Abstract
The objective of this study is to measure the preliminary efficacy of a pilot intervention, grounded in behavioural economics, increasing adherence of dual protection (simultaneous use of effective modern contraception and a barrier method, such as a condom) to protect against HIV, other sexually transmitted infections, and unintended pregnancy. Between 2015 and 2016, 100 women aged 18–40 years, seeking post-abortion care in Cape Town, South Africa were recruited to Empower Nudge, a randomised controlled trial to test a lottery incentive intervention designed to increase dual protection. At baseline, the mean age of participants was 27 years; 82% of them were from South Africa; 58% self-identified as Black African; average education completed was 11.7 years. At three months, assignment to the lottery intervention was associated with higher odds of returning for study visits (OR: 6.0; 95%CI: 2.45 to 14.7, p < 0.01), higher condom use (OR: 4.5; 95%CI: 1.43 to 14.1; p < 0.05), and higher use of dual protection (OR: 3.16; 95%CI: 1.01 to 9.9; p < 0.05). Only 60% of the study population returned after three months and only 38% returned after six months. Women who receive post-abortion care represent a neglected population with an urgent need for HIV and pregnancy prevention. Dual protection is a critically important strategy for this population. Lottery-based behavioural economics strategies may offer possible ways to increase dual protection use in this population. Further research with larger samples, longer exposure time, and more sites is needed to establish fully powered efficacy of lottery incentives for dual protection; using objective verification for monitoring.
Keywords: Behavioural economics, conditional economic incentives, dual protection, HIV prevention, long-acting reversible contraceptives, post-abortion care, South Africa
Résumé
L’objectif de cette étude est de mesurer l’efficacité préliminaire d’une intervention pilote, fondée sur l’économie comportementale, destinée à augmenter l’observance d’une double protection (utilisation simultanée d’une contraception moderne efficace et d’une méthode barrière comme le préservatif) pour se protéger contre le VIH, d’autres infections sexuellement transmissibles et les grossesses non désirées. De 2015 à 2016, 100 femmes âgées de 18 à 40 ans qui avaient bénéficié de soins après avortement au Cap, Afrique du Sud, ont été recrutées pour Empower Nudge, un essai randomisé contrôlé qui souhaitait tester une intervention incitative avec loterie, conçue de façon à augmenter la double protection. Au début de l’essai, l’âge moyen des participantes était de 27 ans; 82% d’entre elles étaient originaires d’Afrique du Sud; 58% s’identifiaient elles-mêmes comme Africaines noires; la durée moyenne d’études achevées était de 11,7 ans. Trois mois après, la participation à l’intervention avec loterie était associée à des probabilités plus élevées de retour pour les visites d’étude (RC : 6,0; 95% IC : 2,45 à 14,7, p<0,01), un emploi accru du préservatif (RC : 4,5; 95% IC : 1,43 à 14,1; p <0,05) et une utilisation supérieure de la double protection (RC : 3,16; 95% IC : 1,01 à 9,9; p<0,05). Seulement 60% des femmes faisant l’objet de l’étude sont revenues après trois mois et à peine 38% après six mois. Les femmes qui ont reçu des soins après avortement représentent une population négligée qui a besoin de toute urgence de mesures de prévention du VIH et des grossesses, et pour qui la double protection est une stratégie capitale. Les stratégies économiques comportementales basées sur une loterie peuvent donner des moyens d’améliorer le recours à une double protection parmi cette population. De nouvelles recherches avec des échantillons plus vastes, un temps d’exposition plus long et davantage de sites sont nécessaires afin d’établir l’efficacité totale des mesures d’incitation à base de loterie pour la protection double, en utilisant une vérification objective pour le suivi.
Resumen
El objetivo de este estudio es medir la eficacia preliminar de una intervención piloto, basada en la economía conductual, para aumentar la adherencia a la doble protección (uso simultáneo de un anticonceptivo moderno eficaz y un método de barrera, como un condón, para proteger contra el VIH, otras infecciones de transmisión sexual y el embarazo no intencional). Entre 2015 y 2016, 100 mujeres de 18 a 40 años de edad, que buscaban atención postaborto en Ciudad del Cabo, Sudáfrica, fueron reclutadas para participar en Empower Nudge, un ensayo controlado aleatorizado para probar una intervención de incentivo de lotería diseñada para aumentar el uso de doble protección. En la línea de base, la edad media de las participantes era de 27 años; el 82% provenía de Sudáfrica; el 58% se identificó como Negra Africana; el nivel de escolaridad promedio era de 11.7 años. Después de tres meses, la asignación a la intervención de lotería fue asociada con mayor probabilidad de regresar para las visitas del estudio (RM: 6.0; IC de 95%: 2.45 a 14.7, p < 0.01), mayor uso de condones (RM: 4.5; IC de 95%: 1.43 a 14.1; p < 0.05) y mayor uso de doble protección (RM: 3.16; IC de 95%: 1.01 a 9.9; p < 0.05). Solo el 60% de la población del estudio regresó después de tres meses y solo el 38% regresó después de seis meses. Las mujeres que reciben atención postaborto representan a una población desatendida con una necesidad urgente de prevención de VIH y embarazo. La doble protección es una estrategia de fundamental importancia para esta población. Las estrategias de economía conductual basada en la lotería podrían ofrecer posibles maneras de aumentar el uso de doble protección en esta población. Se necesitan más estudios de investigación con mayores muestras, más tiempo de exposición y más lugares de estudio para establecer la plena eficacia de los incentivos de lotería para usar doble protección, utilizando verificación objetiva para el monitoreo.
