Abstract
Despite 2 decades of effort by the public health community to combat obesity, obesity rates in the United States continue to rise. This lack of progress raises fundamental questions about the adequacy of our current approaches. Although the causes of population-wide obesity are multifactorial, attention to food systems as potential drivers of obesity has been prominent. However, the relationships between broader food systems and obesity are not always well understood. Our efforts to address obesity can be advanced and improved by the use of systems approaches that consider outcomes of the interconnected global food system, including undernutrition, climate change, the environmental sustainability of agriculture, and other social and economic concerns. By implementing innovative local and state programs, taking new approaches to overcome political obstacles to effect policy, and reconceptualizing research needs, we can improve obesity prevention efforts that target the food systems, maximize positive outcomes, and minimize adverse consequences. We recommend strengthening innovative local policies and programs, particularly those that involve community members in identifying problems and potential solutions and that embrace a broad set of goals beyond making eating patterns healthier. We also recommend undertaking interdisciplinary research projects that go beyond testing targeted interventions in specific populations and aim to build an understanding of the broader social, political, and economic context.
Keywords: obesity, healthy eating, food systems, systems science, systems approaches
Rates of overweight and obesity have increased sharply worldwide since the 1980s.1,2 Worldwide, 39% of adults were overweight (ie, had body mass index [BMI] ≥25 kg/m2) and 13% were obese (ie, had BMI ≥30 kg/m2) in 2016, compared with 22% overweight and 5% obese in 1980.1,2 Obesity rates in the United States (40% of adults aged ≥20 were obese in 2015-2016) are substantially higher than the global average, with higher rates of obesity seen in some racial/ethnic minority populations.3 In 2015, rates of obesity in adults aged ≥18 were 40% among African American adults, 44% among American Indian/Alaska Native adults, 33% among Hispanic/Latino adults, and 35% among Native Hawaiian/Pacific Islander adults, compared with 29% among non-Hispanic white adults.4-7 Among children and teenagers aged 2-19, 19% were also obese during 2015-2016.3 High rates of overweight and obesity have substantial consequences for public health. For example, overweight and obesity are associated with cardiovascular disease, diabetes, kidney disease, and several kinds of cancer, and high BMI contributed to an estimated 4.0 million deaths globally in 2015.8
Increases in obesity prevalence are caused by the overconsumption of calories relative to energy expenditure; the relative importance of changes in energy expenditure compared with changes in energy intake is less certain.9,10 With regard to energy intake, people in the United States consume 23% more calories on average than they did in 1970.11 These excess calories are a function of both the type and quantity of food consumed. The quality of diets of people in the United States falls short of federal dietary recommendations: the diets of 91% of people in the United States do not include the recommended amount of fruit and vegetables, and most people in the United States consume more than the recommended amount of sodium and added sugars.12,13 Factors linked to caloric consumption, weight gain, and obesity include sugar consumption, increased portion sizes, the low relative price of energy-dense foods, food marketing (ie, the types of products, where they are available, and how they are promoted and priced), and increased consumption of food away from home.14 Sugar-sweetened beverages are a major source of added sugars and calories, adding an average of 138 calories to the daily diet of US adults.15
Food systems are potential drivers of obesity. In this article, we refer to a food system as “all the elements (environment, people, inputs, processes, infrastructures, institutions) and the activities that relate to the production, processing, distribution, preparation, and consumption of food, as well as the output of these activities, including socioeconomic and environmental outcomes.”16 As the food energy supply in various countries has increased, the average body weight in those countries has also increased.17 As the characteristics of food systems have changed, such as the increased processing of food and improved food distribution, convenient, energy-dense foods have become more available and they are heavily promoted to appeal to consumers.18-20 Because repeated exposure and familiarity with tastes creates a preference for those tastes, the prevalence of energy-dense foods has presumably encouraged the formation of preferences for those foods.21 Concurrently, portion sizes have increased, with larger portions linked to greater consumption.22-24 In addition, prices of energy-dense manufactured foods have fallen compared with the prices of less energy-dense foods, such as fruit and vegetables, and this price discrepancy has also contributed to caloric overconsumption.25,26
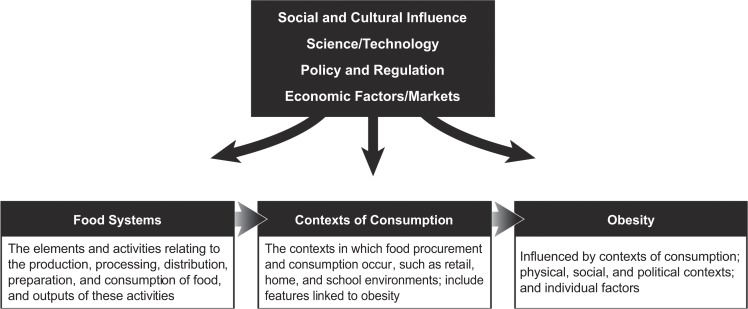
Contexts of consumption—those contexts in which food procurement and consumption occur, such as retail, home, and school environments—are embedded within larger food systems. The prevailing view in public health is that features of food systems push excess calories and lower-quality food into contexts of consumption in ways that lower the average person’s ability to avoid overconsumption (Figure). However, before this prevailing view can be used as the basis of major food system interventions, it must be corroborated. New research approaches are needed to better understand how food systems behave holistically and how they affect consumption and obesity.
