Abstract
Background:
Distraction of the hip joint is a necessary step during hip arthroscopic surgery. The force of traction needed to distract the hip is not routinely measured, and little is known about which patient factors may influence this force.
Purpose:
To quantify the force of traction required for adequate distraction of the hip during arthroscopic surgery and explore the relationship between hip joint stiffness and patient-specific demographics, flexibility, and anatomy.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 101 patients (61 female) undergoing primary hip arthroscopic surgery were prospectively enrolled. A load cell attached to the traction boot continuously measured traction force. Fluoroscopic images were obtained before and after traction to measure joint displacement. The stiffness coefficient was calculated as the force of traction divided by joint displacement. Relationships between the stiffness coefficient and patient demographics and clinical parameters were investigated using a univariable regression model. The regression analysis was repeated separately by patient sex. Variables significant at P < .05 were included in a multivariable regression model.
Results:
The instantaneous peak force averaged 80 ± 18 kilogram-force (kgf), after which the force required to maintain distraction decreased to 57 ± 13 kgf. In univariable regression analysis, patient sex, alpha angle, hamstring flexibility, and Beighton hypermobility score were each correlated to stiffness. However, patient sex was the only significant variable in the multivariable regression model. Intrasex analysis demonstrated that increased hamstring flexibility correlated with decreased final holding stiffness in male patients and that higher Beighton scores correlated with decreased maximal stiffness in female patients.
Conclusion:
Male patients undergoing primary arthroscopic surgery have greater stiffness to hip distraction during arthroscopic surgery compared with female patients. In male patients, stiffness increased with decreasing hamstring flexibility. In female patients, increased Beighton scores corresponded to decreased stiffness. The presence of a labral tear was not correlated with stiffness to distraction. These data may be used to identify patients in whom a specific focus on capsular repair and/or plication may be warranted.
Keywords: hip arthroscopic surgery, femoroacetabular impingement, traction force, hip distraction, hip stiffness, patient characteristics
Distraction of the hip joint is necessary during arthroscopic procedures for orthopaedic surgeons to safely gain access to the central hip compartment.8 Traction forces commonly used for distraction are not routinely measured, as modern fracture tables with traction arms are not equipped with measurement devices. Increased traction forces are reported to cause complications, such as nerve injuries, skin necrosis, or tearing,2,14,24 and reports of traction forces measured with custom systems vary from 200 to 400 N.3,8,11
Many different variables may be associated with the amount of force needed to obtain necessary joint distraction during hip arthroscopic surgery. Patient factors such as age, sex, and body mass index (BMI) should be considered. Male sex and BMI have recently been shown to increase required traction forces.10 Hormonal variances between male and female patients have been associated with increased ligamentous laxity. In particular, higher serum relaxin concentrations in female patients have been suggested to influence hip distraction forces.6
Anatomic features may also affect the required force of traction. A borderline dysplastic acetabulum or a large cam/pincer lesion with limited internal rotation and capsular stiffness has the potential to decrease or increase traction force, respectively; however, this has not been specifically studied. Common radiographic measurements of femoroacetabular impingement (FAI) such as the lateral center-edge angle (LCEA) and alpha angle (AA) have not been correlated with traction forces during hip distraction. Additionally, biomechanical data have suggested that labral tears or labral insufficiency may increase hip instability and reduce hip distraction forces.5,17,21 However, these studies have not clinically evaluated the association of intraoperative labral tears with the traction force required for distraction during hip arthroscopic surgery. Finally, hip capsular laxity is increasingly recognized as a cause of atraumatic hip microinstability, which can be related to generalized ligamentous laxity, as confirmed by the Beighton hypermobility scale.4,9,15,19,20,22,23 The Beighton score has been shown to be predictive of hip capsular thickness7 but has not been correlated with the force of traction during hip arthroscopic surgery.
Overall, limited data have been collected to determine which factors influence the variability of traction forces among patients. Additionally, measurements of traction force alone do not account for differing amounts of distraction attained. A measurement of stiffness to account for both displacement and traction applied to the joint would provide a more complete description of the scenario. A deeper understanding of the variation in traction forces during distraction for hip arthroscopic surgery, and its correlation to patient factors, may deepen our understanding of how to prevent traction-related complications.
