Abstract
This study aimed to provide the first description of the whole-body bioimpedance vector of nine non-professional triathletes, and to assess body mass (BM) and vector variations evoked by an ultra-endurance triathlon event. Anthropometric and bioelectrical assessments were performed before (PRE), after (POST), and 48 hours following the race (POST48h). Bioimpedance vector analysis (BIVA) showed triathletes’ vectors placed to the left of the major axis and mostly outside the 50% tolerance ellipse of the reference population. Vector migration in POST indicated dehydration, paralleled by a decrease in BM (p = 0.0001). Increased hydration status from POST to POST48h was suggested by a reversed vector migration and increased BM (p = 0.0001). Compared to PRE, POST48h values reflected fluid retention by changes in BIVA, while BM was still lower (p = 0.0001). Racing time was positively related to basal resistance -R/h- (r = 0.68; p = 0.04) and bioimpedance -Z/h- (r = 0.68; p = 0.045). Besides, basal R/h and Z/h were positively related to PRE-to-POST changes of R/h and Z/h (r = 0.80; p = 0.009). PRE-to-POST changes of R/h and Z/h were positively related to racing time (r = 0.80, p = 0.01) and internal workload (r = 0.80, p ≤ 0.02). Notwithstanding the lack of significant correlation between BM and bioelectrical parameters, the vector’s behavior was explained from a multifactorial perspective (including BM variations) by using multiple regression analysis. On the other hand, BM changes were not related to racing time, internal workload or energy deficit (ranges: r = - 0.46 to 0.65; p = 0.06 to 0.98). In conclusion, these triathletes exhibit a specific bioelectrical distribution. Furthermore, vector migration was consistent with fluid loss induced by the event. Finally, vector analysis seems to provide additional information about hydration changes 48h after the event in comparison with BM alone.
Key points.
BIVA shows a specific bioelectrical distribution in a group of triathletes in comparison with the healthy, general reference population.
Although BIVA is not currently able to identify type and magnitude of fluid loss, vector migration appears to be consistent with fluid loss induced by a UET event and with fluid retention 48 h after the race.
BIVA seems to provide additional information about hydration changes 48 h after the UET event compared with BM alone. However, it is important to highlight that neither BM nor BIVA can really identify what happened to TBW. BIVA reflect changes in ECW estimates only. Thus, ICW may still be reduced (captured by BM 48h post-race) with a migration of fluids to the ECW space.
This method could be sensitive to different performance levels between triathletes and to muscle disruption 48 hours after completing a UET event.
Key words: Body composition, hydration, bioimpedance, BIVA, performance, triathlon
Introduction
Ultra-endurance triathlon (UET) combines three disciplines (3.8-km swimming, 180-km cycling, 42.2-km running) and involves from 8 to 17 hours of competition depending on the fitness level and efficiency rates of the triathlete (Laursen and Rhodes, 2001). During a UET, dehydration and glycogen depletion are the main causes of metabolic fatigue, whereas gastrointestinal problems, hyperthermia and hyponatremia are potential threats to the triathletes’ health (Jeukendrup et al., 2005).
Dehydration decreases endurance performance (Cheuvront and Kenefick, 2014) and increases the injury risk (Oppliger and Bartok, 2002). Furthermore, it is an important factor in race completion in ultra-endurance events (Knechtle et al., 2015). However, the lack of a ‘gold-standard’ marker of hydration status must be emphasized. The assessment of body hydration status is a dynamic and complex process and no method is valid for all situations (Armstrong, 2007). Finding a method which is sensitive to the type (intra- or extra-cellular) and magnitude of dehydration is necessary (Cheuvront and Kenefick, 2017).
A common method to assess dehydration in endurance athletes has been pre- and post-exercise body mass (BM) control (McGarvey et al., 2010). Ultra-endurance athletes may suffer great BM losses (Hew-Butler et al., 2007; Laursen et al., 2006; Sharwood et al., 2004), principally due to the sweat rate (Cheuvront and Kenefick, 2017). Other possible sources are the respiratory and urinary/fecal water losses (Cheuvront and Kenefick, 2017).
Literature supports that reductions in total BM of ≥ 2% generate negative effects on the endurance performance of the athletes (Cheuvront and Kenefick, 2014; McDermott et al., 2017). However, well-trained ultra-triathletes should expect to lose about 3% of their BM without any adverse consequences (Laursen et al., 2006). Therefore, despite the fact that measuring BM variation provides a simple estimate of post-race hydration status in athletes (Maughan et al., 2007; McGarvey et al., 2010), it is not always a reliable measure. Furthermore, it may give rise to misleading results since, for instance, a significant loss of BM may be observed without an effective hypohydration resulting (Cheuvront and Kenefick, 2017; Maughan et al., 2007).
In this regard, the bioelectrical impedance vector analysis (BIVA) emerges as a technique to assess hydration status with no inherent errors of bioimpedance equations or requirements for biological assumptions such as the constant tissue hydration (Lukaski and Piccoli, 2012; Norman et al., 2012). The method is used in the clinical context for the analysis of both homeostatic state and possible vector variations resulting from modifications in body fluid status (Norman et al., 2012; Piccoli, 2010). In the exercise context, as mentioned in Heavens et al. (2016), directional changes in vector values from serial measurements are consistent with fluid loss according to the theory (Piccoli et al., 1994; Piccoli et al., 2002). Therefore, since any vector change is a function of extracellular water –ECW- changes (Segal et al., 1991) because a 50 kHz current does not penetrate cells (De Lorenzo et al., 1997), a potential strength of BIVA would be to afford insight into ECW dehydration (Heavens et al., 2016). Moreover, it might help to provide additional information about hydration changes in ultra-endurance events than, for instance, BM loss alone. Thus, due to the already mentioned deleterious effects of dehydration and to the potential strengths of the method, BIVA is especially interesting for hydration assessment in both sport training and competitive event (Carrasco-Marginet et al., 2017; Koury et al., 2014).
In this way, this study aimed at providing the first description of the whole-body bioelectrical impedance vector in a group of ultra-endurance triathletes, and to assess the variation in the BM and the bioimpedance vector of the athletes evoked during a UET event. We hypothesized that a specific distribution of BIVA would be found in the triathletes when compared to the reference population, and that the BM and the directional changes of the vector in this type of events would be consistent with a decrease in body fluids, according to the literature.
Methods
Participants
An advertisement was placed on the triathlon race webpage to recruit non-professional male triathletes. The inclusion criteria were to train at least 10 h per week and the participation in a minimum of one UET during the past 3 years.
Sample size was calculated based on a potential increase of the impedance vector module (Z) of 4% based on our previous observations in synchronized swimmers after a high-intensity training session (Carrasco-Marginet et al., 2017) as the only available estimate for short-term (< 24 hours) bioelectrical changes (Castizo-Olier et al., 2018). Seven athletes per intervention group were required (two-tailed > = 0.05, > = 0.80, effect size = 0.95, change SD = 2.5).