1. Introduction
In South Africa, where over 6.4 million people are living with HIV,1 supporting women’s sexual and reproductive health includes supporting their desires to avoid or delay pregnancy, while also reducing their chances of HIV infection and transmission.2 Dual protection, or the simultaneous prevention of both pregnancy and HIV/STIs, is a policy priority in recognition of the high rates of sexually transmitted infections (STIs), including HIV, as well as unintended pregnancy rates.3–5 Dual protection occurs via (a) correct and consistent use of a condom alone (because appropriate condom use can prevent both HIV and pregnancy), or (b) via dual method use (DMU) which is correct and consistent use of a condom/barrier method, plus correct and consistent use of another effective method of contraception, including long-acting reversible contraception (LARC).2
In Southern Africa, 55% of pregnancies in women aged 15–44 are unintended.6 Young women in South Africa face a high risk of unintended pregnancy. By age 18, 19% of women have been pregnant, a figure that rises to 43% at age 21, and 72% by age 25.7 Incorrect or inconsistent use of contraception is common. Male partners often oppose contraceptive use and access to services can be limited, particularly in the teenage years. Unprotected sex resulting in unintended pregnancy also places women at risk for STIs, including HIV infection. Women are disproportionately affected by South Africa’s HIV epidemic, with 23% of women (ages 15–49) HIV-infected.1 At 39%, pregnant women have the highest HIV infection levels compared to other sub-populations.8 Moreover, pregnancy increases the risk of vertical transmission of HIV/STIs.9 Use of effective contraception is thus critically important for women wishing to avoid pregnancy, as is dual protection to prevent transmission or acquisition of HIV/STIs.10–12 Since 2014, the National Department of Health encourages the use of other long-acting reversible hormonal contraception, in addition to hormonal injectable contraception (the etonogestrel contraceptive implant and intrauterine devices), together with condoms, for dual protection.13
Conditional lottery incentives, whereby participants have a chance to win a prize if they fulfil some protective requirement, have proven effective in various realms of public health,14 and they may also help in the uptake of HIV prevention behaviours. For example, conditional lotteries created excitement and renewed interest in HIV testing and counselling among automotive workers in two industrial plants in South Africa.15 Most significantly, a lottery rewarding staying free of new curable STIs was effective at reducing HIV incidence among a heterosexual adult, rural population in Lesotho.16
Behavioural economics is a relatively new science which combines features of economics and psychology to address systematic biases in human behaviour.17 One of the main insights of behavioural economics is that we, as humans, do not always maximise our own “utility” or well-being in a “rational” manner.18 That is, we do not necessarily act in a way that would fully maximise our long-term benefits. We may be present-biased or shortsighted because we are more focused on our actions in the very short term rather than on what may or may not happen in the distant future. Another important insight is that of salience: we tend to make decisions based on information that has been received more recently, or that has been received from a particular source. Given that we have started to understand these systematic human biases,19 behavioural economics attempts to address them with interventions to improve public policies. Thus behavioural economic approaches can have important implications for HIV prevention and treatment.20,21
Behavioural economics can provide a framework to explain why some women may not follow through with their stated intentions to initiate and particularly to continue using LARC and dual protection.22 First, life stressors can negatively affect decision-making: for example, worries about personal finances can compromise the ability to make decisions, and may compromise self-regulation.23,24 Lotteries may help to address hidden health-seeking costs, which are sometimes unaffordable, due to factors such as transportation costs or missed work time because of long waiting times in clinics and the need for multiple clinic appointments. Second, decisions for LARC may be done in a “cold” (or calculating) state of mind, while decisions about condom use may often be decided in the heat of the moment.25 Thus, lotteries may help to counterbalance the different weights given to the decisions in different “hot/ cold” states. Third, undue weight to small probabilities is another behavioural economics concept that has been applied to lotteries. The proposed intervention – a lottery conditional on fulfilling goals of dual protection to win a small monetary prize – aims to turn around this common human shortcoming and re-focus it toward health benefits. Lotteries are popular around the world because they generally present a small probability of winning a large prize. Although the probability of winning the large prize is only slightly greater than zero, millions of people buy lottery tickets every day. We seek to use this paradigm to help women follow through their stated goals of health promotion by using a lottery with a greater probability of winning.
Given many women’s dual desire to avoid pregnancy and HIV infection and transmission, and the success of conditional lotteries in nudging individuals towards healthier behaviours, we pilot tested a behavioural economics innovation – the Empower, Nudge Lottery – in combination with best practices for contraceptive use and HIV/STI prevention to promote dual protection (via DMU) among women wishing to avoid a repeat unintended pregnancy. Though incentives have been used to promote contraception,26 to our knowledge, lotteries have not been used, nor has dual protection been measured as a specific outcome.
2. Methods
We conducted a randomised controlled pilot as a proof-of-concept to test a lottery to promote dual protection among young women seeking post-abortion care in South Africa. After post-abortion care, women are regularly offered contraception, thus facilitating the goals of the lottery trial. We followed participants for six months individually (during May 2015–April 2016). We obtained written informed consent from all participants. Institutional Review Boards at the University of Cape Town, South Africa, and at Brown University, Providence, RI, USA approved all procedures. We registered the protocol at ClinicalTrials.gov under identifier number NCT02536612.
2.1. Experimental design and site
A total of 100 women who had recently experienced an abortion were randomly assigned in a 1:1 ratio to one of two groups. Group 1 (control) received only transport compensation (R100 each time, ∼US$8 at the time of the intervention) for study visits at enrolment and at months 3 and 6. Group 2 (intervention) received transport compensation (R100 each time) for study visits at enrolment and at months 3 and 6, plus the opportunity to enter a lottery (with a 50% chance of winning R400, ∼US$33, each time, at months 3 and 6). Participants in the intervention group had a chance to receive: (a) one lottery ticket subject to confirmation of the continued use of modern contraceptive methods at 3 months; and (b) another lottery ticket subject to confirmation of dual protection use at 6 months.
At the initial clinic visit, in consultation with a healthcare provider and unrelated to the study, women selected a contraceptive method from various options: injectable hormonal contraception (Depo-Provera or Nur-Isterate); implant; intrauterine device (IUD); or oral contraceptives (OCs). All participants received condoms (male and female), and brief counselling/basic information about dual protection from the project nurse. Women who continued method use, as determined by a clinical specialist, at the month 3 visit, received their first lottery ticket. (Being STI free was not a condition at three months; this gave us more confidence in the self-reported condom use outcome as it was explicitly stated that condom use was in no way tied to lottery eligibility at month 3). The second ticket was provided at the end of the study (month 6) to those with successful dual protection: those who had renewed (or not discontinued) their contraception method, and who were STI-free. (Syphilis served as a proxy for non-condom use because of cost and ease of implementation. We did not expect to find many cases, but we expected participants to use condoms more to make sure they did not test positive. This was another innovative use of the tendency to over-weight small probabilities; the theory suggests that a representative participant may have thought: even if I know that few women contract syphilis, I’ll still use condoms because I [overweight small probabilities and] don’t want to lose my lottery ticket. A urine pregnancy test was also administered, though pregnancy status was not used as conditionality at any point in the study.