The specific aims of this study were 2-fold:
Establish a method for quantifying the stiffness coefficient of a hip during distraction by measuring the traction force applied and amount of distraction attained during hip arthroscopic surgery. Calculate 2 stiffness coefficients: k_max (the peak traction force divided by distraction) and k_hold (the holding force required to maintain distraction divided by distraction).
Determine if the stiffness coefficients vary with the following factors: (a) patient demographics (age, sex, BMI), (b) objective measures of joint hypermobility and hip microinstability (Beighton hypermobility scale, hamstring flexibility test), (c) hip radiographic osseous anatomy, and (d) presence of a labral tear.
We hypothesized that each of the variables contributes to hip stiffness during distraction.
Methods
Patient Population
This prospective study was approved by an institutional review board. All adult patients (≥18 years) undergoing primary hip arthroscopic surgery for the treatment of FAI during the study period (February 2015 to December 2016) by 1 of 2 fellowship-trained, high-volume orthopaedic surgeons (S.K.A., T.G.M.) specializing in hip arthroscopic surgery were eligible to participate in the study.
Inclusion/Exclusion Criteria
Inclusion criteria for this study were (1) subjective hip pain and a preoperative clinical diagnosis of FAI with a positive impingement (FADIR) test finding; (2) cam, pincer, or mixed FAI with a radiographic AA >55° or LCEA >40° or both, as directly measured on anteroposterior (AP) or lateral plain radiography or magnetic resonance imaging/computed tomography; (3) joint space preservation >2 mm; (4) Tönnis grade 0 or 1; and (5) age ≥18 years to <65 years. A labral tear or cartilage tear on magnetic resonance imaging was not used as an indication for surgical intervention, given the previously documented high prevalence of asymptomatic labral tears.16
Exclusion criteria for this study were (1) insufficient or incomplete preoperative AP and/or frog-leg radiographs, (2) a history of surgery on the affected hip, (3) a concomitant extra-articular injury requiring treatment (eg, gluteal tear), (4) other intra-articular lesions (eg, evidence of slipped capital femoral epiphysis, true dysplasia [LCEA <18° or LCEA of 18°-25° with increased Tönnis angle], Legg-Calve-Perthes disease, etc), or (5) symptomatic extra-articular impingement. Patients with incomplete standard-of-care data in their medical record required for analysis in this study (eg, preoperative examination or radiographic data) were also excluded (n = 85). One patient was excluded because his height prohibited integration of the load cell into the traction system.
Traction Measurement and Fluoroscopic Images
A custom attachment was created to allow integration of a 500-lb (226.8 kg) capacity S-type load cell (Model OP-312; Optima Scale Manufacturing) into the traction system (Advanced Supine Hip Positioning System; Smith & Nephew) (Figure 1). The patient was positioned on the surgical table and traction system. The pelvis was leveled, and the nonsurgical limb was secured with direct boot fixation after anesthesia induction and before the application of traction to the surgical limb. At this time, a fluoroscopic image was obtained to define the pretraction joint position. The position of the leg was maintained at a horizontal position (0°) for all images. To minimize the impact of the parallax effect, all images were obtained using the same fluoroscopic imaging machine (OEC 9800 Mobile C-arm; GE Healthcare) with identical magnification (normal) and collimation settings. Moreover, the beam height of the fluoroscopy machine was consistently maintained between patients by utilizing the distance between the image intensifier and surgical table base. This distance was maintained throughout imaging acquisition and provided a reproducible method of positioning to further minimize fluoroscopic imaging variability. Traction was then applied to the surgical limb by direct manual traction with the leg in a 30° abducted position, followed by adduction to neutral and fine traction if necessary.
Figure 1.
Image of the custom attachment that was created to allow integration of an S-type load cell into the traction system. The patient was positioned on the surgical table and traction system. After anesthesia induction, a fluoroscopic image was obtained to define the pretraction joint position. Traction was then applied to the surgical limb, and a second fluoroscopic image was acquired in the same plane to confirm that sufficient distraction had been achieved to allow completion of all components of hip arthroscopic surgery in the central compartment. Traction force was continuously measured through this process.
