Abstract
Background:
Older adults with opioid use disorder (OUD) are a medically complex population. The current study evaluated trends in older adults seeking treatment for OUD, with a focus on primary heroin versus prescription opioid use. This study also compared older adults with OUD to the younger OUD population on demographics and drug use behaviors.
Methods:
Publicly available data from state-certified addiction treatment centers were collected via the Treatment Episode Data Set – Admissions (TEDS-A) between 2004-2015. This study utilized Joinpoint Regression to conduct a cross-sectional, longitudinal analysis of trends in first-time treatment admissions for OUD in adults 55 and older (older adults; n=400,421) versus adults under the age of 55 (n=7,795,839). Given the rapid increase in older adults seeking treatment for OUD between 2013-2015, secondary outcomes include changes in demographics and drug use between 2012 (as a baseline year) and 2015.
Results:
The proportion of older adults seeking treatment for OUD rose steadily between 2004-2013 (41.2% increase; p-trend=0.046), then rapidly between 2013-2015 (53.5% increase; p-trend=0.009). The proportion of older adults with primary heroin use more than doubled between 2012- 2015 (p<0.001); these individuals were increasingly male (p<0.001), African American (p<0.001), and using via the intranasal route of administration (p<0.001).
Conclusions:
There has been a recent surge in older adults seeking treatment for OUD, particularly those with primary heroin use. Specialized treatment options for this population are critically needed, and capacity for tailored elder care OUD treatments will need to increase if these trends continue.
Keywords: Older Adults, Opioid Use Disorder, Treatment, Trend Analysis, Heroin, Prescription Opioids
1. Introduction
The opioid crisis has affected Americans from all walks of life. The rate of U.S. adults engaging in non-medical prescription opioid use has declined in recent years, yet the overall rate of illicit opioid use (including heroin and prescription opioids) and opioid use disorder (OUD) continues to rise (Jones, 2017). Older adults may have been overlooked as a potentially vulnerable population during this nation-wide tragedy. Although alcohol remains the most common substance use problem among older adults (Han et al., 2017a), illicit drug use is becoming more common in this population. The number of older adults seeking treatment for OUD is projected to increase (Cicero et al., 2012), and the magnitude of this trend has not been assessed in recent years. Since there is no consensus in the scientific literature regarding the definition of “older adults” (Carew and Comiskey, 2017), this term will be used here to refer to adults 55 and older because they are through their “mid-life” years and beginning to retire and experience age-related health problems (Petry, 2002).
Persons with OUD are often categorized as using either prescription opioids or heroin as their primary drug of choice. This is an artificial distinction, as prescription opioids and heroin both act on the μ-opioid receptor and are often co-used; however, classifying individuals by their drug of choice (e.g. prescription opioids or heroin) may also have value, as prescription opioid misuse is often an initial step toward heroin use (Jones et al., 2015; Compton et al., 2016; Mital et al., 2018). It is unclear how the opioid crisis has affected older adults compared to the larger population of persons with OUD, yet older adults might have unique risk factors that make them susceptible to opioid misuse and OUD.
Older adults have a higher rate of prescription opioid exposure than any other age group (Han et al., 2017b), and chronic opioid use for the purpose of pain relief can progress to physical dependence and/or the onset of OUD. Older adults at risk of developing OUD often engage the medical community, and a recent study reported that 40-50% of adults 50 and older who misused prescription opioids obtained those medications through physicians (Schepis et al., 2018). Likewise, as individuals age they are less likely to obtain prescription opioids illicitly (from ‘dealers’) and more likely to obtain prescription opioids via the medical community (Cicero et al., 2012).
Research examining trends in older adults using and seeking treatment for illicit drugs has generally found increased opioid use over relatively long periods of time. Between 1990 and 2010 illicit opioid use increased among older adults and this group was less likely than younger adults to perceive their drug use as problematic, and seek treatment (Wu and Blazer, 2011). Moreover, the proportion of older adults seeking treatment for heroin increased markedly between the mid 1990s and 2000s (Lofwall et al., 2008; Arndt et al., 2011). In general, the average age when individuals first seek treatment for OUD has increased since the 1960s (Carew and Comiskey, 2017), although in 2010 the average age of initiation of opioid use was still relatively low (23 years old) (Cicero et al., 2014).
Older adults are inherently more complicated to treat medically (Qato et al., 2008; Gerlach et al., 2017; Davis et al., 2017), and while it is well established that this growing population is often exposed to opioids for pain management, the longitudinal trends in older adults seeking treatment for OUD remains unclear. This information is necessary to help treatment facilities prepare for the unique needs of this population. The purpose of this report is to quantify trends in United States OUD admissions for older adults versus the rest of the OUD population (those under the age of 55) between 2004-2015. In addition, individuals were stratified by whether their primary substance of use at admission was heroin or prescription opioids. Associated demographics and routes of opioid administration over time were also evaluated.
