Abstract
Providing a fast and accurate diagnosis of acute large-vessel occlusion on computed tomography angiograms (CTAs) is essential for timely intervention and good stroke outcomes. However, the detection and appropriate management of incidental findings are also important parts of any clinical radiology practice and can greatly affect patient care. The intricate anatomy covered by CTAs of the head and neck coupled with the time pressures of acute stroke diagnosis creates an environment in which unrelated, important findings can potentially be missed. The purpose of our study was to document clinically actionable incidental findings on CTA in 225 patients undergoing acute stroke intervention.
After institutional review board approval, a retrospective six-year review of CTAs of the head and neck in patients undergoing acute stroke intervention was performed for actionable incidental vascular and nonvascular findings.
A total of 225 patients undergoing acute stroke intervention with documented intracranial large-vessel occlusion on CTAs were consecutively enrolled in the study. Incidental vascular findings were identified in 17 of 225 patients (7.5%, 95% confidence interval 5% to 12%). Previously unreported aneurysms ranging from 2 mm to 10 mm in size represented 18 of 19 vascular findings in these patients. Incidental nonvascular findings were identified in 32 patients (14%, 95% confidence interval 5% to 12%). These included malpositioned support lines and tubes; pneumothorax; interstitial lung disease; newly diagnosed metastatic disease; nasopharyngeal, parotid, and pituitary masses; and cervical spine compression fractures.
CTAs of the head and neck in patients undergoing acute stroke intervention contain a relatively high frequency of vascular and nonvascular incidental findings requiring further follow-up, and therefore should be evaluated carefully and systematically.
Keywords: Acute stroke, CTA head and neck, incidental findings, large-vessel occlusion, mechanical thrombectomy
Introduction
Several trials have firmly established mechanical thrombectomy as first-line treatment for patients with acute ischemic stroke related to large-vessel occlusion.1–4 Computed tomographic angiogram (CTA) of the head and neck is a widely used diagnostic study, because of its accuracy, availability, and speed of acquisition, for the detection of large-vessel stenosis and occlusion in patients presenting with symptoms of acute stroke.5 Prompt review of these studies is critical given the time-sensitive nature of acute stroke intervention. In addition to confirming acute stroke, CTAs have the potential to reveal a wide variety of incidental findings given the extent of anatomic coverage, which includes the brain parenchyma, soft tissues of the head and neck, and upper thorax. Urgency of acute stroke diagnosis coupled with the volume of imaging data acquired can often result in missed secondary diagnoses.
Incidental findings are not only a byproduct of imaging the necessary volume for a specific examination, but also a byproduct of continuous improvements in contrast and spatial resolution allowing for better visualization and detection.6 While some incidental findings are of little clinical significance, such as the classic example of a nonhypersecreting adrenocortical adenoma seen on abdominal CT,7 others pose a risk to the patient and warrant further workup or treatment. A retrospective study by Atalay et al.8 evaluating noncardiac findings on cardiac magnetic resonance imaging (MRI) demonstrated clinically significant findings associated with a new diagnosis, treatment, or intervention in 10% of cases. Similarly, a study by Hall et al.9 examining the prevalence of clinically relevant incidental findings on chest CTA for diagnosis of pulmonary embolism demonstrated new incidental findings requiring follow-up in 24% of cases.
The purpose of our study was to determine the nature and prevalence of incidental findings on head and neck CTAs in patients undergoing intervention for acute stroke.
Materials and methods
This study was approved by the institutional review board and was compliant with Health Insurance Portability and Accountability Act regulations. Patients were included with permission for a retrospective chart review. CTAs of patients who underwent intervention for acute stroke at a tertiary-care university medical center were reviewed from years 2011 to 2016. Acutely symptomatic patients with documented intracranial large-vessel occlusion on CTA who subsequently underwent mechanical thrombectomy were consecutively enrolled in the study. All patients were imaged with CTA within 24 hours of symptom onset or last-known-normal. The institutional CTA protocol consisted of noncontrast axial head CT with section thickness of 5 mm followed by CTA from the vertex to the aortic arch (80 ml of iodinated intravenous contrast material administered at 3–4 ml/second via a large-bore intravenous line; section thickness 1.25 mm, 120 kV, 281 mAs). Studies were performed on a multidetector helical CT scanner. Imaging technique included maximum intensity projection and three-dimensional volume-rendered images created by the radiologist on a separate workstation.
