Abstract
Drug overdose is now the leading cause of injury death in the United States. Most overdose fatalities involve opioids, which include prescription medication, heroin, and illicit fentanyl. Current data reveal that the overdose crisis affects all demographic groups and that overdose rates are now rising most rapidly among African Americans. We provide a public health perspective that can be used to mobilize a comprehensive local, state, and national response to the opioid crisis. We argue that framing the crisis from a public health perspective requires considering the interaction of multiple determinants, including structural factors (eg, poverty and racism), the inadequate management of pain, and poor access to addiction treatment and harm-reduction services (eg, syringe services). We propose a novel ecological framework for harmful opioid use that provides multiple recommendations to improve public health and clinical practice, including improved data collection to guide resource allocation, steps to increase safer prescribing, stigma-reduction campaigns, increased spending on harm reduction and treatment, criminal justice policy reform, and regulatory changes related to controlled substances. Focusing on these opportunities provides the greatest chance of making a measured and sustained impact on overdose and related harms.
Keywords: addiction, health disparities, health policy, injury, pain management, stigma
In 2016, 64 000 people died from drug overdose in the United States.1 Overdose is now the leading cause of injury death in the United States, contributing to an unprecedented decline in life expectancy among non-Hispanic white people without a college degree.2 The current drug overdose crisis is substantially driven by opioids, which accounted for 42 000 deaths in 2016, a 5-fold increase since 1999.1 Much of the current response to this crisis, which is aimed at reducing the wide-ranging health consequences of the opioid epidemic, lacks comprehensive vision and strategy. Public health approaches that focus on reducing overdose risk among the most vulnerable populations show great promise, but implementing these approaches requires policies rooted in a broad conceptualization of the drivers of the epidemic.
Understanding the Opioid Epidemic
Epidemiological and clinical data provide context for understanding the range of adverse outcomes directly related to fatal opioid overdose, opioid use and misuse, and opioid use disorder; the medical and social consequences that are driven by opioid misuse; and programs and policies that may either contribute to or mitigate negative outcomes (Table 1).
Table 1.
Major indicators tracking the opioid overdose epidemic: current state of knowledge and key limitations
| Indicator | What We Know | Key Limitations of Indicator |
|---|---|---|
| Fatal opioid overdose rates and types of opioids associated with overdose |
|
|
| Nonfatal opioid overdoses |
|
|
| Use of prescribed opioid pain relievers |
|
|
| Nonmedical use of pain relievers, use of heroin, and opioid use disorder |
|
|
| National drug laboratory data |
|
|
| Harm reduction |
|
|
| Criminal justice involvement |
|
|
| Incidence of HIV and hepatitis C virus (HCV) |
|
|
| Hospitalizations and data on nonfatal overdoses |
|
|
| Access to drug treatment programs |
|
Opioid Overdose Deaths
Most fatal opioid overdoses in the early 2000s were exclusively linked to prescription medication, yet most opioid overdoses today involve heroin and illicit fentanyl. Nationally, people who died of opioid overdose in recent years were disproportionately white, male, middle-aged adults.1 Unlike the last major national surge of heroin use in the 1970s, which mainly affected urban minority populations, since the 2000s, opioid overdose rates have been elevated in urban, suburban, and rural communities.17 Geographically, the greatest burden of overdoses is in Appalachia, the Southwest, and New England.1 These realities, combined with rising political attention to rural and low-income white people in the United States, may explain increased interest in addressing opioid overdose in these hard-hit regions.18 Trends among other affected populations are also concerning. For example, drug overdose mortality among Native Americans has been highly elevated since the inception of the drug overdose crisis in the early 2000s, and the incidence of overdose mortality among African Americans is now rising faster than among other racial/ethnic groups.18
Opioid Use and Misuse, and Opioid Use Disorder
Consistent with the mortality shift away from prescription opioids and toward illicit opioids, national data indicate that opioid prescription volume leveled during the past decade,5 although it is higher than in many peer countries.6 Simultaneously, the potency and lethality of street drugs increased, because heroin is frequently adulterated with fentanyl.19 Fentanyl is increasingly entering the cocaine and methamphetamine supply.9
The 2016 National Survey of Drug Use and Health estimated that at any point in the year, 92 million people in the United States used opioid pain relievers,20 11.5 million misused opioid pain relievers, 0.9 million used heroin, and 2.1 million had symptoms of an opioid use disorder (ie, opioid use caused impairment and/or dependence).21 National Survey of Drug Use and Health data indicate that misuse of prescription opioids has declined since the mid-2000s.22 These data mirror trends in medical claims and administrative databases, which track quantities of opioids legally distributed in various areas7 and provide insight into the dosage and quantity of prescription opioids used by patients.23 Patients who use high-dosage opioids are broadly distributed across the medical system, rarely concentrating in practices that might be considered “pill mills” (ie, clinics with aberrant prescribing),24 suggesting that efforts to change prescribing likely need to be broadly targeted. National Survey of Drug Use and Health data also indicate that the number of heroin users has increased, and the demographic characteristics of people who use heroin have also changed; most new users are non-Hispanic white and, increasingly, female.25 High-risk opioid use and negative outcomes disproportionately affect urban communities26 and vulnerable groups, including the criminal justice–involved population,11 sex workers,27 and gender minority populations.28
Other Adverse Outcomes