2. Methods
2.1. Sample Collection: The Treatment Episode Data Set (TEDS)
Data were collected from the Treatment Episode Data Set for Admissions (TEDS-A) between 2004-2015 (N=22,160,542), a database of U.S. state certified substance abuse treatment systems maintained by the Center for Behavioral Health Statistics and Quality within the Substance Abuse and Mental Health Services Administration (Center for Behavioral Health Statistics and Quality, 2018). Each case in the TEDS-A represents a single treatment admission, and as such, the same individual could account for multiple cases in a given year or across years if they had multiple treatment admissions. To eliminate the possibility that individuals could account for multiple cases in the dataset, and to focus on individuals who were new to addiction treatment, only first-time admissions were included in these analyses (n=8,196,260). These admissions were further divided into the target population of adults 55 and older (n=400,421) and the rest of the OUD population as a comparator group, i.e. all adults under the age of 55 (n=7,795,839). Yearly numbers and proportions of older adults (hereafter defined as adults 55 and older) that were identified within the TEDS-A system as presenting to treatment for OUD with an opioid as their primary drug of choice (either primary heroin or primary prescription opioids) can be found in Supplementary Tables 1 and 2*.
2.2. Key Demographic Variables
Several variables within the TEDS-A database that might explain the shift in older adult populations presenting to treatment and/or changes in drug use behaviors among older adults with OUD were evaluated. These included demographic variables such as sex, race, ethnicity, living arrangement (dependent living such as nursing home or in-home care versus independent living), treatment location (dichotomized as urban [micro/metropolitan area] versus non-urban), veteran status, and employment status; as well as drug use variables such as primary route of administration and other substances used at the time of admission.
2.3. Data Analyses
Demographic variables for first-time treatment admissions among older adults between 2004–2015 are presented in Supplementary Table 1* for primary heroin use and Supplementary Table 2* for primary prescription opioid use. Joinpoint Regression was utilized to identify trends between 2004–2015 in first-time admissions for OUD among older adults and adults under 55. Joinpoint analysis derives the optimal number of trends in cross-sectional data by incorporating point estimates and standard errors to a regression model with either no joinpoints (i.e. single regression line throughout the sample) versus alternative models with one or more joinpoints using Monte Carlo simulation to determine best fit. The significance of each identified trend is defined as the slope of the regression line being significantly different from 0 at alpha < 0.05, and is reported as p-trend (Jones and McAninch, 2015). Joinpoint was also used to determine the average annual percent change (AAPC) of treatment admissions for OUD between 2004–2015, and to compare AAPCs for individual trends between adults 55 and older, versus adults under 55 (Clegg et al., 2009).
Given that the most recent statistically significant rise in first time treatment admissions for the older group occurred between 2013-2015, chi-squared analyses were used to determine the shift in demographic variables and route of opioid administration between the most recent year (2015), and a baseline year (2012). These analyses were performed separately for older adults presenting to treatment for primary heroin and primary prescription opioid use.
Additionally, bivariate logistic regression was utilized to determine adjusted odds ratios (AORs) for key demographic variables between older adults versus adults under 55 during the most the recent trend in new treatment admissions (2013-2015). p-trends across time including AAPC were analyzed via Joinpoint version 4.6.0 (National Cancer Institute, Bethesda, MD) and all other analyses were performed using SPSS version 24.0 (IBM, Armonk, NY).
3. Results
3.1. Trends in Older Adults Seeking Treatment for Opioid Use Disorder
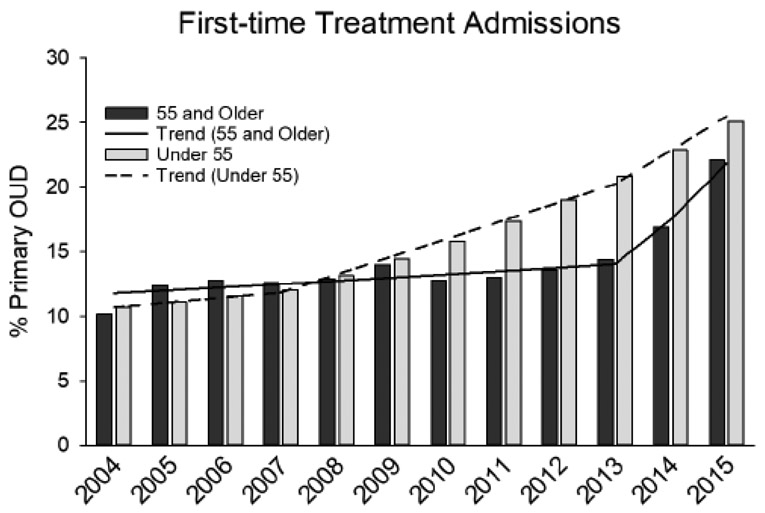
Joinpoint regression analysis identified two trends (joinpoint in 2013) in older adults presenting to treatment for primary OUD between 2004-2015. First-time OUD admissions among older adults increased 41.2% between 2004-2013 (p-trend=0.046), with an AAPC of 8.0% (95% CI: 6.5%-9.7%), i.e. first-time admissions increased an average of 8% each year compared to the previous year. Subsequently, first-time OUD admissions increased 53.5% between 2013-2015 (p-trend=0.009), with an AAPC of 24.7% (95% CI: 7.9%-44.1%) (Figure 1).
Figure 1.