Nine experienced, well-trained, non-professional ultra-endurance male triathletes volunteered for the study [mean ± SD: age 36.6 ± 5.5 years; body mass (BM) 76.0 ± 6.9 kg; height 1.75 ± 0.06 m; body mass index (BMI) 24.8 ± 2.0 kg/m2; V̇O2max = 66.3 ± 4.3 ml/kg/min]. The participants had an average of 10 ± 3 years of experience in UET and ultra-endurance events, and they had been training regularly for approximately 14–20 hours per week for at least three years. All participants passed a medical examination before the race and gave their informed written consent prior to their participation. The study was performed following the Helsinki Declaration Statement and was approved by the Ethics Committee for Clinical Sport Research of Catalonia.
Study design
The participants completed a UET race, specifically, the “Extreme Man Salou–Costa Daurada Triathlon”, composed of three segments consisting of a 3.8 km swim, 180 km cycle with a positive elevation over 2600 m and a 42.2 km marathon run. The mean (range) ambient temperature was 26 °C (13-30 °C), the water temperature was 21 °C (20.8-21.2 °C) and the relative humidity was 77% (64% - 94%). The mean wind speed was 1.3 m/s (range 0.3 – 5.0 m/s). All the triathletes undertook the tests measurements designed for the study at three time points: before the race (PRE), after finishing the race (POST) and 48h after POST measurements (POST48h). Detailed information about the study design, race characteristics and procedures related to the performance variables analyzed in the present study (racing time, internal workload and energy deficit) can be consulted in a previously published article (Barrero et al., 2014).
Procedures
Anthropometric and bioelectrical variables were obtained by the same trained investigator in a thermally neutral room (25.0 ± 1.0ºC).
Anthropometric assessment: Anthropometric measurements were performed according to the standard criteria of The International Society for the Advancement of Kinanthropometry (ISAK) (Stewart et al., 2011). Body height (h) was assessed to the nearest 1 mm using a telescopic stadiometer (Seca 220®, Hamburg, Germany). BM was measured to the nearest 0.05 kg using a calibrated weighing scale (Seca 710®, Hamburg, Germany). BMI (kg/m2) was calculated as body mass / height2. The circumferences of the left and right thigh –CLT and CRT, respectively- (taken at mid-thigh) and the left and right calf –CLC and CRC, respectively- (taken at the greater perimeter of the calf) were measured to the nearest 1 mm using an anthropometric tape (Lufkin Executive®, Lufkin, USA), in order to evaluate possible variations between the different time points. This is important since the whole-body impedance can be significantly reduced if a lower limb affected by swelling is in the same side as the electrodes (Codognotto et al., 2008).
Whole-Body Bioimpedance assessment: BIVA uses raw bioelectrical impedance parameters, i.e., resistance (“R”, the opposition to flow through intra- and extracellular ionic solutions) and reactance (“Xc”, additional opposition from the capacitance effect of cell membranes and tissue interfaces), standardized by height in order to remove the effect of conductor length, yielding a vector, which is plotted in an RXc graph (Piccoli et al., 1994). The vector direction (PA) is the geometric relationship between R and Xc. PA is a validated indicator of cellular health (Norman et al., 2012; Yanovski et al., 1996) and has been interpreted as an indicator of fluid distribution between intra- and extracellular compartments (Goovaerts et al., 1998), reporting an inverse correlation with the ECW - total body water (TBW) ratio (Chertow et al., 1995). The length of the vector states hydration status from fluid overload (short vector) to exsiccosis (longer vector), and lateral migration of the vector projects a decrease or increase in the dielectric mass (membranes and tissue interfaces) of soft tissues (Piccoli, 2005). Individual vectors can be normalized to Z scores and classified on the RXc score graph, according to the tolerance ellipses (50%, 75% and 95%) of a reference population, independently of the bioimpedance analyzer used (Piccoli et al., 2002). Individuals positioned within the 50% tolerance ellipses, according to the literature (Lukaski, 2013; Lukaski and Piccoli, 2012) are considered “normally hydrated”.
In the present study, R and Xc were measured by a previously calibrated multifrequency bioimpedance analyser (Z-Métrix®, BioparHom®, Bourget du Lac, France) that emitted 77 µA alternating sinusoidal current at different frequencies (1 to 325 kHz). The device provides impedance values with an accuracy characterized by an average error of 0.95% ± 1.58% and an average repeatability errors of 0.55% ± 0.38% for all the frequency range (Moreno, 2015). The 50-kHz frequency was selected for BIVA (Piccoli, 2010). The bioimpedance module [Z=√((R2+Xc2))] and phase angle [PA=arctan(Xc/R)·(180/π)] were derived from the bioelectrical raw parameters. Triathletes were tested under controlled conditions through the standard whole-body, tetrapolar, distal BIA technique (Yanovski et al., 1996). All the participants arrived to the measurements after voiding their bladder and rectum (Rush et al., 2006). Triathletes were tested in PRE and POST48h in euhydration state according to a standardized 8-point urine color chart –PRE: 1.7 ± 0.7; POST48h: 1.8 ± 0.8- (Armstrong et al., 1994). Before placing the electrodes (Red Dot™, 3M Corporate Headquarters, St. Paul, MN, USA), the skin was prepared by shaving the electrode site to remove hair, rubbing with gel and cleaning with alcohol in order to reduce possible interferences in the assessment (Hermens et al., 1999). A waterproof pen was used to mark the anatomical sites for electrodes, in order to preserve the same location, due to the influence of the electrode placement modification in the bioelectrical outputs (Gualdi-Russo and Toselli, 2002). Just before the bioimpedance measurements, core and skin temperatures were registered. PRE and POST48h bioimpedance assessments were performed after 10 minutes of stabilization (Slinde et al., 2003). Measurements were repeated until they were stable to within 1 Ω (usually up to three times within an interval of 20-30 s) and the average value was used in calculations. POST measurements were perfomed once the core and skin temperatures were close to the basal values (± 1 ºC), 35 ± 5 min after finishing the race. Before measurements, participants were instructed to take a cold shower (as cold as tolerable) for 10 minutes post-race, in order to reduce cutaneous blood flow and temperature and remove accumulated electrolytes (Peiffer et al., 2009).
Temperature assessment: An increase in the skin temperature can lead to an important decrease in R (Caton et al., 1988). Temperature variations within the range of 1 ºC seem not to significantly affect the impedance (Liang and Norris, 1993) and greater differences must be avoided. Therefore, in the present study, core (ºCcore) and skin temperatures of the right hand (ºChand) and foot (ºCfoot) were measured using thermistors connected to a data logger (Squirrel 2010, Grant Instruments Ltd, Cambridge, UK).
Internal workload assessment: To estimate the total workload of exercise performed by each participant in the race, the training impulse (TRIMP) method was used.
Energy deficit assessment: All the wraps and bottles of each participant were collected in order to calculate the energy intake during the race. The energy expenditure during the race was estimated through three different individualized equations (one for each segment), derived from preliminary exercise tests. Finally, the energy deficit was calculated as energy intake minus energy expenditure.