Figure.
Hypothetical relationship among food systems, contexts of consumption, and obesity: food systems affect the contexts of consumption embedded within them in ways that drive overconsumption and lead to obesity.
The US food system is poorly aligned with current recommendations for healthy eating.14,27 Consider, for example, the 2015 US dietary recommendation to consume 4½ cups of fruit and vegetables daily.13 All along the food-supply chain, there is a misalignment between this recommendation and the realities of the US food system: not enough fruit and vegetables are produced for everyone to eat the recommended amount, energy-dense foods such as candy and sugar-sweetened beverages are widely available in retail environments, and fruit and vegetables are not as heavily marketed as many other foods.14
Unanswered Questions
Food systems plausibly do shape contexts of consumption in ways that cause overconsumption and poor dietary quality, but the causal relationships are not well understood. Many questions must be answered. What food system features are most strongly related to caloric overconsumption and obesity? Would certain changes to food systems help improve consumption patterns in certain populations? How do the causal pathways work, and what are the most feasible, effective, and sustainable points of intervention from a whole society and systems perspective? Would certain combinations of interventions act synergistically?
We must recognize the effects of the interconnected global food system on the US context, and vice versa. Interventions targeting the US food system are complicated, in part because they may implicate other global health, environmental, and social problems. For example, despite high worldwide rates of obesity, the rates of hunger are also substantial. In 2016, an estimated 11% of the global population, or 815 million people, were undernourished (ie, they were unable to acquire enough food to meet dietary energy requirements).28 In addition, some food systems may have environmental costs, because food systems worldwide account for a high proportion (19%-33%) of all global greenhouse gas emissions and use 40% of the world’s land area.29-31 Thus, it is important to recognize the global effects of interventions aimed at the US food system. Sometimes, US policy recommendations designed to mitigate obesity can have unintended adverse global health, environmental, economic, or social consequences. For example, US dietary recommendations to consume more fish could, if followed, deplete global fish supplies and threaten fishers’ livelihoods.14
Ideally, efforts to improve diets can support the positive environmental, economic, and social outcomes produced by food systems. For example, policies that reduce consumption of red meat while also increasing fruit and vegetable consumption may achieve environmental and health benefits for many populations.32
A US Public Health Agenda on Obesity and Food Systems: The Importance of a Systems Approach
New approaches are needed to reduce the rates of obesity and minimize the unintended consequences of interventions in US food systems. The public health tools needed to do this—policies, local programs, and research—should be reconceptualized to work at multiple levels, including the individual, family, community, and society levels, as well as for localities, nations, and the global community. They should reach beyond public health to other sectors, such as education, planning, and economic development, as well as other government agencies and nongovernmental organizations.33,34
Systems Approaches
Applying a systems approach to a problem means understanding that the problem is part of a system with many interrelated parts and recognizing that this system may work in surprising ways. Sometimes, for example, an effort might be intuitively compelling, but it might backfire or produce unintended consequences, both positive and negative, elsewhere in the system.
The field of systems science has developed qualitative and quantitative methods, including methods for mapping and modeling systems.35,36 During the past decade, obesity researchers have begun to use the kinds of systems approaches used successfully in mathematics, engineering, the social sciences, and other areas of public health, and an even greater use of these approaches would be beneficial.14,21,33,37-44 These approaches can, for example, help identify the relationships between food systems and patterns of food consumption and design new policies. In addition, systems approaches can assist in designing interventions that modify the drivers of overconsumption while minimizing unintended consequences, such as adverse health, environmental, and economic effects.14
Systems approaches are being used to design obesity interventions, food system policies, and other public health interventions, to identify the most effective places to intervene in systems, to model potential consequences of interventions, and to identify sets of interventions in which the interventions reinforce rather than undermine one another (Box).14,21,33,35,40,45,46 Systems methods also are being used to monitor and evaluate obesity interventions,46,49-51 to understand how social relationships and networks operate, to explore how this operation can be leveraged to improve outcomes,52,53 and to understand important social, economic, and political contexts. These methods also can be used to identify political obstacles to progress, policies that might alienate potential supporters, and policies that might build a broad alliance beyond public health.
Box.
