Abstract
Background:
The quality-adjusted life year (QALY) is the preferred outcome measurement for cost-effectiveness analysis in health care. QALYs measure patient health-related quality of life with use of a value between 0 and 1. Few studies have provided original data delineating QALYs after hip and knee arthroplasty. In the present study, we evaluated patient utility preoperatively and 2 years after total hip arthroplasty, hip resurfacing, revision hip arthroplasty, total knee arthroplasty, unicompartmental knee arthroplasty, and revision knee arthroplasty.
Methods:
A single-hospital joint registry, which enrolled patients from 2007 to 2011, was retrospectively examined for all patients who underwent primary or revision hip or knee arthroplasty and who had preoperative and 2-year postoperative Short Form-36 (SF-36), Short Form-12 (SF-12), or EuroQol 5-Dimension (EQ-5D) scores available. Patient age, body mass index (BMI), sex, American Society of Anesthesiologists (ASA) score, and Charlson Comorbidity Index were recorded. QALYs were determined from the EQ-5D index and the Short Form-6 Dimension (SF-6D) index.
Results:
Five thousand, four hundred and sixty-three patients underwent total hip arthroplasty, with a mean annual increase (and standard deviation) of 0.25 ± 0.2 QALY; 843 patients underwent hip resurfacing, with a mean annual increase of 0.24 ± 0.17 QALY; 5,398 patients underwent primary total knee arthroplasty, with a mean annual increase of 0.17 ± 0.19 QALY; and 240 patients underwent medial unicompartmental knee arthroplasty, with a mean annual increase of 0.16 ± 0.17 QALY. Aseptic revision arthroplasty (440 hips, 323 knees) was associated with a smaller QALY gain than primary arthroplasty. Patient age, BMI, female sex, ASA category, and higher preoperative health-related quality of life were negative predictors for QALY gain after primary arthroplasty. Forty additional hip procedures and 35 additional knee procedures were also analyzed.
Conclusions:
Primary hip and knee arthroplasty, on average, result in substantially increased patient quality of life. Revision hip and knee replacement result in a lower, but still positive, gain in quality of life. However, there is a considerable variation in patient outcomes across all procedures. Our results may be used to improve the certainty of future cost-effectiveness analyses of hip and knee arthroplasty.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Primary total hip arthroplasty and total knee arthroplasty are safe and effective procedures for patients with end-stage osteoarthritis1. New techniques and technologies have been developed to improve the outcomes of total hip arthroplasty and total knee arthroplasty, including renewed interest in the direct anterior hip approach2, dual-mobility hip implants3, patient-specific instrumentation and implants4, and robotic and computer-assisted navigation5-8. While such technologies may potentially improve outcomes, they add expense to these procedures. As health-care costs continue to rise, an emphasis on value-based care necessitates that new technologies be considered not only for their clinical effectiveness but also for their cost effectiveness9.
The quality-adjusted life year (QALY) is the preferred outcome measurement for cost-effectiveness analysis in health care according to the U.S. Panel on Cost-Effectiveness in Health and Medicine10. QALYs are a generic measurement of health-related quality of life as defined on a 0 to 1 scale; a year of perfect health is worth 1 QALY, and a year of less-than-perfect health is worth <1. QALYs are a measure of patient utility and can be determined with use of the EuroQol 5-Dimension (EQ-5D), Short Form 6-Dimension (SF-6D), and Health Utility Index (HUI) questionnaires11.
To our knowledge, no recent studies have comprehensively provided patient utility outcomes after both primary and revision hip and knee arthroplasty. Several studies have provided information on QALY gains after primary total hip arthroplasty12-15 and primary total knee arthroplasty13,14,16. However, those studies included small numbers of patients and did not delineate QALY outcomes after numerous other hip and knee reconstruction procedures such as revision surgery, hip resurfacing, and partial knee arthroplasty. Furthermore, it is not known what factors predict the changes in patient utility after joint replacement.
The goal of the present study was to comprehensively determine patient health-related quality of life after hip and knee replacement as assessed with the EQ-5D and SF-6D instruments. For hip arthroplasty, we examined primary total hip arthroplasty, hip resurfacing, aseptic revision total hip arthroplasty, septic revision total hip arthroplasty, conversion of prior hemiarthroplasty to total hip arthroplasty, and conversion of prior hip resurfacing to total hip arthroplasty. For knee arthroplasty, we examined primary total knee arthroplasty, medial unicompartmental knee arthroplasty, aseptic revision total knee arthroplasty, septic revision total knee arthroplasty, conversion of unicompartmental knee arthroplasty to total knee arthroplasty, and patellofemoral replacement. Furthermore, we examined patient-related factors that predict the gain in patient utility after joint replacement.
Materials and Methods
Patients
We conducted a retrospective review of patients who had been prospectively enrolled in our institution’s institutional review board-approved joint database from May 2007 to December 2011. The present study included all patients who had available preoperative and 2-year postoperative EQ-5D, SF-36, or SF-12 data who had undergone primary total hip arthroplasty, hip resurfacing, aseptic revision total hip arthroplasty, septic revision total hip arthroplasty, conversion of prior hemiarthroplasty to total hip arthroplasty, conversion of prior hip resurfacing to total hip arthroplasty, primary total knee arthroplasty, medial unicompartmental knee arthroplasty, aseptic revision total knee arthroplasty, septic revision total knee arthroplasty, conversion of unicompartmental knee arthroplasty to total knee arthroplasty, or patellofemoral replacement. Age, sex, body mass index (BMI), the Charlson Comorbidity Index (CCI), the American Society of Anesthesiologists (ASA) score, and the preoperative diagnosis were recorded for each patient. The patient characteristics for select procedures are summarized in Table I. Patients were excluded if no scores were available for any of the 3 instruments (EQ-5D, SF-36, and SF-12).
TABLE I.