Statistical analysis
Descriptive statistics for each independent variable were calculated. After testing each variable for the normality of the distribution (Shapiro-Wilks test), differences in anthropometric (BM and circumferences of the thigh and calf), temperature and bioelectrical data (R, Xc, Z, R/h, Xc/h, Z/h and PA) PRE, POST and POST48h were analyzed through a repeated-measures one-way ANOVA (RM-ANOVA). Post-hoc analyses were performed using the Bonferroni correction and the p-value was adjusted at padj = 0.017. The magnitude of ratio changes was computed as delta percent values (Δ%). Effect sizes (ES) were calculated using Cohen’s d and defined as small, d ≤ 0.2; medium, d ≤ 0.5; and large, d ≤ 0.8. Pearson’s correlation coefficient was applied to determine possible associations between: a) bioelectrical baseline values (PRE; POST; POST48h) vs. bioelectrical delta values (PRE-to-POST; POST-to-POST48h; and PRE-to-POST48h); b) bioelectrical data (baseline and delta values) vs. racing time, internal workload, energy deficit and BM delta values; c) BM delta values vs. racing time, internal workload, energy deficit. A multiple linear regression analysis was performed in order to explain the changes at the same time points of each bioelectrical (dependent) variable in relation to performance (independent) variables: racing time, internal workload, energy deficit, and BM changes. The adjusted square multiple regression coefficient (rm2adj) was used to quantify the goodness-of-fit of the model. To add information to the multivariate analysis, the process was further applied in reverse, alternating the role between dependent and independent variables (i.e. the analysis was performed to explain the performance variables results in relation to the changes of each bioelectrical variable). Whole-body individual bioimpedance vectors were analyzed by the standard, reference RXc score graph (Piccoli et al., 2002), according to the healthy, Italian reference population (Piccoli et al., 1995). The RXc mean graph was performed to compare the whole-body mean vector of triathletes vs. the reference population. A two-sample Hotelling’s T2 test was used to determine the vector differences between triathletes vs. the reference population. P < 0.05 was considered significant.
Results
The triathletes of the present study completed the race in 752 ± 70 min, the estimated internal workload was 1055 ± 172 arbitrary units, and the energy deficit was 30.5 ± 5.5 MJ (7283 ± 1321 kcal).
All bioelectrical variables significantly increased post-race and decreased at POST48h (Table 1), except PA. No statistically significant differences were found for lower-limbs circumferences in any time points (Table 1). The same was observed for the temperature differences: PRE-to-POST ºCcore: 0.0 ± 1.2 %; PRE-to-POST48h ºCcore: -0.3 ± 1.3 %; PRE-to-POST ºChand: 0.1 ± 1.9 %; PRE-to-POST48h ºChand: 0.4 ± 2.4 %; PRE-to-POST ºCfoot: -0.3 ± 2.4 %; PRE-to-POST48h ºCfoot: 0.2 ± 2.1 %; p > 0.05.
Table 1.
Anthropometric and bioelectrical variables before (PRE), after (POST), and 48 hours after the race (POST48h).
| PRE | POST | POST48h | PRE–POST | Δ-value (%) | Cohen’s d | ||||
|---|---|---|---|---|---|---|---|---|---|
| POST–POST48h | PRE–POST48h | PRE–POST | POST–POST48h | PRE–POST48h | |||||
| Anthropometric | |||||||||
| BM (kg) | 76.0 (6.9) | 72.1 (6.1) | 75.0 (6.3) | -5.0 (0.9)* | 4.0 (0.9)* | -1.3 (1.1)* | 3.9‡ | -4.3‡ | 1.1‡ |
| CRT (mm) | 54.0 (1.7) | 53.3 (1.9) | 53.9 (1.7) | -1.3 (1.7) | 1.1 (1.8) | -0.2 (0.3) | 0.8‡ | -0.6† | 0.8‡ |
| CLT (mm) | 54.2 (1.8) | 53.5 (2.0) | 54.1 (1.7) | -1.2 (1.7) | 1.1 (1.7) | -0.2 (0.3) | 0.7† | -0.6† | 0.5† |
| CRC (mm) | 38.1 (1.3) | 37.7 (1.5) | 38.0 (1.3) | -1.1 (1.6) | 0.9 (1.6) | -0.3 (0.4) | 0.7† | -0.6† | 0.8‡ |
| CLC (mm) | 38.3 (1.3) | 37.8 (1.5) | 38.2 (1.2) | -1.2 (1.6) | 1.0 (1.8) | -0.2 (0.4) | 0.7† | -0.5† | 0.6† |
| Bioelectrical | |||||||||
| R (Ω) | 452.6 (45.8) | 470.0 (56.6) | 435.2 (46.4) | 3.7 (2.3)* | -7.2 (2.9)* | -3.9 (2.1)* | -1.4‡ | 2.2‡ | 1.9‡ |
| Xc (Ω) | 60.6 (4.4) | 65.6 (4.6) | 55.5 (3.7) | 8.3 (3.7)* | -15.2 (4.5)* | -8.2 (4.8)* | -2.3‡ | 3.0‡ | 1.7‡ |
| Z (Ω) | 456.6 (45.8) | 474.6 (56.5) | 438.8 (46.2) | 3.8 (2.3)* | -7.4 (2.9)* | -3.9 (2.0)* | -1.5‡ | 2.2‡ | 2.0‡ |
| R/h (Ω/m) | 258.4 (22.4) | 268.3 (28.3) | 248.6 (24.0) | 3.7 (2.3)* | -7.2 (2.9)* | -3.9 (2.1)* | -1.5‡ | 2.3‡ | 1.9‡ |
| Xc/h (Ω/m) | 34.7 (2.8) | 37.5 (2.8) | 31.8 (2.4) | 8.3 (3.7)* | -15.2 (4.5)* | -8.2 (4.8)* | -2.3‡ | 3.0‡ | 1.7‡ |
| Z/h (Ω/m) | 260.8 (22.4) | 270.9 (28.3) | 250.7 (23.9) | 3.8 (2.3)* | -7.4 (2.9)* | -3.9 (2.0)* | -1.5‡ | 2.3‡ | 2.0‡ |
| PA (Ω) | 7.7 (0.5) | 8.0 (0.7) | 7.3 (0.7) | 3.7 (4.9) | -8.7 (4.9)* | -5.4 (6.4) | -0.8‡ | 1.7‡ | 0.9‡ |
| r (R/h, Xc/h) | 0.52 | 0.65 | 0.27 | – | – | – | – | – | – |
Values are mean ± SD (95% CI); BM, body mass; CRT, circumference of the right thigh; CLT, circumference of the left thigh; CRC, circumference of the right calf; CLC, circumference of the left calf; R, resistance; Xc, reactance; Z, impedance vector module; h, body height; PA, phase angle; r, Pearson’s correlation coefficient between R/h and Xc/h; time-point differences:
*RM-ANOVA, repeated measures analysis of variance with Bonferroni post-hoc test, significance at padj < 0.017
†, medium effect size (d ≤ 0.5)
‡, large effect size (d ≤ 0.8).
The BIVA score graph (Figure 1A) showed that the triathletes’ vectors fell mostly outside the 50% tolerance ellipse and occupied a position more to the left of the major axis compared with the reference population, indicating a higher density of body cell mass (BCM) than the reference population.
