leading to difficulties in assessing the real efficacy of DN. For future clinical trials, we suggest that the best manipulation method of DN should be explored and standardized.
4.4. Implications for future research
High-quality RCTs are not only the foundation of health assessment reports and policy decision reports, they are also important for conducting authoritative SRs. In order to judge the validity of RCTs, researchers and readers should be informed on all details about random sequence generation, allocation concealment, and blinding. With regard to risk of bias for methodological domains among the included studies in this SR, compared with 7 foreign RCTs, most trials conducted in China failed to adequately report allocation concealment and blinding, which in turn greatly reduced the quality of RCTs. Moreover, based on outcomes measured at different time points of the included RCTs, we found that pain intensity and functional disability measured immediately after one session or at follow-up were not adequately reported. Only 1 trial[17] reported immediate outcomes and 8 RCTs[14,20,25–30] provided follow-up outcomes. Consequently, the design, performance, and reporting of RCTs in future research should be more rigorous, which could be achieved by training of researchers, using standardized reporting criterion such as CONSORT for traditional Chinese medicine.[48]
4.5. Study limitations
It should be acknowledged that this review has several limitations. Most importantly, the majority of the included studies had high/unclear risk of bias with regard to randomization, allocation concealment, and blinding. Most relevant RCTs were published only as brief reports. Particularly, this was frequently the case for those studies published in Chinese, for which published versions were often >2 pages long. Although we made efforts to contact authors to confirm study eligibility, we did not have adequate time or resources to successfully contact all authors for further information and details. Thus, in general the completeness of study information was low, resulting in a high number of studies for which risk of bias was classed as “unclear.” Due to the characteristic of DN, although blinding of the therapist who applied DN was difficult, blinding of patients and outcome assessors should be attempted to minimize the performance and assessment bias. Consequently, these significant methodological shortcomings of the included studies greatly reduced the quality of evidence. The level of all current evidence from this review was very low and should be recommended in great caution. Secondly, the clinical heterogeneity should not be ignored in this review. Substantial heterogeneity was detected in some subgroups. With insufficient studies included, I2 also had low statistical power and its confidence intervals could be large.[23] Thirdly, some included RCTs adopted response rate as the primary outcome measure, which was calculated based on 3 different levels of VAS reduction at postintervention (1. markedly effective, 2. effective, 3. Inefficacious). Response rate meant the percentage of the total number of participants who were categorized in the first two levels. Compared with other generally acknowledged outcome measures like VAS, RMQ, or ODI, response rate was a relatively ambiguous and subjective measurement, which could not reflect the real efficacy of DN. Thus, any result involving meta-analysis of response rate should be interpreted prudently. To further confirm the efficacy of DN, outcome assessments should be conducted more rigorously in future trials.
5. Conclusions
Compared with acupuncture and sham needling, current evidence reveals that DN is more effective for alleviating pain intensity and functional disability at postintervention in LBP, while its effectiveness on pain intensity and functional disability at follow-up was equal to acupuncture. Besides, it remains uncertain whether the efficacy of DN at postintervention and follow-up is superior to other treatments (laser, physical therapy, trigger point injection other combined treatments, etc.) for treating LBP. In addition, the safety of DN also remains unclear due to inadequate reporting of adverse events.
Nevertheless, it is worth noting that all current evidence is very limited due to the overall “high” or “unclear” risk of bias of the included studies. Thus, the body of evidence identified cannot yet permit a robust conclusion regarding the efficacy and safety of DN for treating LBP. Large-scale, long-term RCTs with rigorous methodological input are urgently required to confirm the outcome validity of this review.
Author contributions
Data curation: Han-Tong Hu.
Formal analysis: Han-Tong Hu.
Investigation: Rui-Jie Ma.
Methodology: Hong Gao, Rui-Jie Ma.
Software: Hong-Fang Tian, Lu Li.
Supervision: Xiao-Feng Zhao.
Validation: Xiao-Feng Zhao.
Writing – original draft: Han-Tong Hu.
Writing – review and editing: Han-Tong Hu, Hong Gao, Xiao-Feng Zhao.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, DN = dry needling, LBP = low back pain, LTR = local twitch response, MTrPs = Myofascial trigger points, ODI = Oswestry disability index, RCT = randomized controlled trial, RMQ = Roland Morris disability questionnaire, RR = risk ratio, SMD = standardized mean difference, SR = systematic review, TCM = Traditional Chinese medicine, VAS = visual analogue scale.
H-TH and HG contributed equally to this work.