Medical claims data track nonfatal opioid overdose and medical comorbidities.14 Opioid-associated infections (eg, hepatitis C virus12 and HIV among younger groups13) have risen in recent years. The opioid crisis has increased the prevalence of neonatal abstinence syndrome, a transient withdrawal syndrome after birth following an opioid-exposed pregnancy that lasts several days to several weeks.29 Neonatal abstinence syndrome can occur when mothers receive methadone or buprenorphine and, in these cases, can be managed without negative long-term effects on infant health.30 In cases in which this syndrome is associated with an unstable home environment, a child’s subsequent healthy development is at risk. Areas hit hardest by the opioid epidemic have had higher rates of foster care involvement than areas where the opioid epidemic has been less severe.31 Opioid use and economic stress are likely related, with some evidence suggesting that opioid use is associated with economic hardship32 and absence from the labor market.33
Programs and Policies
Access to treatment and harm-reduction programs is growing but remains limited. In 2004-2013, only one-fifth of people with opioid use disorder received treatment.15 Admissions-level data on drug treatment programs show that in 2005-2015, only one-quarter of patients received opioid agonist treatment (eg, methadone or buprenorphine), the treatment option best supported by clinical evidence.16 About half of all people who inject drugs used syringe service programs in 2015, an increase from one-third of all people who inject drugs in 2005.34 The amount of naloxone dispensed by retail pharmacies increased 12-fold from late 2013 to mid-2015, and the number of naloxone kits distributed to laypeople increased 3-fold from 2010 to 2014.35 Naloxone distribution programs can help reduce opioid overdose deaths by putting life-saving medication in the hands of people who are close to overdose victims.36
Limitations of Current Data
Lack of standardization in toxicology and coding practices among medical examiners and coroners can lead to misclassification of cause of death, poor identification of types of opioids involved in overdoses, and undercounting of intentional poisonings.37-41 Additionally, focusing on mortality does not adequately disentangle fatality risk per user (or per use) over time and specific drugs involved in overdoses—research questions that could be informed by nonfatal overdose surveillance data or drug seizure data.42
Although the National Survey of Drug Use and Health does sample people with a history of criminal justice involvement, it does not include data on people who are in jails or prisons or homeless people. The now-defunct Arrestee Drug Abuse Monitoring program provided useful surveillance data on drug use among arrestees.43 Similarly, data on illicit drug markets, including price and purity of street drugs and the intersection between opioids and other illicit drugs, are limited. Finally, although robust epidemiological studies have been performed for small geographic areas,44 nationally representative longitudinal studies of people who use opioids are lacking, making it difficult to examine initiation of use and transition across various misused substances (eg, prescribed opioids, heroin).
Evaluating policy change is also problematic. Multiple legislative and programmatic interventions are often pursued simultaneously,45 thereby complicating efforts to discern the effects of a particular element. For example, mixed evidence on the effectiveness of prescription drug monitoring programs46-53 may stem from challenges in isolating their effects when states simultaneously implement laws on expanded naloxone access, pain clinic regulation, and opioid prescribing caps.54 Finally, data are limited on how accessible various types of programs and services are to people who use opioids, making it difficult to quantify the effectiveness of these programs in improving health and safety.
Framing the Opioid Epidemic as a Public Health Issue
The national dialogue around opioids has been dominated by several approaches that on their own are inadequate or harmful. “War on drugs” approaches that would increase arrests and incarceration to deter drug use and distribution have had long-term scarring effects on many communities, primarily those of color,55,56 without measurably reducing access to street drugs.57,58 Likewise, defining drug use as an individual’s moral failing that can be remedied through willpower alone is inconsistent with biological triggers that create susceptibility to addiction.54 The moral failing approach also fails to recognize the role of trauma and adverse childhood experiences in addiction. Most importantly, the willpower approach lacks evidence for efficacy.59 Likewise, a single-minded focus on abstinence led to opposition from several self-help advocates against highly effective treatments such as methadone, buprenorphine,60,61 and harm reduction.62 Moving beyond moralized and punitive approaches to addiction could help reduce stigma and increase acceptance of treatment, not only for people who use opioids but also for the safety and wellbeing of society at large.
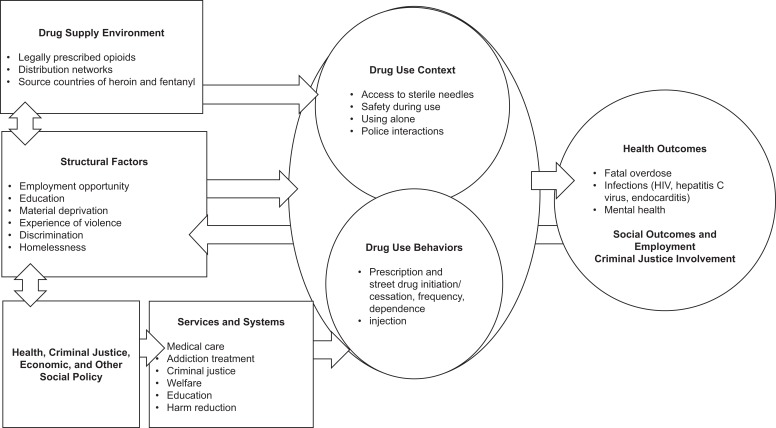
Drawing on ecological models of health behavior (eg, McLeroy’s model, which posits that health outcomes emerge from the interaction of individual, institutional, community, and policy factors),63,64 we developed a novel public health approach that draws attention to multiple determinants of drug use and emphasizes the role of upstream factors that drive addiction, overdose, and associated social outcomes (Figure). At the center is the interaction between individual drug use behaviors and drug use context; a particular opioid use behavior (eg, injection) is more likely to result in negative outcomes when it occurs in an unsafe environment than, for example, when it occurs in a supervised consumption context.65 Both context and behaviors are influenced by upstream factors. Structural factors reflect social and economic conditions that drive social disadvantage and lack of opportunity in many communities.66 Structural factors influence, and are influenced by, the drug supply environment and by health, criminal justice, economic, and social policy. These policy factors also have a downstream influence on services and systems that interact with people who use drugs, particularly opioids. Individual health and social outcomes are driven by the nexus between drug use behaviors and the drug use context. We posit that health and social outcomes flow back to structural factors, because living in communities with a high prevalence of overdose has an adverse effect on the social and economic environment.