Trends in first-time treatment admissions for primary opioid use among adults 55 and older versus adults under 55 who present to State-certified addiction treatment facilities. Lines represent joinpoint regression analyses for significantly different trends within groups, across time. OUD = opioid use disorder.
Joinpoint analysis identified two trends (joinpoint in 2007) in adults under 55 presenting to treatment for primary OUD between 2004-2015. For this group, first-time OUD admissions increased 10.5% between 2004-2007 (p-trend=0.172), with an AAPC of 3.9% (95% CI: −2.1% - 10.3%), followed by a 69.2% increase between 2007-2015 (p-trend<0.001), with an AAPC of 9.6% (95% CI: 8.6% - 10.7%) (Figure 1).
There was no significant difference in AAPC between older adults and adults under 55 across the entire time period of 2004-2015 (−2.3%, 95% CI: −5.4% - 0.8%; p=0.149). There was a significant difference in AAPC between 2007-2013 (−7.7%, 95% CI: −9.5% - −5.9%; p<0.001), such that the proportion of adults under 55 presenting to OUD treatment outpaced older adults over this period. Conversely, there was a significant difference in AAPC between 2013-2015 (15.0%, 95% CI: 0.1% – 30.0%; p=0.049), such that the proportion of older adults outpaced adults under 55 presenting to OUD treatment.
3.2. Shift in Demographics of Older Adults with Opioid Use Disorder (2012-2015)
3.2.1. Primary Heroin Use:
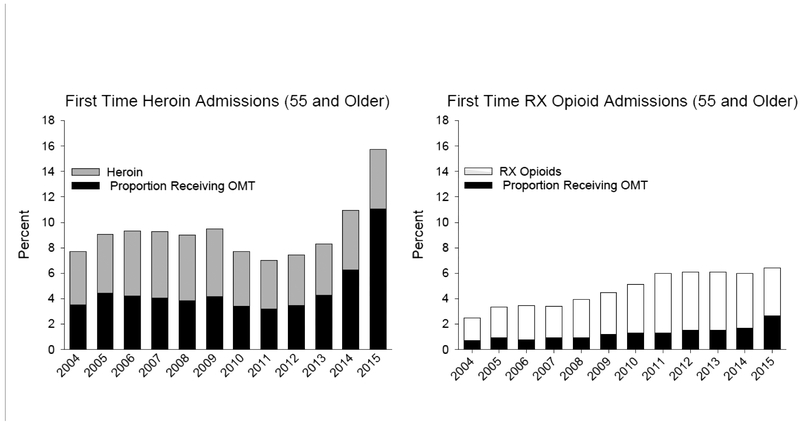
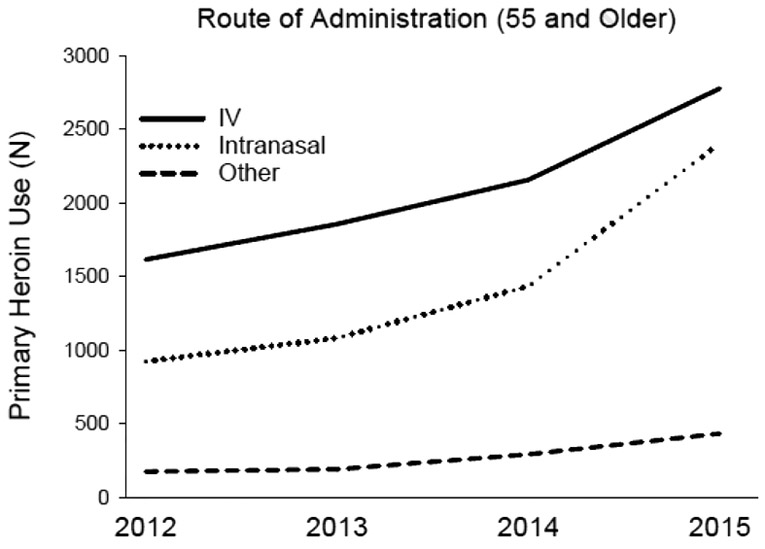
Between 2012 and 2015, new admissions for older adults presenting to treatment with heroin as their primary drug of choice increased significantly (110% increase) (Table 1). There was a 53% increase between 2012-2015 in planned opioid maintenance therapy (OMT) for first time admissions of older adults with primary heroin use (Table 1/Figure 2). During this period, older adults seeking OUD treatment were significantly less likely to be male (7% decrease), more likely to be black or African American (10% increase), less likely to be Hispanic (24% decrease), and were less likely to live in urban areas (37% decrease); they were also significantly more likely to use heroin via intranasal (26% increase) as opposed to IV (16.9%) routes (Table 1). Notably, the total number of older adults presenting to treatment with IV heroin use continued to increase between 2012 and 2015 (Figure 3). In addition, between 2012 and 2015 older adults were significantly less likely to be homeless (29% decrease), reside in a dependent living situation (38% decrease), or be unemployed (16% decrease); they were significantly more likely to be retired (26% increase) and reside in an independent living situation (11% increase).
Table 1.