The studies were all interpreted by six board-certified neuroradiologists with five to 20 years of experience at the time of the study, including one of the authors (A.E.F, 20 years of experience). Each final report and imaging study were retrospectively reviewed by a radiology resident for the location of large-vessel occlusion on the CTA imaging study. Additional pertinent findings, including incidental vascular findings (such as aneurysm or presence of fibromuscular dysplasia) and incidental nonvascular findings (such as tumor, infection, pleural effusions, location of lines/tubes) were recorded for each study.
The electronic medical records were reviewed for each patient to determine the patient’s age at the time of each study. Patient history and physical notes and progress notes were evaluated as available to determine if findings concerning for malignancy were previously known, and for follow-up for certain imaging findings. Prior and subsequent radiology imaging studies were also reviewed as available to determine if findings concerning for malignancy were previously seen, and for follow-up for certain imaging findings.
Pulmonary and thyroid nodules measuring less than 1 cm were excluded given the variability and relatively long duration of time required for follow-up for these findings. Similarly, findings of degenerative disc disease were excluded given variability in clinical management and follow-up.
Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the study institution. REDCap is a secure, web-based application designed to support data collection for research studies.10 Data were tabulated for total counts for various types of findings using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA).
Results
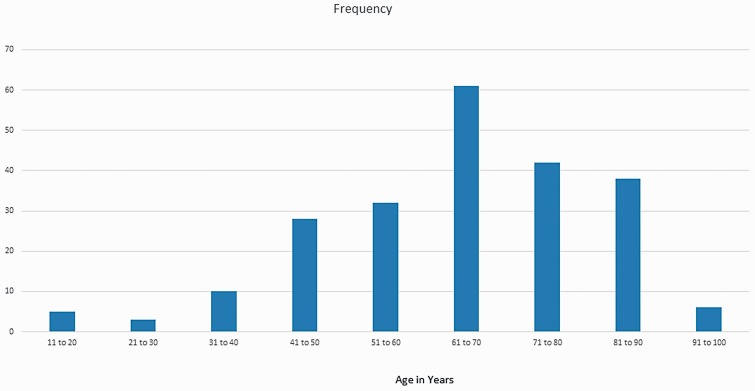
Between 2011 and 2016, a total of 225 patients undergoing acute stroke intervention with CTA of the head and neck were identified (see Table 1). Fifty of 225 patients (22%) had occlusions of the internal cerebral artery, 143 of 225 patients (64%) had occlusions of the middle cerebral artery, and 32 of 225 patients (14%) had occlusions of the basilar artery. The average patient age was 65 years (range, 16–95 years), and median age was 67 years (see Figure 1). A total of 119 patients were female (53%). Incidental vascular and nonvascular findings were identified in 47 of 225 patients (20.8%).
Table 1.
Demographics of 225 patients with large vessel occlusion on computed tomography angiogram undergoing stroke intervention.
| Male | 106/225 |
| Female | 119/225 (53%) |
| Average age in years | 65 (range 16 to 95) |
| Internal carotid artery occlusion | 51/225 (23%) |
| Middle cerebral artery occlusion | 144/225 (64%) |
| Basilar artery occlusion | 30/225 (13%) |
Figure 1.
Histogram showing age distribution of patients included in the study.