Potential uses of systems approaches in obesity and food system efforts
Systems approaches may enhance work on obesity and food systems by helping researchers and practitioners to:
Understand the relationships between food environments and broader contexts, including food systems
Understand the relevant features of a food system and how they relate to one another
Identify intervention targets or policy goals that multiple stakeholder groups have in common or that will address multiple food system problems simultaneously; for example, reducing consumption of red meat to pursue environmental, health, and animal welfare gains
Design policies or interventions that accomplish multiple goals; for example, design policies to promote dietary patterns that are both healthy and environmentally sustainable32
Use systems-based community engagement strategies to engage community members in identifying the causes of, and potential solutions to, the problem of obesity and in designing community-built action plans45-47
Design policies or interventions that appeal to multiple stakeholder groups outside of public health; for example, allocating revenue from a tax on sugar-sweetened beverages to educational programs supported by stakeholder groups
Design a multipronged intervention or set of policies that mutually reinforce and support each other; for example, in Massachusetts, the Shape Up Somerville program (2002-2005) used strategies intended to work synergistically to increase physical activity and healthy eating at schools, reinforced by changes within the home and community48
Foresee policies’ unintended consequences on broader food systems, assess the acceptability of these consequences, and minimize them as needed14
Identify political obstacles to policy adoption by identifying groups that may be negatively affected by the policy, such as companies or workers who may lose income because of dietary shifts
Identify a coalition of stakeholder groups that share the policy’s goals or that could support the policy if it is suitably designed
Identify effective ways of promoting the intervention or policy; for example, support for an effort may be increased by emphasizing the nonhealth benefits of the effort, such as the economic benefits of opening grocery stores in an underserved neighborhood
Monitor and evaluate interventions and policies
Systems approaches are especially useful now, when numerous nutrition and food policies and programs exist or are recommended to address obesity and dietary quality but have never been fully coordinated or scaled sufficiently.39,54 Examples include policies and programs (both newly generated and updated) that address food insecurity or maternal and child nutrition at the global, federal, state, and local levels.55-57 By helping us understand how whole systems work and how individual policies function within larger systems, systems approaches can help in the design of coordinated and converging sets of policies.
Enhancing Current Obesity Prevention and Control Efforts in the United States
Policy Initiatives
In the United States, governments at all levels have enacted a range of obesity prevention and control policies that target diverse populations and are aimed at meeting Healthy People 2020 goals to reduce adult and childhood obesity.58 Most of these policies target children in school or daycare settings, and the primary goals of these policies are increasing physical activity and changing what children eat.59 School-based policies that target increasing physical activity and promoting healthy eating show small reductions in childhood obesity, although evidence of the success of these policies is mixed partly because of the lower quality of some of the studies.60,61
Governments at all levels in the United States, including state, county, municipal, and tribal governments, also have adopted antiobesity regulations. For example, changes in national food policy have included nutrition labeling, such as the Patient Protection and Affordable Care Act’s requirement that chain restaurants post calories on menus and the US Food and Drug Administration’s 2016 redesign of the Nutrition Facts panel. The Nutrition Facts panel, which is mandatory for all packaged foods, is now required to include a larger font size for calories, list added sugar, and use serving sizes that reflect the servings people typically consume.62,63
Localities and states have taken legislative and regulatory actions focused on various aspects of food systems—for example, tax incentives for using land in urban areas for gardening or farming and nutritional standards on government food procurement.64 Some of these actions are directed toward the retail space, such as providing financial incentives for retailers to open locations in underserved areas and taxing sugar-sweetened beverages; these taxes have been implemented by 7 US cities.64,65 Other policies target food marketing, such as a 2014 California bill proposing a health warning on sugar-sweetened beverages and San Francisco’s prohibition of the distribution of free toys with children’s fast-food meals, unless the meals meet nutrition standards.64 Minneapolis, Minnesota, requires licensed grocery stores (including corner stores, gas stations, dollar stores, and pharmacies) to stock a minimum number of staple foods, such as fruit, vegetables, and cereals.66
Challenges and Opportunities for Policy
Although isolated regulatory interventions may succeed in changing food environments, any one action is unlikely to reduce the prevalence of obesity on its own.67 Scaling up regulatory interventions is important but may be difficult because of opposition from industry and variable public support. Although most of the US public sees obesity as the most serious health problem facing the nation, public consensus on whether the government should take action to address obesity is lacking.68,69 For example, a 2017 poll found that 31% of US adults supported more regulatory action to address obesity, and 30% of people wanted less regulatory action to address obesity.68 In a 2013 survey, 54% of US adults responded that the government should not play a substantial role in reducing obesity, and only 42% responded that it should.69 However, public support varies depending on the obesity policy in question, and support for some policies (eg, junk food taxes) is growing.68-70
One explanation for poor public support is that obesity prevention and control efforts may not be sufficiently aligned with the US public’s preferences and values or do not promote modes of healthier eating that fit easily into people’s lives.71-75 Some actors in the food industry also have attempted to turn the public against regulatory policy.76-78 Political opposition to some obesity policies might be seen as a warning sign that there is a need not only to mobilize more political support but also to better understand the public’s experiences, preferences, and values and to design policies that more closely align with them. A need exists to engage with people on all sides of the political spectrum, including those who critique antiobesity efforts as misguided or unethical.72,73,79-81