Figure 1.
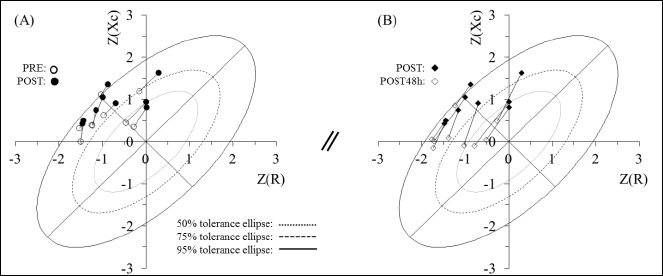
Individual vector score values for the RXc score graph with 50%, 75%, and 95% tolerance ellipses are plotted for: A) PRE- to POST-race, B) POST- to POST48h-race. Z(R), resistance Z score; Z(Xc), reactance Z score.
The BIVA mean graph (Figure 2) also showed the mean triathletes’ vector shifted to the left and upwards (T2 = 18.6; p = 0.0001), and therefore with greater PA, in comparison with the reference population.
Figure 2.
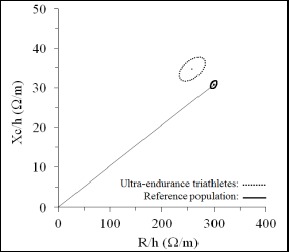
RXc mean graph. The 95% confidence ellipses for the mean impedance vectors of triathletes (dotted line ellipse) and the healthy male reference population (solid line ellipse with vector) (Piccoli et al., 1995) are shown. R/h, height-adjusted resistance; Xc/h, height-adjusted reactance.
The BIA vector migration was characterized by an increase in R/h and Xc/h (p = 0.001), indicating dehydration after the race (Figure 1A). This was in agreement with the observed loss of BM (p = 0.0001).
On the other hand, increased BM and decreased bioelectrical values (p = 0.0001) were observed from POST to POST48h. When PRE to POST48h were compared, BM values were still significantly lower than at baseline. In turn, bioelectrical values were found to be significantly lower compared with PRE values, also identified by BIVA (Figures 1B).
A positive relationship was found between racing time and basal R/h (r = 0.68; p = 0.04) and Z/h (r = 0.68; p = 0.045). Besides, basal R/h and Z/h were highly and positively related to PRE-to-POST bioelectrical changes of R/h and Z/h (r = 0.8; p = 0.009). PRE-to-POST bioelectrical changes of R/h and Z/h were also highly and positively related to racing time (r = 0.8, p = 0.01) and TRIMP (r = 0.8, p ≤ 0.02). Finally, no statistically significant correlation was observed between bioelectrical changes in relation to BM. Furthermore, no statistically significant correlation was observed between BM changes in the different time points and racing time, internal workload and energy deficit (ranges: r = - 0.46 to 0.65; p = 0.06 to 0.98).
On the other hand, multiple linear regression analysis revealed that an increase in R/h and Z/h after the race was explained by a larger decrease in BM, greater TRIMP, and a slower racing time and (rm2adj = 0.88) (Table 2). On the other hand, the racing time was found to be moderately explained by an increase in Z/h at POST (rm2adj = 0.58)
Table 2.
Multiple linear regression analysis of bioelectrical, anthropometric and performance parameters before (PRE) and after the race (POST).
| Dependent Variables | Explanatory equations | rm2 | ANOVA | SEE | ||||
|---|---|---|---|---|---|---|---|---|
| Exact | Adjusted | F | df1 | df2 | p | |||
| R/hPRE-POST (Δ%) | -28.40 - (1.14 · BMPRE-POST) + (0.021 · time) + (0.010 · TRIMP) |
0.92 | 0.88 | 19.95 | 3 | 5 | 0.003 | 0.80 |
| Z/hPRE-POST (Δ%) | -28.62 - (1.17 · BMPRE-POST) + (0.022 · time) + (0.010 · TRIMP) |
0.93 | 0.88 | 29.42 | 3 | 5 | 0.003 | 0.79 |
| Racing time (min) | 660.3 + (24.4 · Z/hPRE-POST) | 0.63 | 0.58 | 11.914 | 1 | 7 | 0.01 | 45.7 |
Fin (p ≤ 0.05), Fout (p ≥ 0.10). R, resistance; Z, impedance module; h, body height; BM, body mass; TRIMP, training impulse; time, racing time; rm2, multiple regression coefficient squared; SEE, standard error of estimation.
Discussion
Bioelectrical patterns in the ultra-endurance triathletes
When triathletes were compared to the healthy reference population, individual vectors were scattered mostly outside the 50% tolerance ellipse, positioned to the left of the major axis (Figure 1A). According to the urine color analysis, participants arrived to PRE in euhydration state. However, only two of them were plotted inside the 50% tolerance ellipse (Figure 1A). Since similar findings have already been observed in other sport samples (Campa and Toselli, 2018; Carrasco-Marginet et al., 2017; Gatterer et al., 2014; Giorgi et al., 2018; Koury et al., 2014; Micheli et al., 2014), this could reflect the specific body composition of athletes, characterized by greater soft tissue mass and different fluid content (Andreoli et al., 2001). Furthermore, the greater PA of the triathletes observed in this study (Figure 2) could indicate better cell function (Norman et al., 2012) and differing fluid distribution (i.e., increased intracellular water content) (Chertow et al., 1995), likely due to the hypertrophy of muscle fibers (Micheli et al., 2014). On the other hand, a significantly positive relationship was found between basal R/h (and therefore, Z/h) and racing time in the triathletes. This implies that the vector of triathletes who had better performance in the race (and, presumably, higher performance levels pre-race) would be displaced to the left, due to lower R/h values. Accordingly, it was observed that triathletes who registered lower basal R/h (and Z/h), racing time and internal workload showed smaller changes in these parameters after the race, experiencing lower decreases of body fluids. Vectors shifted to the left have been already reported with performance level in different sport samples (Carrasco-Marginet et al., 2017; Giorgi et al., 2018; Micheli et al., 2014), probably as a result of the specific training process. This particularly relevant finding highlights the need of further research regarding this matter, since the application of a non-invasive technique could eventually help to discriminate between performance levels of athletes according to the position of their vectors.
BM and bioelectrical changes evoked by UET
Regarding the changes induced by UET, the event evoked a mild-to-moderate dehydration, according to the average BM loss of ~5% (McDermott et al., 2017). Furthermore, individual vectors’ migration along the major axis was observed due to an increase in R and Xc (Figure 1A), which is consistent with fluid loss according to the literature. To our knowledge, only three studies have applied BIVA to analyze short-term vector changes induced by exercise. The articles revealed similar findings to those of the present study, reporting increased R and Xc after exercise, as well as a vector migration (Carrasco-Marginet et al., 2017; Gatterer et al., 2014, Heavens et al., 2016).
Since R is the opposition of the conductor to the flow of current, a significant increase in these values would indicate a decrease in body fluids (O’Brien et al., 2002), which was supported by the significant decrease in BM.