A second fluoroscopy image was acquired after final traction using the greater and lesser trochanteric comparative anatomy to confirm neutral rotation in the same plane and to confirm that sufficient distraction had been achieved to allow completion of all components of hip arthroscopic surgery in the central compartment. Distraction was deemed sufficient when safe arthroscopic entry into the hip joint was possible, including minimizing the risk of iatrogenic chondrolabral injuries. While interpatient variability existed, the typical femoroacetabular distraction distance was 10 to 15 mm. The force of traction was measured beginning before the application of traction, continuously measured throughout the application of traction, and for 5 minutes after the final traction application. As traction was applied, an audible and visible “pop” was typically observed and appeared to correspond to a peak in the force measurements. The maximum force recorded during the load cell’s continuous measurement was identified. Immediately after the peak, the force dropped to a point at which stress relaxation began (rate not evaluated). The initial force on this stress relaxation curve was recorded as the holding force. All traction measurements were obtained before any capsular penetration, venting, or arthrotomy.
Displacement
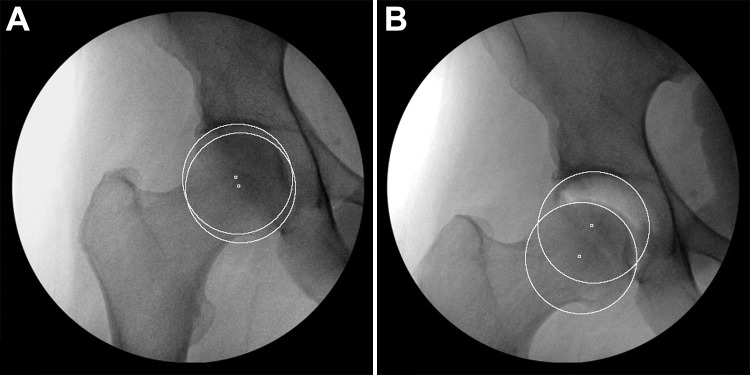
Fluoroscopic images of the joint in the pretraction and final distracted positions were imported into ImageJ (v 1.50i; National Institutes of Health) to determine displacement of the femoral head relative to the acetabulum (Figure 2). In the pretraction image, a best-fit circle was drawn around the femoral head and then translated to the inner edge of the sourcil. The distance between circles was divided by the diameter of the circle and recorded as the normalized distance between the femoral head and acetabulum. This process was repeated for the distracted image. Displacement due to traction was calculated as the normalized distance in the distracted image minus the normalized distance in the pretraction image.
Figure 2.
Illustration of the method to measure displacement using intraoperative fluoroscopic images of the joint in (A) pretraction and (B) final distracted positions. Example from a 45-year-old male patient undergoing primary arthroscopic surgery. In the pretraction image, a best-fit circle was drawn around the femoral head and then translated to the inner edge of the sourcil. The distance between circles was divided by the diameter of the circle and recorded as the normalized distance between the femoral head and acetabulum. This process was repeated for the distracted image. The displacement due to traction was calculated as the normalized distance in the distracted image minus the normalized distance in the pretraction image.
Stiffness Coefficient
The stiffness coefficient of the joint (k) was calculated following a modified version of the Hooke law, F = kx, where F is the traction force and x is the normalized displacement of the femoral head. Two stiffness values were calculated at the final displacement value using the maximum distraction force (resulting in k_max), which occurred during traction application, and the holding force (resulting in k_hold), which occurred immediately after traction completion.
Chart Data
The electronic medical record of each study participant was reviewed to retrieve demographic information including age, sex, and BMI. Preoperative clinic notes were reviewed for results of the Beighton hypermobility scale, which is a test frequently used to assess joint hypermobility,20 and the hamstring flexibility test in passive knee extension, in which higher angles correspond to decreased flexibility.1,12 Intraoperative notes were reviewed to determine the presence or absence of a labral tear.
Radiographic Measurements
Preoperative imaging was also performed to assess joint anatomy using radiographic measurements including the LCEA of Wiberg25 on AP pelvis radiography and the maximum AA on 45° Dunn lateral radiography.18 All measurements were completed by the corresponding author (T.G.M.). The repeatability of these radiographic measurements has been previously reported.26
Statistical Analysis
Univariable linear regression was performed with the stiffness coefficient (k_max or k_hold) as the dependent variable and each of the following independent variables: age, sex, BMI, operating physician, Beighton hypermobility score, hamstring flexibility, AA, LCEA, and presence of a labral tear. For dichotomous independent variables (eg, sex, operating physician, labral tear), the P value resulting from linear regression was equivalent to that from an independent t test, and the slope represents the mean difference.