Figure.
A conceptual framework for the opioid overdose epidemic.
These complex factors are inadequately reflected in current data. Our public health approach posits that harmful drug use is closely intertwined with social structures that create stigma and isolation, the labor market, and the functioning of the public safety net. Once the contributors to overdose are reconceptualized from a public health lens, it becomes clear that reducing morbidity and mortality associated with the use of opioids can be fully achieved only by simultaneously addressing the forces that drive opioid use, the context of drug use, and the factors making such use increasingly lethal.
Opportunities for Public Health Impact
Several approaches could decrease opioid overdoses and other harms associated with opioid drug use if implemented to scale. These elements could form the basis for a national response strategy focused on opioid overdose risk (Table 2). These approaches are optimally pursued through partnership among federal, state, and local government.
Table 2.
Key priorities for a public health approach to reduce morbidity and mortality associated with the opioid overdose epidemic
| Key Priority | Strategy | Responsible Group |
|---|---|---|
| Improved data collection |
|
|
| Safer prescribing |
|
|
| Stigma reduction |
|
|
| Harm reduction |
|
|
| Treatment expansion |
|
|
| Criminal justice reform |
|
|
| Regulatory change |
|
|
Improving Data Collection
Data collection can be improved by building overdose tracking into existing sentinel surveillance systems focused on vulnerable populations (eg, men who have sex with men and people who inject drugs). Implementing new surveillance systems requires overcoming legal and data exchange barriers. Ideally, practitioners could track local risk factors in real time and identify the resources (eg, naloxone distribution) that can mitigate risks. One area of data collection that has recently seen progress is developing dashboards, such as Rhode Island’s PreventOverdose, RI,67 which reports timely statewide data on key indicators, including overdose incidence and admissions to specialty treatment programs. States can invest in improving drug overdose fatality surveillance, which has improved the accuracy of data collected in states such as Kentucky.68 Creating data warehouses that link individual-level records across multiple public service systems (eg, Massachusetts through its Chapter 55 legislation69) is another promising strategy.
Safer Prescribing
Improving opioid prescribing practices has the potential to prevent addiction. Efforts to improve prescribing need to be aligned with broader efforts to deliver patient-centered pain treatment deploying a range of treatment modalities. Opioids have important clinical benefits in some contexts, including management of pain from cancer, sickle-cell disease, and acute injuries, whereas risks of long-term opioid therapy for chronic noncancer pain resulting from conditions such as lower back pain, headache, and osteoarthritis often outweigh the benefits.70,71 The 2016 Centers for Disease Control and Prevention guidelines for prescribing opioids for chronic pain offer helpful criteria for how clinicians should consider various pain treatment options, including opioid and nonopioid pharmacotherapies (eg, ibuprofen) and nonpharmacologic pain treatments (eg, physical therapy) that have been shown to be safer and more effective than opioids in some contexts.70
Several measures can be taken to improve opioid prescribing. The first is educating clinicians and patients. It is important to manage patient expectations (eg, that some pain is expected after a surgery) and to talk with patients about goals other than pain relief, such as improving functional status.72 Insurers often inadequately cover nonpharmacologic pain treatments such as physical therapy, suggesting a need for changes in pain treatment reimbursement policies.73 A second measure is to better integrate addiction medicine with pain management, because many patients with opioid use disorder also have chronic pain.74 The worst outcome is for physicians managing pain to refuse to treat patients who demonstrate signs of opioid dependence.75 Instead, physicians have a duty to either treat dependence (eg, by using buprenorphine) or develop a clear linkage to specialty care. Achieving such integration will require various financing (eg, mechanisms for pain specialists to be reimbursed for coordinating addiction care) and delivery (eg, sharing medical records across pain management and addiction treatment providers) strategies.
Stigma Reduction
Many people in the United States believe that people with opioid use disorder are to blame for their addiction and do not want to work closely with them or have them marry into their families. Stigma toward people who use opioids is correlated with low support for allocating substance use treatment resources and high preference for punitive policies.76 Furthermore, stigma can impede help seeking by people with drug problems because they may fear negative social, legal, and employment repercussions if they disclose their drug use.77
Personal stories describing the experiences of people who use opioids can reduce stigma,78 as can messages emphasizing the effectiveness of treatment and depicting examples of successful treatment and recovery.78,79 Language used when discussing addiction also matters. Person-centered language (eg, “person with a substance use disorder” as opposed to “addict”) is destigmatizing.80 Several promising efforts are underway to destigmatize opioid use disorder through such language changes.81,82 Reducing stigmatizing attitudes among law enforcement, clinicians, emergency medical responders, and others who work closely with people who use opioids should be a priority of public health policy makers.