A further policy challenge derives from the connection between obesity and other health, social, and environmental problems in food systems. Ideally, obesity policies would be designed to produce benefits along multiple dimensions, but trade-offs are inevitable, and stakeholders may disagree about which trade-offs are acceptable. From one perspective, the connections between obesity and other problems simply magnify the political challenges—stakeholders outside of the food industry may oppose obesity policies because of their negative effects (eg, on food security). However, from another perspective, the connections between obesity and other problems afford opportunities to create broader, more diverse alliances for obesity efforts by aligning these efforts with other food system goals (eg, by selecting obesity policies that align with environmental sustainability efforts). Systems approaches can help on this front by making possible an analysis of the potential effects of food policies on multiple variables of interest (eg, health, environmental, economic, and social) over time, helping to identify win-wins and identifying affected groups to form political alliances.14
Local Programs: Promising New Approaches
Some of the most exciting obesity work is happening at the local level. Local action includes programs that adjust the distribution of food outlets (eg, by increasing the number of grocery stores), modify the mix of foods and prices of foods available in those outlets, or target other actors in the food-supply chain, as well as community-level programs that target food consumption and physical activity. In many places, cross-sectoral food policy councils are building a constituency for change and leading innovative efforts in local and state governments, institutions (eg, schools), community common areas, and workplaces to further a system-wide approach.82,83 Local efforts to modify the mix of food outlets and foods available include programs that provide training and financial incentives to retailers to increase healthy food offerings or open locations in underserved areas and programs that offer incentives to increase healthy food purchases.64,84,85
Community-level programs, including programs that have intervened in multiple settings in a coordinated, mutually reinforcing way, have had some success.86 For example, Shape Up Somerville (2002-2005) was a 3-year, controlled, multilevel, multisetting childhood obesity prevention intervention in Massachusetts. It used a community-based participatory research approach to increase physical activity and healthy eating in early elementary schoolchildren before, during, and after school. The intervention was designed to develop strategies to work synergistically (ie, the changes in the school environment were reinforced by changes in the home and community).48 The BMI z-score (a measure of relative weight adjusted for child age and sex) and prevalence of overweight and obesity decreased among intervention students and their parents compared with control students and their parents.87,88 The program has been maintained as a citywide program.89 Currently, a variant of the program that focuses on children aged 0-5, Shape Up Under 5, is underway.90
Local programs face numerous challenges. For example, one challenge for programs aimed at increasing the availability of healthy food in retail environments is that even when implemented successfully, these programs may change consumption only modestly, if at all.67,91 Increasing access to healthy foods will not make diets healthier if consumers do not want to eat these foods or if their consumption of unhealthy food does not decrease.92-94 Efforts to increase food availability may also be undermined by what happens elsewhere in local, state, or national food systems. For example, retailers cannot stock more fruit and vegetables if they are not available from wholesalers at affordable prices.94
Another obstacle to designing effective programs is that although data on dietary intake are available from national surveys, few local- and state-level data exist. Community Commons (www.communitycommons.org) provides community-level data with mapping capabilities. However, additional collaborative efforts to gather local-level and state-level data on nutrition, dietary behaviors, and food access are needed.
Insights from systems approaches may offer opportunities for enhancing programs, such as recognizing the value of targeting multiple parts of the system. For example, when trying to increase healthy food offerings in retail locations, practitioners could work with retailers who make decisions about what to stock in their stores and the wholesalers who sell to those retailers to ensure that healthy items are affordable and with consumers to stimulate demand for the healthy items. This is what the B’More Healthy Communities for Kids program did in Baltimore, Maryland. The program provided incentives and assistance to carryout restaurant owners and corner store owners to stock healthier food items, persuaded wholesalers to agree to stock the healthier items and to offer discounts on these items, and implemented programming for consumers to increase their demand for the healthier food items, including taste tests and educational sessions in stores.84,85,94 The need to be aware of multiple levels of a system is another lesson from systems approaches. For example, working with local retailers to increase healthy food offerings may benefit from understanding national trends in the home delivery of food.95
What if, even after systems approaches are used to improve antiobesity programs (eg, programs that increase the availability of healthy food) and policies, these programs do not affect rates of obesity in the short term? Should these efforts then be abandoned? Systems approaches could help practitioners to identify reasons why these efforts are not working and ways to increase their impact. For example, the reasons why efforts are not working may lie outside the local area, and addressing them may require a broader effort with state or national collaborators. Systems approaches may also reveal ways to combine efforts to increase their effectiveness, such as combining a program that increases the availability of healthy food with a program that promotes physical activity. Programs and policies might not affect obesity rates in the short term, but they might affect dietary patterns in the long term. In the meantime, they may have economic benefits, such as when opening a grocery store in a neighborhood creates jobs and attracts other businesses to the community. Increasing access to healthy food may increase people’s well-being by increasing their choice of desired food items, and increasing access to healthy food is seen as an important social justice goal in and of itself, even if it does not improve health.96 Local work on obesity prevention and control and on food systems may also engage civic and community leaders and enhance their capacity to advocate for local food policy efforts.34
Programs that do not result in short-term reductions in obesity may still have value by promoting local coalition building. Including a diverse group of stakeholders in the design of obesity prevention and control efforts and aligning them with the goals of stakeholders outside of public health can help attract and maintain the support of a broad alliance. In this context, the more than 200 local food policy councils in the United States, which engage stakeholders from various food system sectors to address access to food, economic development, land-use planning, procurement, and hunger, can be key players. Operating at the state, local, and regional levels, most of these food councils aim to improve the community’s health through improving food systems.97
Conclusions and Recommendations
There are no quick fixes when it comes to improving food systems or reducing rates of obesity. Public health practitioners, policy makers, and researchers need to think expansively about how to prevent obesity, incorporate food systems as a target of their interventions, and embrace a broad set of long-term goals. Public health needs an ambitious research agenda that applies innovative methods and study designs to address the complexity of the obesity problem.