Independent variables that were significant at P < .05 in the univariable linear regression model were combined in a multivariable linear regression model. As sex was the only significant predictor in the multivariable linear regression model, the univariable linear regression analysis described above was then repeated separately for men and women.
Two reviewers (A.L.K., T.F.A.) independently completed the displacement measurements on 26 randomly selected participants. The intraclass correlation coefficient was calculated to quantify interobserver repeatability. All statistical analyses were completed in Stata/MP 13.1 (StataCorp).
Results
Overall, 101 patients (61 women, 40 men) undergoing primary arthroscopic surgery were included in this study (Table 1). The instantaneous peak force required to distract the hip averaged 80 ± 18 kilogram-force (kgf) and was often associated with a visible or audible “pop,” after which the force required to maintain sufficient space in the hip joint decreased to 57 ± 13 kgf and subsequently slowly decreased with stress relaxation. The displacement of the femoral head relative to the acetabulum averaged 21% ± 3.7% of the diameter of the femoral head. These measurements resulted in a mean k_max of 387 ± 113 kgf/% distraction and a mean k_hold of 275 ± 79 kgf/% distraction.
TABLE 1.
Demographics and Traction Results by Sexa
| Variable | Males (n = 40) | Females (n = 61) |
|---|---|---|
| Age, y | 35 ± 11 (18-54) | 33 ± 10 (18-64) |
| BMI, kg/m2 | 27.0 ± 4.4 (20.9-42.4) | 25.5 ± 5.7 (18.3-45.2) |
| LCEA on AP radiography, deg | 27 ± 5.5 (18-38) | 26 ± 6.7 (19-45) |
| AA on 45° Dunn lateral radiography, deg | 62 ± 11.0 (41-80) | 49 ± 9.1 (35-70) |
| Beighton score | 0.2 ± 0.5 (0-2) | 1.9 ± 2.8 (0-9) |
| Hamstring flexibility, deg | 51 ± 21 (5-110) | 27 ± 20 (0-75) |
| Presence of a labral tear, n (%) | 31 (78) | 38 (62) |
| Final traction force, kgf | 66 ± 12 (45-97) | 51 ± 10 (36-84) |
| Maximum traction force, kgf | 91 ± 16 (61-134) | 72 ± 16 (39-112) |
| Distraction, % of femoral head diameter | 20 ± 2.9 (13-26) | 22 ± 3.9 (15-31) |
| k_max, kgf/% of femoral head diameter | 465 ± 97 (278-762) | 335 ± 91 (205-663) |
| k_hold, kgf/% of femoral head diameter | 335 ± 70 (209-526) | 236 ± 58 (156-431) |
aData are shown as mean ± SD (range) unless otherwise indicated. AA, alpha angle; AP, anteroposterior; BMI, body mass index; LCEA, lateral center-edge angle.
In univariable regression analysis, sex, AA, hamstring flexibility, and Beighton score were each correlated with k_hold (Table 2) as well as k_max (Table 3). Specifically, male sex, AA, and hamstring flexibility (in which greater angles indicated decreased flexibility) were positively correlated with the stiffness coefficient, while the Beighton score (in which increased values indicate increased hypermobility) was negatively correlated.
TABLE 2.