This project was supported by Tianjin Natural Science Foundation of China (Grant No. 17JCZDJC36700), National Natural Science Foundation of China (Grant No. 81574057), Training project of Human Resources for Health in Zhejiang Province of China (Zhejiang Health [2013] No. 245), Key Subject of traditional Chinese medicine of acupuncture ([2009] No. 30) and Project of Administration of Traditional Chinese Medicine of Zhejiang Province of China (2017ZA070).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Deyo RA, Von KM, Duhrkoop D. Opioids for low back pain. BMJ 2015;350:g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Van MM, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 2011;20:19–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kalichman L, Vulfsons S. Dry needling in the management of musculoskeletal pain. J Am Board Fam Med 2010;23:640–6. [DOI] [PubMed] [Google Scholar]
- [6].Dunning J, Butts R, Mourad F, et al. Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev 2014;19:252–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Liu L, Skinner MA, Mcdonough SM, et al. Traditional Chinese Medicine acupuncture and myofascial trigger needling: the same stimulation points? Complement Ther Med 2016;26:28–32. [DOI] [PubMed] [Google Scholar]
- [8].Tough EA, White AR, Cummings TM, et al. Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomised controlled trials. Eur J Pain 2009;13:3–10. [DOI] [PubMed] [Google Scholar]
- [9].Morihisa R, Eskew J, McNamara A, et al. Dry needling in subjects with muscular trigger points in the lower quarter: a systematic review. Int J Sports Phys Ther 2016;11:1–4. [PMC free article] [PubMed] [Google Scholar]
- [10].Kietrys DM, Palombaro KM, Azzaretto E, et al. Effectiveness of dry needling for upper-quarter myofascial pain: a systematic review and meta-analysis. J Orthop Sports Phys Ther 2013;43:620–34. [DOI] [PubMed] [Google Scholar]
- [11].Rodríguez-Mansilla J, González-Sánchez B, García áDT, et al. Effectiveness of dry needling on reducing pain intensity in patients with myofascial pain syndrome: a Meta-analysis. J Tradit Chin Med 2016;36:1–3. [DOI] [PubMed] [Google Scholar]
- [12].Liu L, Huang QM, Liu QG, et al. Evidence for dry needling in the management of myofascial trigger points associated with low back pain: A systematic review and meta-analysis. Arch Phys Med Rehabil 2017;99:144.e2–52.e2. [DOI] [PubMed] [Google Scholar]
- [13].Cummings TM, White AR. Needling therapies in the management of myofascial trigger point pain: a systematic review. Arch Phys Med Rehabil 2001;82:986–92. [DOI] [PubMed] [Google Scholar]
- [14].Garvey TA, Marks MR, Wiesel SW. A prospective, randomized, double-blind evaluation of trigger-point injection therapy for low-back pain. Spine (Phila Pa 1976) 1989;14:962–4. [DOI] [PubMed] [Google Scholar]
- [15].Wu SF. The Study Of Shallow Needles All Round Thorns Trigger Point Combined With Massage In The Treatment Of Back Myofascial Pain Syndrome [in Chinese]. Guangzhou: Guangzhou Univ Chin Med; 2014. [Google Scholar]
- [16].Nong HS. Clinical research of muscular fasciae trigger point combined with meridian point in the treatment of lumbar back myofascial pain syndrome [in Chinese]. Chin J Chin Med 2013;28:1091–2. [Google Scholar]
- [17].Fu LJ. Study on the New Method of Myofascial Pain by Acupuncture Stimulation to Ah Sih Points] [in Chinese]. Beijing: Beijing Univ Chin Med; 2011. [Google Scholar]
- [18].Jiang GM, Lin MD, Wang LY. Comparative study on effect of acupuncture and lidocaine block for lumbar myofascial pain syndrome [in Chinese]. Zhongguo Zhen Jiu 2013;33:223–6. [PubMed] [Google Scholar]
- [19].Qaseem A, Wilt TJ, Mclean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2017;166:514–30. [DOI] [PubMed] [Google Scholar]
- [20].Mahmoudzadeh A, Rezaeian ZS, Karimi A, et al. The effect of dry needling on the radiating pain in subjects with discogenic low-back pain: a randomized control trial. J Res Med Sci 2016;21:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].The Cochrane collaboration, Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0 [updated Mar 2011]. 2011. [Google Scholar]
- [22].Higgins J, Altman D, Sterne J. Chapter 8: Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0 [updated March 2011]. Cochrane Handbook System Rev Interv Vers 2011;5:187–241. [Google Scholar]
- [23].Deeks J, Higgins J, Altman D. Chapter 9–Analysing data and undertaking meta-analyses: Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011]. Cochrane Handbk System Rev Interv Vers 2011;5:235–78. [Google Scholar]