Patient Characteristics for Hip and Knee Procedures*
| Hip |
Knee |
|||||
| Primary Total Hip Arthroplasty | Hip Resurfacing | Aseptic Revision Total Hip Arthroplasty | Primary Total Knee Arthroplasty | Unicompartmental Knee Arthroplasty | Aseptic Revision Total Knee Arthroplasty | |
| No. of patients† | 5,463 | 843 | 440 | 5,398 | 240 | 323 |
| Age‡ (yr) | 64.2 ± 11.5 | 51.2 ± 7.6 | 66.4 ± 12.3 | 66.9 ± 9.5 | 63.7 ± 10.2 | 65.3 ± 10.7 |
| Sex | 55.6% female, 44.4% male | 21.5% female, 78.5% male | 50.0% female, 50.0% male | 61.2% female, 38.8% male | 60.4% female, 39.6% male | 48.3% female, 51.7% male |
| BMI‡ (kg/m2) | 27.7 ± 5.5 | 27.3 ± 4.4 | 27.3 ± 5.4 | 30.1 ± 6.1 | 28.8 ± 4.9 | 30.3 ± 6.2 |
| CCI‡ | 0.36 ± 0.92 | 0.12 ± 0.47 | 0.46 ± 0.97 | 0.44 ± 0.95 | 0.4 ± 0.84 | 0.48 ± 0.83 |
| ASA score§ | ||||||
| 1 or 2 | 4,496 (82.3%) | 816 (96.8%) | 310 (70.5%) | 4,280 (79.3%) | 208 (86.7%) | 234 (72.4%) |
| 3 or 4 | 967 (17.7%) | 27 (3.2%) | 130 (29.5%) | 1,118 (20.7%) | 32 (13.3%) | 89 (27.6%) |
| Diagnosis# | Osteoarthritis (5,163; 94.5%), inflammatory arthritis (54; 1%), other (246; 4.5%) | Osteoarthritis (816; 96.8%), inflammatory arthritis (1; 0.1%), other (25; 3%) | Aseptic failure (440; 100%) | Osteoarthritis (5,192; 96.2%), inflammatory arthritis (64; 1.2%), other (142; 2.6%) | Osteoarthritis (231; 96.3%), inflammatory arthritis (0; 0%), other (9; 3.8%) | Aseptic failure (323; 100%) |
BMI = body mass index, CCI = Charlson Comorbidity Index, and ASA = American Society of Anesthesiologists.
Number of patients with preoperative EQ-5D, SF-36, and/or SF-12 scores available.
The values are given as the mean and the standard deviation.
The values are given as the number of patients, with the percentage in parentheses.
The number and percentage of patients with each diagnosis are shown in parentheses.
EQ-5D
The EQ-5D health questionnaire17 includes 5 domains: mobility, self-care, usual activities, pain or discomfort, and anxiety or depression. Responses have 3 levels of severity, ranging from no problems to extreme problems. This instrument allows for 243 health states, which are correlated with utility values from a sample United States population with use of time-tradeoff methods. The utility values for each health state are scored between 0 and 1.
SF-6D
The SF-6D utility score, which is derived from the SF-36 and SF-12 scoring systems, includes 6 categories: vitality, pain, mental health, social functioning, physical functioning, and role limitations. Each category is scored by severity level. Different answers produce a large number of possible health states. Each health state is correlated with an index utility score of between 0 and 1, with 0 representing death and 1 representing full health, by applying a weighting specific for the United States that is based on a standard gamble technique11. All SF-36 or SF-12 scores were converted into SF-6D index scores.
Statistical Analysis
For all procedures with available data for >100 patients, we utilized multivariate linear regression to analyze the effect of patient-related factors on the predicted change in QALYs from the preoperative baseline to 2 years postoperatively. These procedures included primary total hip arthroplasty, hip resurfacing, aseptic revision total hip arthroplasty, primary total knee arthroplasty, unicompartmental knee arthroplasty, and aseptic revision total knee arthroplasty. Explanatory variables were patient age, sex, BMI, ASA score, CCI, preoperative utility, and diagnosis.
Results
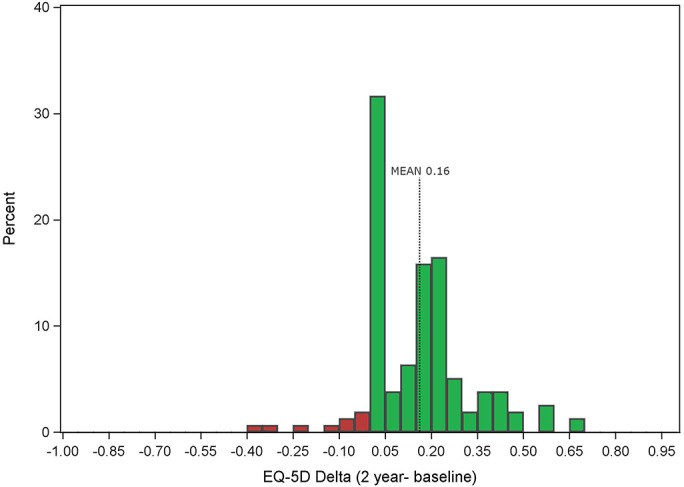
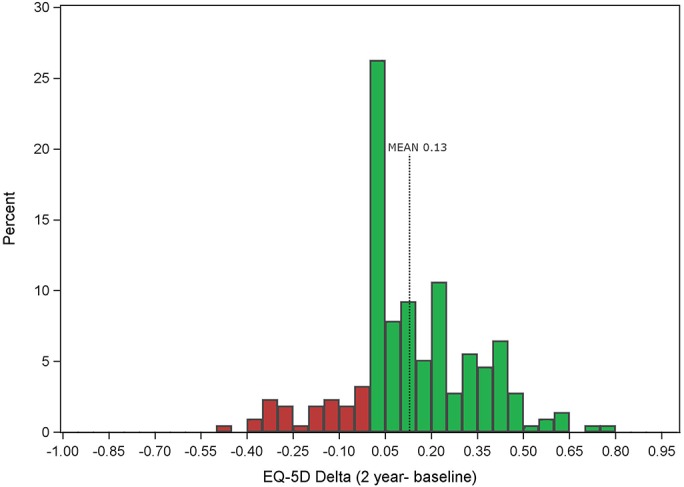
Six thousand, seven hundred and eighty-six patients were analyzed after hip arthroplasty procedures, including primary total hip arthroplasty (5,463 patients; 80.5%), hip resurfacing (843 patients; 12.4%), aseptic revision total hip arthroplasty (440 patients; 6.5%), septic revision total hip arthroplasty (4 patients; 0.06%), conversion of hemiarthroplasty to total hip arthroplasty (24 patients; 0.4%), and conversion of hip resurfacing to total hip arthroplasty (12 patients; 0.2%). Five thousand, nine hundred and ninety-six patients underwent knee arthroplasty procedures, including primary total knee arthroplasty (5,398 patients; 90.0%), medial unicompartmental knee arthroplasty (240 patients; 4.0%), aseptic revision total knee arthroplasty (323 patients; 5.4%), septic revision total knee arthroplasty (6 patients; 0.1%), conversion of prior unicompartmental knee arthroplasty to total knee arthroplasty (15 patients; 0.25%), and patellofemoral replacement (14 patients; 0.23%). Patient characteristics by procedure are summarized in Table I. Annual gain in QALYs after surgery are summarized in Figures 1-A through 2-C.