Incidental vascular findings were identified in 17 of 225 patients (7.5%, 95% confidence interval 5% to 12%). Of these 17 patients, the location of the initial large-vessel occlusion was reported as the internal carotid artery for four patients, middle cerebral artery for 12 patients, and basilar artery for one patient. A total of 19 incidental vascular findings were reported. Aneurysms represented the majority of incidental vascular findings (18 of the 19 vascular findings). Fibromuscular dysplasia represented only one of the 19 vascular findings, with involvement of the distal contralateral internal carotid artery and ipsilateral vertebral artery in a patient with internal carotid artery occlusion. All aneurysms were unknown prior to CTA head and neck imaging. The size of aneurysms identified ranged from 2 to 10 mm, with an average size of 3 mm (Figure 1). Eleven of the 18 aneurysms were contralateral in location compared to the site of occlusion, while six of the 18 aneurysms were ipsilateral in location. One of the 18 aneurysms was located at the basilar tip. The largest 10 mm aneurysm was identified in the ipsilateral carotid terminus in a patient with middle cerebral artery occlusion. Bilateral aneurysms at the level of the middle cerebral artery trifurcations, measuring 5 mm and 6 mm, were identified in one patient with basilar artery occlusion. Two internal cerebral artery aneurysms, measuring 2 mm each, were identified on the contralateral side of one patient with middle cerebral artery occlusion.
Incidental nonvascular findings were identified in 32 of 225 patients (14%, 95% confidence interval 10% to 20%). Four of 225 patients (1.8%) had critical incidental intrathoracic findings, including three malpositioned endotracheal tubes in the right main stem bronchus and a moderate-sized pneumothorax. One malpositioned peripherally inserted central catheter was identified and found to have its tip looping in the internal jugular vein. Eight of 225 patients (3.5%) had pleural effusions, with one pleural effusion demonstrating worsening with development of associated mediastinal shift on same-day follow-up chest radiograph. Four of 225 patients (1.7%) were incidentally found to have pneumonia. One patient was found to have ground-glass opacities and reticular thickening concerning for interstitial lung disease, which was confirmed on follow-up dedicated chest CT imaging.
There were three patients with imaging findings concerning for previously undiagnosed malignancy, and one patient with a known lung mass redemonstrated on preprocedural CTA. One patient had an incidental right nasopharyngeal soft tissue mass extending into the carotid space with associated bony erosion of the skull base, concerning for tumor. Another patient had a 2.7 cm irregular lung mass concerning for primary malignancy, for which a biopsy was recommended. Mediastinal and cervical lymphadenopathy with a pathologic C7 compression fracture were noted in a third patient, with follow-up whole-body CT imaging demonstrating a spiculated 1.5 cm lung nodule and extensive metastatic disease (Figure 2).
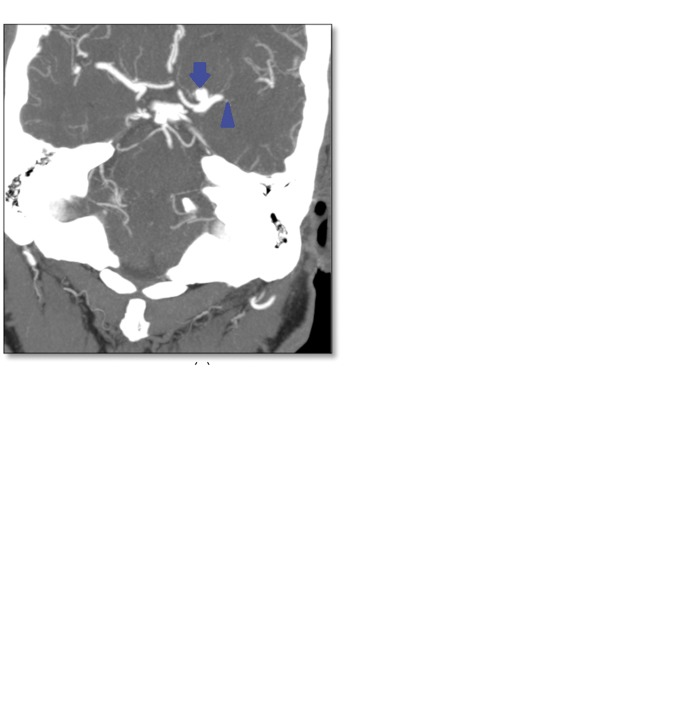
Figure 2.