Trends in Treatment Admissions for Primary Heroin or Prescription Opioid Use Among Older Adults between 2012-2015
| Heroin | RX Opioids | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | % Change from 2012-2015 | 2012 | 2013 | 2014 | 2015 | % Change from 2012-2015 | |
| Number of Adults 55 and Older | 2725 | 3143 | 3927 | 5636 | 2236 | 2297 | 2137 | 2291 | ||
| Proportion of Adults 55 and Older (%) | 7.5 | 8.3 | 10.9 | 15.7 | 110.4*** | 6.1 | 6.1 | 6.0 | 6.4 | 4.2** |
| Sex (% Male) | 77.5 | 76.4 | 75.4 | 72.1 | −6.9*** | 54.7 | 53.8 | 52.9 | 54.3 | −0.7 |
| Race/Ethnicity (%) | ||||||||||
| Caucasian | 38.1 | 39.1 | 38.7 | 34.2 | −10.2* | 84.5 | 83.4 | 80.4 | 76.6 | −9.3*** |
| Black or African American | 47.1 | 46.4 | 45.6 | 52 | 10.4*** | 9.6 | 9.1 | 11.6 | 13.8 | 43.8*** |
| Other | 14.8 | 14.5 | 15.7 | 13.8 | −6.8*** | 5.2 | 6.6 | 7 | 7.2 | 38.5** |
| Hispanic | 17.9 | 17.9 | 19.3 | 13.6 | −24.0*** | 6 | 8.1 | 8.3 | 10.8 | 80* |
| Usual Route of Administration (%) | ||||||||||
| Oral | 2.2 | 2.4 | 2 | 1.6 | −27.3* | 87.1 | 84.6 | 84.7 | 77.3 | −11.3*** |
| Nasal | 33.8 | 34.4 | 36.5 | 42.6 | 26.0*** | 5.1 | 5.1 | 4.4 | 7.3 | 43.1** |
| Injection (IV or IM) | 59.2 | 59 | 54.9 | 49.2 | −16.9*** | 4.1 | 6.4 | 5.4 | 5.3 | 29.3* |
| Other | 4.1 | 3.6 | 5.4 | 6.1 | 48.8*** | 3.3 | 3.6 | 6.7 | 8.8 | 166.7*** |
| Other Drug Use (%) | ||||||||||
| Alcohol | 15.6 | 15.6 | 12.3 | 10.5 | −32.7*** | 16.2 | 15.4 | 15.6 | 13.8 | −14.8* |
| Marijuana | 7.3 | 8.2 | 6.8 | 5.9 | −19.2* | 8.5 | 7.7 | 8.4 | 7.2 | −15.3 |
| Prescription Opioid | 7.7 | 7.8 | 6.7 | 5.2 | −32.5* | 100 | 100 | 100 | 100 | 0.0 |
| Heroin | 100 | 100 | 100 | 100 | 0.0 | 4.2 | 4 | 5.1 | 3.8 | −9.5 |
| Cocaine | 22.1 | 20.5 | 17.2 | 15.7 | −29.0** | 4.2 | 4.5 | 3.6 | 4.2 | 0.0 |
| Living Arrangement (%) | ||||||||||
| Homeless | 15.3 | 14.1 | 14 | 10.8 | −29.4*** | 5.6 | 5.1 | 6.2 | 6 | 7.1 |
| Dependent Living | 18.8 | 17.9 | 17.6 | 11.6 | −38.3*** | 11.2 | 11.4 | 11.4 | 11.6 | 3.6 |
| Independent Living | 65.3 | 67.7 | 67 | 72.6 | 11.2*** | 81.6 | 82.7 | 81 | 77.5 | −5.0 |
| Urban (%) | 89.9 | 88.9 | 88.8 | 56.9 | −36.7*** | 70.7 | 69.6 | 68.8 | 57.5 | −18.7*** |
| Veteran (%) | 7.4 | 8.3 | 6.7 | 5.4 | −27.0*** | 6.9 | 8.4 | 6.9 | 6.6 | −4.3 |
| Retired (%) | 23.6 | 24.4 | 19.7 | 29.8 | 26.3*** | 33.8 | 32.1 | 32.4 | 31.7 | −6.2 |
| Unemployed (%) | 31.5 | 30.5 | 31.8 | 26.6 | −15.6*** | 22.3 | 27.2 | 26.9 | 24.8 | 11.2 |
| Planned OMT (%) | 45.9 | 51.5 | 57.3 | 70.4 | 53.4*** | 24.7 | 24.9 | 27.8 | 41 | 66.0*** |
Trends in treatment admissions between 2012 (as a baseline year) and 2015 (final year of the most recent spike in admissions; see Figure 1). Older adults with OUD are split into primary heroin use (left) and primary prescription opioid use (right). Change in proportion between 2012-2015 measured via chi-squared analysis;
=p<0.05
=p<0.01
=p<0.001. Urban represents micropolitan and metropolitan areas. RX=prescription, IV=intravenous, IM=intramuscular, OMT=opioid maintenance therapy.
Figure 2.
Left: percent of older adults (55 and older) presenting to treatment for the first time with opioid use disorder using heroin as their primary drug of choice. Right: percent of older adults presenting to treatment for the first time with opioid use disorder using prescription opioids as their primary drug of choice. Both graphs show the relative proportion (in black) of older adults where opioid maintenance therapy (OMT) was planned as part of treatment for opioid use disorder (OUD). RX = prescription.