Harm Reduction
Many fatal and nonfatal overdoses can be prevented by changing the circumstances surrounding drug use. Changing circumstances includes improving the safety of the drugs themselves and the environments in which drugs are used. Expanded access to naloxone among people who use drugs, nearby peers, family, and friends is needed.83 National and local data indicate that many overdose reversals are enacted by fellow drug users.84 Although overdose education programs, naloxone programs, and syringe services programs can deploy peer employees to provide life-saving services to those at risk for overdose death,85 formal overdose education and naloxone programs that use peers have not been expanded upon in the United States.
From the early days of the HIV epidemic, syringe services programs were shown to be a cost-effective, low-threshold strategy to reduce blood-borne infections.86 They also can reduce fatal overdoses through education and naloxone distribution and substantially increase uptake of drug treatment.87 Safe consumption spaces (ie, places where individuals can consume previously purchased drugs under medical supervision)88 and drug-checking services (which help people to identify adulterants in drugs they have obtained) are underused in the United States but are an important harm-reduction approach throughout Europe.89 For example, most street drug users in the United States seek to avoid fentanyl but lack the knowledge of how to do so.90 Bucking opposition from the US Department of Justice, jurisdictions such as San Francisco, Seattle, and Philadelphia adopted comprehensive plans for safe consumption spaces, providing a model for others to follow.91
Treatment Expansion
Improving treatment uptake requires bringing effective treatments to people when they need them most, without barriers such as waitlists, travel distance, and high out-of-pocket cost. Promising innovations in the treatment-on-demand approach, such as buprenorphine induction in emergency departments and comprehensive treatments in jails, have been introduced. These approaches can be optimally combined with continued treatment in the community after release from jails and hospitals.92,93 Communities have overcome obstacles such as waitlists by linking specialty treatment to office-based prescribers. For example, the “hub-and-spoke” model in Vermont creates partnerships between office-based prescribers and specialty care to create better integration of services.94 Promising investments have been made in developing the treatment workforce, such as providing additional funding to states through grants authorized by the 21st Century Cures Act.95
Sustained progress, however, requires bolder action. First, Congress needs to expand its commitment to financing treatment through Medicaid and other federally funded programs. Medicaid expansion through the Affordable Care Act has been an important lever for increasing resources for substance use treatment,96 but it has not been adopted in many states and has been continually threatened by repeal efforts. Beyond expanding insurance coverage, Medicaid and private insurers need to support long-term recovery options, eliminate barriers to effective medications, and cover a wider array of treatments (eg, peer services, vocational support).97
Second, opioid agonist treatments must be easier to access and less expensive than illicit opioids. Buprenorphine is tightly regulated. Scope-of-practice laws prevent nurse practitioners from prescribing buprenorphine in many states despite recent federal policy change.98 Beyond the scope of practice, eliminating the additional regulations placed on buprenorphine prescribing altogether is likely to be beneficial. When France ended buprenorphine restrictions in the 1990s, access to buprenorphine increased and overdoses decreased.99 Likewise, methadone is available only in opioid treatment programs, but several peer countries have made it available at pharmacies.100 Several states, including West Virginia, are beginning to cover methadone maintenance; however, more than a dozen states do not cover methadone maintenance under Medicaid.101 Finally, ending spending on ineffective approaches, such as treatment that is administered under the coercion of civil commitment laws,58 can improve outcomes. Licensing bodies should require providers to offer access to (or linkages with) opioid agonist treatment and withhold licensure from providers that do not meet this standard of care.
Criminal Justice Reform
Although the mantra that “we cannot arrest our way out of this problem” has gained adherents in recent years, the US Department of Justice is interested in increasing criminal prosecution of people who use drugs.102 This tough-on-crime approach has a high likelihood of backfiring: overzealous law enforcement can lead fewer people to come forward when their companions are overdosing, thereby increasing health risks.103 Likewise, reducing the minimum amount of fentanyl required by law to trigger federal mandatory minimum sentencing could encourage the sale and distribution of even more concentrated fentanyl doses, which would increase the drug’s lethality.104 However, police, courts, and correctional settings can improve access to treatment and harm reduction.105 The growing use of naloxone by law enforcement and the implementation of Good Samaritan laws that protect people who summon law enforcement in the event of an overdose are promising models.106 Public health and public safety goals are more closely aligned than has been traditionally recognized, although disparate metrics, intervention modalities, professional cultures, and resource competition have so far prevented collaboration.
Recalibrating criminal justice approaches requires examining policies governing drug use, dealing, and prior convictions. Policy change is necessary but is insufficient to transform criminal justice practice; as such, aligning policing with public health goals also requires transforming the tools and incentives used in street-level policing. Broader criminal justice reform efforts, such as improving police accountability, diversity, and training, are also critical to reorienting police practice. Several jurisdictions including Seattle, which adopted the Law Enforcement Assisted Diversion program, have had success with programs offering treatment and harm-reduction services as an alternative to arrests.105 Broader diffusion of these programs should be a priority.