With regard to reactance, the increased Xc after exercise has been suggested as an indicator of fluid shifts between intra- and extracellular compartments (Gatterer et al., 2014). Nevertheless, the meaning of Xc after performing exercise remains to be clarified. As mentioned in Castizo-Olier et al. (2018), multiple factors may affect Xc values (e.g. size, thickness, composition and distance between cell membranes; fluid distribution and characteristic frequency variations; ...) and further research should focus on this parameter in the exercise context.
In relation to the vector analysis, however, it is important to highlight that although directional changes in vector values from serial measurements seem consistent with fluid loss, BIVA is not currently able to identify type and magnitude of fluid loss. This is probably because the range of “normal hydration” comprised by the ellipses is wider than a hydration status/change considered as “dehydration” through other methodologies (Heavens et al., 2016). As mentioned in Heavens et al. (2016), the analysis of the vector length could be the key for serial measurements of hydration status.
On the other hand, although significant differences were found after the race, no correlation was observed between changes in BM and BIA variations in any situation. The lack of correlation found PRE-to-POST has been also depicted in Gatterer et al. (2014) and Carrasco-Marginet et al. (2017). The authors related the absence of correlation with a decrease in BM without an effective net negative fluid balance as a result of exercise-related factors such as sweat rate, respiratory water loss and oxidative water production (Maughan et al., 2007).
The multiple regression analysis allows the study of the bioelectrical vector’s behavior from a multifactorial perspective. Thus, while BM does not correlate with bioelectrical parameters as an isolated variable, it is selected as an explanatory factor in the multivariate model (Table 2). When the bioelectrical parameters were analyzed as dependent variables, the changes observed in R/h and Z/h after the race were significantly explained by the behavior of BM, the racing time and the estimated internal workload, which makes sense. When the process was further applied in reverse in order to add information to the multivariate analysis, alternating the role between dependent and independent variables, the racing time was significantly explained by the behavior of Z/h from PRE-to-POST. In the event that, in the future, this methodology could be validated, it could be a possible indicator of the training/competition load. In addition, using the multivariate analysis, some variables (e.g., race time) could be estimated analyzing the behavior of other parameters, with a certain degree of error. Therefore, this type of analysis should be taken into consideration both in the interpretation of certain variables related to vector behavior and in future studies about this topic. However, the limited sample analyzed in the present study forces us to be cautious in drawing robust conclusions.
In relation with PRE-to-POST48h changes, the individual vectors’ migration along the major axis due to significant decreases in R and Xc (Figure 1B) indicates fluid accumulation (Lukaski and Piccoli, 2012), while BM values were still significantly lower than at baseline. Triathletes followed individual uncontrolled POST-to-POST48h recovery strategies (nutrition, hydration, physical activity, environmental conditions, etc.). However, the other mentioned factors that could affect the accuracy and reliability of BM and BIA measurements were controlled, being PRE and POST48h on equal terms. Thus, while BM alone does not detect a return to basal conditions, significant bioelectrical decreases below basal values were observed, indicating fluid retention in comparison with PRE. This highlights the potential advantage of BIVA in providing additional information about hydration changes in comparison with BM alone. However, it is important to clarify that neither BM nor BIVA can really identify what happened to TBW. As already mentioned, BIVA reflects changes in ECW estimates only. Thus, ICW may still be reduced (captured by BM at this time point) with a migration of fluids to the ECW space.
Fluid retention has been already reported in ultra-endurance events (Knechtle et al., 2008a; Knechtle et al., 2008b; Knechtle et al., 2009). As explained by Knechtle et al. (2009), although the reasons and mechanisms for the fluid increase are still unknown, it could be due to several factors. One explanation for this fluid retention could be an increase in plasma volume due to a higher activity of aldosterone and antidiuretic hormone (Neumayr et al., 2005). Moreover, protein catabolism with consequent fluid shifts (hypoproteinemic edema) might occur in an ultra-endurance effort (Lehmann et al., 1995). Another possible factor for the observed fluid expansion could be the increased plasma protein concentration inducing an increase in plasma oncotic pressure (Maughan et al., 1985; Mischler et al., 2003). On the other hand, the increase of body fluids could also be a result of the impairment of renal function due to the rhabdomyolysis that may occur in ultra-endurance events (Kim et al., 2007; Skenderi et al., 2006; Uberoi et al., 1991), although in general, acute renal failure in an ultra-endurance event is very rare (MacSearraigh et al., 1979). Finally, regarding the putative factors explaining the fluid increase 48 hours after the race, the already mentioned individual uncontrolled POST-to-POST48h recovery strategies may have affected these findings. Therefore, the identification of fluid retention after ultra-endurance events through BIVA should be further studied together with tests investigating the aforementioned mechanisms, in order to analyze possible associations.
Regarding the behavior of Xc from PRE-to-POST48h, the decreased values could indicate a reduction in soft tissues, since Xc is proposed as an indicator of dielectric mass (membranes and tissue interfaces) in soft tissues (Lukaski, 1996). As already mentioned, there is evidence of muscle damage after prolonged exercise. Significant modifications in markers of muscle damage and inflammation two days after the end of the event have been reported (Carmona et al., 2015; Millet et al., 2011; Overgaard et al., 2002). Further studies should investigate the relationship between the behavior of Xc and muscle damage biomarkers after completing this type of events. It would be interesting to analyze the validity of this parameter (obtained from a minimally invasive method) in order to control the muscle disruption recovery after exercise. Nevertheless, taking into account the aforementioned limitation of not controlling individual recovery strategies, it is difficult at present to elucidate the reasons why this behavior occurs due to the already mentioned problems in the interpretation of Xc when the fluid distribution changes.
Limitations of the study
In protocols measuring acute vector changes (before and after exercise), some factors should be controlled due to their influence in the bioelectrical signal in order to avoid measurement errors and provide accurate and reliable results (Castizo-Olier et al., 2018). The present study attempted to control all these factors. Nevertheless, in order to respect an ecological design and due to the characteristics of the sport event, the free consumption of food and beverage was allowed. The ingestion of food or beverages has an influence on Z, which may decrease over a 2- to 4-h period after a meal, generally representing a change of < 3% in Z values (Kushner et al., 1996). The ultra-endurance triathlon race started at 6:00 a.m. and lasted for many hours (~12.5 h on average). Therefore, each participant had her/his own nutritional strategies before competition (e.g., usually they have breakfast 2-3 hours before the race), which we could not control. This could have influence the bioelectrical values obtained pre-race. Furthermore, due to the free consumption of food and beverage during the race, an underestimation of ~14 Ω in Z values could have occurred in the post-exercise bioelectrical measurements. However, the amount of water intake at the end of the race should not have affected these measurements because the recent ingestion of a meal or beverage (< 1 h from the ingestion to bioelectrical measurements) appears to be “electrically silent” and to have a minimal effect on whole-body Z (Evans et al., 1998).