Linear Regression Results for k_hold (Dependent Variable) in Primary Arthroscopic Surgerya
| Variable | Univariable Regression in All Primary Cases (N = 101) |
Multivariable Regression in All Primary Cases (N = 101) | Univariable Regression in All Female Primary Cases (n = 61) |
Univariable Regression in All Male Primary Cases (n = 40) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Regression Coefficient (Slope) |
r 2 | P | Regression Coefficient (Slope) |
P | Regression Coefficient (Slope) |
r 2 | P | Regression Coefficient (Slope) |
r 2 | P | |
| Sex (female = 0, male = 1) | 99.7 | 0.38 | <.001 | 70.4 | <.001 | ||||||
| AA on 45° Dunn lateral radiography | 3.0 | 0.20 | <.001 | 0.9 | .165 | 0.8 | 0.01 | .360 | 1.3 | 0.04 | .195 |
| Hamstring flexibility | 1.5 | 0.18 | <.001 | 0.4 | .24 | 0.6 | 0.04 | .122 | 0.5 | 0.02 | .347 |
| Beighton score | –13.3 | 0.15 | <.001 | –5.3 | .074 | –6.0 | 0.08 | .023 | –32.6 | 0.06 | .120 |
| LCEA on AP radiography | 1.8 | 0.02 | .166 | 0.9 | 0.01 | .402 | 1.0 | <0.01 | .629 | ||
| BMI | 1.7 | 0.01 | .266 | 0.9 | <0.01 | .501 | –0.9 | <0.01 | .736 | ||
| Surgeon (S.K.A. = 0, T.G.M. = 1) | 18.6 | 0.01 | .288 | –15.9 | 0.01 | .358 | 34.4 | 0.03 | .138 | ||
| Labral tear (no = 0, yes = 1) | 15.6 | <0.01 | .359 | 12.8 | 0.01 | .404 | –29.8 | 0.03 | .264 | ||
| Age | 0.2 | <0.01 | .831 | –0.4 | <0.01 | .612 | –0.3 | <0.01 | .750 | ||
aBolded values indicate statistical significance. AA, alpha angle; AP, anteroposterior; BMI, body mass index; LCEA, lateral center-edge angle.
TABLE 3.
Linear Regression Results for k_max (Dependent Variable) in Primary Arthroscopic Surgerya
| Variable | Univariable Regression in All Primary Cases (N = 101) |
Multivariable Regression in All Primary Cases (N = 101) | Univariable Regression in All Female Primary Cases (n = 61) |
Univariable Regression in All Male Primary Cases (n = 40) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Regression Coefficient (Slope) |
r 2 | P | Regression Coefficient (Slope) |
P | Regression Coefficient (Slope) |
r 2 | P | Regression Coefficient (Slope) |
r 2 | P | |
| Sex (female = 0, male = 1) | 130.0 | 0.32 | <.001 | 88.4 | .001 | ||||||
| AA on 45° Dunn lateral radiography | 3.8 | 0.16 | <.001 | 0.9 | .328 | 2.4 | 0.06 | .058 | –0.2 | 0.001 | .890 |
| Hamstring flexibility | 2.1 | 0.19 | <.001 | 0.8 | .096 | 0.6 | 0.02 | .267 | 1.5 | 0.103 | .043 |
| Beighton score | –17.4 | 0.13 | <.001 | –6.3 | .149 | –8.2 | 0.06 | .050 | –33.9 | 0.035 | .251 |
| LCEA on AP radiography | 1.6 | <0.01 | .373 | 1.5 | 0.01 | .397 | –1.5 | 0.008 | .591 | ||
| BMI | 1.3 | <0.01 | .554 | –0.2 | <0.01 | .933 | –1.1 | 0.002 | .770 | ||
| Surgeon (S.K.A. = 0, T.G.M. = 1) | 14.9 | <0.01 | .551 | 3.8 | <0.01 | .890 | –6.8 | 0.001 | .836 | ||
| Labral tear (no = 0, yes = 1) | 22.7 | 0.01 | .349 | 28.8 | 0.02 | .232 | –56.4 | 0.060 | .128 | ||
| Age | 0.6 | <0.01 | .607 | 0.0 | <0.01 | .973 | –0.3 | 0.001 | .819 | ||
aAA, alpha angle; AP, anteroposterior; BMI, body mass index; LCEA, lateral center-edge angle.
Sex was the only variable that remained significant in the multivariable regression model for both k_hold (Table 2) and k_max (Table 3). In univariable regression analysis conducted separately for male and female patients undergoing primary arthroscopic surgery, the Beighton score was significantly correlated with k_hold in women (P = .023) (Table 2), and hamstring flexibility was significant correlated with k_max in men (P = .043) (Table 3).
The intraclass correlation coefficient for the radiographic displacement measurement was 0.93 (95% CI, 0.85-0.97), suggesting excellent interobserver repeatability of this measurement.