Systems approaches can help obesity researchers, public health policy makers, and practitioners think about what an ideal research program and programmatic or policy agenda might address. From a systems perspective, gaps in data represent not only the information on which interventions and policies shift consumption or which populations to target, but also the knowledge of how the broader systems, within which these efforts are embedded, function.
We offer several recommendations for future obesity research and practice. First, interdisciplinary research projects are needed that bring together diverse stakeholders, including community members, policy makers, obesity researchers, food systems researchers, and researchers from other fields, including social scientists with qualitative research skills who can address the broader social, cultural, and political context. A research approach that uses targeted population-specific interventions could be enhanced by focusing on community contexts that can amplify or limit interventions and by implementing changes at multiple levels (ie, a systems approach to intervention delivery). Second, consulting and engaging with a broad array of researchers across the fields of obesity, food systems, and the social sciences is needed. Third, public health should work to strengthen innovative local policies and programs, particularly those that include community members in identifying problems and solutions. Fourth, although interventions should aim to improve healthy eating patterns in the short term and measure the interventions’ success, these interventions should also embrace a broader set of goals and a lengthy time horizon and be evaluated accordingly. Long-term indicators of success will include not only changes in diet and obesity but also indicators of improving community well-being in other ways, building local capacity, building political momentum, and addressing other problems in food systems. Fifth, the field of public health should support interdisciplinary, multistakeholder research teams with broad sets of goals and the ability to study change during long periods, while growing opportunities for training and collaboration for obesity researchers that bring together multiple disciplines and perspectives and teach new skills in systems methods. Finally, funders should create mechanisms to support longer-term commitments to researchers and communities to sustain projects that can be repeated, improved, and, rigorously evaluated.
Acknowledgments
The authors thank the attendees and presenters at the Bloomberg American Health Initiative Obesity and the Food System Symposium at the Johns Hopkins Bloomberg School of Public Health in March 2018 for their contribution to the symposium that resulted in the writing of this article.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article was produced with the support of the Bloomberg American Health Initiative, which is funded by a grant from the Bloomberg Philanthropies.
ORCID iD: Anne Barnhill, PhD  http://orcid.org/0000-0003-1478-6609
http://orcid.org/0000-0003-1478-6609
References
- 1. World Health Organization. Prevalence of overweight among adults, BMI ≥ 25, crude estimates by WHO region. 2017. http://apps.who.int/gho/data/view.main.BMI25CREGv?lang=en. Accessed September 22, 2018.
- 2. World Health Organization. Prevalence of obesity among adults, BMI ≥ 30, crude estimates by WHO region. 2017. http://apps.who.int/gho/data/view.main.BMI30CREGv?lang=en. Accessed September 22, 2018.
- 3. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. US Department of Health and Human Services, Office of Minority Health. Obesity and African Americans. 2017. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=25. 2017. Accessed September 22, 2018.
- 5. US Department of Health and Human Services, Office of Minority Health. Obesity and Native Hawaiians/Pacific Islanders. 2017. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=85. Accessed September 22, 2018.
- 6. US Department of Health and Human Services, Office of Minority Health. Obesity and Hispanic Americans. 2017. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=70. Accessed September 22, 2018.
- 7. US Department of Health and Human Services, Office of Minority Health. Obesity and American Indians/Alaska Natives. 2017. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlID=40. Accessed September 22, 2018.
- 8. Afshin A, Forouzanfar MH, Reitsma MB, et al. ; GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Spiegelman BM, Flier JS. Obesity and the regulation of energy balance. Cell. 2001;104(4):531–543. [DOI] [PubMed] [Google Scholar]
- 10. Bleich SN, Ku R, Wang YC. Relative contribution of energy intake and energy expenditure to childhood obesity: a review of the literature and directions for future research. Int J Obes (Lond). 2011;35(1):1–15. [DOI] [PubMed] [Google Scholar]
- 11. Desilver D. How America’s diet has changed over time. FactTank Pew Research Center. December 13, 2016 http://www.pewresearch.org/fact-tank/2016/12/13/whats-on-your-table-how-americas-diet-has-changed-over-the-decades. Accessed September 22, 2018.
- 12. Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in state-specific adult fruit and vegetable consumption—United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(45):1241–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. US Department of Health and Human Services and US Department of Agriculture. Dietary guidelines for Americans, 2015-2020. 8th ed 2015. https://health.gov/dietaryguidelines/2015/guidelines . Accessed September 22, 2018.
- 14. Institute of Medicine, National Research Council. A Framework for Assessing Effects of the Food System. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 15. Bleich SN, Vercammen KA, Koma JW, Li Z. Trends in beverage consumption among children and adults, 2003-2014: trends in beverage consumption. Obesity (Silver Spring). 2018;26(2):432–441. [DOI] [PubMed] [Google Scholar]
- 16. Food and Agriculture Organization, Committee on World Food Security. Nutrition and food systems: a report by the High Level Panel of Experts on Food Security and Nutrition. 2017. http://www.fao.org/3/a-i7846e.pdf. Accessed September 22, 2018.