The ecological design of the study itself implied also certain limitations. The post-race measurement was notably the most difficult assessment because of the multiple factors that must be controlled due to their influence on the bioelectrical signal at a moment in which athletes are extremely tired and less motivated (after exercising for more than 12 h). Moreover, the time at which the fluid/food intakes were performed during the race was not registered. On the other hand, there were no records of each individual’s recovery strategies. Although the sample size was previously estimated (see Participants) and post-tests power calculation was within the expected values, underpowered sample size cannot be completely discarded, which limit the possibility of reaching stronger inferences, especially in the multiple regression models. Finally, no specific triathlon tolerance ellipses exist yet to allow a more enriching analysis.
Conclusion
A specific bioelectrical distribution was found in the present group of triathletes in comparison with the healthy, general reference population. This justifies the need to create specific tolerance ellipses that could discriminate triathletes of different performance level, age, sex, race, etc. Furthermore, the relationship between basal vector position of triathletes and performance variables should be further investigated, since it could help to discriminate between performance levels of athletes according to the position of their vectors. Although BIVA is not currently able to identify type and magnitude of fluid loss, vector migration appears to be consistent with fluid loss induced by a UET event. Furthermore, reversed vector displacement beyond the basal position 48 h after the race is consistent with fluids recovery, while BM did not return to PRE values. This highlights the potential advantage of BIVA in better informing about hydration changes in comparison with BM alone. Furthermore, the bioelectrical analysis seems to be consistent to muscle disruption in the recovery period after completing this type of events. Although with the utmost caution, there seems to be a relationship between the behavior of the bioelectrical vector and certain performance parameters. The multivariate analysis may help to better understand the bioelectrical vector’s behavior pre- to post-exercise. BIVA may be helpful in assessing hydration changes in real time and could also complement the current hydration biomarkers that require a mobile laboratory. Nonetheless, further research must investigate the applicability of BIVA as a valid and reliable biomarker of hydration status, especially regarding the behavior of Xc after exercise.
Acknowledgements
This work was supported by the Government of Catalonia, Agency for Management of University and Research Grants (AGAUR) under Grant 2015 FI_B 00217. The study was conducted with the support of the National Institute of Physical Education of Catalonia (INEFC), Government of Catalonia. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript. The authors have no conflicts of interest to declare. All experiments comply with the current laws of the country.
Biographies
Jorge CASTIZO-OLIER
Employment
INEFC-Barcelona Sport Sciences Research Group, Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
BSc, MSc, PhD candidate
Research interests
Body composition, bioimpedance, sports and exercise physiology
E-mail: j.castizo9@gmail.com
Marta CARRASCO-MARGINET
Employment
INEFC-Barcelona Sport Sciences Research Group, Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
BSc, MSc, PhD
Research interests
Dietetics and sports nutrition
E-mail: martacm8@gmail.com
Alex ROY
Employment
Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
BSc, MSc, PhD candidate
Research interests
Triathlon, trail running, aquatic, cyclic and intermittent sports physiology, bioimpedance
E-mail: alex.roy.torner@gmail.com
Diego CHAVERRI
Employment
INEFC-Barcelona Sport Sciences Research Group, Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
BSc, MSc, PhD
Research interests
Swimming, cycling and triathlon physiology and bioenergetics
E-mail: chaverri.diego@gmail.com
Xavier IGLESIAS
Employment
Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
BSc, PhD
Research interests
Fencing, bioenergetics and observational methodology in the field of sport
E-mail: xiglesias@gmail.com
Carla PÉREZ-CHIRINOS
Employment
Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
BSc, MSc, PhD candidate
Research interests
Bioimpedance, body composition, muscle injuries
E-mail: carla.perez.chirinos@gmail.com
Ferran A. RODRÍGUEZ
Employment
INEFC-Barcelona Sport Sciences Research Group, Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
MD, PhD
Research interests
Aquatic, cyclic and intermittent sports physiology and bioenergetics, environmental physiology and medicine
E-mail: farodriguez@gencat.cat
Alfredo IRURTIA
Employment
INEFC-Barcelona Sport Sciences Research Group, Institut Nacional d’Educació Física de Catalunya (INEFC), Universitat de Barcelona (UB), Barcelona, Spain
Degree
BSc, PhD
Research interests
Gymnastics, body composition, sports and exercise physiology
E-mail: airurtia@gencat.cat
References
- Andreoli A., Monteleone M., Van Loan M., Promenzio L., Tarantino U., De Lorenzo A. (2001) Effects of different sports on bone density and muscle mass in highly trained athletes. Medicine and Science in Sports and Exercise 33, 507-511. [DOI] [PubMed] [Google Scholar]
- Armstrong L.E. (2007) Assessing hydration status: the elusive gold standard. Journal of the American College of Nutrition 26, 575S-584S. [DOI] [PubMed] [Google Scholar]
- Armstrong L.E., Maresh C.M., Castellani J.W., Bergeron M.F., Kenefick R.W., LaGasse K.E., Riebe D. (1994) Urinary indices of hydration status. International Journal of Sport Nutrition 4, 265-279. [DOI] [PubMed] [Google Scholar]
- Barrero A., Erola P., Bescós R. (2014) Energy balance of triathletes during an ultra-endurance event. Nutrients 7, 209-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campa F., Toselli S. (2018) Bioimpedance Vector Analysis of Élite, Sub-Élite and Low-Level Male Volleyball Players. International Journal of Sports Physiology and Performance 1-13. [DOI] [PubMed] [Google Scholar]
- Carmona G., Roca E., Guerrero M., Cussó R., Irurtia A., Nescolarde L., Brotons D., Bedini J.L., Cadefau J.A. (2015) Sarcomere disruptions of slow fiber resulting from mountain ultramarathon. International Journal of Sports Physiology and Performance 10, 1041-1047. [DOI] [PubMed] [Google Scholar]