Discussion
Our study demonstrated that the main predictor of variation in the stiffness coefficient during primary hip arthroscopic surgery was patient sex, with men demonstrating greater stiffness. While male sex, increased AA, lower Beighton score, and decreased hamstring flexibility were each individually correlated to increased stiffness coefficients in univariable regression, only sex remained significant in multivariable regression. This is likely because the other variables (AA, Beighton score, and hamstring flexibility) notably differed between sexes. For example, the maximum Beighton score in men was 2, while it was 9 in women. Similarly, AA and hamstring flexibility were both substantially higher in the male patients compared with the female patients. The finding that male sex is the only significant predictor of stiffness in primary arthroscopic surgery is similar to that found by Ellenrieder et al,10 who demonstrated a significantly increased force needed to obtain hip distraction at the time of arthroscopic surgery in male patients. While little data exist regarding the cause of the differences between male and female hip laxity, the data in this study suggest that, on average, female patients require less traction force to achieve an equivalent normalized distraction measurement. However, the increased stiffness observed in men may in part be because of the normalization of the distraction measurement to the diameter of the femoral head. Because men are typically larger, on average, than women, their normalized distances may have been smaller than those for women for the same physical distance, resulting in increased stiffness coefficients.
The observations that increased Beighton scores correlated with decreased values of k_hold in female patients undergoing primary arthroscopic surgery and that decreased hamstring flexibility correlated with decreased values of k_hold in male patients undergoing primary arthroscopic surgery are not surprising. High Beighton scores are found in patients with notable hypermobility, such as patients with collagen disorders (eg, Ehlers-Danlos syndrome). In such patients, increased collagen elasticity in the tissue surrounding the hip would require less force for distraction. While male patients with high Beighton scores indicative of collagen disorders would be expected to demonstrate decreased joint stiffness during distraction, similar to their female counterparts, this variable was not detected as significant in the male cohort, likely because of the lack of male patients with a Beighton score >2 in the present study. While Beighton scores were low in the male cohort, the male patients did demonstrate variation in hamstring flexibility, which was found to be correlated with k_max. Here, the hamstring flexibility test was used as a surrogate to understand general soft tissue flexibility around the hip. It is logical then that those with decreased flexibility on examination would demonstrate greater stiffness in response to intraoperative distraction. This information is clinically useful to the surgeon who can counsel male patients with low Beighton scores and decreased hamstring flexibility that they may require increased traction force to adequately distract the hip, thereby potentially increasing the risk of nerve injuries24 including pudendal nerve palsy, among others.
The traction force was recorded at 2 distinct points during distraction. The audible and visible pop during the application of traction corresponded to a peak in the force measurements, of which the maximum force was recorded for the calculation of k_max. Immediately after the peak, the force dropped to a point at which stress relaxation began, and the initial force on this stress relaxation curve was recorded as the holding force and used in the calculation of k_hold. The factors influencing the peak and holding forces are multifactorial and certainly seem to be correlated with markers of general flexibility and hypermobility, discussed above. In addition, the acetabular labrum has been discussed as a contributor to hip stability, with a suggested function in forming a suction seal in the joint.5,21 If this suction seal is indeed present, it would have to be disrupted to achieve sufficient distraction during hip arthroscopic surgery. The audible and visible pop observed at the time of hip distraction may represent this disruption. Venting the joint before the application of traction may result in less force required to disrupt the suction seal, but the effects of venting were not studied at this time.
Data from cadaveric studies suggest that damage to the labrum may compromise its function in the suction seal. Crawford et al5 reported that the forces required to distract the hip joint to 3 mm decreased by 60% with a 1.5-cm tear at the chondral labral junction. However, the force was only reduced by 51% at 5 mm of distraction and was assumed by the authors to be caused by disruption of the suction seal at this distance of distraction. Philippon et al21 reported significantly less distraction force with complete labral resection but found no significant difference in the distraction force needed to disrupt the suction seal with a 3.5-cm tear. This is similar to the results of the present study, in which clinically relevant labral tears observed at the time of arthroscopic surgery were not correlated with stiffness to distraction. Therefore, at large distractions, damage to the labrum may not affect the suction seal or joint stability. However, it may still influence stability and stiffness during motions and forces within the range of normal activity.
