Abstract
Actinomycosis is caused by Gram-positive filamentous anaerobic organisms of genus Actinomyces, which are commensals of mucosal membranes of the oropharyngeal cavity, and gastrointestinal and genitourinary tracts. Central nervous system involvement is rare and may present as cerebral abscess, meningitis, meningoencephalitis, subdural empyema or epidural abscess. The radiological appearances of actinomycotic brain abscesses are not well recognized. Here, we present the characteristic imaging features of an actinomycotic brain abscess.
Clinical presentation
A 50-year-old male presented with a 2-day history of progressive difficulties with his speech. He reported no other relevant symptoms. His past medical history included ischaemic heart disease and cardiac stents. He smoked 20 cigarettes per day. There was no history of immunosuppression. Neurological examination revealed an alert patient with mild expressive dysphasia and right-sided facial weakness. The remainder of the physical examination was normal. He was apyrexial and the pulse rate, blood pressure and oxygen saturations were normal. Blood tests, including full blood count, urea and electrolytes, and liver function tests were normal. The C-reactive protein level was 29.6 mg l−1 (normal range 0–10 mg l−1).
Imaging findings
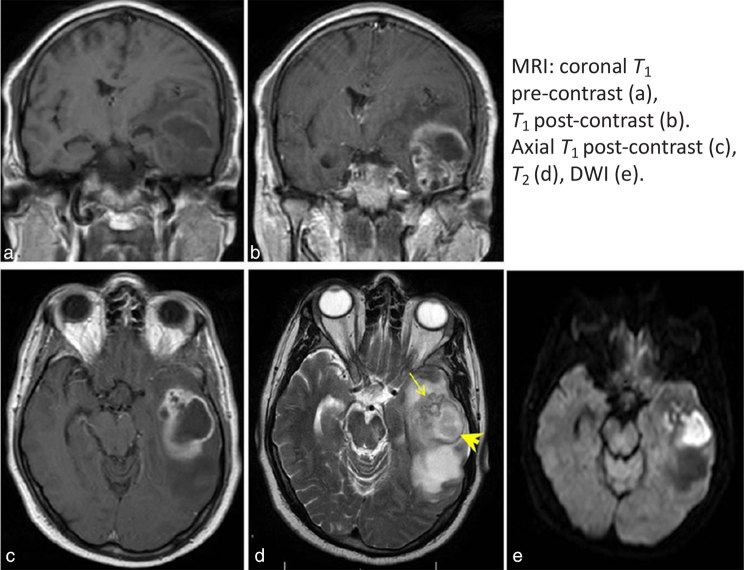
MRI demonstrated a large, peripherally enhancing thick-walled lesion in the left temporal lobe. The lesion comprised a larger cavity posteriorly and grape-like clustering anteriorly (Figure 1, arrow). The wall was T2 hypointense and T1 hyperintense (arrowhead) (Figure 1). The contents of the lesion showed restricted diffusion.
Figure 1.
There is a large, peripherally enhancing thick-walled lesion in the left temporal lobe. The lesion comprises a larger cavity posteriorly and grape-like clustering anteriorly (arrow). The wall is T2 hypointense and T1 hyperintense (arrowhead). The contents of the lesion show restricted diffusion, which is consistent with an abscess. The diagnosis is suggested by the grape-like cluster pattern with a T2 hypointense wall, which is a characteristic feature of an actinomycotic abscess. DWI, diffusion-weighted imaging.
The principal differential diagnosis of a peripherally enhancing lesion in the brain is between a necrotic or cystic tumour and an abscess. Radiological diagnosis of the lesion is important because it may influence the initial surgical strategy. Tumours typically present insidiously, whereas a cerebral abscess may present rapidly with clinical features of infection. The history and clinical examination may not, however, be suggestive, especially in abscesses caused by atypical organisms. Radiologically, an irregular peripheral enhancement pattern can be seen with high-grade intrinsic tumours such as glioblastoma multiforme. Pyogenic abscess walls are usually smooth and well defined with a disproportionate amount of oedema. Homogeneous restricted diffusion in a smooth-walled enhancing lesion is suggestive of a pyogenic abscess, whereas restricted diffusion related to a high-grade tumour is often heterogeneous.1 Infections that may appear similar to brain tumours on imaging include Actinomyces, Nocardia, tuberculous granuloma, neurocysticercosis and eumycetoma.