- Carrasco-Marginet M., Castizo-Olier J., Rodríguez-Zamora L., Iglesias X., Rodríguez F. A., Chaverri D., Brotons D., Irurtia A. (2017) Bioelectrical impedance vector analysis (BIVA) for measuring the hydration status in young elite synchronized swimmers. PLoS One 12, e0178819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castizo-Olier J., Irurtia A., Jemni M., Carrasco-Marginet M., Fernández-García R., Rodríguez F.A. (2018) Bioelectrical impedance vector analysis (BIVA) in sport and exercise: systematic review and future perspectives. PLoS One, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caton J.R., Mole P.A., Adams W.C., Heustis D.S. (1988) Body composition analysis by bioelectrical impedance: effect of skin temperature. Medicine and Science in Sports and Exercise 20, 489-491. [PubMed] [Google Scholar]
- Chertow G.M., Lowrie E.G., Wilmore D.W., Gonzalez J., Lew N.L., Ling J., Leboff M.S., Gottlieb M.N., Huang W., Zebrowski B. (1995) Nutritional assessment with bioelectrical impedance analysis in maintenance hemodialysis patients. Journal of the American Society of Nephrology 6, 75-81. [DOI] [PubMed] [Google Scholar]
- Cheuvront S.N., Kenefick R.W. (2014) Dehydration: physiology, assessment, and performance effects. Comprehensive Physiology 4, 257-285. [DOI] [PubMed] [Google Scholar]
- Cheuvront S.N., Kenefick R.W. (2017) CORP: Improving the status quo for measuring whole body sweat losses. Journal of Applied Physiology 123, 632-636. [DOI] [PubMed] [Google Scholar]
- Codognotto M., Piazza M., Frigatti P., Piccoli A. (2008) Influence of localized edema on whole-body and segmental bioelectrical impedance. Nutrition 24, 569-574. [DOI] [PubMed] [Google Scholar]
- De Lorenzo A., Andreoli A., Matthie J., Withers P. (1997) Predicting body cell mass with bioimpedance by using theoretical methods: a technological review. Journal of Applied Physiology 82, 1542-1558. [DOI] [PubMed] [Google Scholar]
- Evans W., McClagish H., Trudgett C. (1998) Factors affecting the in vivo precision of bioelectrical impedance analysis. Applied Radiation and Isotopes 49, 485-487. [DOI] [PubMed] [Google Scholar]
- Gatterer H., Schenk K., Laninschegg L., Schlemmer P., Lukaski H., Burtscher M. (2014) Bioimpedance identifies body fluid loss after exercise in the heat: a pilot study with body cooling. PLoS One 9, e109729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giorgi A., Vicini M., Pollastri L., Lombardi E., Magni E., Andreazzoli A., Orsini M., Bonifazi M., Lukaski H., Gatterer H. (2018) Bioimpedance patterns and bioelectrical impedance vector analysis (BIVA) of road cyclists. Journal of Sports Sciences 1-6. [DOI] [PubMed] [Google Scholar]
- Goovaerts H., Faes T.J., De Valk-De Roo G., Ten Bolscher M., Netelenbosch J., Van der Vijgh W., Heethaar R. (1998) Extra-cellular volume estimation by electrical impedance-phase measurement or curve fitting: a comparative study. Physiological Measurement 19, 517. [DOI] [PubMed] [Google Scholar]
- Gualdi-Russo E., Toselli S. (2002) Influence of various factors on the measurement of multifrequency bioimpedance. Homo 53, 1-16. [DOI] [PubMed] [Google Scholar]
- Heavens K.R., Charkoudian N., O’Brien C., Kenefick R.W., Cheuvront S.N. (2016) Noninvasive assessment of extracellular and intracellular dehydration in healthy humans using the resistance-reactance–score graph method. The American Journal of Clinical Nutrition 103, 724-729. [DOI] [PubMed] [Google Scholar]
- Hermens H. J., Freriks B., Merletti R., Stegeman D., Blok J., Rau G., Disselhorst-Klug C., Hägg G. (1999) European recommendations for surface electromyography. Roessingh Research and Development 8, 13-54. [Google Scholar]
- Hew-Butler T., Collins M., Bosch A., Sharwood K., Wilson G., Armstrong M., Jennings C., Swart J., Noakes T. (2007) Maintenance of plasma volume and serum sodium concentration despite body weight loss in ironman triathletes. Clinical Journal of Sport Medicine 17, 116-122. [DOI] [PubMed] [Google Scholar]
- Jeukendrup A.E., Jentjens R. L., Moseley L. (2005) Nutritional considerations in triathlon. Sports Medicine 35, 163-181. [DOI] [PubMed] [Google Scholar]
- Kim H.J., Lee Y.H., Kim C.K. (2007) Biomarkers of muscle and cartilage damage and inflammation during a 200 km run. European Journal of Applied Physiology 99, 443-447. [DOI] [PubMed] [Google Scholar]
- Knechtle B., Duff B., Schulze I., Kohler G. (2008a) A multi-stage ultra-endurance run over 1,200 km leads to a continuous accumulation of total body water. Journal of Sports Science and Medicine 7, 357.24149903 [Google Scholar]
- Knechtle B., Fraire O.S., Andonie J., Kohler G. (2008b) Effect of a multistage ultra-endurance triathlon on body composition: World Challenge Deca Iron Triathlon 2006. British Journal of Sports Medicine 42, 121-125. [DOI] [PubMed] [Google Scholar]
- Knechtle B., Wirth A., Knechtle P., Rosemann T. (2009) Increase of total body water with decrease of body mass while running 100 km nonstop—formation of edema? Research Quarterly for Exercise and Sport 80, 593-603. [DOI] [PubMed] [Google Scholar]
- Knechtle B., Zingg M.A., Rosemann T., Stiefel M., Rüst C.A. (2015) What predicts performance in ultra-triathlon races?–a comparison between Ironman distance triathlon and ultra-triathlon. Open Access Journal of Sports Medicine 6, 149-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koury J., Trugo N., Torres A. (2014) Phase angle and bioelectrical impedance vectors in adolescent and adult male athletes. International Journal of Sports Physiology and Performance 9, 798-804. [DOI] [PubMed] [Google Scholar]
- Kushner R., Gudivaka R., Schoeller D. (1996) Clinical characteristics influencing bioelectrical impedance analysis measurements. The American Journal of Clinical Nutrition 64, 423S-427S.8780358 [Google Scholar]
- Laursen P.B., Rhodes E.C. (2001) Factors affecting performance in an ultraendurance triathlon. Sports Medine 31, 195-209. [DOI] [PubMed] [Google Scholar]
- Laursen P.B., Suriano R., Quod M.J., Lee H., Abbiss C.R., Nosaka K., Martin D.T., Bishop D. (2006) Core temperature and hydration status during an Ironman triathlon. British Journal of Sports Medicine 40, 320-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann M., Huonker M., Dimeo F., Heinz N., Gastmann U., Treis N., Steinacker J., Keul J., Kajewski R., Häussinger D. (1995) Serum amino acid concentrations in nine athletes before and after the 1993 Colmar ultra triathlon. International Journal of Sports Medicine 16, 155-159. [DOI] [PubMed] [Google Scholar]
- Liang M.T., Norris S. (1993) Effects of skin blood flow and temperature on bioelectric impedance after exercise. Medicine and Science in Sports and Exercise 25, 1231-1239. [PubMed] [Google Scholar]
- Lukaski H.C. (1996) Biological indexes considered in the derivation of the bioelectrical impedance analysis. The American Journal of Clinical Nutrition 64, 397S-404S.8780355 [Google Scholar]
- Lukaski H.C. (2013) Evolution of bioimpedance: a circuitous journey from estimation of physiological function to assessment of body composition and a return to clinical research. European Journal of Clinical Nutrition 67, S2. [DOI] [PubMed] [Google Scholar]