In the patients of the present study, the maximum force during distraction averaged 80 kgf (785 N), and the holding force required to maintain sufficient distraction averaged 57 kgf (559 N), both of which are higher than values previously reported in the literature. Griffin et al13 reported that a force of 200 to 300 N was needed to obtain adequate joint distraction to access the hip, although the authors did not mention whether this was the peak force or holding force. Ellenrieder et al10 specifically measured the “initial” traction force at the point of at least 10 mm of joint distraction and reported a mean value of 477 N. As the peak force was not recorded by those authors, this value may be compared with the holding force in the current study. The differences between forces could possibly be explained by differences in traction methods or distraction preferences between surgeons or characteristics of the patients being evaluated.
Limitations
This study has a number of limitations. First, the desired distraction distance and the exact method of manual application of traction may have differed between the 2 orthopaedic surgeons who performed the application of traction in this study. However, the stiffness coefficient calculated in this study utilized patient-specific osseous anatomy and distraction distance to normalize measurements between the 2 surgeons and across participants. By using the stiffness coefficient instead of the traction force in interparticipant comparisons, the effect of differences in the distraction distance was minimized. Further, operating physician (surgeon) was included as a covariate in regression analysis to account for differences in traction preferences. Second, because force was only measured in 1 direction, it was not possible to calculate a 3-dimensional stiffness matrix. The stiffness reported in this study represents the hip’s resistance to a force applied longitudinally and does not account for lateral forces imposed by the perineal post during hip adduction. Third, the overall traction force is also distributed over the ankle and knee joints, and there may also be some slippage between the foot and the traction boot. Therefore, the measured traction force represents a conservative maximum of the force distributed over the hip. Fourth, while we acknowledge that pelvic shift occurs during traction application, the pelvis was leveled, and the nonsurgical limb was secured equally among all patients. Moreover, pelvic shift during traction occurs before distraction of the joint, and thus, the traction forces and stiffness coefficient should not be affected by pelvic tilt when accounting for the final distraction distance and traction force. Next, the AA and LCEA were only obtained from 2-dimensional radiographs, as preoperative 3-dimensional images were not available for all patients. Last, differences in muscle volume may partially explain the differences in stiffness between sexes. However, muscle volume was not measured in the present study.
Conclusion
Male patients undergoing primary arthroscopic surgery have greater stiffness to hip distraction during arthroscopic surgery compared with female patients. In male patients, stiffness increased with decreasing hamstring flexibility. In female patients, increased Beighton scores corresponded to decreased stiffness.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This investigation was supported by the University of Utah Population Health Research and Population Health Research Foundation for Discovery, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764). S.K.A. is a consultant for Stryker and Pivot Medical and has received hospitality payments from Aesculap Biologics and Stryker. T.G.M. is a paid speaker/presenter for Arthrex and has received hospitality payments from Arthrex and Aesculap Biologics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Utah Institutional Review Board (#74533).