The clinical study site was a public healthcare facility in Cape Town, South Africa. This facility has adequate space and administrative privacy and is used frequently by post-abortion clients (with referrals from a secondary hospital) as it provides a full range of contraceptive options. It also has a history of close collaboration between research and clinical staff.
2.2. Eligibility and randomisation
Women, 18–40 years, presenting for post-abortion family planning services were eligible to participate, regardless of HIV/STI status. Study participants had sought abortion services (both surgical and medical). Medical abortions were performed with Mifepristone at the clinic followed by Misoprostol at home. Surgical abortions, using manual vacuum aspiration (MVA), were performed at the clinic. Women who chose to receive injectables, implant, or an IUD were eligible for the study; those who received OCs were not (as objective monitoring of daily pill use was deemed less feasible). As of 2015, modern contraceptive prevalence among married or in-union women, 15–49 years of age in South Africa was reported to be 64.8%; injectables accounted for 30.3% of contraceptive prevalence, male condoms for 4.9%, IUDs for 1.1%, and implants with a negligible proportion near 0%.27 Participants were approached while in an observation/recovery area (after the medical or surgical procedure had been completed, and after they had chosen a contraceptive method for future use). They underwent informed consent procedures in a separate, private room (the Supplementary Appendix has a blank informed consent form). If they agreed to participate, they filled out a brief baseline survey, and then they agreed to return for 3- and 6-month follow-ups.
A statistical expert, independent from the study, generated a random sequence and filled opaque envelopes (to conceal the allocation) with cards that said either “Lottery” or “No lottery.” After enrolling a participant, the study research assistant opened the next envelope and assigned the participant accordingly. Because knowledge of the intervention (lottery) was a design feature, assignment was unblinded after randomisation.
2.3. Rationale for design and eligibility
The justification for the study design and eligibility criteria is as follows. First, we used a lottery rather than a guaranteed payment scheme as an incentive because we wanted to test specific behavioural economic hypotheses; and most of the previous literature on incentives and contraception focused on guaranteed payments.26 Some of the guaranteed payment schemes, such as conditional cash transfers, however, have shown mixed results.28,29 One reason for some of the null findings in guaranteed schemes may be because of the complex interactions with education,30 which has been traditionally used as the conditionality. Thus, lottery incentives may be innovative if they can be tied directly to some verifiable outcome; and they could be potentially more cost-effective. Second, we targeted women who received post-abortion care for enrolment because they are a population that would be highly motivated to take up contraception. Although this study population may be non-representative of all young South African women, it serves as a highly-at-need population for whom this proof-of-concept idea of lottery incentives for dual protection may be beneficial.
2.4. Measures
The primary outcome was whether a lottery increased return rates for the 3-month follow-up study interview. Secondary outcomes were dual protection and condom use. A study research assistant conducted the survey for the assessment. Condom use was assessed as part of a series of options for the question: “Are you currently using any method to delay or avoid getting pregnant?” (See Appendix for selected questions). Dual protection use was assessed with the question: “Do you currently practice ‘dual protection’, that is do you use a male or female condom as well as a modern contraceptive method (IUD, or injectable contraceptive) to prevent STIs and pregnancy?” Exploratory outcomes included assessing the feasibility of objectively measuring dual protection at 3 and 6 months via clinical examinations, as well as conducting urine pregnancy tests and STI (syphilis) tests as proxy marker for objectively verifying condom use.
2.5. Statistical analysis
The main analysis presents the treatment effects at 3 and at 6 months. We estimated unadjusted odds ratios (ORs) comparing control and intervention groups in a logistic regression framework at 3 and 6 months separately.31 As sensitivity analyses, we first included adjusted odds ratios (aOR) using covariates including demographic and socio-economic characteristics. Given the experimental design, regression adjustment is not really needed; however, many researchers continue to use it.32,33 Second, to address factors related to loss to follow up, we used marginal structural modelling using each participant’s return visit history to derive inverse probability of treatment weights (IPTW).34,35 Finally, if we found an initial main effect, and to explore potential effect differences at different times, we also used fully interacted models with the main effect of the lottery intervention, time (visit) dummies, and interaction terms (intervention group × time) using a generalised estimating equation (GEE) framework.36 We conducted the analyses using Stata SE 15.1 (College Station, TX) with xtgee and glm commands for the GEE and generalised linear models using robust standard errors clustered at the individual level.
2.6. Sample size and statistical power
The original sample size estimation was based on the secondary outcome of dual protection. The most recent nationally representative data we found for the prevalence of dual protection (18.6%) was from 2010.37 Relevant sub-regional data showed dual protection prevalence between 14% and 33%.38 We hence assumed that about 20% would be using dual protection in our sample, and that the effect size would be 0.3. Thus, we needed 34 women per arm to detect differences with 95% confidence and 80% power. The target of 50 per arm allowed for loss-to-follow-up of 32%. All data were collected in paper surveys administered by research assistant, double-entered into EpiData (http://www.epidata.dk/) and imported to Stata for analysis.
3. Results
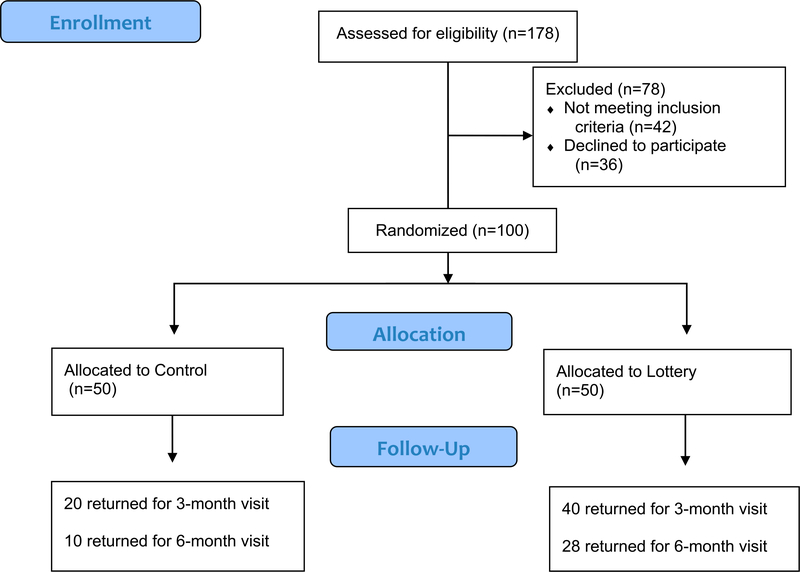
A total of 178 women were assessed for eligibility, of which 42 (24%) were not eligible and 36 (20%) declined to participate. Thus, 100 participants were enrolled, randomised, and included for sub-sequent analyses (Figure 1). Only 60% of the study population returned at 3 months and only 38% of the population returned after 6 months.