- 17. Vandevijvere S, Chow CC, Hall KD, Umali E, Swinburn BA. Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull World Health Organ. 2015;93(7):446–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. [DOI] [PubMed] [Google Scholar]
- 19. Harris JL, Pomeranz JL, Lobstein T, Brownell KD. A crisis in the marketplace: how food marketing contributes to childhood obesity and what can be done. Annu Rev Public Health. 2009;30:211–225. [DOI] [PubMed] [Google Scholar]
- 20. Grier SA, Kumanyika S. Targeted marketing and public health. Annu Rev Public Health. 2010;31:349–369. [DOI] [PubMed] [Google Scholar]
- 21. Hawkes C, Smith TG, Jewell J, et al. Smart food policies for obesity prevention. Lancet. 2015;385(9985):2410–2421. [DOI] [PubMed] [Google Scholar]
- 22. Young LR, Nestle M. Expanding portion sizes in the US marketplace: implications for nutrition counseling. J Am Diet Assoc. 2003;103(2):231–234. [DOI] [PubMed] [Google Scholar]
- 23. Livingstone MBE, Pourshahidi LK. Portion size and obesity. Adv Nutr. 2014;5(6):829–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zlatevska N, Dubelaar C, Holden S. Sizing up the effect of portion size on consumption: a meta-analytic review. J Marketing. 2014;78(3):140–154. [Google Scholar]
- 25. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. [DOI] [PubMed] [Google Scholar]
- 26. Wilde PE, Llobrera J, Valpiani N. Household food expenditures and obesity risk. Curr Obes Rep. 2012;1(3):123–133. [Google Scholar]
- 27. Miller PE, Reedy J, Kirkpatrick SI, Krebs-Smith SM. The United States food supply is not consistent with dietary guidance: evidence from an evaluation using the Healthy Eating Index-2010. J Acad Nutr Diet. 2015;115(1):95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Food and Agriculture Organization, International Fund for Agricultural Development, UNICEF, World Food Programme, and World Health Organization. The State of Food Security and Nutrition in the World. Building Resilience for Peace and Food Security. Rome, Italy: Food and Agriculture Organization; 2017. [Google Scholar]
- 29. Foley JA, Defries R, Asner GP, et al. Global consequences of land use. Science. 2005;309(5734):570–574. [DOI] [PubMed] [Google Scholar]
- 30. Garnett T. Where are the best opportunities for reducing greenhouse gas emissions in the food system (including the food chain)? Food Policy. 2011;36(suppl 1):S23–S32. [Google Scholar]
- 31. Vermeulen SJ, Campbell BM, Ingram JSI. Climate change and food systems. Annu Rev Environ Resour. 2012;37(1):195–222. [Google Scholar]
- 32. Springmann M, Mason-D’Croz D, Robinson S, et al. Mitigation potential and global health impacts from emissions pricing of food commodities. Nature Climate Change. 2017;7(1):69–74. [Google Scholar]
- 33. Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: National Academies Press; 2012. [Google Scholar]
- 34. Huang TT, Cawley JH, Ashe M, et al. Mobilisation of public support for policy actions to prevent obesity. Lancet. 2015;385(9985):2422–2431. [DOI] [PubMed] [Google Scholar]
- 35. Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Annu Rev Public Health. 2012;33:357–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hammond RA. Complex systems modeling for obesity research. Prev Chronic Dis. 2009;6(3):A97. [PMC free article] [PubMed] [Google Scholar]
- 37. Government Office for Science, Department of Health and Social Care. Tackling obesities: future choices. 2007. https://www.gov.uk/government/collections/tackling-obesities-future-choices. Accessed September 22, 2018.
- 38. Finegood DT, Merth TDN, Rutter H. Implications of the Foresight Obesity System Map for solutions to childhood obesity. Obesity (Silver Spring). 2010;18(suppl 1):S13–S16. [DOI] [PubMed] [Google Scholar]
- 39. Johnston LM, Matteson CL, Finegood DT. Systems and obesity policy: a novel framework for analyzing and rethinking population-level planning. Am J Public Health. 2014;104(7):1270–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mabry PL, Milstein B, Abraido-Lanza AF, Livingood WC, Allegrante JP. Opening a window on systems science research in health promotion and public health. Health Educ Behav. 2013;40(1 suppl):5S–8S. [DOI] [PubMed] [Google Scholar]
- 41. Lee BY, Bartsch SM, Mui Y, Haidari LA, Spiker ML, Gittelsohn J. A systems approach to obesity. Nutr Rev. 2017;75(suppl 1):94–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Huang TT, Ferris EB. Connecting the dots: translating systems thinking into innovative solutions for childhood obesity In: Goran MI, ed. Childhood Obesity: Causes, Consequences, and Intervention Approaches. Boca Raton, LA: CRC Press; 2017:465–478. [Google Scholar]
- 43. Huang TT, Glass TA. Transforming research strategies for understanding and preventing obesity. JAMA. 2008;300(15):1811–1813. [DOI] [PubMed] [Google Scholar]
- 44. Huang TT, Drewnosksi A, Kumanyika S, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):A82. [PMC free article] [PubMed] [Google Scholar]
- 45. Economos CD, Hammond RA. Designing effective and sustainable multifaceted interventions for obesity prevention and healthy communities. Obesity (Silver Spring). 2017;25(7):1155–1156. [DOI] [PubMed] [Google Scholar]