Figure 3.
Number of older adults presenting to treatment for the first time for opioid use disorder using heroin as their primary drug of choice. Lines represent the primary heroin route of administration. Years are restricted to the most recent surge in OUD treatment among older adults (2013-2015; see Figure 1) and include 2012 as a baseline comparator. The line marked “Other” encompasses oral, smoked, or any “other” route of administration as defined by the Treatment Episode Data Set.
3.2.2. Primary Prescription Opioid Use:
Between 2012 and 2015, the proportion of older adults presenting to treatment with prescription opioids as their primary drug of choice remained relatively flat (4% increase; Figure 2). During this time, there was a 66% increase in planned OMT for older adults with primary prescription opioid use (Figure 2). Between 2012-2015, older adults were significantly more likely to be black or African American (44% increase), Hispanic (80% increase), and they were less likely to live in urban areas (18% decrease) (Table 1); they were also more likely to use prescription opioids via intranasal (43% increase) as opposed to oral (11% decrease) routes (Table 1).
3.3. Comparison of Adults 55 and Older versus Adults Under 55 (2013-2015)
3.3.1. Primary Heroin Use:
There were several significant differences in first time admissions of older adults versus adults under 55 using heroin as their primary drug of choice. Older adults versus adults under 55 were more likely to be male (AOR=1.74, p<0.001), black or African American (AOR=4.33, p<0.001), and Hispanic (AOR=1.43, p<0.001) (Table 2). Regarding route of heroin administration, older adults were more likely than adults under 55 to use heroin via intranasal (AOR=1.37, p<0.001) and IV (AOR=1.62, p<0.05) routes. In addition, older adults were more likely than adults under 55 to use alcohol (AOR=1.08, p<0.05), but less likely to use other illicit substances (see Table 2); they were also more likely to live in urban areas (AOR=1.14, p<0.001) and did not differ in the use of OMT as part of their treatment plan (AOR=1.01, ns) (Table 2).
Table 2.
Odds Ratios For Treatment Seeking Adults 55 and Older Compared to Under 55 (2013-2015)
| Heroin | RX Opioid | |||
|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | |
| Sex (Male) | 1.74*** | 1.66-1.82 | 1.35*** | 1.28-1.43 |
| Race/Ethnicity | ||||
| Caucasian | 0.60*** | 0.56-0.65 | 0.91 | 0.82-1.02 |
| Black or African American | 4.33*** | 4.00-4.70 | 1.51*** | 1.32-1.73 |
| Other | Ref | Ref | ||
| Hispanic | 1.43*** | 1.33-1.53 | 0.81*** | 0.72-0.91 |
| Usual Route of Administration | ||||
| Oral | 2.35*** | 1.99-2.78 | 1.69*** | 1.48-1.92 |
| Nasal | 1.37*** | 1.25-1.50 | 0.49*** | 0.41-0.58 |
| Injection (IV or IM) | 1.62* | 1.10-2.39 | 0.63*** | 0.50-0.81 |
| Other | Ref | Ref | ||
| Other Drug Use | ||||
| Alcohol | 1.08* | 1.01-1.14 | 1.13** | 1.05-1.21 |
| Marijuana | 0.36*** | 0.33-0.38 | 0.32*** | 0.29-0.35 |
| Heroin | 1.00 | 1.00-1.00 | 0.81** | 0.70-0.93 |
| Prescription Opioid | 0.59*** | 0.54-0.64 | 1.00 | 1.00-1.00 |
| Cocaine | 0.79*** | 0.75-0.83 | 0.65*** | 0.57-0.74 |
| Benzodiazepines | 0.46*** | 0.40-0.52 | 0.84*** | 0.77-0.92 |
| Employment Status | ||||
| Employed | 0.53*** | 0.50-0.57 | 0.48*** | 0.45-0.52 |
| Unemployed | 0.51*** | 0.49-0.53 | 0.46*** | 0.43-0.50 |
| Not in Work Force | Ref | Ref | ||
| Retired | 3.57*** | 3.37-3.79 | 4.09*** | 3.80-4.40 |
| Homeless | 0.94* | 0.89-0.99 | 1.06 | 0.95-1.19 |
| Urban | 1.14*** | 1.09-1.20 | 1.25*** | 1.19-1.33 |
| Veteran | 1.01* | 1.0-1.02 | 1.00 | 0.99-1.01 |
| Planned OMT | 1.01 | 1.00-1.02 | 0.99 | 0.98-1.00 |
Adjusted odds ratios (AOR) for comparison of key demographics and drug use behaviors between adults 55 and older (older adults) and adults under 55 during the most recent spike in treatment seeking for OUD (see Figure 1). Primary heroin use is displayed on the right and primary prescription opioid use on the left. AORs derived from logistic regression analysis;
=p<0.05,
=p<0.01,
=p<0.001. Urban represents micropolitan and metropolitan areas. RX=prescription, IV=intravenous, IM=intramuscular, OMT=opioid maintenance therapy.