- Lukaski H.C., Piccoli A. (2012) Bioelectrical impedance vector analysis for assessment of hydration in physiological states and clinical conditions. In: Handbook of Anthropometry. Ed; Preedy V. London: Springer; 287-305. [Google Scholar]
- MacSearraigh E.T., Kallmeyer J.C., Schiff H.B. (1979) Acute renal failure in marathon runners. Nephron 24, 236-240. [DOI] [PubMed] [Google Scholar]
- Matthie J., Withers P. (1995) The ambiguities of predicting total body water and body cell mass with a single frequency (50KHz) measurement of bioimpedance. Journal of the American Society of Nephrology 6, 1682-1685. [PubMed] [Google Scholar]
- Maughan R., Whiting P., Davidson R. (1985) Estimation of plasma volume changes during marathon running. British Journal of Sports Medicine 19, 138-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan R.J., Shirreffs S.M., Leiper J.B. (2007) Errors in the estimation of hydration status from changes in body mass. Journal of Sports Sciences 25, 797-804. [DOI] [PubMed] [Google Scholar]
- McDermott B.P., Anderson S.A., Armstrong L.E., Casa D.J., Cheuvront S.N., Cooper L., Kenney W.L., O’Connor F.G., Roberts W.O. (2017) National Athletic Trainers’ Association Position Statement: Fluid Replacement for the Physically Active. Journal of Athletic Training 52, 877-895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarvey J., Thompson J., Hanna C., Noakes T. D., Stewart J., Speedy D. (2010) Sensitivity and specificity of clinical signs for assessment of dehydration in endurance athletes. British Journal of Sports Medicine 44, 716–719. [DOI] [PubMed] [Google Scholar]
- Micheli M.L., Pagani L., Marella M., Gulisano M., Piccoli A., Angelini F., Burtscher M., Gatterer H. (2014) Bioimpedance and Impedance Vector Patterns as Predictors of League Level in Male Soccer Players. International Journal of Sports Physiology and Performance 9, 532-539. [DOI] [PubMed] [Google Scholar]
- Millet G.Y., Tomazin K., Verges S., Vincent C., Bonnefoy R., Boisson R.-C., Gergelé L., Féasson L., Martin V. (2011) Neuromuscular consequences of an extreme mountain ultra-marathon. PLoS One 6, e17059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mischler I., Boirie Y., Gachon P., Pialoux V., Mounier R., Rousset P., Coudert J., Fellmann N. (2003) Human albumin synthesis is increased by an ultra-endurance trial. Medicine and Science in Sports and Exercise 35, 75-81. [DOI] [PubMed] [Google Scholar]
- Moreno M.V., Ribbe-Cornet E., Rebeyrol J., Vannicatte A., Krief L. (2015) Evaluation of a new impedancemeter to independently measure extracellular, intracellular and total body water volumes: application to the measurement of hydration. Medical and Biological Engineering and Computing 53, 989-999. [DOI] [PubMed] [Google Scholar]
- Neumayr G., Pfister R., Hoertnagl H., Mitterbauer G., Prokop W., Joannidis M. (2005) Renal function and plasma volume following ultramarathon cycling. International Journal of Sports Medicine 26, 2-8. [DOI] [PubMed] [Google Scholar]
- Norman K., Stobäus N., Pirlich M., Bosy-Westphal A. (2012) Bioelectrical phase angle and impedance vector analysis - Clinical relevance and applicability of impedance parameters. Clinical Nutrition 31, 854-861. [DOI] [PubMed] [Google Scholar]
- O’Brien C., Young A., Sawka M. (2002) Bioelectrical impedance to estimate changes in hydration status. International Journal of Sports Medicine 23, 361-366. [DOI] [PubMed] [Google Scholar]
- Oppliger R.A., Bartok C. (2002) Hydration testing of athletes. Sports Medicine 32, 959-971. [DOI] [PubMed] [Google Scholar]
- Overgaard K., Lindstrøm T., Ingemann-Hansen T., Clausen T. (2002) Membrane leakage and increased content of Na+-K+ pumps and Ca2+ in human muscle after a 100-km run. Journal of Applied Physiology 92, 1891-1898. [DOI] [PubMed] [Google Scholar]
- Peiffer J.J., Abbiss C.R., Nosaka K., Peake J.M., Laursen P.B. (2009) Effect of cold water immersion after exercise in the heat on muscle function, body temperatures, and vessel diameter. Journal of Science and Medicine in Sport 12, 91-96. [DOI] [PubMed] [Google Scholar]
- Piccoli A. (2005) Whole body-single frequency bioimpedance. Contributions to Nephrology 149, 150-161. [DOI] [PubMed] [Google Scholar]
- Piccoli A. (2010) Bioelectric impedance measurement for fluid status assessment. Contributions to Nephrology 164, 143-152. [DOI] [PubMed] [Google Scholar]
- Piccoli A., Nigrelli S., Caberlotto A., Bottazzo S., Rossi B., Pillon L., Maggiore Q. (1995) Bivariate normal values of the bioelectrical impedance vector in adult and elderly populations. The American Journal of Clinical Nutrition 61, 269-270. [DOI] [PubMed] [Google Scholar]
- Piccoli A., Pillon L., Dumler F. (2002). Impedance vector distribution by sex, race, body mass index, and age in the United States: standard reference intervals as bivariate Z scores. Nutrition 18, 153-167. [DOI] [PubMed] [Google Scholar]
- Piccoli A., Rossi B., Pillon L., Bucciante G. (1994) A new method for monitoring body fluid variation by bioimpedance analysis: the RXc graph. Kidney International 46, 534-539. [DOI] [PubMed] [Google Scholar]
- Rush E.C., Crowley J., Freitas I.F., Amy L. (2006) Validity of hand-to-foot measurement of bioimpedance: standing compared with lying position. Obesity 14, 252-57. [DOI] [PubMed] [Google Scholar]
- Segal K.R., Burastero S., Chun A., Coronel P., Pierson R.N., Jr, Wang J. (1991) Estimation of extracellular and total body water by multiple-frequency bioelectrical-impedance measurement. The American Journal of Clinical Nutrition 54, 26-29. [DOI] [PubMed] [Google Scholar]
- Sharwood K., Collins M., Goedecke J., Wilson G., Noakes T. (2004) Weight changes, medical complications, and performance during an Ironman triathlon. British Journal of Sports Medicine 38, 718-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skenderi K.P., Kavouras S.A., Anastasiou C.A., Yiannakouris N., Matalas A. (2006) Exertional rhabdomyolysis during a 246-km continuous running race. Medicine and Science in Sports and Exercise 38, 1054-1057. [DOI] [PubMed] [Google Scholar]
- Slinde F., Bark A., Jansson J., Rossander-Hulthén L. (2003) Bioelectrical impedance variation in healthy subjects during 12 h in the supine position. Clinical Nutrition 22, 153-157. [DOI] [PubMed] [Google Scholar]
- Stewart A., Marfell-Jones M., Olds T., de Ridder H. (2011) International standards for anthropometric assessment. Portsmouth: International Society for the Advancement of Kinanthropometry. [Google Scholar]
- Uberoi H., Dugal J., Kasthuri A., Kolhe V., Kumar A., Cruz S. (1991) Acute renal failure in severe exertional rhabdomyolysis. The Journal of the Association of Physicians of India 39, 677-679. [PubMed] [Google Scholar]
- Yanovski S.Z., Hubbard V.S., Heymsfield S.B., Lukaski H.C. (1996) Bioelectrical impedance analysis in body composition measurement: National institutes of health technology assessment conference statement. The American Journal of Clinical Nutrition 64, 524S-532S. [DOI] [PubMed] [Google Scholar]