- 46. Allender S, Owen B, Kuhlberg J, et al. A community based systems diagram of obesity causes. PLoS One. 2015;10(7):e0129683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Korn AR, Hennessy E, Hammond RA, et al. Development and testing of a novel survey to assess stakeholder-driven community diffusion of childhood obesity prevention efforts. BMC Public Health. 2018;18(1):681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Economos CD, Curtatone JA. Shaping Up Somerville: a community initiative in Massachusetts. Prev Med. 2010;50(suppl 1):S97–S98. [DOI] [PubMed] [Google Scholar]
- 49. Owen B, Brown AD, Kuhlberg J, et al. Understanding a successful obesity prevention initiative in children under 5 from a systems perspective. PLoS One. 2018;13(3):e0195141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hennessy E, Ornstein JT, Economos CD, et al. Designing an agent-based model for childhood obesity interventions: a case study of ChildObesity180. Prev Chronic Dis. 2016;13:E04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Brennan LK, Sabounchi NS, Kemner AL, Hovmand P. Systems thinking in 49 communities related to healthy eating, active living, and childhood obesity. J Public Health Manag Pract. 2015;21(suppl 3):S55–S69. [DOI] [PubMed] [Google Scholar]
- 52. Petrescu-Prahova M, Belza B, Leith K, Allen P, Coe NB, Anderson LA. Using social network analysis to assess mentorship and collaboration in a public health network. Prev Chronic Dis. 2015;12:E130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Christensen LO, O’Sullivan R. Using social network analysis to measure changes in regional food systems collaboration: a methodological framework. J Agric Food Syst Community Dev. 2015;5(3):113–129. [Google Scholar]
- 54. Lloyd-Williams F, Bromley H, Orton L, et al. Smorgasbord or symphony? Assessing public health nutrition policies across 30 European countries using a novel framework. BMC Public Health. 2014;14:1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Neuner K, Kelly S, Raia S. Planning to Eat? Innovative Local Government Plans and Policies to Build Healthy Food Systems in the United States | Cleveland-Cuyahoga County Food Policy Coalition. Buffalo, NY: University at Buffalo, The State University of New York, Food Systems Planning and Healthy Communities Lab; 2011. http://cccfoodpolicy.org/document/planning-eat-innovative-local-government-plans-and-policies-build-healthy-food-systems-unit. Accessed September 22, 2018. [Google Scholar]
- 56. Dietz WH. The response of the US Centers for Disease Control and Prevention to the obesity epidemic. Annu Rev Public Health. 2015;36(1):575–596. [DOI] [PubMed] [Google Scholar]
- 57. Calancie L, Leeman J, Jilcott Pitts SB, et al. Nutrition-related policy and environmental strategies to prevent obesity in rural communities: a systematic review of the literature, 2002-2013. Prev Chronic Dis. 2015;12:E57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Office of Disease Prevention and Health Promotion, US Department of Health and Human Services. Healthy People 2020 topics & objectives: nutrition and weight status. https://www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status/objectives#4928 . Accessed September 22, 2018.
- 59. Bennett WL, Wilson RF, Zhang A, et al. Methods for evaluating natural experiments in obesity: a systematic review. Ann Intern Med. 2018;168(11):791–800. [DOI] [PubMed] [Google Scholar]
- 60. Bramante C, Thornton R, Bennett W, et al. Effectiveness of obesity prevention and control policies and programs for children: a systematic review of natural experiment study designs. Am J Prev Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wang Y, Cai L, Wu Y, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16(7):547–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. US Food and Drug Administration. Changes to the nutrition facts label. https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm385663.htm. Accessed September 22, 2018.
- 63. US Food and Drug Administration. Food labeling; nutrition labeling of standard menu items in restaurants and similar retail food establishments. Fed Register. 2014:71156 https://www.federalregister.gov/documents/2014/12/01/2014-27833/food-labeling-nutrition-labeling-of-standard-menu-items-in-restaurants-and-similar-retail-food. Accessed September 22, 2018. [PubMed]
- 64. Reeve B, Ashe M, Farias R, Gostin L. State and municipal innovations in obesity policy: why localities remain a necessary laboratory for innovation. Am J Public Health. 2015;105(3):442–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Healthy Food America. Taxing sugary drinks. http://www.healthyfoodamerica.org/taxing_sugary_drinks. Accessed September 22, 2018.
- 66. Ch. 203, grocery stores. Code of Ordinances, Minneapolis: https://library.municode.com/mn/minneapolis/codes/code_of_ordinances?nodeId=COOR_TIT10FOCO_CH203GRST. Accessed September 22, 2018. [Google Scholar]
- 67. Sisnowski J, Street JM, Merlin T. Improving food environments and tackling obesity: a realist systematic review of the policy success of regulatory interventions targeting population nutrition. PLoS One. 2017;12(8):e01825 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Politico, Harvard T.H. Chan School of Public Health. The public’s views of tax reform and other domestic issues. 2017. https://www.politico.com/f/?id=0000015e-a4d7-d873-adfe-bdd740140000. Accessed September 22, 2018.
