Abstract
Gastrointestinal bleeding in HIV patients secondary to coinfection by HHV8 and development of Kaposi's sarcoma (KS) is a rare complication even if no skin lesions are detected on physical examination. This article indicates which patients might develop this type of clinical sign and also tries to recall that absence of skin lesions never rules out the presence of KS, especially if gastrointestinal involvement is documented. Gastrointestinal bleeding in terms of hematemesis has rarely been reported in the literature. We review some important clinical findings, diagnosis, and treatment approach. We present the case of an HIV patient who presented to the emergency department with hematemesis and gastrointestinal signs of KS on upper gastrointestinal endoscopy without any dermatological involvement.
Keywords: Kaposi's sarcoma, Gastrointestinal bleeding, Human immunodeficiency virus
Clinical Case
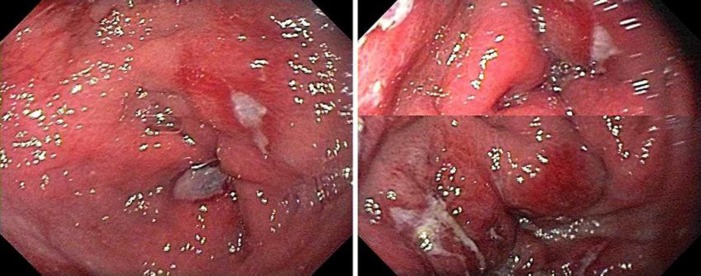
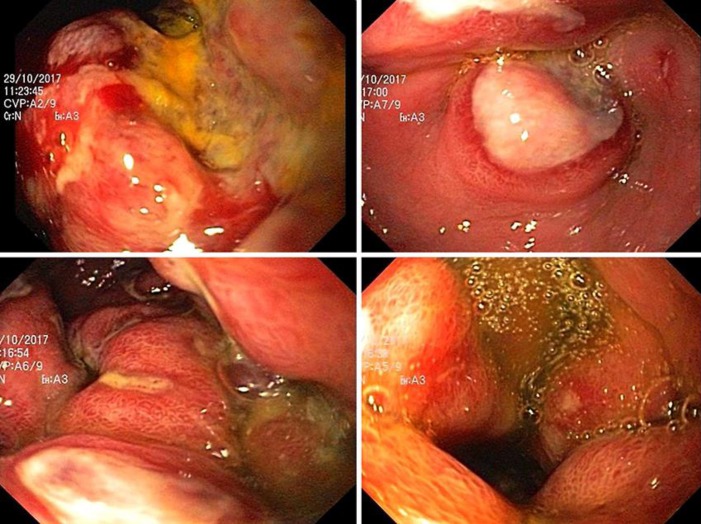
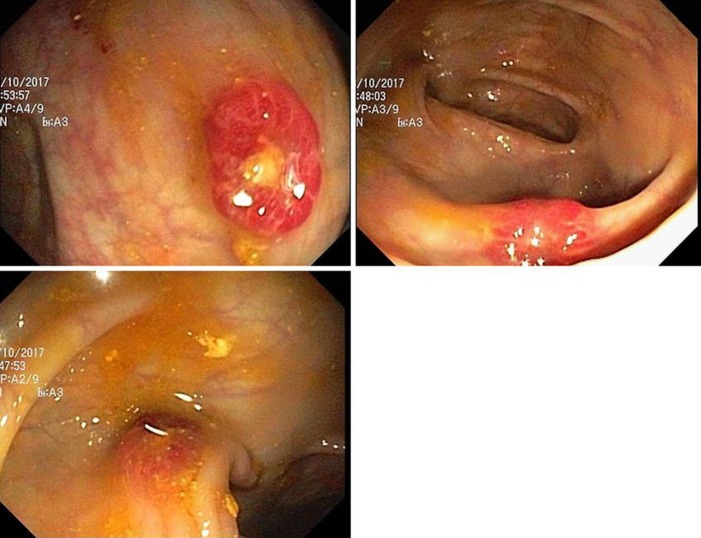
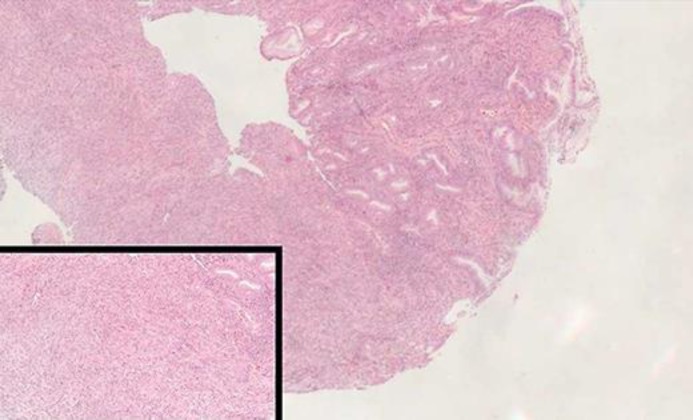
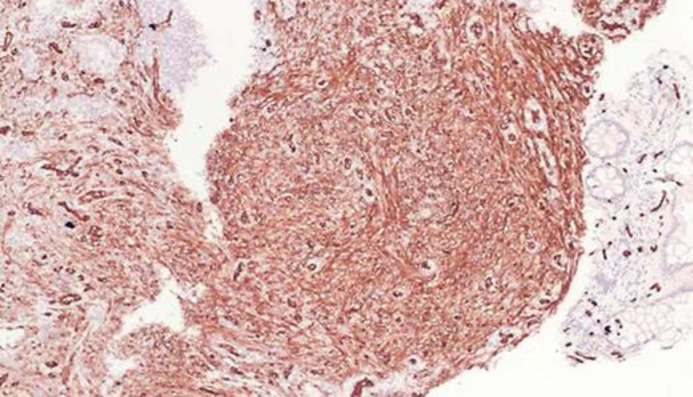
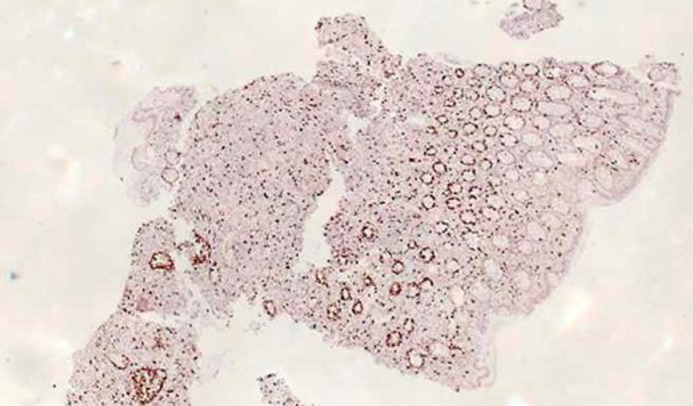
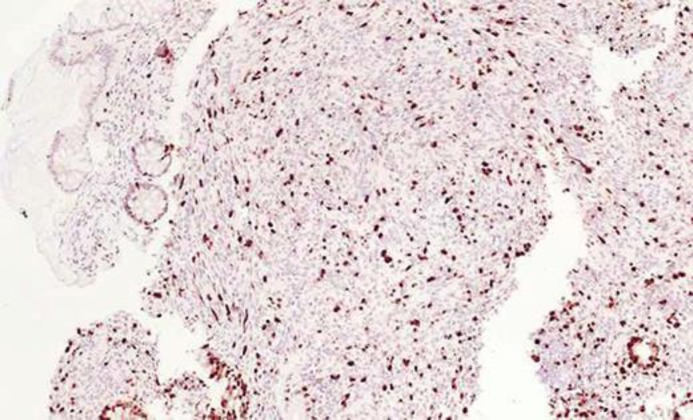
A 23-year-old human immunodeficiency virus (HIV)-positive male patient with a CD4 count of 64/mm3 and a viral load of 123,422 copies/mL was treated with efavirenz 600 mg and emtricitabine/tenofovir 200/300 mg daily. He was admitted to the emergency department due to epigastralgia, pyrosis, hematemesis, and dysphagia for solids lasting 15 days. No abnormalities were seen on vital signs, but signs of severe dehydration, whitish plaques on tongue surface and retro-auricular, submaxillary, and bilateral inguinal adenopathies were seen on physical examination. Initial workout showed normal blood chemistry without hydroelectrolytic imbalances, preserved renal function, and normal hepatic profile. Initial upper gastrointestinal endoscopy (UGE) (Fig. 1) showed multiple lesions at the antro-corporal level, ulcerated with a whitish halo compatible with gastroesophageal candidiasis. Anti-fungal treatment was started, with a slight improvement of symptoms described