Figs. 1-A, 1-B, and 1-C Changes in annual QALYs (as measured with the EQ-5D questionnaire) 2 years after hip procedures. The blue bars represent QALY gains, and the red bars represent QALY losses.
Fig. 1-A.
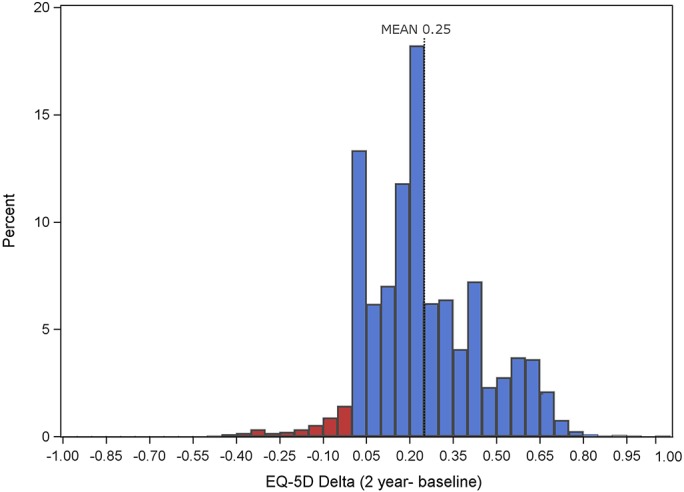
QALY gains and losses after total hip arthroplasty.
Fig. 1-B.
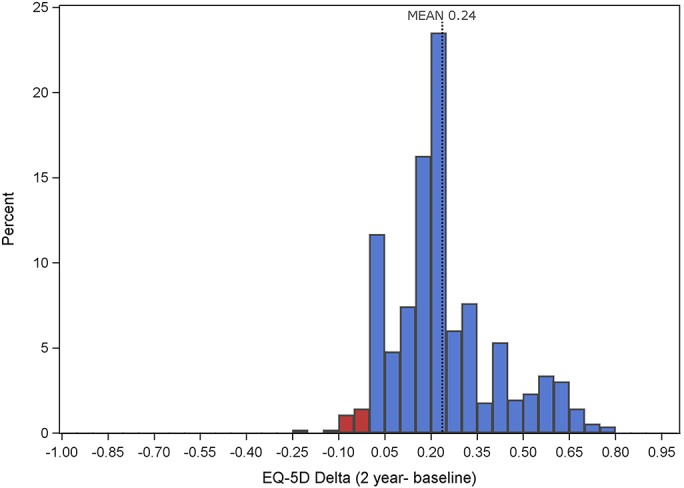
QALY gains and losses after hip resurfacing.
Fig. 1-C.
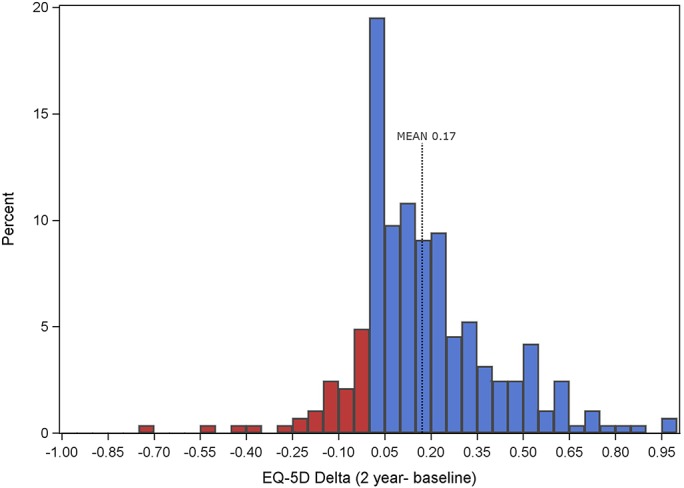
QALY Gains and losses after aseptic revision total hip arthroplasty.
Figs. 2-A, 2-B, and 2-C Changes in annual QALYs (as measured with the EQ-5D questionnaire) 2 years after knee procedures. The green bars represent QALY gains, and the red bars represent QALY losses.
Fig. 2-A.
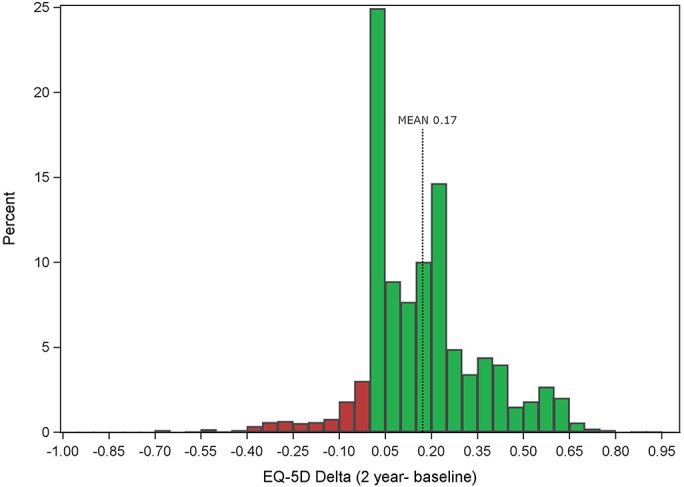
QALY gains and losses after total knee arthroplasty.
Fig. 2-B.
QALY gains and losses after medial unicompartmental knee arthroplasty.
Fig. 2-C.
QALY gains and losses after aseptic revision total knee arthroplasty.
Primary Total Hip Arthroplasty
Table II summarizes the change in utility after hip arthroplasty. Three thousand, four hundred and fifty-three patients who underwent primary total hip arthroplasty had a mean 2-year postoperative increase in the EQ-5D score (and standard deviation) of 0.25 ± 0.2. Four thousand, eight hundred and thirty-four patients who underwent primary total hip arthroplasty had a 2-year postoperative increase in the SF-6D score of 0.18 ± 0.13. Three thousand, six hundred and one patients who underwent primary total hip arthroplasty had a 5-year postoperative increase in the SF-6D score of 0.2 ± 0.13. For primary total hip arthroplasty, the variables of age, sex, BMI, ASA score, and preoperative utility as measured with the EQ-5D index were all significant predictors of annual QALY gain (p < 0.0001 for all) and collectively predicted 58.8% of the variation in patient outcomes (Table III). Higher age, BMI, ASA score, and CCI were all associated with a slightly lower QALY gain. A moderately higher QALY gain was associated with male sex. The strongest predictor of QALY gain was a lower baseline preoperative quality of life; the lower the preoperative annual QALY, the higher the expected postoperative QALY gain.