- 69. Kam CD. The polls-trends obesity. Public Opin Q. 2017;81(4):973–995. [Google Scholar]
- 70. Rosenthal R, Morton J, Brethauer S, et al. Obesity in America. Surg Obes Relat Dis. 2017;13(10):1643–1650. [DOI] [PubMed] [Google Scholar]
- 71. Mulvaney-Day N, Womack CA. Obesity, identity and community: leveraging social networks for behavior change in public health. Public Health Ethics. 2009;2(3):250–260. [Google Scholar]
- 72. Resnik D. Trans fat bans and human freedom. Am J Bioeth. 2010;10(3):27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Guthman J. Weighing in: Obesity, Food Justice, and the Limits of Capitalism. Berkeley, CA: University of California Press; 2011. [Google Scholar]
- 74. Guthman J. Can’t stomach it: how Michael Pollan et al. made me want to eat Cheetos. Gastronomica. 2007;7(3):75–79. [Google Scholar]
- 75. Bowen S, Elliott S, Brenton J. The joy of cooking? Contexts. 2014;13(3):20–25. [Google Scholar]
- 76. Koplan JP, Brownell KD. Response of the food and beverage industry to the obesity threat. JAMA. 2010;304(13):1487–1488. [DOI] [PubMed] [Google Scholar]
- 77. Nestle M. Food Politics: How the Food Industry Influences Nutrition and Health. Berkeley and Los Angeles, CA: University of California Press; 2007. [Google Scholar]
- 78. Brownell KD, Warner KE. The perils of ignoring history: Big Tobacco played dirty and millions died. How similar is Big Food? Milbank Q. 2009;87(1):259–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Holm S. Obesity interventions and ethics. Obes Rev. 2007;8(suppl 1):207–210. [DOI] [PubMed] [Google Scholar]
- 80. Kirkland A. The environmental account of obesity: a case for feminist skepticism. Signs (Chic). 2011;36(2):463–486. [DOI] [PubMed] [Google Scholar]
- 81. Williams G. The IDEFICS intervention: what can we learn for public policy? Obes Rev. 2015;16(suppl 2):151–161. [DOI] [PubMed] [Google Scholar]
- 82. Johns Hopkins Center for a Livable Future. Food Policy Council achievements. http://www.foodpolicynetworks.org/_pdf/directory/FPC%20Achievements-final-1.pdf. Published 2018. Accessed September 22, 2018.
- 83. Johns Hopkins Center for a Livable Future . Food Policy Council directory 2016. http://www.foodpolicynetworks.org/directory. Accessed September 22, 2018.
- 84. Schwendler T, Shipley C, Budd N, et al. Development and implementation: B’More Healthy Communities for Kid’s store and wholesaler intervention. Health Promot Pract. 2017;18(6):822–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Budd N, Jeffries JK, Jones-Smith J, Kharmats A, McDermott AY, Gittelsohn J. Store-directed price promotions and communications strategies improve healthier food supply and demand: impact results from a randomized controlled, Baltimore City store-intervention trial. Public Health Nutr. 2017;20(18):3349–3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Mikkelsen BE, Novotny R, Gittelsohn J. Multi-level, multi-component approaches to community based interventions for healthy living—a three case comparison. Int J Environ Res Public Health. 2016;13(10):piiE1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Coffield E, Nihiser AJ, Sherry B, Economos CD. Shape Up Somerville: change in parent body mass indexes during a child-targeted, community-based environmental change intervention. Am J Public Health. 2015;105(2):e83–e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Economos CD, Hyatt RR, Must A, et al. Shape Up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev Med. 2013;57(4):322–327. [DOI] [PubMed] [Google Scholar]
- 89. City of Somerville. Shape Up Somerville. http://archive.somervillema.gov//departments/health/sus. Accessed September 22, 2018.
- 90. Cambridge Health Alliance. Somerville Under 5 obesity prevention pilot. 2018. https://www.challiance.org/about/newsroom/somerville_under_5_obesity_prevention_pilot_1007. Accessed September 22, 2018.
- 91. Mayne SL, Auchincloss AH, Michael YL. Impact of policy and built environment changes on obesity-related outcomes: a systematic review of naturally occurring experiments. Obes Rev. 2015;16(5):362–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Handbury J, Rahkovsky IM, Schnell M. What drives nutritional disparities? Retail access and food purchases across the socioeconomic spectrum. 2015. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2632216. Accessed September 22, 2018.
- 93. Rahkovsky I, Snyder S. Food Choices and Store Proximity. Washington, DC: US Department of Agriculture, Economic Research Service; 2015. [Google Scholar]
- 94. Kim M, Budd N, Batorsky B, et al. Barriers to and facilitators of stocking healthy food options: viewpoints of Baltimore City small storeowners. Ecol Food Nutr. 2017;56(1):17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Vaughan CA, Collins R, Ghosh-Dastidar M, Beckman R, Dubowitz T. Does where you shop or who you are predict what you eat? The role of stores and individual characteristics in dietary intake. Prev Med. 2017;100:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Dieterle JM. Food deserts and lockean property In: Dieterle JM, ed. Just Food: Philosophy, Justice and Food. London, UK: Rowman & Littlefield International; 2015:39–55. [Google Scholar]
- 97. Sussman L, Bassarab K. Food Policy Council Report 2016 . Baltimore, MD: Johns Hopkins Center for a Livable Future; 2016. https://assets.jhsph.edu/clf/mod_clfResource/doc/FPC%20Report%202016_Final.pdf. Accessed September 22, 2018. [Google Scholar]