Figure 1.
Flow of participants for Empower Nudge Lottery initial pilot study
3.1. Baseline data
Table 1 shows that baseline socio-demographic characteristics of study participants were similar in the control and lottery groups prior to randomisation. The mean age was 27 years; 69% had a stable sexual partner (married/committed/regular); 82% were South African nationals; 58% self-identified as Black African (while the rest were of mixed race); 20% were students and the average number of years of education was 11.7 years. They lived in households composed of four people on average; and were living in the same area for almost a decade. On average, they had 7.6 basic household items (out of 10), and the monthly earnings were about US$130. The HIV positivity rate was 17%. There were no statistically significant differences in the intervention and control groups.
Table 1.
Baseline comparison of intervention and control groups
| Control [n = 50] | Lottery [n = 50] | Full Sample [n = 100] | Pa | ||||
|---|---|---|---|---|---|---|---|
| Age in years, mean (SD) | 26.6 | (6.2) | 27.2 | (5.5) | 26.9 | (5.9) | 0.62 |
| Stable partner | 36 | (72) | 33 | (66) | 69 | (69) | 0.52 |
| South African | 42 | (84) | 40 | (80) | 82 | (82) | 0.61 |
| Black African | 27 | (54) | 31 | (62) | 58 | (58) | 0.47 |
| Student | 12 | (24) | 8 | (16) | 20 | (20) | 0.32 |
| Highest school grade completed, mean (SD) | 11.9 | (1.8) | 11.5 | (1.8) | 11.7 | (1.8) | 0.31 |
| Household size, mean (SD) | 4.14 | (1.94) | 4.02 | (1.62) | 4.08 | (1.78) | 0.74 |
| Years living at current area, mean (SD) | 10.52 | (10.70) | 9.24 | (10.51) | 9.88 | (10.60) | 0.55 |
| Wealth based on asset indexb, mean (SD) | 7.86 | (2.08) | 7.34 | (2.32) | 7.60 | (2.21) | 0.24 |
| Monthly earnings (US $), median, interquartile range | 133 | (93–177) | 130 | (86–163) | 130 | (90–168) | 0.60 |
| HIV-positive | 6 | (12) | 11 | (22) | 17 | (17) | 0.19 |
Notes: Table presents number, n, and percentage (%), unless otherwise noted.
Chi-squared test conducted for binary variables and analysis of variance for continuous variables.
Wealth was measured using an asset index, defined as the sum of affirmative responses to questions about ownership of 10 household items.
Earnings data were transformed from South African Rand at an average exchange rate of 12 Rand per US $.
Table 2 shows that self-reported sexual behaviour and stated demand for contraception was also similar between control and lottery groups. Among the 69 participants (69%) with stable sex partners, more than a fourth (26%) were married, 41% described their relationship as “serious/committed” and a third (33%) said they had a regular boyfriend. Among this group, almost a fourth (23%) had sexual activity several times per week, almost half (49%) had sexual activity weekly and about a fifth (19%) had sex on a monthly basis. More than half of this group (54%) stated that they use condoms only “sometimes” while more than a third (34%) said they never use condoms.
Table 2.
Self-reported sexual behaviour and demand for contraception
| Control (n = 50) | Lottery (n = 50) | Full sample (n = 100) | Pa | ||||
|---|---|---|---|---|---|---|---|
| Sexual behaviour | |||||||
| Involved in sexual relationship | 36 | (72) | 33 | (66) | 69 | (69) | 0.52 |
| Type of partner | |||||||
| Married/permanent | 11 | (31) | 7 | (21) | 18 | (26) | 0.38 |
| Serious/committed | 16 | (44) | 12 | (36) | 28 | (41) | 0.49 |
| Regular boyfriend | 9 | (25) | 14 | (42) | 23 | (33) | 0.12 |
| Regularity of sexual activity | |||||||
| Daily | 0 | (0) | 1 | (3) | 1 | (1) | 0.29 |
| Several times per week | 10 | (28) | 6 | (18) | 16 | (23) | 0.34 |
| Weekly | 20 | (56) | 14 | (42) | 34 | (49) | 0.28 |
| Monthly | 3 | (8) | 10 | (30) | 13 | (19) | 0.02 |
| Less than once per month | 3 | (8) | 2 | (6) | 5 | (7) | 0.72 |
| Condom use regularity with partner | |||||||
| Always | 5 | (14) | 3 | (9) | 8 | (12) | 0.51 |
| Sometimes | 20 | (57) | 17 | (52) | 37 | (54) | 0.64 |
| Never | 10 | (29) | 13 | (39) | 23 | (34) | 0.35 |
| Partner’s feelings about condom use | |||||||
| Supports condom use | 13 | (36) | 11 | (33) | 24 | (35) | 0.80 |
| He doesn’t like it | 23 | (64) | 22 | (67) | 45 | (65) | 0.81 |
| Number of abortions | |||||||
| One (current ToP)b | 42 | (84) | 40 | (80) | 82 | (82) | 0.60 |
| Two or more | 8 | (16) | 10 | (20) | 18 | (18) | 0.60 |
| Contraception method to be used | |||||||
| Intra-uterine device (IUD) | 3 | (6) | 4 | (8) | 7 | (7) | 0.72 |
| Injection: Depo-Provera | 28 | (56) | 23 | (46) | 51 | (51) | 0.27 |
| Injection: Nur-Isterate | 5 | (10) | 6 | (12) | 11 | (11) | 0.78 |
| Implant | 15 | (30) | 18 | (36) | 33 | (33) | 0.57 |
| Likelihood of stopping contraception use in next 6 months | |||||||
| Not at all likely | 46 | (92) | 41 | (82) | 87 | (87) | 0.14 |
| Don’t know | 4 | (8) | 9 | (18) | 13 | (13) | 0.14 |
| The lottery can help continue using contraceptive you are planning to use | |||||||
| Strongly agree | 6 | (12) | 7 | (14) | 13 | (13) | 0.77 |
| Agree | 37 | (74) | 39 | (78) | 76 | (76) | 0.64 |
| Disagree | 7 | (14) | 4 | (8) | 11 | (11) | 0.34 |
Notes: Table presents number, n, and percentage (%), unless otherwise noted.