- [24].Sutton AJ, Duval SJ, Tweedie RL, et al. Empirical assessment of effect of publication bias on meta-analyses. BMJ 2000;320:1574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hirota S, Itoh K, Katsumi Y. A controlled clinical trial comparing trigger point acupuncture with tender point acupuncture treatments for chronic low back pain-a pilot study on 9 elderly patients [in Japanese]. Zen Nihon Shinkyu Gakkai Zasshi 2006;56:68–75. [Google Scholar]
- [26].Itoh K, Katsumi Y. Effect of acupuncture treatment on chronic low back pain with leg pain in aged patients: a controlled trial about short-term effects of trigger point acupuncture [in Japanese]. J Japn Acupuncture Moxibustion Soc 2005;55:530–7. [Google Scholar]
- [27].Itoh K, Katsumi Y, Hirota S, et al. Effects of trigger point acupuncture on chronic low back pain in elderly patients–a sham-controlled randomised trial. Acupunct Med 2006;24:5–12. [DOI] [PubMed] [Google Scholar]
- [28].Tellez-Garcia M, de-la-Llave-Rincon AI, Salom-Moreno J, et al. Neuroscience education in addition to trigger point dry needling for the management of patients with mechanical chronic low back pain: a preliminary clinical trial. J Bodyw Mov Ther 2015;19:464–72. [DOI] [PubMed] [Google Scholar]
- [29].Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients–a blinded RCT. Acupunct Med 2004;22:170–7. [DOI] [PubMed] [Google Scholar]
- [30].Chen Z. Study on the Super Laser Therapy on Trigger Points for Low Back Myofascial Pain Syndrome [in Chinese]. Guangzhou: Guangzhou Univ Chin Med; 2014. [Google Scholar]
- [31].Yang XC, Zhou YM. Clinical observation of effectiveness in the treatment of myofascial pain syndrome in the lower back with intramuscular stimulation therapy [in Chinese]. Chin J Rural Med Pharm 2010;17:44–5. [Google Scholar]
- [32].Shen CG, Ding JM. Clinical observation of effectiveness in the treatment of lumbar disc herniation with intramuscular stimulation therapy 30 cases reports [in Chinese]. Zhejiang J Tradit Chin Med 2015;50:676. [Google Scholar]
- [33].Kuang JF. A Research on Acupuncture at Trigger Points Treatment for Chronic Low Back Myofascial Pain Syndrome [in Chinese]. Guangzhou: Guangzhou Univ Chin Med; 2013. [Google Scholar]
- [34].Long JJ, Zhuang XQ, Tan SS, et al. Clinical observation of needling of myofascial trigger points and acupoints for myofascial pain syndrome in the lower back [in Chinese]. J Guangxi Univ Chin Med 2012;15:17–9. [Google Scholar]
- [35].Hong CZ, Simons DG. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch Phys Med Rehabil 1998;79:863–72. [DOI] [PubMed] [Google Scholar]
- [36].Williams & Wilkins, Simons DG, Travell JG, Simons LS. Travell & Simons’ Myofascial Pain and Dysfunction: the Trigger Point Manual. 1999. [Google Scholar]
- [37].JGb T, Simons D. Myofascial Pain and Dysfunction: The Trigger Point Manual. 1983;Baltimore: Williams and Wilkins, 308–328. [Google Scholar]
- [38].Zhou K, Ma Y, Brogan MS. Dry needling versus acupuncture: the ongoing debate. Acupunct Med 2015;33:485–90. [DOI] [PubMed] [Google Scholar]
- [39].Fan AY, He H. Dry needling is acupuncture. Acupunct Med 2016;34:241. [DOI] [PubMed] [Google Scholar]
- [40].Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain 1977;3:3–23. [DOI] [PubMed] [Google Scholar]
- [41].Stephen B. Trigger point--acupuncture point correlations revisited. J Altern Complement Med 2003;9:91–103. [DOI] [PubMed] [Google Scholar]
- [42].He W, Zhu B, Yu X, et al. Comparison between western and Chinese acupuncture and its enlightenment [in Chinese]. Chin Acupunct Moxibustion 2015; 35: 105–108. [PubMed] [Google Scholar]
- [43].Dunning J, Butts R, Mourad F, et al. Dry needling: a literature review with implications for clinical practice guidelines. Phy Ther Rev 2014;19:252–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Dommerholt J, Mayoral del Moral O, Gröbli C. Trigger point dry needling. J Man Manip Ther 2006;14:70E–87E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Dommerholt J. Trigger Point Dry Needling, An Evidence and Clinical-Based Approach. 1st ed.New York: Churchill Livingstone Press; 2013. [Google Scholar]
- [46].Hong CZ, Torigoe Y. Electrophysiological characteristics of localized twitch responses in responsive taut bands of rabbit skeletal muscle fibers. J Musculoskeletal Pain 1994;2:17–43. [Google Scholar]
- [47].Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil 1994;73:256–63. [DOI] [PubMed] [Google Scholar]
- [48].Moher SDD. Consolidated standards for reporting trials of traditional Chinese Medicine (CONSORT for TCM). Chin J Evid Based Med 2007;7:625–30. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