TABLE II.
Utility Changes After Hip Arthroplasty Procedures
| EQ-5D |
SF-6D |
||||||||||
| Preop. | 2-Yr Postop. | P Value (2-Yr vs. Preop.) | 2-Yr Change | Preop. | 2-Yr Postop. | P Value (2-Yr vs. Preop.) | 5-Yr Postop. | P Value (5-Yr vs Preop.) | 2-Yr Change | 5-Yr Change | |
| Primary total hip arthroplasty | |||||||||||
| No. of patients | 5,353 | 3,514 | 3,453 | 5,154 | 5,076 | 3,785 | 4,834 | 3,601 | |||
| Score* | 0.63 ± 0.19 | 0.88 ± 0.14 | <0.0001 | 0.25 ± 0.20 | 0.6 ± 0.11 | 0.79 ± 0.13 | <0.0001 | 0.81 ± 0.13 | <0.0001 | 0.18 ± 0.13 | 0.2 ± 0.13 |
| Hip resurfacing | |||||||||||
| No. of patients | 829 | 576 | 566 | 807 | 814 | 637 | 782 | 611 | |||
| Score* | 0.68 ± 0.16 | 0.93 ± 0.11 | <0.0001 | 0.24 ± 0.17 | 0.63 ±0.10 | 0.82 ± 0.12 | <0.0001 | 0.84 ± 0.12 | <0.0001 | 0.19 ± 0.13 | 0.21 ± 0.12 |
| Aseptic revision total hip arthroplasty | |||||||||||
| No. of patients | 434 | 292 | 287 | 411 | 399 | 268 | 380 | 254 | |||
| Score* | 0.63 ± 0.22 | 0.8 ± 0.17 | <0.0001 | 0.17 ± 0.23 | 0.6 ± 0.12 | 0.72 ± 0.14 | <0.0001 | 0.74 ± 0.15 | <0.0001 | 0.12 ± 0.14 | 0.14 ± 0.15 |
| Septic revision total hip arthroplasty | |||||||||||
| No. of patients | 3 | 4 | 3 | 3 | 3 | 2 | 2 | 1 | |||
| Score* | 0.58 ± 0.35 | 0.72 ± 0.19 | 0.52 | 0.13 ± 0.51 | 0.64 ± 0.03 | 0.69 ± 0.05 | 0.21 | 0.62 ± 0.05 | 0.60 | 0.04 ± 0.03 | 0.04 |
| Conversion of hemiarthroplasty to total hip arthroplasty | |||||||||||
| No. of patients | 23 | 18 | 17 | 23 | 24 | 13 | 23 | 13 | |||
| Score* | 0.64 ± 0.15 | 0.78 ± 0.18 | 0.0098 | 0.13 ± 0.18 | 0.63 ± 0.11 | 0.71 ± 0.12 | 0.022 | 0.75 ± 0.13 | 0.0058 | 0.09 ± 0.1 | 0.09 ± 0.13 |
| Conversion of hip resurfacing to total hip arthroplasty | |||||||||||
| No. of patients | 12 | 5 | 5 | 11 | 12 | 9 | 11 | 8 | |||
| Score* | 0.67 ± 0.18 | 0.93 ± 0.1 | 0.0089 | 0.18 ± 0.13 | 0.59 ± 0.10 | 0.74 ± 0.16 | 0.015 | 0.79 ± 0.17 | 0.0042 | 0.13 ± 0.13 | 0.16 ± 0.11 |
The scores are given as the mean and the standard deviation. The p values were determined with use of the Student t test.
TABLE III.
| Primary Total Hip Arthroplasty |
Hip Resurfacing |
Aseptic Revision Total Hip Arthroplasty |
||||
| Parameter | Coefficient and Standard Deviation | P Value | Coefficient and Standard Deviation | P Value | Coefficient and Standard Deviation | P Value |
| Intercept‡ | 0.898 ± 0.020 | <0.0001 | 0.793 ± 0.044 | <0.0001 | 0.605 ± 0.075 | <0.0001 |
| Age | −0.001 ± 0.0002 | <0.00001 | 0.001 ± 0.001 | 0.199 | 0.001 ± 0.001 | 0.485 |
| BMI | −0.002 ± 0.0004 | <0.0001 | −0.001 ± 0.001 | 0.585 | 0.0002 ± 0.002 | 0.902 |
| CCI | −0.004 ± 0.002 | 0.056 | 0.010 ± 0.009 | 0.304 | −0.005 ± 0.010 | 0.613 |
| Sex (male vs. female) | 0.025 ± 0.005 | <0.0001 | 0.020 ± 0.011 | 0.068 | 0.045 ± 0.019 | 0.021 |
| ASA score (3 or 4 vs. 1 or 2) | −0.030 ± 0.006 | <0.0001 | −0.081 ± 0.023 | 0.001 | −0.020 ± 0.023 | 0.374 |
| Preoperative EQ-5D index score | −0.812 ± 0.012 | <0.0001 | −0.860 ± 0.028 | <0.0001 | −0.771 ± 0.044 | <0.0001 |
The outcome variable was defined as the change from the baseline preoperative EQ-5D index score to the 2-year postoperative EQ-5D index score. BMI = body mass index, CCI = Charlson Comorbidity Index, and ASA = American Society of Anesthesiologists.
R2 = 0.588 for primary total hip arthroplasty, 0.639 for hip resurfacing, and 0.523 for aseptic revision total hip arthroplasty.
The intercept is the expected value when all of the values in the regression model are set to 0.
Hip Resurfacing
Five hundred and sixty-six patients who underwent hip resurfacing had a 2-year postoperative increase in the EQ-5D score of 0.24 ± 0.17. Seven hundred and eighty-two patients who underwent hip resurfacing had a 2-year increase in the SF-6D score of 0.19 ± 0.13. Six hundred and eleven patients who underwent hip resurfacing had a 5-year increase in the SF-6D score of 0.21 ± 0.12. There were no statistically significant differences in annual QALY gain as measured with the EQ-5D or SF-6D index when primary total hip arthroplasty was compared with hip resurfacing (p = 0.638, p = 0.507). The ASA score (p = 0.001) and preoperative baseline utility scores as measured with the EQ-5D index (p < 0.0001) were predictive of QALY gain after hip resurfacing; these 2 variables explained 63.9% of the variation in QALY gain (Table III). A lower preoperative utility score was associated with a higher postoperative annual QALY gain.