Chi-squared test conducted for binary variables and analysis of variance for continuous variables.
ToP = termination of pregnancy.
For most of the women (82%), the current termination of pregnancy (ToP) was their first abortion; however, for almost a fifth (18%) it was their second (or higher number) abortion. After the current ToP, most of them (51%) chose an injectable contraceptive (Depo-Provera), a third (33%) chose the implant, followed by another injectable (Nur-Isterate) (11%), and the IUD (7%). The majority (89%) agreed or strongly agreed that the lottery intervention would help them to continue using the contraceptive of choice that they were planning to use.
3.2. Preliminary efficacy of lottery intervention
Table 3 presents the effects of the intervention on primary and secondary outcomes. At months 3 and 6 (in the last two columns), the primary outcome (returning for study interview) shows ORs greater than 1 for the two follow-ups. In particular, the lottery group was more than 6 times more likely to return at 3 months than the control group (OR: 6.0, 95%CI: 2.45 to 14.7, p < 0.01) and over 5 times more likely to return at 6 months (OR: 5.09, 95%CI: 2.09 to 12.4, p < 0.01). The lottery group was also over 4 times more likely to use condoms at 3 months (OR: 4.5, 95%CI: 1.43 to 14.1, p < 0.05); and over twice as likely to do so at 6 months, (OR: 2.5, 95%CI: 0.57 to 11.1), though the latter was not statistically significant. Finally, we also observed significant improvements in dual protection use at 3 months, with the lottery group being over 3 times more likely to be using dual protection than the control group (OR: 3.16, 95%CI: 1.01 to 9.91, p < 0.05); and also more likely to do so at 6 months (OR: 1.3, 95%CI: 0.31 to 5.67) though the latter was not statistically significant.
Table 3.
Unadjusted effects of the intervention on primary and secondary outcomes
| Control, N = 50 | Lottery, N = 50 | Effect estimates | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted, n (%) | Unadjusted, n (%) | 3-month | 6-month | |||||
| Baseline | 3-month | 6-month | Baseline | 3-month | 6-month | OR (95% CI) | OR (95% CI) | |
| Returned for study visit | 50 (100) | 20 (40) | 10 (20) | 50 (100) | 40 (80) | 28 (56) | 6.00*** | 5.09*** |
| (2.45 to 14.7) | (2.09 to 12.4) | |||||||
| Condom use | 11 (22) | 8 (40) | 5(50) | 6(12) | 30 (75) | 20 (72) | 4.50** | 2.50 |
| (1.43 to 14.1) | (0.57 to 11.1) | |||||||
| Dual protection |
3(6) | 6(30) | 5(50) | 1 (2) | 23 (58) | 16(57) | 3.16** | 1.33 |
| (1.01 to 9.91) | (0.31 to 5.67) | |||||||
Notes: Table reports effects estimates using odds ratio (OR) from logistic regression using the control group as the reference category, and 95% confidence interval (CI).
p < 0.10,
p < 0.05,
p < 0.01.
3.3. Sensitivity analyses
The sensitivity analyses did not qualitatively change the main results, and also suggested increased dual protection and condom use in the lottery group. We summarise the results below with detailed tables shown as Supplementary Materials.
3.3.1. Regression adjustment
Appendix Table A (see Supplementary Material) presents adjusted odds ratios (aORs) controlling for age, nationality, race, student status, schooling, household size, years living in the area, an asset index (as a proxy for wealth), monthly earnings (to measure income), and HIV status. The lottery group was more than 9 times more likely to return at 3 months than the control group (aOR: 9.08, 95% CI: 3.32 to 27.8, p < 0.01); and almost 6 times more likely to return at 6 months (aOR: 5.94, 95%CI: 2.19 to 16.1, p < 0.01). The lottery group was also almost 9 times more likely to use condoms at 3 months (aOR: 8.85, 95%CI: 2.17 to 63, p < 0.01); and almost twice as likely to do so at 6 months, (aOR: 1.81, 95%CI: 0.20 to 16.0), though the latter was not statistically significant. Finally, we also observed significant improvements in dual protection use at 3 months, with the lottery group being over 3 times more likely to be using dual protection than the control group (aOR: 3.91, 95%CI: 0.89 to 17.2, p < 0.05); yet slightly less likely to do so at 6 months (OR: 0.96, 95%CI: 0.14 to 6.76) though the latter result was not statistically significant.
3.3.2. Inverse probability weighting
Appendix Table B (see Supplementary Material) presents inverse-probability-weighted (IPW) adjusted odds ratios controlling for age, nationality, race, student status, schooling, household size, years living in the area, an asset index (as a proxy for wealth), monthly earnings (to measure income), and HIV status. The lottery group was almost 8 times more likely to return at 3 months than the control group (IPW aOR: 7.94, 95%CI: 2.62 to 24, p < 0.01); and almost 4 times more likely to return at 6 months (IPW aOR: 3.82, 95%CI: 0.80 to 18.2, p < 0.10). The lottery group was also over 9 times more likely to use condoms at 3 months (IPW aOR: 9.83, 95%CI: 1.32 to 72.9, p < 0.01); and over 4 time more likely to do so at 6 months, (IPW aOR: 4.19, 95%CI: 0.44 to 40), though the latter was not statistically significant. Finally, we also observed significant improvements in dual protection use at 3 months, with the lottery group being over 3 times more likely to be using dual protection than the control group (IPW aOR: 3.94, 95%CI: 0.80 to 19.3, p < 0.10); and also more likely to do so at 6 months (IPW OR: 2.29, 95%CI: 0.24 to 22.3) though the latter result was not statistically significant.