Treatment
The patient underwent stereotactic aspiration of the lesion and 16 ml of pus was aspirated. Cultures grew Actinomyces meyeri and Fusobacterium nucleatum. The treatment of actinomycotic brain abscess includes surgical aspiration and a substantive course of antibiotics.2 Our patient was treated with metronidazole and clindamycin following surgical aspiration. The abscess recurred after a month and required re-aspiration, but subsequently responded to further antibiotic treatment. We were unable to identify the source of infection in our patient, although periodontal disease, which is associated with smoking,3 may have played a role.
Discussion
There is a paucity of literature with focus on the radiological appearances of actinomycotic brain abscesses.4,5 Imaging descriptions in case reports often do not contain much detail on characteristic radiological features.6–8 Actinomycotic brain abscesses have been described as irregular, thick and nodular,5 or thin4,6 peripherally enhancing lesions4–9 with a hypointense core and a rim that is hyperintense on T1 non-contrast imaging4,5 and hypointense on T2 images.5 Restricted diffusion of the core is often seen4,5,7 but is not the rule.9 The periphery may not restrict the diffusion.4,5 In our patient, the diagnosis was suggested by the grape-like cluster pattern with a T2 hypointense wall, which is a characteristic feature of an actinomycotic abscess, which, to our knowledge, has not been reported in the literature. This imaging appearance was also well demonstrated in another patient treated in our department, a 60-year-old male with no relevant medical history who presented to our department with confusion and falls, and was found to have an actinomycotic brain abscess (A. meyeri). MRI showed the T2 hypointense grape-like clustering pattern in the right parietal lobe (Figure 2).
Figure 2.
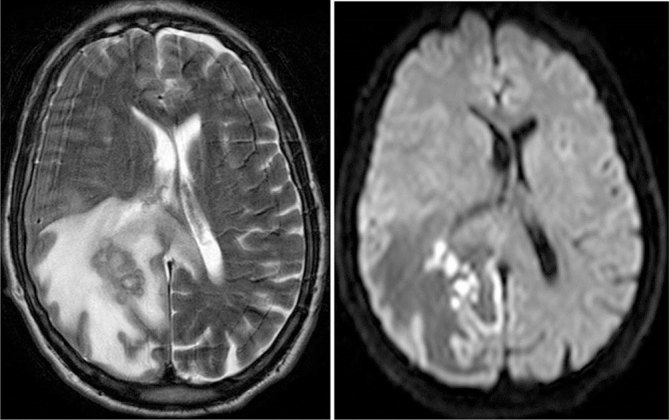
Axial T2 and diffusion-weighted MRI in a 60-year-old male with an actinomycotic brain abscess in the right parietal lobe with surrounding oedema. There is grape-like clustering with a T2 hypointense thick wall. The contents show restricted diffusion.
Actinomycosis is caused by Gram-positive filamentous anaerobic organisms of genus Actinomyces, which are commensals of mucosal membranes of the oropharyngeal cavity, and the gastrointestinal and genitourinary tracts.2,10 Actinomyces israelii is most commonly isolated in clinical infections. A. meyeri is less common but has a propensity to cause disseminated disease.2,11 Infection begins with a breach of the mucosa and is associated with poor dental hygiene, trauma and intrauterine devices. Infection is often polymicrobial and can be associated with Fusobacterium (as in this case)12 or other commensal organisms.2 Brain abscesses represent approximately two-thirds of central nervous system infections, the rest being meningitis, encephalitis, subdural empyema and epidural abscess.10 The organisms grow in clusters of tangled filaments and may exhibit an outer zone of granulation around the central purulent fluid, which contains tiny yellow clumps (“sulfur granules”) formed by a matrix of bacteria, calcium phosphate and host tissue.13 The granulation zone is usually very thick and consists of a highly cellular fibrous tissue containing collagen fibres, fibroblasts, capillaries and inflammatory cells, mainly lymphocytes and monocytes.14 We postulate that these pathological features may lead to the grape-like clustering pattern, although it is interesting that this imaging feature has not been reported in Nocardia and fungal infections that share similar morphological and pathological features.15
Learning points
Actinomycotic brain abscess is a rare but potentially life-threatening infection.