Aseptic Revision Total Hip Arthroplasty
Two hundred and eighty-seven patients who underwent aseptic revision total hip arthroplasty had a 2-year postoperative increase in the EQ-5D score of 0.17 ± 0.23. This increase was significantly lower than the EQ-5D utility gained after primary total hip arthroplasty (p < 0.0001). Three hundred and eighty patients who underwent aseptic revision total hip arthroplasty had a 2-year gain in the SF-6D score of 0.12 ± 0.14. Likewise, this increase was significantly lower than the SF-6D utility gained after primary total hip arthroplasty after 2 years (p < 0.0001). Two hundred and fifty-four patients demonstrated a 5-year postoperative increase in the SF-6D score of 0.14 ± 0.15, which was also significantly lower than the corresponding 5-year outcome after primary total hip arthroplasty (p < 0.0001). Patient sex (p = 0.021) and preoperative utility (p < 0.0001) explained 52.3% of the variation in annual QALY gain after revision total hip arthroplasty (Table III).
Additional Hip Procedures
Fewer patients had complete utility scores available after conversion of hemiarthroplasty to total hip arthroplasty (17 patients), conversion of hip resurfacing to total hip arthroplasty (5 patients), and septic revision total hip arthroplasty (3 patients). Utilities for these patients are summarized in Table II.
Primary Total Knee Arthroplasty
Table IV summarizes the change in utility after knee arthroplasty. Three thousand, three hundred and nine patients who underwent total knee arthroplasty had a 2-year postoperative increase in the ED-5D score of 0.17 ± 0.19. Four thousand, eight hundred and fifty-one patients who underwent primary total knee arthroplasty had a 2-year postoperative increase in the SF-6D score of 0.14 ± 0.13. Three thousand, three hundred and fifty-four patients who underwent primary total knee arthroplasty had a 5-year postoperative increase in the SF-6D score of 0.15 ± 0.13. Patient BMI, CCI, sex, ASA score, and preoperative baseline utility as measured with the EQ-5D index were all significant predictors of 2-year postoperative utility gain (Table V). Together, these factors explained 44.6% of the variation in utility gain after primary total knee arthroplasty. The strongest predictor of utility gain was preoperative baseline utility.
TABLE IV.
Utility Changes After Knee Arthroplasty Procedures
| EQ-5D |
SF-6D |
||||||||||
| Preop. | 2-Yr Postop. | P Value (2-Yr vs. Preop.) | 2-Yr Change | Preop. | 2-Yr Postop. | P Value (2-Yr vs. Preop.) | 5-Yr Postop. | P Value (5-Yr vs. Preop.) | 2-Yr Change | 5-Yr Change | |
| Primary total knee arthroplasty | |||||||||||
| No. of patients | 5,282 | 3,379 | 3,309 | 5,127 | 5,064 | 3,509 | 4,851 | 3,354 | |||
| Score* | 0.68 ± 0.17 | 0.84 ± 0.15 | <0.0001 | 0.17 ± 0.19 | 0.63 ± 0.11 | 0.76 ± 0.13 | <0.0001 | 0.79 ± 0.13 | <0.0001 | 0.14 ± 0.13 | 0.15 ± 0.13 |
| Unicompartmental knee arthroplasty | |||||||||||
| No. of patients | 235 | 160 | 158 | 232 | 233 | 162 | 226 | 159 | |||
| Score* | 0.71 ± 0.14 | 0.87 ± 0.13 | <0.0001 | 0.16 ± 0.17 | 0.65 ± 0.11 | 0.8 ± 0.13 | <0.0001 | 0.8 ± 0.14 | <0.0001 | 0.15 ± 0.12 | 0.15 ± 0.12 |
| Aseptic revision total knee arthroplasty | |||||||||||
| No. of patients | 312 | 225 | 217 | 301 | 307 | 197 | 288 | 186 | |||
| Score* | 0.61 ± 0.2 | 0.74 ± 0.18 | <0.0001 | 0.13 ± 0.21 | 0.59 ± 0.11 | 0.69 ± 0.14 | <0.0001 | 0.72 ± 0.14 | <0.0001 | 0.1 ± 0.13 | 0.13 ± 0.14 |
| Septic revision total knee arthroplasty | |||||||||||
| No. of patients | 6 | 5 | 5 | 5 | 6 | 2 | 5 | 2 | |||
| Score* | 0.5 ± 0.3 | 0.71 ± 0.22 | 0.23 | 0.28 ± 0.21 | 0.51 ± 0.14 | 0.65 ± 0.16 | 0.16 | 0.69 ± 0.24 | 0.25 | 0.14 ± 0.12 | 0.15 ± 0.03 |
| Conversion of unicompartmental knee arthroplasty to total knee arthroplasty | |||||||||||
| No. of patients | 15 | 8 | 8 | 15 | 15 | 12 | 15 | 12 | |||
| Score* | 0.69 ± 0.14 | 0.82 ± 0.08 | 0.025 | 0.08 ± 0.13 | 0.62 ± 0.1 | 0.71 ± 0.1 | 0.02 | 0.78 ± 0.14 | 0.002 | 0.09 ± 0.12 | 0.15 ± 0.16 |
| Patellofemoral arthroplasty | |||||||||||
| No. of patients | 14 | 8 | 8 | 14 | 14 | 12 | 14 | 12 | |||
| Score* | 0.66 ± 0.18 | 0.85 ± 0.1 | 0.013 | 0.08 ± 0.09 | 0.62 ± 0.09 | 0.76 ± 0.14 | 0.004 | 0.78 ± 0.1 | 0.0003 | 0.13 ± 0.15 | 0.14 ± 0.1 |
The scores are given as the mean and the standard deviation. The p values were determined with use of the Student t test.