3.3.2. Primary Prescription Opioid Use:
There were also several significant differences in first time admissions of older adults versus adults under 55 using prescription opioids as their primary drug of choice. Older adults were more likely than adults under 55 to be male (AOR=1.35, p<0.001), black or African American (AOR=1.51, p<0.001), and less likely to be Hispanic (AOR=0.81, p<0.001) (Table 2). Regarding route of prescription opioid administration, older adults were more likely than adults under 55 to use prescription opioids via the oral route (AOR=1.69, p<0.001) and less likely to use via intranasal route (AOR=0.49, p<0.001). In addition, older adults versus adults under 55 using prescription opioids were more likely to use alcohol (AOR=1.13, p<0.01), but less likely to use other illicit substances (see Table 2); they were also more likely to live in urban areas (AOR=1.25, p<0.001) and did not differ in the use of OMT as part of their treatment plan (AOR=0.99, ns) (Table 2).
4. Discussion
Analysis of the TEDS-A database indicated a marked surge in older adults seeking firsttime treatment for OUD between 2013- 2015 (Figure 1). While the U.S. population of adults 55 and older grew by 5.7% percent between 2013-2015 (United States Census Bureau, 2018), the proportion of older adults seeking treatment for OUD increased 53.5%, outpacing both population growth and the rest of the OUD treatment-seeking population (Figure 1). Using 2012 as a baseline year, the proportion of older adults seeking treatment for heroin more than doubled between 2012 and 2015; prior to this, there also was a rise in older adults seeking treatment for prescription OUD, although this trend curtailed in 2011 and remained relatively flat thereafter (Table 1/Figure 2). It is also noteworthy that the absolute number of older adults seeking treatment for heroin more than doubled between 2012 and 2015 (Table 1), suggesting that the rise in proportion was not due to a decrease in other substance use disorders, but instead can be attributed to an increase in the absolute number of persons over 55 seeking treatment for primary heroin use. In some instances, older adults who use heroin may be expressly different than those who use prescription opioids, yet there is often a progression in OUD as some individuals begin using prescription opioids and later switch to heroin (Cicero and Ellis, 2015), and there is no clear demarcation among persons with OUD who primarily use prescription opioids or heroin. The current study examined heroin and prescription opioid use separately to provide a more granular analysis, although many of the trends for persons primarily using heroin or prescription opioids were similar when comparing across 2012 and 2015.
4.1. Primary Heroin Use
There were several important shifts in demographics and drug use behaviors of older adults seeking treatment for primary heroin use between 2012 and 2015. For example, older adults with primary heroin use were increasingly female and black or African American (Table 1). There was also an increase in the number of older adults living outside urban areas seeking treatment (Table 1). However, when compared to adults under 55, older adults with OUD were more likely to be male, black, and reside in urban areas (Table 2). Although much of the national attention regarding the opioid crisis has been focused on white individuals living in non-urban areas (Kuehn, 2014), these data suggest that a significant proportion of older adults who are seeking treatment for heroin are black and reside in urban areas. This should be taken into account as policies/interventions are designed to reach older adults with OUD. The primary route of heroin administration has also changed, as the proportion of older adults primarily using heroin via intranasal administration increased 26% between 2012 and 2015, and the proportion using intravenously decreased 17% during this time (Table 1). However, it is important to note that the absolute number (not the proportion) of older adults presenting for IV heroin use increased between 2012 and 2015 (Figure 3). Older adults were also more likely to administer heroin intravenously than adults under 55 (Table 2). This is particularly concerning, and while any heroin use is inherently dangerous, intravenous administration carries a high risk of disease transmission and overdose death (Degenhardt and Hall, 2012).
4.2. Primary Prescription Opioid Use
Whereas the number of older adults presenting to treatment with primary prescription opioid use has not significantly changed since 2012, the trends in this population were similar to those observed in older adults using heroin (Table 1). For instance, there was a 44% increase in treatment admissions who were black or African American and a growing number of older adults seeking treatment outside of urban areas (Table 1). In general, rural compared to urban areas have a higher population of older adults, and rural populations across the U.S. have experienced a rise in non-medical prescription opioid use and opioid-related fatalities (Keyes et al., 2014).
4.3. Clinical Implications
The utilization of OMT increased by 53% for primary heroin and 66% for primary prescription opioid use among older adults between 2012 and 2015, with no difference in OMT utilization between adults 55 and older versus those under 55 (Tables 1 and 2). Previous comparisons of older and younger adults in OMT reported that older adults initiated their substance use later in life (Lofwall et al., 2005), and it is possible that some older adults have a long history of OUD, while others may have a form of “late-onsef‘ OUD brought on by prescription opioid exposure later in life. There is little research and guidance on the potential special needs of older adults in OMT. As this population of older adults in OMT grows, there may be a need to develop and refine specialized programs that address treatment needs and vulnerabilities for these patients, as have occurred for other groups (e.g., adolescents, pregnant patients with OUD) (Han et al., 2015; Cotton et al., 2018). For example, published guidelines recommend starting methadone at lower doses in adults > 60 years old and proceeding more slowly to avoid respiratory depression (Substance Abuse and Mental Health Services Administration, 2018). However, these guidelines may lead to greater drop-out in this population due to poorly controlled withdrawal symptoms. Relatively little evidence exists from controlled studies for utilization of buprenorphine and extended-release naltrexone in this population. Older adults in OMT also tend to have poor general health and high rates of psychiatric comorbidities compared to population norms (Lofwall et al., 2005), and targeted services accounting for these clinical features are needed.