A 66-year-old man with a left M1 occlusion and an incidental 7 mm middle cerebral artery aneurysm just proximal to the site of occlusion. The first image is a maximum intensity projection from the computed tomography angiogram showing a 7 mm aneurysm (arrow) adjacent to the site of occlusion (arrowhead). Intraprocedural angiogram (second image) during stroke intervention shows the aneurysm (arrow) and site of occlusion (arrowhead). The third image is a control angiogram showing successful recanalization of the previously occluded middle cerebral artery after mechanical thrombectomy (arrowhead) as well as the left middle cerebral artery aneurysm (arrow).
Additional incidental masses included a 10 mm meningioma at the vertex, a 17 mm orbital venolymphatic malformation, and an 8 mm pituitary mass. One patient was found to have multiple scattered intracranial hyperdensities that were determined to represent multiple cavernous malformations on subsequent MRI evaluation. Five parotid gland masses ranging in size from 1.2 cm to 2.1 cm and three thyroid nodules ranging in size from 1 cm to 2.3 cm were identified on CTA.
Bony abnormalities were identified in four of 225 (1.8%) patients, mostly associated with underlying malignancy or infection. One patient had an acute comminuted clavicular fracture, sustained during a fall following the onset of acute hemiplegia.
When the results were analyzed according to age, incidental findings were present in 11 out of 47 patients under the age of 50 (23%), and 36 out of 178 patients over the age of 50 (20%); this difference was not statistically significant. When analyzed using the median age of 67 years, incidental findings occurred in almost an equal number of patients below and above the age cut-off. Analysis by gender revealed no statistically significant difference in the incidence of unexpected/incidental findings on CTA either.
Discussion
Our study identified potentially actionable, incidental vascular and nonvascular findings in 47 of 225 patients (20.8%, 95% confidence interval 16% to 27%). This is similar to a study within cardiac imaging, which identified potentially significant, incidental findings in 19.7% of patients undergoing cardiac CTA immediately after coronary artery bypass grafting surgery.11 In our study, aneurysms represented the majority of incidental vascular findings. Multiple important incidental pulmonary findings were also identified, including four critical findings requiring timely communication with the clinical team. At least three patients had findings concerning for previously unreported malignancy, with multiple incidental masses identified in other studies. While the absolute number of incidental findings was higher in patients older than age 50 compared with patients younger than 50, the proportion of incidental findings was not statistically significant by age or gender, underscoring the fact that important incidental findings may occur in a patient of any age or gender.
CTAs of the head and neck in patients undergoing acute stroke intervention harbor important and urgent findings with surprising frequency, and should not be overlooked even in this time-sensitive clinical scenario. A widely publicized study by Drew et al. provided evidence that radiologists are not immune to inattentional blindness; 83% of radiologists failed to see a picture of a gorilla on a chest CT while looking for lung nodules.12 In another study, multiple radiologists, intensivists, and emergency physicians missed a retained guidewire on chest radiograph and chest CTs in a patient with pulmonary edema and large pulmonary emboli.13 A study by Wnorowski et al. on the diagnostic yield of triple-rule-out chest CTs in symptomatic patients presenting to the emergency department showed incidental findings in 35% of cases, the majority of which required follow-up.14 In that study, there was a 10% incidence of thoracic malignancy, excluding pulmonary nodules. An additional 10% incidence of noncoronary chest pain was also reported. Another study by Vernooji et al. on incidental findings on brain MRI in asymptomatic healthy volunteers showed incidental findings in 10% of patients, most commonly infarcts, aneurysms, and benign brain tumors.15 The reported frequency of incidental findings in the study by Vernooji et al. is lower than in our population for several reasons: The anatomic coverage in our study is greater, from the pulmonary arteries to the vertex of the skull, our patient population was not asymptomatic or necessarily healthy, and our study was optimized for the evaluation of the craniocervical vasculature. It is also probable that the true frequency of incidental findings on imaging studies is underestimated, as some findings are probably missed by the interpreting radiologist for a variety of reasons. Satisfaction of search certainly plays a role; this phenomenon is familiar to radiologists, and is extensively documented in the radiology literature.16,17
While many incidental findings are inconsequential and pose minimal (if any) risk to the patient, some findings can be detrimental to the patient if missed. Aneurysms bear special consideration in our patient population because of the surprisingly frequent occurrence in our patient cohort. A ruptured intracranial aneurysm carries a 51% case fatality rate on average, with a 30% rate of disability in survivors.18 Timely intervention can be life saving. An additional consideration is that four-vessel cerebral angiograms are not typically performed in stroke interventions because of time constraints and the clinical status of the patient: Only the vessel of interest is investigated with the goal of complete recanalization as rapidly as possible. As a result, a missed aneurysm could remain undetected until rupture.