TABLE V.
| Primary Total Knee Arthroplasty |
Unicompartmental Knee Arthroplasty |
Aseptic Revision Total Knee Arthroplasty |
||||
| Parameter | Coefficient and Standard Deviation | P Value | Coefficient and Standard Deviation | P Value | Coefficient and Standard Deviation | P Value |
| Intercept‡ | 0.749 ± 0.026 | <0.0001 | 0.695 ± 0.101 | <0.0001 | 0.494 ± 0.096 | <0.0001 |
| Age | −0.001 ± 0.0003 | 0.051 | 0.000 ± 0.001 | 0.986 | 0.003 ± 0.001 | 0.002 |
| BMI | −0.001 ± 0.0004 | 0.008 | 0.000 ± 0.002 | 0.843 | −0.004 ± 0.002 | 0.047 |
| CCI | −0.006 ± 0.003 | 0.023 | 0.012 ± 0.012 | 0.341 | −0.020 ± 0.013 | 0.115 |
| Sex (male vs. female) | 0.027 ± 0.005 | <0.0001 | 0.032 ± 0.021 | 0.124 | 0.034 ± 0.022 | 0.126 |
| ASA score (3 or 4 vs. 1 or 2) | −0.044 ± 0.006 | <0.0001 | −0.022 ± 0.029 | 0.440 | −0.097 ± 0.025 | 0.0001 |
| Preoperative EQ-5D index score | −0.753 ± 0.015 | <0.0001 | −0.802 ± 0.070 | <0.0001 | −0.718 ± 0.056 | <0.0001 |
The outcome variable was defined as the change from the baseline preoperative EQ-5D index score to the 2-year postoperative EQ-5D index score. BMI = body mass index, CCI = Charlson Comorbidity Index, and ASA = American Society of Anesthesiologists.
R2 = 0.446 for primary total knee arthroplasty, 0.467 for unicompartmental knee arthroplasty, and 0.454 for aseptic revision total knee arthroplasty.
The intercept is the expected value when all of the values in the regression model are set to 0.
Unicompartmental Knee Arthroplasty
One hundred and fifty-eight patients who underwent medial compartment unicompartmental knee arthroplasty had a mean 2-year increase in the ED-5D score of 0.16 ± 0.17; this increase was not significantly different from that following primary total knee arthroplasty (p = 0.814). Two hundred and twenty-six patients who underwent unicompartmental knee arthroplasty had a 2-year increase in the SF-6D score of 0.15 ± 0.12, whereas 159 patients demonstrated a 5-year increase of 0.15 ± 0.12. Neither value was statistically different from the corresponding value following primary total knee arthroplasty. Only preoperative baseline utility as measured by the EQ-5D index was predictive of 2-year utility gain after unicompartmental knee arthroplasty (p < 0.0001); this factor explained 46.7% of the variability in the utility gain after surgery (Table V).
Aseptic Revision Total Knee Arthroplasty
Two hundred and seventeen patients who underwent aseptic revision total knee arthroplasty had a 2-year increase in the EQ-5D score of 0.13 ± 0.21. Two hundred and eighty-eight patients had a 2-year increase in the SF-6D score of 0.1 ± 0.13, and 186 patients had a 5-year increase in the SF-6D score of 0.13 ± 0.14. In all cases, postoperative utility gain was significantly lower after aseptic revision total knee arthroplasty than after primary total knee arthroplasty (p < 0.0001). Age, BMI, ASA score, and preoperative utility as measured by the EQ-5D index were all significant predictors of 2-year utility gain after aseptic revision total knee arthroplasty; these factors explained 45.4% of the variation in utility gain after aseptic revision total knee arthroplasty (Table V).
Additional Knee Procedures
Fewer patients had complete utility scores available after conversion of unicompartmental knee arthroplasty to total knee arthroplasty (8 patients), patellofemoral replacement (8 patients), and septic revision total knee arthroplasty (5 patients). Utilities associated with these procedures are summarized in Table IV.
Discussion
The present study summarizes preoperative and postoperative health-related quality of life in terms of annual QALYs gained after hip and knee arthroplasty. Our results demonstrated that hip and knee osteoarthritis had a negative impact on health-related quality of life comparable to that of major medical conditions18-21 (Table VI). Both hip and knee arthroplasty resulted in a large increase in quality of life as measured in QALYs with use of either the EQ-5D or the SF-6D instrument. After primary arthroplasty, the average patient health-related quality of life was similar to values in the literature for healthy patients without osteoarthritis (Table VI).
TABLE VI.
Comparison of Health-Related Quality of Life for Different Health States
| Health State | QALY | Source |
| Healthy, age 55-59 yr | 0.906 | Kwon et al.19 (2016) |
| Healthy, age 60-64 yr | 0.885 | Kwon et al.19 (2016) |
| Healthy, age 65-69 yr | 0.837 | Kwon et al.19 (2016) |
| Healthy, age 70-74 yr | 0.807 | Kwon et al.19 (2016) |
| 5 yr after primary total hip arthroplasty* | 0.81 | Current study |
| 5 yr after primary total knee arthroplasty* | 0.79 | Current study |
| Minor stroke | 0.73 | Luengo-Fernandez et al.18 (2013) |
| Venous thromboembolism | 0.697 | Kwon et al.19 (2016) |
| Knee osteoarthritis* | 0.63 | Current study |
| Hip osteoarthritis* | 0.6 | Current study |
| Acute myocardial infarction | 0.54 | Soto et al.20 (2016) |
| Hip fracture | 0.535 | Kwon et al.19 (2016) |
| Moderate stroke | 0.56 | Luengo-Fernandez et al.18 (2013) |
| Metastatic lung cancer | 0.53 | Doble et al.21 (2017) |
| Severe stroke | 0.38 | Luengo-Fernandez et al.18 (2013) |
Values reported with use of the SF-6D.
We found no differences in annual QALY gain between primary total hip arthroplasty and hip resurfacing. Similarly, we found no difference between utility gain after primary total knee arthroplasty and unicompartmental knee arthroplasty. Total hip arthroplasty resulted in greater utility gain than total knee arthroplasty. Revision hip and knee replacement resulted in a positive gain in annual QALYs, although the gain was lower than that after primary surgery.
We observed considerable variation in quality-of-life outcomes. Higher preoperative QALYs were consistently the strongest negative predictor of postoperative QALY gain after total hip arthroplasty, hip resurfacing, aseptic revision total hip arthroplasty, total knee arthroplasty, unicompartmental knee arthroplasty, and aseptic revision total knee arthroplasty. This finding is intuitive: patients who have the lowest preoperative quality of life will potentially benefit the most from surgical intervention, whereas those with mild symptoms can expect small or even negative changes in their quality of life.