3.3.3. Effects-by-time
Appendix Table C (see Supplementary Material) summarises the effects-by-time results using fully interacted effects-by-time models with main effects and interactions for primary and secondary outcomes to explore differential effects at specific times. The main effect was large and significant for returning for visit interview with OR = 5.091 (p < 0.01) and aOR = 5.801 (p < 0.01). Importantly, the characteristics of those who returned for clinic visit interviews were similar than those who did not; we found no significant differences in the main socio-demographic indicators, with the exception of race: Black Africans were 2.9 times more likely to return for the study interview (column 2). The 3-month-by-visit interactions were significant for condom use and dual protection. In the unadjusted model for condom use (column 3), the 3-month × Lottery interaction had OR = 9.085 (p < 0.01); and the results were similar in the adjusted model (column 4) with aOR = 9.5 (p < 0.01). Likewise, in the unadjusted model for dual protection (column 5), the 3-month × Lottery interaction had OR = 10.02 (p < 0.10), and the results were large also in the adjusted model (column 6) with aOR = 13.36 (p < 0.05). The 6-month-by-visit interactions were marginally significant for condom use and non-significant dual protection. Not surprisingly, higher earnings are associated with higher condom use and dual protection. Of note, HIV-positive status is significantly associated with higher condom use [aOR = 7.4 (p < 0.01)], though non-significantly associated with higher dual protection [aOR = 2.4].
3.3.4. Exploratory outcomes
In terms of the exploratory outcomes, objective verification of contraception method (by clinician observation) was possible for about a fourth of the lottery participants (13/50 = 26%) and a sixth of the control group (8/50 = 16%), whose main contraception provider was the clinical site. In addition, the STI results (for syphilis) as well as the pregnancy results were not analysed because of low cell size: there was only one case of syphilis (in the control group), and no documented cases of pregnancy.
4. Discussion
This is the first pilot trial, to our knowledge, documenting the preliminary efficacy of a lottery intervention to promote sustained use of dual protection among young women intending to avoid pregnancy in South Africa. The sample’s mean age of 27 years with a 17% HIV positivity rate is reflective of the most affected populations in South Africa, the country with the largest HIV epidemic in the world. Compared to the control group, women in the intervention group who had the opportunity to win a lottery prize were more likely to return to study visits, use condoms and use dual protection methods for the prevention of unwanted pregnancies and HIV infection at the 3-month follow-up. There was a signal at 6 months that follow-up interviews were more likely, but the condom use and dual protection results were no longer significant, possibly because of the smaller sample size due to loss-to-follow-up.
This pilot trial shows short-term preliminary efficacy to nudge young women receiving c-abortion care in South Africa to use dual protection methods using conditional lottery incentives. Similar lottery approaches have been used in the prevention of HIV/STIs in other settings.39–41 Notably, a study in Lesotho showed that a lottery ticket, conditional on negative test results for STIs, was associated with lower HIV incidence.16 Previous experiences in South Africa and elsewhere, suggest that conditional incentive policies should be informed by carefully conducted research, and ethical oversight.42 Finding ways to ensure choice in the absence of coercion is essential. As part of this, incentive-based interventions should be built upon best practices for contraceptive care, including informed decision-making, expanded choice, non-coercion, and human rights. If so designed, such interventions may well offer promise to support and empower women in achieving their goals.
This study was designed carefully to adhere to the ethical principles outlined above. Most significantly, choice to use contraception and choice of method occurred outside of, and prior to, the study. Women, in consultation with their clinical care providers, made an informed decision to use a long-acting reversible contraception option; thus, the lottery served only as an additional tool to support them in fulfilling their intention. Furthermore, by choosing women who were receiving post-abortion care, we targeted a population of women who did not want to carry a pregnancy to term, and who, through opting to use long-acting contraception following an abortion, were highly motivated to take up contraception. Designing an intervention to align with “revealed preferences,” as we do here, offers one way for lottery incentives to avoid coercion. Other economic-based interventions should be assessed similarly from an ethics perspective, and choose carefully the conditionality.43,44
These exploratory, proof-of-concept findings highlight the critical need for innovative interventions using behavioural economic insights to curtail the negative effects of unwanted pregnancy and HIV infection in low-resource settings. Participants’ knowledge of modern contraception was high (>70%), but actual use was inconsistent. Nevertheless, a large majority (89%) agreed that an incentive-based intervention would motivate them to continue contraceptive use over time, indicating overall enthusiasm for the intervention (data from project questionnaire, not shown). Surprisingly, HIV status was not associated with return for study visits although previous evidence suggests that HIV status is associated with increased contact with various healthcare providers.38,45 Nevertheless, there are different demands for dual protection from an HIV-positive versus HIV-negative population. Although HIV-positive women had higher likelihood of condom use –in line with recommended preventative actions– HIV status did not affect dual protection. This may be reflective of continued and strong childbearing desire and/ or fertility for women who are HIV-positive and receiving ART.9
While this study assesses return at the 3-month study interview and demonstrates that conditional lotteries may lead to differential loss-to-follow-up, in the current context of dual protection, this return for clinic visits is also an important proxy for LARC, suggesting that lotteries have the potential to influence continued use of dual protection methods. Correct and sustained use of dual protection and LARC – which require periodic clinic visits– continue to be important policy goals to expand choice.3
4.1. Long-term costs and feasibility
One of the major concerns of conditional incentives is that they may increase adherence in the short term while the reward is offered, but they may fail to address the underlying motivations behind health choices and thus may not be successful over time.21 Further research is thus needed on lottery incentives as a longer-term strategy, including the feasibility of scaling up such an intervention as well as the costs and cost-effectiveness.