Regulatory Change
Deregulation of medication-assisted treatment and targeted decriminalization approaches are incremental steps toward a reevaluation of the federal controlled substances regulatory system. Under the federal Controlled Substances Act, the US Drug Enforcement Agency has broad purview over health care and pharmacy practices as they relate to controlled substances. The US Drug Enforcement Agency has been driven by criminal justice metrics that bear little relation to public health and lack the scientific expertise to appropriately calibrate patient care. Better public health outcomes could result if the regulatory system were reevaluated based on the likely balance of risks and benefits to public health. This process should be holistic in its focus on overall health and consider opioid regulations alongside other controlled substances. For example, marijuana is a promising alternative pain-relief medication, although marijuana also carries its own health risks.107
Conclusion
The United States is in the midst of an opioid crisis that will not abate without sustained public health interventions. Many policy makers are seeking solutions in the wrong places, and we believe that criminal penalties and a commitment to abstinence-only methods will cause more people to needlessly die of overdoses and will fail to keep the public safe. As in the early days of the AIDS epidemic, political will needs to be built to effect change, and a vision is needed to create policies that will actually work to reduce overdose. Public health has an important role in helping to understand why people use drugs, offering less stigmatizing strategies to assist people who use opioids, and disseminating innovative programs that help these populations to safely use drugs, receive treatment, and enter long-term recovery. Ultimately, overdose deaths are preventable, lives can be saved, and people can recover, regain stability, and have productive futures.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Brendan Saloner and Susan G. Sherman gratefully acknowledge funding support from the Bloomberg American Health Initiative. Funding support from the National Institute on Drug Abuse is acknowledged by Brendan Saloner (K01 DA042139), Leo Beletsky (R01DA039073 [multiple principal investigators: Beletsky/Strathdee] and R37DA019829 [principal investigator: Strathdee]), and Ricky Bluthenthal (R01DA038965 [multiple principal investigators: Bluthenthal/Kral]). This article was produced with the support of the Bloomberg American Health Initiative, which was funded by a grant from the Bloomberg Philanthropies.
References
- 1. Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999-2016. NCHS Data Brief. 2017;(294):1–8. [PubMed] [Google Scholar]
- 2. Case A, Deaton A. Mortality and morbidity in the 21st century. Brook Pap Econ Act. 2017;2017:397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Weiss AJ, Elixhauser A, Barrett ML, Steiner CA, Bailey MK, O’Malley L. Opioid-Related Inpatient Stays and Emergency Department Visits by State, 2009-2014. Rockville, MD: Agency for Healthcare Research and Quality; 2017. [PubMed] [Google Scholar]
- 4. Wood E, Tyndall MW, Spittal PM, et al. Impact of supply-side policies for control of illicit drugs in the face of the AIDS and overdose epidemics: investigation of a massive heroin seizure. CMAJ. 2003;168(2):165–169. [PMC free article] [PubMed] [Google Scholar]
- 5. Guy GP, Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. United Nations. Report of the International Narcotics Control Board for 2016 New York, NY: United Nations; 2017. [Google Scholar]
- 7. Centers for Disease Control and Prevention. Prescription painkiller overdoses in the US. https://www.cdc.gov/vitalsigns/painkilleroverdoses/index.html. Published 2011. Accessed June 24, 2018.
- 8. Mack KA, Jones CM, Ballesteros MF. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas—United States. Am J Transplant. 2017;17(12):3241–3252. [DOI] [PubMed] [Google Scholar]
- 9. O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 states, July–December 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1197–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Adams JM. Increasing naloxone awareness and use: the role of health care practitioners. JAMA. 2018;319(20):2073–2074. [DOI] [PubMed] [Google Scholar]
- 11. Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zibbell JE, Asher AK, Patel RC, et al. Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. Am J Public Health. 2018;108(2):175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ocfemia MCB, Dunville R, Zhang T, Barrios LC, Oster AM. HIV diagnoses among persons aged 13-29 years—United States, 2010-2014. MMWR Morb Mortal Wkly Rep. 2018;67(7):212–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. BlueCross BlueShield. America’s opioid epidemic and its effect on the nation’s commercially-insured population. https://www.bcbs.com/sites/default/files/file-attachments/health-of-america-report/BCBS-HealthOfAmericaReport-Opioids.pdf. Published 2017. Accessed February 28, 2018.
- 15. Saloner B, Karthikeyan S. Changes in substance abuse treatment use among individuals with opioid use disorders in the United States, 2004-2013. JAMA. 2015;314(14):1515–1517. [DOI] [PubMed] [Google Scholar]
- 16. Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS) 2005-2015: State Admissions to Substance Abuse Treatment Services. Rockville, MD: US Department of Health and Human Services; 2017. [Google Scholar]
- 17. Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821–826. [DOI] [PubMed] [Google Scholar]
- 18. Schmitz Bechteler S, Kane-Willis K. Whitewashed: The African American Opioid Epidemic. Chicago, IL: The Chicago Urban League; 2017. [Google Scholar]
- 19. Ciccarone D. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int J Drug Policy. 2017;46:107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Results from the 2016. National Survey on Drug Use and Health: detailed tables. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf. Published 2017. Accessed June 24, 2018.