Actinomycotic brain abscesses appear on MRI as peripherally enhancing lesions that may exhibit a hyperintense rim on T1 non-contrast imaging and a grape-like cluster pattern with a T2 hypointense wall.
Consent
We were unable to obtain signed informed consent from our patient as the patient is deceased and attempts to contact the next of kin were unsuccessful. Exhaustive attempts have been made to contact the family and the paper has been sufficiently anonymized not to cause harm to the patient or his family.
Contributor Information
Maryam Rahiminejad, Email: Maryam.rahn@gmail.com.
Harutomo Hasegawa, Email: H.hasegawa@nhs.net.
Marios Papadopoulos, Email: Marios.papadopoulos@stgeorges.nhs.uk.
Andrew MacKinnon, Email: Andrew.Mackinnon@stgeorges.nhs.uk.
References
- 1.Omuro AM, Leite CC, Mokhtari K, Delattre JY. Pitfalls in the diagnosis of brain tumours. Lancet Neurol 2006; 5: 937–48. [DOI] [PubMed] [Google Scholar]
- 2.Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, et al. . Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist 2014; 7: 183–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sreedevi M, Ramesh A, Dwarakanath C. Periodontal status in smokers and nonsmokers: a clinical, microbiological, and histopathological study. Int J Dent 2012; 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang S, Wolf RL, Woo JH, Wang J, O'Rourke DM, Roy S, et al. . Actinomycotic brain infection: registered diffusion, perfusion MR imaging and MR spectroscopy. Neuroradiology 2006; 48: 346–50. [DOI] [PubMed] [Google Scholar]
- 5.Heo SH, Shin SS, Kim JW, Lim HS, Seon HJ, Jung SI, et al. . Imaging of actinomycosis in various organs: a comprehensive review. Radiographics 2014; 34: 19–33. [DOI] [PubMed] [Google Scholar]
- 6.Akhaddar A, Elouennass M, Baallal H, Boucetta M. Focal intracranial infections due to Actinomyces species in immunocompetent patients: diagnostic and therapeutic challenges. World Neurosurg 2010; 74: 346–50. [DOI] [PubMed] [Google Scholar]
- 7.Clancy U, Ronayne A, Prentice MB, Jackson A. Actinomyces meyeri brain abscess following dental extraction. BMJ Case Rep 2015; 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haggerty CJ, Tender GC. Actinomycotic brain abscess and subdural empyema of odontogenic origin: case report and review of the literature. J Oral Maxillofac Surg 2012; 70: e210℃e213. [DOI] [PubMed] [Google Scholar]
- 9.Ham HY, Jung S, Jung TY, Heo SH. Cerebral actinomycosis: unusual clinical and radiological findings of an abscess. J Korean Neurosurg Soc 2011; 50: 147–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smego RA. Actinomycosis of the central nervous system. Rev Infect Dis 1987; 9: 855–65. [DOI] [PubMed] [Google Scholar]
- 11.Fabbri G, Guardigni V, Sarubbo S, Cultera R, Contini C. Brain abscess sustained by Actinomyces meyeri in an immunocompetent patient. J Neurol Neurophysiol. 2014; 5: 184 [Google Scholar]
- 12.Honda H, Bankowski MJ, Kajioka EH, Chokrungvaranon N, Kim W, Gallacher ST. Thoracic vertebral actinomycosis: Actinomyces israelii and Fusobacterium nucleatum. J Clin Microbiol 2008; 46: 2009–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Dellen JR. Actinomycosis: an ancient disease difficult to diagnose. World Neurosurg 2010; 74: 263–4. [DOI] [PubMed] [Google Scholar]
- 14.Roth J, Ram Z. Intracranial infections caused by Actinomyces species. World Neurosurg 2010; 74: 261–2. [DOI] [PubMed] [Google Scholar]
- 15.Smego RA, Foglia G. Actinomycosis. Clin Infect Dis 1998; 26: 1255–63. [DOI] [PubMed] [Google Scholar]