There are several limitations to this study. First and foremost, the generalizability of this study is limited as the study cohort is composed of critically ill patients who presented with high clinical suspicion for acute stroke, who underwent CTA, and who ultimately received acute stroke intervention. In addition, this is a retrospective study in which prior and follow-up documentation is unavailable for multiple patients. Specifically, lack of clinical, radiologic and/or pathologic follow-up limits the ability to determine eventual outcomes for all potentially actionable or malignant findings. Similarly, subcentimeter masses and degenerative disease were excluded from the study as these often require relatively long-term imaging and clinical follow-up for further evaluation. A prospective study would be better able to eliminate bias and provide better follow-up for eventual outcomes of various abnormalities.
Conclusions
Incidental findings on imaging studies are inevitable in radiology. Familiarity with the breadth of abnormalities that are often identified in addition to large-vessel occlusion on CTA of the head and neck may better guide future interpretation of these studies. In addition, timely recognition and communication of these abnormalities to the primary team can have a significant impact on patient safety and quality of patient care beyond successful intracranial revascularization.
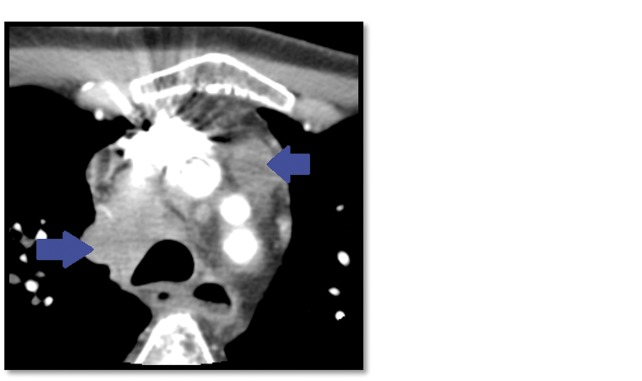
Figure 3.
A 59-year-old man presenting with an acute stroke caused by intracranial large-vessel occlusion, found to have an incidentally discovered metastatic mediastinal adenopathy (arrows, first image) and a pathologic fracture of the C7 vertebral body (arrow, second image) on computed tomography angiogram of the head and neck. Both findings were new and unknown to the patient and clinical team at the time of the scan.
Table 2.
Incidental intracranial aneurysms identified in 225 patients with acute stroke. Incidental intracranial aneurysms identified in 16/225 patients (8%, 95% confidence interval 4% to 11%).
| No. of female patients with incidental aneurysms | 11 out of 16 (one patient had two aneurysms) |
| Ipsilateral to stroke territory | 5/18 (31%) |
| Location (n%) | |
| Internal carotid artery | 9/18 (50%)a |
| Anterior communicating | 2/18 (11%) |
| Middle cerebral artery | 2/18 (11%)a |
| Anterior cerebral artery | 1/18 (6%) |
| Posterior communicating | 1/18 (6%) |
| Posterior cerebral artery | 1/18 (6%) |
| Basilar artery | 1/18 (6%) |
| Vertebral artery | 1/18 (6%) |
Denotes two intracranial aneurysms detected in a single patient.
Table 3.