- 21. Ahrnsbrak R, Bose J, Hedden SL, Lipari RN, Park-Lee E. Key Substance Use and Mental Health Indicators in the United States: Results From the 2016 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.htm. Accessed June 24, 2018. [Google Scholar]
- 22. Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468–1478. [DOI] [PubMed] [Google Scholar]
- 23. Dart RC, Severtson SG, Bucher-Bartelson B. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(16):1573–1574. [DOI] [PubMed] [Google Scholar]
- 24. Chang HY, Murimi IB, Jones CM, Alexander GC. Relationship between high-risk patients receiving prescription opioids and high-volume opioid prescribers. Addiction. 2018;113(4):677–686. [DOI] [PubMed] [Google Scholar]
- 25. Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users—United States, 2002-2013. MMWR Morb Mortal Wkly Rep. 2015;64(26):719–725. [PMC free article] [PubMed] [Google Scholar]
- 26. Mack KA, Jones CM, Ballesteros MF. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas—United States. Am J Transplant. 2017;17(12):3241–3252. [DOI] [PubMed] [Google Scholar]
- 27. Strathdee SA, West BS, Reed E, Moazen B, Azim T, Dolan K. Substance use and HIV among female sex workers and female prisoners: risk environments and implications for prevention, treatment, and policies [published erratum appears in J Acquir Immune Defic Syndr. 2015;69(3):e119]. J Acquir Immune Defic Syndr. 2015;69(suppl 2):S110–S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Medley G, Lipari R, Bose J, Cribb DS, Kroutil LA, McHenry G. Sexual Orientation and Estimates of Adult Substance Use and Mental Health: Results From the 2015 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 29. Kocherlakota P. Neonatal abstinence syndrome. Pediatrics. 2014;134(2):e547–e561. [DOI] [PubMed] [Google Scholar]
- 30. Jones HE, Kaltenbach K, Heil SH, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N Engl J Med. 2010;363(24):2320–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Quast T, Storch EA, Yampolskaya S. Opioid prescription rates and child removals: evidence from Florida. Health Aff (Millwood). 2018;37(1):134–139. [DOI] [PubMed] [Google Scholar]
- 32. Hollingsworth A, Ruhm CJ, Simon K. Macroeconomic conditions and opioid abuse. J Health Econ. 2017;56:222–233. [DOI] [PubMed] [Google Scholar]
- 33. Krueger AB. Where have all the workers gone? An inquiry into the decline of the U.S. labor force participation rate. Brookings Papers on Economic Activity. 2017. https://www.brookings.edu/bpea-articles/where-have-all-the-workers-gone-an-inquiry-into-the-decline-of-the-u-s-labor-force-participation-rate. Accessed June 24, 2018. [DOI] [PMC free article] [PubMed]
- 34. Use of syringe services programs increases, but access must improve for greater HIV prevention [press release]. Washington, DC: Centers for Disease Control and Prevention; 2016. https://www.cdc.gov/media/releases/2016/p1129-HIV-syringe-services.html . Accessed March 18, 2018. [Google Scholar]
- 35. National Institute on Drug Abuse. Medications to treat opioid addiction. https://www.drugabuse.gov/publications/research-reports/medications-to-treat-opioid-addiction/access-to-naloxone. Published 2018. Accessed March 18, 2018.
- 36. Irvine MA, Buxton JA, Otterstatter M, et al. Distribution of take-home opioid antagonist kits during a synthetic opioid epidemic in British Columbia, Canada: a modelling study. Lancet Public Health. 2018;3(5):e218–e225. [DOI] [PubMed] [Google Scholar]
- 37. Slavova S, O’Brien DB, Creppage K, et al. Drug overdose deaths: let’s get specific. Public Health Rep. 2015;130(4):339–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rockett IR, Hobbs GR, Wu D, et al. Variable classification of drug-intoxication suicides across US states: a partial artifact of forensics? PLoS One. 2015;10(8):e0135296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Horon IL, Singal P, Fowler DR, Sharfstein JM. Standard death certificates versus enhanced surveillance to identify heroin overdose-related deaths. Am J Public Health. 2018;108(6):777–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ruhm CJ. Corrected US opioid-involved drug poisoning deaths and mortality rates, 1999-2015. Addiction. 2018;113(7):1339–1344. [DOI] [PubMed] [Google Scholar]
- 41. Buchanich JM, Balmert LC, Williams KE, Burke DS. The effect of incomplete death certificates on estimates of unintentional opioid-related overdose deaths in the United States, 1999-2015. Public Health Rep. 2018;133(4):423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Creppage KE, Yohannan J, Williams K, et al. The rapid escalation of fentanyl in illicit drug evidence in Allegheny County, Pennsylvania, 2010-2016. Public Health Rep. 2018;133(2):142–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Casteel K. Data on drug use is disappearing just when we need it most. FiveThirtyEight. 2017. https://fivethirtyeight.com/features/data-on-drug-use-is-disappearing-just-when-we-need-it-most . Accessed March 1, 2018.