References
- 1. Bandy WD, Irion JM, Briggler M. The effect of time and frequency of static stretching on flexibility of the hamstring muscles. Phys Ther. 1997;77(10):1090–1096. [DOI] [PubMed] [Google Scholar]
- 2. Brumback RJ, Ellison TS, Molligan H, Molligan DJ, Mahaffey S, Schmidhauser C. Pudendal nerve palsy complicating intramedullary nailing of the femur. J Bone Joint Surg Am. 1992;74(10):1450–1455. [PubMed] [Google Scholar]
- 3. Byrd JW. Hip arthroscopy: the supine position. Clin Sports Med. 2001;20(4):703–731. [PubMed] [Google Scholar]
- 4. Charbonnier C, Kolo FC, Duthon VB, et al. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011;39(3):557–566. [DOI] [PubMed] [Google Scholar]
- 5. Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award: the biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22. [DOI] [PubMed] [Google Scholar]
- 6. Dehghan F, Haerian BS, Muniandy S, Yusof A, Dragoo JL, Salleh N. The effect of relaxin on the musculoskeletal system. Scand J Med Sci Sports. 2014;24(4):e220–e229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Devitt BM, Smith BN, Stapf R, Tacey M, O’Donnell JM. Generalized joint hypermobility is predictive of hip capsular thickness. Orthop J Sports Med. 2017;5(4):2325967117701882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dienst M, Seil R, Gödde S, et al. Effects of traction, distension, and joint position on distraction of the hip joint: an experimental study in cadavers. Arthroscopy. 2002;18(8):865–871. [DOI] [PubMed] [Google Scholar]
- 9. Duthon VB, Charbonnier C, Kolo FC, et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy. 2013;29(3):411–419. [DOI] [PubMed] [Google Scholar]
- 10. Ellenrieder M, Tischer T, Bader R, Kreuz PC, Mittelmeier W. Patient-specific factors influencing the traction forces in hip arthroscopy. Arch Orthop Trauma Surg. 2017;137(1):81–87. [DOI] [PubMed] [Google Scholar]
- 11. Eriksson E, Arvidsson I, Arvidsson H. Diagnostic and operative arthroscopy of the hip. Orthopedics. 1986;9(2):169–176. [DOI] [PubMed] [Google Scholar]
- 12. Gajdosik RL, Rieck MA, Sullivan DK, Wightman SE. Comparison of four clinical tests for assessing hamstring muscle length. J Orthop Sports Phys Ther. 1993;18(5):614–618. [DOI] [PubMed] [Google Scholar]
- 13. Griffin DR, Villar RN. Complications of arthroscopy of the hip. J Bone Joint Surg Br. 1999;81(4):604–606. [DOI] [PubMed] [Google Scholar]
- 14. Harris JD, McCormick FM, Abrams GD, et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29(3):589–595. [DOI] [PubMed] [Google Scholar]
- 15. Larson CM, Giveans MR, Samuelson KM, Stone RM, Bedi A. Arthroscopic hip revision surgery for residual femoroacetabular impingement (FAI): surgical outcomes compared with a matched cohort after primary arthroscopic FAI correction. Am J Sports Med. 2014;42(8):1785–1790. [DOI] [PubMed] [Google Scholar]
- 16. Lee AJ, Armour P, Thind D, Coates MH, Kang AC. The prevalence of acetabular labral tears and associated pathology in a young asymptomatic population. Bone Joint J. 2015;97-B(5):623–627. [DOI] [PubMed] [Google Scholar]
- 17. Lertwanich P, Plakseychuk A, Kramer S, et al. Biomechanical evaluation contribution of the acetabular labrum to hip stability. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2338–2345. [DOI] [PubMed] [Google Scholar]
- 18. Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. [DOI] [PubMed] [Google Scholar]
- 19. Mitchell RJ, Gerrie BJ, McCulloch PC, et al. Radiographic evidence of hip microinstability in elite ballet. Arthroscopy. 2016;32(6):1038–1044. [DOI] [PubMed] [Google Scholar]
- 20. Naal FD, Hatzung G, Muller A, Impellizzeri F, Leunig M. Validation of a self-reported Beighton score to assess hypermobility in patients with femoroacetabular impingement. Int Orthop. 2014;38(11):2245–2250. [DOI] [PubMed] [Google Scholar]
- 21. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal, part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722–729. [DOI] [PubMed] [Google Scholar]
- 22. Shu B, Safran MR. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30(2):349–367. [DOI] [PubMed] [Google Scholar]
- 23. Smith MV, Sekiya JK. Hip instability. Sports Med Arthrosc. 2010;18(2):108–112. [DOI] [PubMed] [Google Scholar]
- 24. Telleria JJ, Safran MR, Harris AH, Gardi JN, Glick JM. Risk of sciatic nerve traction injury during hip arthroscopy: is it the amount or duration? An intraoperative nerve monitoring study. J Bone Joint Surg Am. 2012;94(22):2025–2032. [DOI] [PubMed] [Google Scholar]
- 25. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand Suppl. 1939;58:7–135. [Google Scholar]
- 26. Wylie JD, Kapron AL, Peters CL, Aoki SK, Maak TG. Relationship between the lateral center-edge angle and 3-dimensional acetabular coverage. Orthop J Sports Med. 2017;5(4):2325967117700589. [DOI] [PMC free article] [PubMed] [Google Scholar]