Recently reported utility gains after primary total hip arthroplasty have ranged from 0.166 to 0.358 (Table VII)12-15. For total hip arthroplasty, our study demonstrated an annual QALY gain of 0.25 for 3,453 patients with use of the EQ-5D index and a gain of 0.18 for 4,834 patients with use of the SF-6D index. Utility changes after primary total knee arthroplasty also have been described13,14,16, with gains ranging from 0.125 to 0.267 (Table VIII). For primary total knee arthroplasty, we found an annual QALY gain of 0.17 for 3,309 patients with use of the EQ-5D index and a gain of 0.14 for 4,851 patients with use of the SF-6D index. Whereas the aforementioned studies involved the use of either the EQ-5D or the SF-6D index, our study involved the use of both instruments to determine utility gain. To our knowledge, the present report describes the largest study on QALY changes after primary hip and knee replacements in the United States. Additionally, to our knowledge, our study provides the first recent report on utility outcomes after hip resurfacings, unicompartmental knee replacements, and aseptic revision hip and knee replacements in a large number of patients.
TABLE VII.
Comparison of Quality-of-Life Changes After Primary Total Hip Arthroplasty*
| Preop. |
2-Yr Postop. |
||||||
| Population | Instrument | No. of Patients | QALY and Standard Deviation | No. of Patients | QALY and Standard Deviation | Change in QALY | |
| Elmallah et al.12 (2017) | United States | SF-6D | 194 | 0.614 ± 0.131 | 182 | 0.77 ± 0.14 | 0.185 |
| Liebs et al.13 (2016) | |||||||
| Early aquatic cohort | Germany | SF-6D | 129 | 0.556 ± 0.098 | 100 | 0.73 ± 0.146 | 0.164 |
| Late aquatic cohort | Germany | SF-6D | 141 | 0.554 ± 0.105 | 110 | 0.744 ± 0.122 | 0.181 |
| Jenkins et al.14 (2013) | United Kingdom | EQ-5D | 348 | 0.323 ± 0.32 | NR† | 0.721 ± 0.255 | 0.358 |
| Fordham et al.15 (2012) | United Kingdom | SF-6D | 938 | 0.537 ± 0.113 | 728 | 0.709 ± 0.159 | 0.166 |
| Current study | |||||||
| EQ-5D cohort | United States | EQ-5D | 5,353 | 0.63 ± 0.19 | 3,453 | 0.88 ± 0.14 | 0.25 |
| SF-6D cohort | United States | SF-6D | 5,154 | 0.68 ± 0.17 | 4,834 | 0.79 ± 0.13 | 0.18 |
QALY changes after total hip replacement in the current study as compared with recent studies.
NR = not reported.
TABLE VIII.
Comparison of Quality-of-Life Changes After Primary Total Knee Arthroplasty*
| Preop. |
2-Yr. Postop. |
||||||
| Population | Utility Measure | No. of Patients | QALY and Standard Deviation | No. of Patients | QALY and Standard Deviation | Change in QALY | |
| Elmallah et al.16 (2015)† | United States | SF-6D | 844 | 0.62 ± NR‡ | 844 | 0.77 ± NR‡ | 0.15 |
| Liebs et al.13 (2016) | |||||||
| Early aquatic cohort | Germany | SF-6D | 87 | 0.581 ± 0.095 | 66 | 0.721 ± 0.119 | 0.125 |
| Late aquatic cohort | Germany | SF-6D | 98 | 0.569 ± 0.101 | 69 | 0.703 ± 0.135 | 0.129 |
| Jenkins et al.14 (2013) | United Kingdom | EQ-5D | 323 | 0.377 ± 0.312 | NR‡ | 0.671 ± 0.268 | 0.267 |
| Current study | |||||||
| EQ-5D cohort | United States | EQ-5D | 5,282 | 0.68 ± 0.17 | 3,309 | 0.84 ± 0.15 | 0.17 |
| SF-6D cohort | United States | SF-6D | 5,127 | 0.63 ± 0.11 | 4,851 | 0.76 ± 0.13 | 0.14 |
QALY changes after total knee replacement in the current study as compared with recent studies.
Study had 3-year follow-up. ‡NR = not reported.
To our knowledge, no prior study has systematically identified characteristics that predict QALY gain after hip and knee arthroplasty. We found that age, BMI, ASA score, sex, and preoperative utility correlated with QALY outcomes after primary total hip arthroplasty and total knee arthroplasty. These factors predicted 59% of the variation of patient outcomes following primary total hip arthroplasty and 45% of the variation in outcomes following primary total knee arthroplasty. These findings imply that patient selection is strongly predictive of postoperative QALY gain. Interestingly, age was a slight negative predictor of QALY gain. This finding may be due to decreased overall quality of life due to age22 as opposed to worse outcomes in elderly patients.
Preoperative health-related quality of life was the strongest predictor of QALY gain after hip and knee arthroplasty, including aseptic revision surgery. The lower the preoperative utility, the higher the expected QALY gain. This relationship was statistically significant and clinically important. For instance, our regression model (Table III) predicts that a patient with a preoperative utility of 0.55 would gain 0.33 QALY annually after total hip replacement; in contrast, a similar patient with a preoperative utility of 0.8 would gain only 0.125 QALY annually. Patients with the most compromised preoperative function gain the greatest postoperative improvement.
The present study had several limitations. Although QALYs are the preferred outcome measurement for economic analysis, they represent generic health outcomes. Therefore, patient-related health factors besides arthroplasty may affect postoperative QALYs. However, QALY outcomes are known to correlate with hip and knee-specific outcome instruments12,16. Also, we were unable to exclude patients with postoperative complications, which may have negatively biased the results. Furthermore, we only had data on patients who had preoperative EQ-5D, SF-36, or SF-12 scores; we did not have information on patients who failed to answer preoperative questionnaires and therefore we were unable to calculate overall loss to follow-up. Additionally, for several procedures—including septic revisions, conversion of hemiarthroplasty or hip resurfacings to total hip arthroplasty, conversions of unicompartmental knee arthroplasty to total knee arthroplasty, and patellofemoral arthroplasties—we provided QALY outcomes for only a limited number of patients. However, we are aware of no previous studies that have provided such data for these procedures. Furthermore, fewer patients completed postoperative EQ-5D forms compared with SF-36 or SF-12 forms. However, as most patients completed other health questionnaires that provided similar results, we believe that this limitation did not strongly bias our results. Finally, we examined a high-volume arthroplasty center, and therefore our results may not be generalizable to institutions that perform fewer cases per year23.
In summary, we have provided preoperative and postoperative annual QALY results for common hip and knee arthroplasty procedures; many of these data were not previously available. We used both the EQ-5D and the SF-6D as the basis for our QALY estimates. Our results demonstrated that average health-related quality of life after primary hip or knee replacement approach those for healthy patients of similar age as reported in the recent literature. We delineated several patient-related factors that were associated with outcomes. While age, BMI, and ASA score were significant predictors, the most important factor for predicting annual QALY gains after hip and knee arthroplasty was the patient’s preoperative quality of life: a lower preoperative utility was found to be highly predictive of larger QALY gains postoperatively. Our results may be used to facilitate future cost-effectiveness studies in arthroplasty, to counsel patients regarding expected outcomes, and to assist in selecting patients who may benefit most from arthroplasty.