- 44. Carlson RG, Nahhas RW, Martins SS, Daniulaityte R. Predictors of transition to heroin use among initially non-opioid dependent illicit pharmaceutical opioid users: a natural history study. Drug Alcohol Depend. 2016;160:127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. McCarty D, Priest KC, Korthuis PT. Treatment and prevention of opioid use disorder: challenges and opportunities. Annu Rev Public Health. 2018;39:525–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Meara E, Horwitz JR, Powell W, et al. State legal restrictions and prescription-opioid use among disabled adults. N Engl J Med. 2016;375(1):44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation of prescription drug monitoring programs associated with reductions in opioid-related death rates. Health Aff (Millwood). 2016;35(7):1324–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011;12(5):747–754. [DOI] [PubMed] [Google Scholar]
- 49. Bao Y, Pan Y, Taylor A, et al. Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Aff (Millwood). 2016;35(6):1045–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chang HY, Lyapustina T, Rutkow L, et al. Impact of prescription drug monitoring programs and pill mill laws on high-risk opioid prescribers: a comparative interrupted time series analysis. Drug Alcohol Depend. 2016;165:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff (Millwood). 2016;35(10):1876–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rutkow L, Chang HY, Daubresse M, Webster DW, Stuart EA, Alexander GC. Effect of Florida’s prescription drug monitoring program and pill mill laws on opioid prescribing and use. JAMA Intern Med. 2015;175(10):1642–1649. [DOI] [PubMed] [Google Scholar]
- 53. Buchmueller TC, Carey C. The Effect of Prescription Drug Monitoring Programs on Opioid Utilization in Medicare. Washington, DC: National Bureau of Economic Research; 2017. [Google Scholar]
- 54. Substance Abuse and Mental Health Services Administration, Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: US Department of Health and Human Services; 2016. http://www.ncbi.nlm.nih.gov/books/NBK424857/. Accessed March 1, 2018. [PubMed] [Google Scholar]
- 55. Lopez G. Under Trump and Sessions, federal prosecutors are ramping up the war on drugs. Vox. October 24, 2017. https://www.vox.com/policy-and-politics/2017/10/24/16534812/trump-sessions-war-on-drugs. Accessed March 1, 2018.
- 56. National Academies of Science, Engineering, and Medicine. The Growth of Incarceration in the United States: Exploring Causes and Consequences. Washington, DC: National Academies Press; 2014. [Google Scholar]
- 57. Pollack HA, Reuter P. Does tougher enforcement make drugs more expensive? Addiction. 2014;109(12):1959–1966. [DOI] [PubMed] [Google Scholar]
- 58. Csete J, Kamarulzaman A, Kazatchkine M, et al. Public health and international drug policy. Lancet. 2016;387(10026):1427–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. National Institute on Drug Abuse. Preface: drugs, brains, and behavior: the science of addiction. https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/preface. Published 2014. Accessed March 1, 2018.
- 60. Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009;(3):CD002209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2008;(2):CD002207. [DOI] [PubMed] [Google Scholar]
- 62. Nadelmann E, LaSalle L. Two steps forward, one step back: current harm reduction policy and politics in the United States. Harm Reduct J. 2017;14(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. [DOI] [PubMed] [Google Scholar]
- 64. Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Burris S, Blankenship KM, Donoghoe M, et al. Addressing the “risk environment” for injection drug users: the mysterious case of the missing cop. Milbank Q. 2004;82(1):125–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Rhode Island Department of Health. PreventOverdose, RI. http://preventoverdoseri.org. Published 2018. Accessed March 1, 2018.
- 68. Slavova S, Bunn T, LaMantia S, Corey T. Improving state drug overdose fatality (DOF) surveillance using policy and epidemiological tools. Inj Prev. 2016;22(suppl 2):A155. [Google Scholar]
- 69. Massachusetts Department of Health. An Assessment of Fatal and Nonfatal Opioid Overdoses in Massachusetts (2011-2015). Boston, MA: Massachusetts Department of Health; 2016. [Google Scholar]
- 70. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Washington State Agency Medical Directors’ Group. Interagency guideline on prescribing opioids for pain. http://www.agencymeddirectors.wa.gov/files/2015amdgopioidguideline.pdf. Published 2015. Accessed June 25, 2018.
- 72. Frantsve LM, Kerns RD. Patient–provider interactions in the management of chronic pain: current findings within the context of shared medical decision making. Pain Med. 2007;8(1):25–35. [DOI] [PubMed] [Google Scholar]
- 73. Volkow N, Benveniste H, McLellan AT. Use and misuse of opioids in chronic pain. Annu Rev Med. 2018;69:451–465. [DOI] [PubMed] [Google Scholar]
- 74. Chang YP, Compton P. Management of chronic pain with chronic opioid therapy in patients with substance use disorders. Addict Sci Clin Pract. 2013;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Rothstein MA. Ethical responsibilities of physicians in the opioid crisis. J Law Med Ethics. 2017;45(4):682–687. [Google Scholar]
- 76. Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE. Social stigma toward persons with prescription opioid use disorder: associations with public support for punitive and public health–oriented policies. Psychiatr Serv. 2017;68(5):462–469. [DOI] [PubMed] [Google Scholar]
- 77. Global Commission on Drug Policy. The world drug perception problem: countering prejudices about people who use drugs. http://www.globalcommissionondrugs.org/reports/changing-perceptions. Published 2018. Accessed March 1, 2018.