The integration of general health care and addiction treatment is still lacking in many areas, and treating OUD in an aging population with greater clinical complexity is inherently difficult (Rao and Roche, 2017). The data presented here do not include factors that could drive the onset of opioid misuse and subsequent development of OUD in older adults, although possible explanations include poor management of chronic pain, undiagnosed depression, and increased exposure to opioids. Unfortunately, non-pharmacological pain management techniques in older adults, such as cognitive behavioral therapy, may be complicated by cognitive decline and/or lack of family and social support (Horgas, 2017). Still, an “opioid sparing” approach to pain treatment has been recommended for older adults (Chang and Compton, 2016). Moreover, depression is a well-known risk factor for opioid misuse, and older adults with primary prescription OUD are more likely than younger adults to have psychiatric disorders (Cicero et al., 2012). Opioid misuse may often be missed or misdiagnosed in older adults (Gossop and Moos, 2008; Wang and Andrade, 2013). Data in this study show that an increasing number and proportion of older adults are presenting to treatment, differing from previous estimates (Dotson et al., 2013), and this cannot be simply explained by population growth (United States Census Bureau, 2018). Comprehensive integration of addiction treatment services with primary, geriatric, and/or psychiatric services may be necessary to effectively treat this population. In addition, understanding the factors that lead to OUD in older adults could lead to the development of early detection and/or interventions tailored specifically to address the opioid crisis in this population.
4.4. Limitations
The term “older adults” is not well defined (Han et al., 2017a; Han et al., 2017b), and the current study used 55 and older as a cutoff because (a) it is the highest age category in the TEDS-A, and (b) older adults that are under the age of 55 might be considered “mid-life” (Petry, 2002). Also, the diagnostic criteria regarding opioid dependence (Diagnostic and Statistical Manual of Mental Disorders 4; DSM-IV) versus OUD (DSM-V), changed in 2014 for the purpose of reimbursement via Medicare, Medicaid, and many private insurance companies, which could have affected older adults access to OMT. Finally, TEDS-A collects data from state certified substance abuse treatment centers and not primary care physicians or other addiction treatment providers that might be more or less likely to treat older adults.
5. Conclusions
Much of the media attention on the opioid crisis has focused on younger adults, however, a hidden consequence of the opioid crisis has been a sharp increase in older adults seeking treatment for OUD. This is a relatively understudied population that may be more susceptible to opioid misuse and OUD given ongoing comorbidities such as chronic pain and mental health conditions. In addition, typical OUD treatment options may not be optimized to treat this medically challenging population, making integration of addiction treatment and primary care medicine even more important for older adults.
Supplementary Material
Highlights.
There was a recent surge in older adults seeking treatment for opioid use disorder
Older adults seeking treatment for heroin use increased 110% between 2012-2015
This population is increasingly female and African American
Older adults are increasingly seeking treatment outside of urban areas
Abbreviations:
- (OUD)
Opioid use disorder
- (TEDS-A)
Treatment Episode Data Set – Admissions
- (IV)
Intravenous
- (OMT)
Opioid Maintenance Therapy
- (AAPC)
Average Annual Percent Change
- (AOR)
Adjusted Odds Ratio
- (CI)
Confidence Intervals
- (DSM)
Diagnostic and Statistical Manual of Mental Disorders
Footnotes
Contributors Statement
All authors contributed to the research design, data interpretation, and manuscript preparation. Author ASH performed all data analyses. All authors approved the final version of this manuscript.
Conflict of Interest Statement
Author DAT has received medication supplies from Indivior for an investigator initiated study, was site PI for a clinical trial sponsored by Alkermes, and is on a scientific advisory board for Alkermes. Author ECS has served as a consultant or served on advisory boards for Analgesic Solutions, Indivior, The Oak Group, Egalet Pharmaceuticals, Caron, Innocoll, and Pinney Associates, and has received research funding through his university from Alkermes. All opinions expressed and implied in this paper are solely those of the authors and do not represent or reflect the views of the Johns Hopkins University or the Johns Hopkins Health System. Authors ASH and KED report no conflicts.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi: ...
This manuscript utilizes publicly available data*
References
- Arndt S, Clayton R, Schultz SK, 2011. Trends in substance abuse treatment 1998–2008: increasing older adult first-time admissions for illicit drugs. Am J Geriatr Psychiatry. 19, 704–711. [DOI] [PubMed] [Google Scholar]
- Carew AM, Comiskey C, 2017. Treatment for opioid use and outcomes in older adults: a systematic literature review. Drug Alcohol Depend. 182, 48–57, [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2018. Treatment Episode Data Set (Admissions): TEDS-A 2004–2015. Retrieved from: https://wwwdasis.samhsa.gov/dasis2/teds.htm.