4.2. Limitations
There were several limitations. First, we collected syphilis data but the incidence rate was low, which limited our ability to use STIs as a proxy for condom use. In future work, data should be collected on other STIs as well including: Chlamydia, gonorrhoea and trichomonas vaginalis. Second, the loss-to-follow-up (LTFU) rates were high, despite repeated attempts via email and text (WhatsApp) to contact the participants and ask them to return for study visits. This may be reflective also of high migration rates.46 Yet for most participants, the post-abortion clinical site was not the site of their regular care, which may have meant that the costs of returning to this specialised clinical site were higher than those they might have experienced if follow-up had occurred elsewhere, which should be a consideration in future work. Further, relying on a population of women receiving post-abortion care, who have chosen long-acting contraception, provides a focused evaluation of lotteries among women with a demonstrated strong preference for contraception. However, this study population is not representative of all women who might be interested in dual protection. Future trials may need less restrictive samples and should use tools to link various health clinic databases at the local and regional levels to allow for more timely and objective verification of contraception use. Cash upfront for transport to the clinic (rather than compensation after the fact) may have reduced LTFU. Third, the sample size was small. The initial effect size, nevertheless, was large and it provides an encouraging signal and initial proof-of-concept. Finally, the short duration of the pilot trial (6 months) implied that we could not observe the discontinuation of longer duration LARCs (such as the implant), and future trials should consider longer periods of follow-up to help provide insight on across methods, including long- and short-term responses.
5. Conclusion
Larger scale studies, with more participants followed for longer periods, are needed to fully evaluate the efficacy of this type of behavioural economics approach for increasing the use of dual protection methods among women at high risk of HIV acquisition and unwanted pregnancy. Conditional lottery incentives tied to dual protection may have public health and policy development implications beyond South Africa, too. The preliminary efficacy results on lottery rewards designed to support contraceptive use and dual protection point to the value of additional research with larger samples, in multiple sites, over a longer period of time. There will be value as well in learning more from women directly, through in-depth interviews, about how they experienced the behavioural economic lottery intervention.
Supplementary Material
Acknowledgements
The authors thank Mariette Momberg for her leadership in the implementation and data collection phases of the project, Nthutu Mvana for her excellent work with the participants, Namhla Sicwebu for assistance in preparing the databases, Sister Judiac Ranape for her passion and dedication to her work as clinical nurse practitioner, and above all to the women who agreed to participate in the Empower Nudge project. The views and opinions expressed are those of the authors alone and do not necessarily represent those of the National Institutes of Health, or Brown University, the Corporation or the Trustees. The funding and implementing organisations did not have any role in the decisions to conduct the trial, analyse data, or prepare manuscripts for publication.
Funding
This research was supported by Brown University Research Seed Funds (Office of the Vice President for Research). This research also benefited from support to the Population Studies and Training Center at Brown University, which receives core support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (US) (P2C HD041020); as well as support from the South African Social Science and HIV Programme (SASH) (R24HD077976). This work was also facilitated by the Providence/Boston Center for AIDS Research (P30AI042853).
Footnotes
Registration: This protocol was registered as a randomized controlled trial in ClinicalTrials.gov: NCT02536612
Supplemental data for this article can be accessed at https://doi.org/10.1080/09688080.2018.1510701.
References
- 1.Shisana O, Rhele T, Simbayi LC, et al. South African national HIV prevalence, incidence and behaviour survey, 2012. Pretoria: Human Sciences Research Council; 2014. [Google Scholar]
- 2.Lince-Deroche N, Pleaner M, Harries J, et al. Achieving universal access to sexual and reproductive health services: the potential and pitfalls for contraceptive services in South Africa. South African Heal Rev. 2016; (1):95–108. [Google Scholar]
- 3.DoH. National contraception and fertility planning policy and service delivery guidelines: a companion to the national contraception clinical guidelines. Pretoria: Department of Health (DoH), Republic of South Africa; 2012. DOI:10.1016/S0968-8080(14)43764-9. [Google Scholar]
- 4.Naidoo S, Wand H, Abbai NS, et al. High prevalence and incidence of sexually transmitted infections among women living in Kwazulu-Natal, South Africa. AIDS Res Ther. 2014;11(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giuliano AR, Botha MH, Zeier M, et al. High HIV, HPV, and STI prevalence among young western cape, South African women. JAIDS J Acquir Immune Defic Syndr. 2015;68 (2):227–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45(3):301–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Lith LM, Yahner M, Bakamjian L. Women’s growing desire to limit births in sub-Saharan Africa: meeting the challenge. Glob Heal Sci Pract. 2013;1(1):97–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kharsany ABM, Frohlich JA, Yende-Zuma N, et al. Trends in HIV prevalence in pregnant women in rural South Africa. J Acquir Immune Defic Syndr. 2015;70(3):289–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarnquist CC, Rahangdale L, Maldonado Y. Reproductive health and family planning needs among HIV-infected women in sub-Saharan Africa. Curr HIV Res. 2013;11 (2):160–168. [cited 2017 April 7] http://www.ncbi.nlm.nih.gov/pubmed/23432491. [DOI] [PubMed] [Google Scholar]
- 10.Secura G Long-acting reversible contraception: a practical solution to reduce unintended pregnancy. Minerva Ginecol. 2013;65(3):271–277. http://www.ncbi.nlm.nih.gov/pubmed/23689169. [PubMed] [Google Scholar]
- 11.United Nations Population Fund, UNFPA. Partnering for results UNFPA South Africa 3rd country programme. Pretoria: United Nations Population Fund (UNFPA); 2013; http://countryoffice.unfpa.org/southafrica/drive/UNFPACountryReport2013-LowerResFORWEB.pdf. [Google Scholar]
- 12.Crankshaw TL, Smit JA, Beksinska ME. Placing contraception at the centre of the HIV prevention agenda. Afr J AIDS Res. 2016;15(2):157–162. [DOI] [PubMed] [Google Scholar]