- 78. McGinty EE, Goldman HH, Pescosolido B, Barry CL. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci Med. 2015;126:73–85. [DOI] [PubMed] [Google Scholar]
- 79. Romer D, Bock M. Reducing the stigma of mental illness among adolescents and young adults: the effects of treatment information. J Health Commun. 2008;13(8):742–758. [DOI] [PubMed] [Google Scholar]
- 80. Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010;21(3):202–207. [DOI] [PubMed] [Google Scholar]
- 81. Botticelli MP, Koh HK. Changing the language of addiction. JAMA. 2016;316(13):1361–1362. [DOI] [PubMed] [Google Scholar]
- 82. Associated Press. The 2018 AP Stylebook. New York, NY: Associated Press; 2018. [Google Scholar]
- 83. Adams JM. Increasing naloxone awareness and use: the role of health care practitioners. JAMA. 2018;319(20):2073–2074. [DOI] [PubMed] [Google Scholar]
- 84. Lambdin BH, Zibbell J, Wheeler E, Kral AH. Identifying gaps in the implementation of naloxone programs for laypersons in the United States. Int J Drug Policy. 2018;52:52–55. [DOI] [PubMed] [Google Scholar]
- 85. PHS Community Services Society. The Portland Hotel. https://www.phs.ca/index.php/project/portland-hotel . Published 2018. Accessed March 1, 2018.
- 86. Strathdee SA, Celentano DD, Shah N, et al. Needle-exchange attendance and health care utilization promote entry into detoxification. J Urban Health. 1999;76(4):448–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Des Jarlais DC, McKnight C, Goldblatt C, Purchase D. Doing harm reduction better: syringe exchange in the United States. Addiction. 2009;104(9):1441–1446. [DOI] [PubMed] [Google Scholar]
- 88. Irwin A, Jozaghi E, Weir BW, Allen ST, Lindsay A, Sherman SG. Mitigating the heroin crisis in Baltimore, MD, USA: a cost-benefit analysis of a hypothetical supervised injection facility. Harm Reduct J. 2017;14(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Pirona A, Bo A, Hedrich D, et al. New psychoactive substances: current health-related practices and challenges in responding to use and harms in Europe. Int J Drug Policy. 2017;40:84–92. [DOI] [PubMed] [Google Scholar]
- 90. Sherman SG, Park JN, Glick J, et al. Fentanyl Overdose Reduction Checking Analysis Study. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; 2018. [Google Scholar]
- 91. Lieber M. Safe injection sites in San Francisco could be first in the US. CNN. February 7, 2018 https://www.cnn.com/2018/02/07/health/safe-injection-sites-san-francisco-opioid-epidemic-bn/index.html . Accessed March 1, 2018.
- 92. Green TC, Clarke J, Brinkley-Rubinstein L, et al. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry. 2018;75(4):405–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Brooklyn JR, Sigmon SC. Vermont hub-and-spoke model of care for opioid use disorder: development, implementation, and impact. J Addict Med. 2017;11(4):286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Clark HW. Health reform and the substance use disorder treatment system: a time of change. J Psychoactive Drugs. 2017;49(2):91–94. [DOI] [PubMed] [Google Scholar]
- 96. Maclean JC, Saloner B. The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence From the Affordable Care Act. Cambridge, MA: National Bureau of Economic Research; 2017. [PMC free article] [PubMed] [Google Scholar]
- 97. Andrews CM, Grogan CM, Westlake MA, et al. Do benefits restrictions limit Medicaid acceptance in addiction treatment? Results from a national study. J Subst Abuse Treat. 2018;87:50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Vestal C. Nurse licensing laws block treatment for opioid addiction. http://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2017/04/21/nurse-licensing-laws-block-treatment-for-opioid-addiction . Published 2017. Accessed March 1, 2018.
- 99. Fatseas M, Auriacombe M. Why buprenorphine is so successful in treating opiate addiction in France. Curr Psychiatry Rep. 2007;9(5):358–364. [DOI] [PubMed] [Google Scholar]
- 100. Health Canada. Dispensing Methadone for the Treatment of Opioid Dependence. Ottawa, Ontario: Health Canada; 1994. [Google Scholar]
- 101. Kaiser Family Foundation. Medicaid’s role in addressing the opioid epidemic. https://www.kff.org/infographic/medicaids-role-in-addressing-opioid-epidemic . Published 2018. Accessed March 1, 2018.
- 102. Lopez G. The new war on drugs. Vox. September 5, 2017. https://www.vox.com/policy-and-politics/2017/9/5/16135848/drug-war-opioid-epidemic . Accessed March 1, 2018.
- 103. Pew Charitable Trusts. More imprisonment does not reduce state drug problems. http://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2018/03/more-imprisonment-does-not-reduce-state-drug-problems. Published 2018. Accessed June 25, 2018.
- 104. Beletsky L, Davis CS. Today’s fentanyl crisis: prohibition’s Iron Law, revisited. Int J Drug Policy. 2017;46:156–159. [DOI] [PubMed] [Google Scholar]
- 105. Clifasefi SL, Lonczak HS, Collins SE. Seattle’s Law Enforcement Assisted Diversion (LEAD) program: within-subjects changes on housing, employment, and income/benefits outcomes and associations with recidivism. Crime Delinq. 2017;63(2):429–445. [Google Scholar]
- 106. Davis CS, Ruiz S, Glynn P, Picariello G, Walley AY. Expanded access to naloxone among firefighters, police officers, and emergency medical technicians in Massachusetts. Am J Public Health. 2014;104(8):e7–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: National Academies Press; 2017. [PubMed] [Google Scholar]