Footnotes
Investigation performed at the Adult Reconstruction & Joint Replacement Division, The Hospital for Special Surgery, New York, NY
Disclosure: No external source funded this investigation. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSOA/A59).
References
- 1.Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol. 2012. October;26(5):649-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao HY, Kang PD, Xia YY, Shi XJ, Nie Y, Pei FX. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplasty. 2017. November;32(11):3421-8. Epub 2017 Jun 8. [DOI] [PubMed] [Google Scholar]
- 3.Rowan FE, Salvatore AJ, Lange JK, Westrich GH. Dual-mobility vs fixed-bearing total hip arthroplasty in patients under 55 years of age: a single-institution, matched-cohort analysis. J Arthroplasty. 2017. October;32(10):3076-81. Epub 2017 May 11. [DOI] [PubMed] [Google Scholar]
- 4.Haglin JM, Eltorai AE, Gil JA, Marcaccio SE, Botero-Hincapie J, Daniels AH. Patient-specific orthopaedic implants. Orthop Surg. 2016. November;8(4):417-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moon YW, Ha CW, Do KH, Kim CY, Han JH, Na SE, Lee CH, Kim JG, Park YS. Comparison of robot-assisted and conventional total knee arthroplasty: a controlled cadaver study using multiparameter quantitative three-dimensional CT assessment of alignment. Comput Aided Surg. 2012;17(2):86-95. [DOI] [PubMed] [Google Scholar]
- 6.Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg. 2013. March;5(1):1-9. Epub 2013 Feb 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nam D, Weeks KD, Reinhardt KR, Nawabi DH, Cross MB, Mayman DJ. Accelerometer-based, portable navigation vs imageless, large-console computer-assisted navigation in total knee arthroplasty: a comparison of radiographic results. J Arthroplasty. 2013. February;28(2):255-61. Epub 2012 Jun 14. [DOI] [PubMed] [Google Scholar]
- 8.Werner SD, Stonestreet M, Jacofsky DJ. Makoplasty and the accuracy and efficacy of robotic-assisted arthroplasty. Surg Technol Int. 2014. March;24:302-6. [PubMed] [Google Scholar]
- 9.Makhni EC, Steinhaus ME, Swart E, Bozic KJ. What are the strength of recommendations and methodologic reporting in health economic studies in orthopaedic surgery? Clin Orthop Relat Res. 2015. October;473(10):3289-96. Epub 2015 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegel JE, Weinstein MC, Russell LB, Gold MR; Panel on Cost-Effectiveness in Health and Medicine. Recommendations for reporting cost-effectiveness analyses. JAMA. 1996. October 23-30;276(16):1339-41. [DOI] [PubMed] [Google Scholar]
- 11.Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96:5-21. Epub 2010 Oct 29. [DOI] [PubMed] [Google Scholar]
- 12.Elmallah RK, Chughtai M, Adib F, Bozic KJ, Kurtz SM, Mont MA. Determining health-related quality-of-life outcomes using the SF-6D following total hip arthroplasty. J Bone Joint Surg Am. 2017. March 15;99(6):494-8. [DOI] [PubMed] [Google Scholar]
- 13.Liebs TR, Herzberg W, Rüther W, Russlies M, Hassenpflug J; Multicenter Arthroplasty Aftercare Project, MAAP. Quality-adjusted life years gained by hip and knee replacement surgery and its aftercare. Arch Phys Med Rehabil. 2016. May;97(5):691-700. Epub 2016 Jan 11. [DOI] [PubMed] [Google Scholar]
- 14.Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J. 2013. January;95-B(1):115-21. [DOI] [PubMed] [Google Scholar]
- 15.Fordham R, Skinner J, Wang X, Nolan J; Exeter Primary Outcome Study Group. The economic benefit of hip replacement: a 5-year follow-up of costs and outcomes in the Exeter Primary Outcomes Study. BMJ Open. 2012. May 25;2(3):e000752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elmallah RK, Cherian JJ, Jauregui JJ, Bhowmik-Stoker M, Beaver WB, Mont MA. Determining health-related quality-of-life outcomes using the SF-6D preference-based measure in patients following total knee arthroplasty. J Arthroplasty. 2015. July;30(7):1150-3. Epub 2015 Feb 7. [DOI] [PubMed] [Google Scholar]
- 17.The EuroQol Research Foundation. EQ-5D. 2018. https://euroqol.org/. Accessed 2018 May 7.
- 18.Luengo-Fernandez R, Gray AM, Bull L, Welch S, Cuthbertson F, Rothwell PM; Oxford Vascular Study. Quality of life after TIA and stroke: ten-year results of the Oxford Vascular Study. Neurology. 2013. October 29;81(18):1588-95. Epub 2013 Oct 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kwon JW, Park HY, Kim YJ, Moon SH, Kang HY. Cost-effectiveness of pharmaceutical interventions to prevent osteoporotic fractures in postmenopausal women with osteopenia. J Bone Metab. 2016. May;23(2):63-77. Epub 2016 May 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soto M, Sampietro-Colom L, Sagarra J, Brugada-Terradellas J. InnovaSEC in action: cost-effectiveness of Barostim in the treatment of refractory hypertension in Spain. Rev Esp Cardiol (Engl Ed). 2016. June;69(6):563-71. Epub 2016 Feb 19. [DOI] [PubMed] [Google Scholar]
- 21.Doble B, John T, Thomas D, Fellowes A, Fox S, Lorgelly P. Cost-effectiveness of precision medicine in the fourth-line treatment of metastatic lung adenocarcinoma: An early decision analytic model of multiplex targeted sequencing. Lung Cancer. 2017. May;107:22-35. Epub 2016 Jun 2. [DOI] [PubMed] [Google Scholar]
- 22.Fryback DG, Dasbach EJ, Klein R, Klein BE, Dorn N, Peterson K, Martin PA. The Beaver Dam Health Outcomes Study: initial catalog of health-state quality factors. Med Decis Making. 1993. Apr-Jun;13(2):89-102. [DOI] [PubMed] [Google Scholar]
- 23.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004. September;86-A(9):1909-16. [DOI] [PubMed] [Google Scholar]