- 13.Cooper D, Harries J, Moodley J, et al. Coming of age? Women’s sexual and reproductive health after twenty-one years of democracy in South Africa. Reprod Health Matters. 2016;24(48):79–89. [DOI] [PubMed] [Google Scholar]
- 14.Haff N, Patel MS, Lim R, et al. The role of behavioral economic incentive design and demographic characteristics in financial incentive-based approaches to changing health behaviors: a meta-analysis. Am J Heal Promot. 2015;29 (5):314–323. [DOI] [PubMed] [Google Scholar]
- 15.Weihs M, Meyer-Weitz A. A lottery incentive system to facilitate dialogue and social support for workplace HIV counselling and testing: a qualitative inquiry. SAHARA J J Soc Asp HIV/AIDS Res Alliance. 2014;11(1):116–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Björkman Nyqvist M, Corno L, de Walque D, et al. Incentivizing safer sexual behavior: evidence from a lottery experiment on HIV prevention. Am Econ J Appl Econ. 2018. DOI:10.1257/APP.20160469. [Google Scholar]
- 17.Kahneman D Maps of bounded rationality: psychology for behavioral economics. Am Econ Rev. 2003;93(5):1449–1475. [Google Scholar]
- 18.Camerer C, Loewenstein G, Rabin M. Advances in behavioral economics. Russell Sage Foundation; 2004. [Google Scholar]
- 19.Psychology DellaVigna S. and economics: evidence from the field. J Econ Lit. 2009;47:315–372. [Google Scholar]
- 20.Operario D, Kuo C, Sosa-Rubí SG, et al. Conditional economic incentives for reducing HIV risk behaviors: integration of psychology and behavioral economics. Heal Psychol. 2013;32(9):932–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galárraga O, Genberg BL, Martin RA, et al. Conditional economic incentives to improve HIV treatment adherence: literature review and theoretical considerations. AIDS Behav. 2013;17(7):2283–2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stevens J, Berlan ED. Applying principles from behavioral economics To promote long-acting reversible contraceptive (LARC) methods. Perspect Sex Reprod Health. 2014;46 (3):165–170. [DOI] [PubMed] [Google Scholar]
- 23.Mani A, Mullainathan S, Shafir E, et al. Poverty impedes cognitive function. Science. 2013;341(6149):976–980. [DOI] [PubMed] [Google Scholar]
- 24.Bernheim BD, Ray D, Yeltekin Ş. Poverty and self-control. Econometrica. 2015;83(5):1877–1911. [Google Scholar]
- 25.Ariely D, Loewenstein G. The heat of the moment: the effect of sexual arousal on sexual decision making. J Behav Decis Mak. 2006;19(2):87–98. [Google Scholar]
- 26.Heil SH, Gaalema DE, Herrmann ES. Incentives to promote family planning. Prev Med (Baltim). 2012;55(Suppl.):S106–S112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.United Nations,Department of Economic and Social Affairs, Population Division. Trends in contraceptive Use worldwide 2015. New York: United Nations; 2015; [cited 2017 April 11]. http://www.un.org/en/development/desa/population/publications/pdf/family/trendsContraceptiveUse2015Report.pdf. [Google Scholar]
- 28.Pettifor A, MacPhail C, Hughes JP, et al. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet Glob Heal. 2016;4: e978–e988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baird SJ, Garfein RS, McIntosh CT, et al. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–1329. [DOI] [PubMed] [Google Scholar]
- 30.Rosenberg M, Pettifor A, Miller WC, et al. Relationship between school dropout and teen pregnancy among rural South African young women. Int J Epidemiol. 2015;44 (3):928–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rabe-Hesketh S, Everitt BS. A handbook of statistical analyses using Stata. 4th ed. Boca Raton (FL): Chapman & Hall/CRC; 2007. [Google Scholar]
- 32.Imbens GW, Wooldridge JM. American economic association recent developments in the econometrics of program evaluation recent developments in the econometrics of program evaluation. J Econ Lit. 2009;47 (471):5–86. [cited 2016 June 24] http://www.jstor.org/stable/27647134. [Google Scholar]
- 33.Athey S, Imbens G. The econometrics of randomized experiments. In: Duflo E, Banerjee A, editors. Handbook of field experiments. Amsterdam: North-Holland (Elsevier); 2017. p. 73–140. DOI:10.1016/bs.hefe.2016.10.003. [Google Scholar]
- 34.Robins JM, Hernán MÁ, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. [cited 2016 June 24] http://www.jstor.org/stable/3703997. [DOI] [PubMed] [Google Scholar]
- 35.Fewell Z, Wolfe F, Choi H, et al. Controlling for time-dependent confounding using marginal structural models. Stata J. 2004;4(4):402–420. [Google Scholar]
- 36.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42 (1):121–130. [cited 2016 Nov 19] http://www.ncbi.nlm.nih.gov/pubmed/3719049. [PubMed] [Google Scholar]
- 37.Peltzer K, Mzolo T, Mbelle N, et al. Dual protection, contraceptive use, HIV status and risk among a national sample of South African women. Gend Behav. 2010;8(1). DOI:10.4314/gab.v8i1.54699. [Google Scholar]
- 38.Kaida A, Laher F, Strathdee SA, et al. Contraceptive use and method preference among women in Soweto, South Africa: the influence of expanding access to HIV care and treatment services. PLoS One. 2010;5(11): e13868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Niza C, Rudisill C, Dolan P. Vouchers versus lotteries: what works best in promoting chlamydia screening? A cluster randomised controlled trial. Appl Econ Perspect Policy. 2014;36(1):109–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dolan P, Rudisill C. The effect of financial incentives on chlamydia testing rates: evidence from a randomized experiment. Soc Sci Med. 2014;105:140–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Petry NM, Alessi SM, Marx J, et al. Vouchers versus prizes: contingency management treatment of substance abusers in community settings. J Consult Clin Psychol. 2005;73 (6):1005–1014. [DOI] [PubMed] [Google Scholar]
- 42.Critics Bateman C. “chew” furiously on Zille’s HIV/drug-testing “carrots”. SAMJ South African Med J. 2012;102 (1):12–13. [PubMed] [Google Scholar]
- 43.Krubiner CB, Merritt MW. Which strings attached: ethical considerations for selecting appropriate conditionalities in conditional cash transfer programmes. J Med Ethics. 2017;43(3):167–176. [DOI] [PubMed] [Google Scholar]
- 44.Kohler HP, Thornton RL. Conditional cash transfers and HIV/AIDS prevention: unconditionally promising? World Bank Econ Rev. 2012;26(2):165–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Manne-Goehler J, Montana L, Gómez-Olivé FX, et al. The ART advantage. JAIDS J Acquir Immune Defic Syndr. 2017;75(5):561–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shearer K, Clouse K, Meyer-Rath G, et al. Citizenship status and engagement in HIV care: an observational cohort study to assess the association between reporting a national ID number and retention in public-sector HIV care in Johannesburg, South Africa. BMJ Open. 2017;7(1): e013908) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.