Incidental nonvascular findings identified in 225 patients on computed tomography angiogram.
| Pleural effusions (moderate) | 8/225 (4%, 95% confidence interval 1.5% to 7%) |
| Parotid masses | 5/225 (2.5%, 95% confidence interval 0.7% to 5%) |
| Pneumonia | 4/225 (2%, 95% confidence interval 0.5% to 4.5%) |
| Malpositioned lines and tubes | 4/225 (2%, 95% confidence interval 0.5% to 4.5%) |
| Thyroid nodules | 3/225 (1.5%, 95% confidence interval 0.3% to 3.8%) |
| Metastases | 3/225 (1.5%, 95% confidence interval 0.3% to 3.8%) |
| Pathologic fractures and erosions | 3/225 (1.5%, 95% confidence interval 0.3% to 3.8%) |
| Traumatic fractures | 1/225 (0.5%, 95% confidence interval 0% to 2.5%) |
| Pneumothorax | 1/225 (0.5%, 95% confidence interval 0% to 2.5%) |
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Eng J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 2.Saver JL, Goyal M, Bonafé A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Eng J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 3.Campbell BC, Donnan GA, Lees KR, et al. Endovascular stent thrombectomy: The new standard of care for large vessel ischaemic stroke. Lancet Neurol 2015; 14: 846–854. [DOI] [PubMed] [Google Scholar]
- 4.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Eng J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 5.Menon BK, d’Esterre CD, Qazi EM, et al. Multiphase CT angiography: A new tool for the imaging triage of patients with acute ischemic stroke. Radiology 2015; 275: 510–520. [DOI] [PubMed] [Google Scholar]
- 6.Lumbreras B, Donat L, Hernández-Aguado I. Incidental findings in imaging diagnostic tests: A systematic review. Br J Radiol 2010; 83: 276–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young WF., Jr The incidentally discovered adrenal mass. N Engl J Med 2007; 356: 601–610. [DOI] [PubMed] [Google Scholar]
- 8.Atalay MK, Prince EA, Pearson CA, et al. The prevalence and clinical significance of noncardiac findings on cardiac MRI. AJR Am J Roentgenol 2011; 196: W387–W393. [DOI] [PubMed] [Google Scholar]
- 9.Hall WB, Truitt SG, Scheunemann LP, et al. The prevalence of clinically relevant incidental findings on chest computed tomographic angiograms ordered to diagnose pulmonary embolism. Arch Intern Med 2009; 169: 1961–1965. [DOI] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mueller J, Jeudy J, Poston R, et al. Cardiac CT angiography after coronary bypass surgery: Prevalence of incidental findings. AJR Am J Roentgenol 2007; 189: 414–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drew T, Võ ML, Wolfe JM. The invisible gorilla strikes again: Sustained inattentional blindness in expert observers. Psychol Sci 2013; 24: 1848–1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lum TE, Fairbanks RJ, Pennington EC, et al. Profiles in patient safety: Misplaced femoral line guidewire and multiple failures to detect the foreign body on chest radiography. Acad Emerg Med 2005; 12: 658–662. [DOI] [PubMed] [Google Scholar]
- 14.Wnorowski AM, Halpern EJ. Diagnostic yield of triple-rule-out CT in an emergency setting. AJR Am J Roentgenol 2016; 207: 295–301. [DOI] [PubMed] [Google Scholar]
- 15.Vernooij MW, Ikram MA, Tanghe HL, et al. Incidental findings on brain MRI in the general population. N Eng J Med 2007; 357: 1821–1828. [DOI] [PubMed] [Google Scholar]
- 16.Berbaum KS, Franken EA, Dorfman DD, et al. Cause of satisfaction of search effects in contrast studies of the abdomen. Acad Radiol 1996; 3: 815–826. [DOI] [PubMed] [Google Scholar]
- 17.Berbaum KS. Satisfaction of search experiments in advanced imaging. [International Society for Optics and Photonics] SPIE Proceedings 8291, Human Vision and Electronic Imaging XVII 2012; 82910V.
- 18.Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Eng J Med 2006; 354: 387–396. [DOI] [PubMed] [Google Scholar]