- Chang YP, Compton P, 2016. Opioid misuse/abuse and quality persistent pain management in older adults. J Gerontol Nurs. 42, 21–30. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, 2015. Abuse-deterrent formulations and the prescription opioid abuse epidemic in the United States: lessons learned from OxyContin. JAMA Psychiatry. 72, 424–430. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP, 2014. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 71, 821–826. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Surratt HL, Kurtz S, Ellis M, Inciardi JA, 2012. Patterns of prescription opioid abuse and comorbidity in an aging treatment population. J Subst Abuse Treat. 42, 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK, 2009. Estimating average annual per cent change in trend analysis. Stat Med. 28, 3670–3682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT, 2016. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 374, 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton BP, Bryson WC, Lohman MC, Brooks JM, Bruce ML, 2018. Characteristics of Medicaid recipients in Methadone Maintenance Treatment: A comparison across the lifespan. J Subst Abuse Treat. 92, 40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MA, Lin LA, Liu EL, Sites BD, 2017. Prescription Opioid Use among Adults with Mental Health Disorders in the United States. J Am Board Fam Med. 30, 407–417. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, 2012. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. The Lancet. 379, 55–70. [DOI] [PubMed] [Google Scholar]
- Dotson G, Duncan J, Ricks S, Bunton D, Davis S, Melvin A, 2013. Get ready for the boom: Why rehabilitation professionals should expect to see more older adults with addiction related disorders and what needs to be done to be prepared to serve them well. Journal of Addictive Behaviors, Therapy & Rehabilitation. 2, 1–9. [Google Scholar]
- Gerlach LB, Olfson M, Kales HC, Maust DT, 2017. Opioids and Other Central Nervous System-Active Polypharmacy in Older Adults in the United States. J Am Geriatr Soc. 65, 2052–2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Moos R, 2008. Substance misuse among older adults: a neglected but treatable problem. Addiction. 103, 347–348. [DOI] [PubMed] [Google Scholar]
- Han BH, Moore AA, Sherman S, Keyes KM., Palamar JJ, 2017a. Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005– 2014. Drug Alcohol Depend. 170, 198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Polydorou S, Ferris R, Blaum CS, Ross S, McNeely J, 2015. Demographic trends of adults in New York City opioid treatment programs-An aging population. Subst Use Misuse. 50, 1660–1667. [DOI] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM, 2017b. Prescription opioid use, misuse, and use disorders in US adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 167, 293–301. [DOI] [PubMed] [Google Scholar]
- Horgas AL, 2017. Pain management in older adults. Nurs Clin North Am. 52, el–e7. [DOI] [PubMed] [Google Scholar]
- Jones CM, 2017. The paradox of decreasing nonmedical opioid analgesic use and increasing abuse or dependence-an assessment of demographic and substance use trends, United States, 2003–2014. Addict Behav. 65, 229–235. [DOI] [PubMed] [Google Scholar]
- Jones CM, McAninch JK, 2015. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am J Prev Med. 49, 493–501. [DOI] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, Bohm MK, 2015. Vital Signs: Demographic and Substance Use Trends Among Heroin Users - United States, 2002–2013. MMWR Morb Mortal Wkly Rep. 64, 719–725. [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Cerda M, Brady JE, Havens JR, Galea S, 2014. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 104, e52–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehn BM, 2014. Driven by prescription drug abuse, heroin use increases among suburban and rural whites. JAMA. 312, 118–119. [DOI] [PubMed] [Google Scholar]
- Lofwall MR, Brooner RK, Bigelow GE, Kindbom K, Strain EC, 2005. Characteristics of older opioid maintenance patients. J Subst Abuse Treat. 28, 265–272. [DOI] [PubMed] [Google Scholar]
- Lofwall MR, Schuster A, Strain EC, 2008. Changing profile of abused substances by older persons entering treatment. J Nerv Ment Dis. 196, 898–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mital S, Windle M, Cooper HL, Crawford ND, 2018. Trends in non-medical prescription opioids and heroin co-use among adults, 2003–2014. Addict Behav. 86, 17–23. [DOI] [PubMed] [Google Scholar]
- Petry NM, 2002. A comparison of young, middle-aged, and older adult treatment-seeking pathological gamblers. Gerontologist. 42, 92–99. [DOI] [PubMed] [Google Scholar]
- Qato DM, Alexander GC, Conti RM, Johnson M, Schumm P, Lindau ST, 2008. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 300, 2867–2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao R, Roche A, 2017. Substance misuse in older people. BMJ. 358, j3885. [DOI] [PubMed] [Google Scholar]
- Schepis TS, McCabe SE, Teter CJ, 2018. Sources of opioid medication for misuse in older adults: results from a nationally representative survey. Pain. 159, 1543–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA), 2018. Medications for Opioid use Disorder. U.S. Department of Health and Human Services, Rockville, MD: Retrieved from: https://store.samhsa.gov/shin/content/SMA18-5063FULLDOC/SMA18-5063FULLDOC.pdf. [Google Scholar]
- United States Census Bureau, Age and Sex Tables. Retrieved from: https://www.census.gov/topics/population/age-and-sex/data/tables.html.
- Wang YP, Andrade LH, 2013. Epidemiology of alcohol and drug use in the elderly. Curr Opin Psychiatry. 26, 343–348. [DOI] [PubMed] [Google Scholar]
- Wu L, Blazer DG, 2011. Illicit and nonmedical drug use among older adults: a review. J Aging Health. 23, 481–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.