initially, so a new UGE was performed (Fig. 2). At this occasion, a subcardial lesion on the lesser curvature and several raised lesions of umbilicated appearance with a central ulcer covered with fibrin were found and extended on the minor curve, distally compromising the angular incisura. Considering initially malignancy due to appearance described with irregular high edges, a poorly defined ulcer covered with fibrin and, in the duodenum, elevated lesions of umbilical aspect with central depression of ulcer appearance covered with fibrin were also identified. Colonoscopy (Fig. 3) was performed due to UGE findings showing elevated umbilicated lesions of 15 mm on the left colon and transverse colon associated with signs of obstruction in the hepatic angle. Biopsies were taken from gastric lesions and reported: spindle tumor cells of endothelial origin compromising mucosa and submucosa layers that subsequently formed irregularity of vasculature lumen and a random pattern with blood extravasation and hyaline globules (Fig. 4, 5). Immunohistochemistry studies showed positivity for human herpes virus type 8 (HHV8) (Fig. 6, 7), CD34 (Fig. 8, 9), and an elevated cell proliferation index evidenced by the KI67 marker (Fig. 10, 11). CD117 was negative which allowed us to rule out gastrointestinal stromal tumor (GIST). Once histological and immunohistochemical results were obtained, the patient was started on anthracyclines without complications during treatment and with significant improvement of symptoms. Currently, the patient is under treatment with a second cycle of anthracyclines without any limiting toxicity.
Fig. 1.
Multiple lesions at the antro-corporal level, ulcerated with whitish halo, compatible with gastroesophageal candidiasis.
Fig. 2.
Subcardial lesion on the lesser curvature and several raised lesions of umbilicated appearance with central ulcer covered with fibrin.
Fig. 3.
Left colon elevated lesions of 15 mm with umbilicated center, transverse colon lesions of 15 mm with umbilicated center, and obstruction for the colonoscopy step in the hepatic angle.
Fig. 4.
Hematoxylin and eosin stain in a sample obtained from the antrum. ×10.
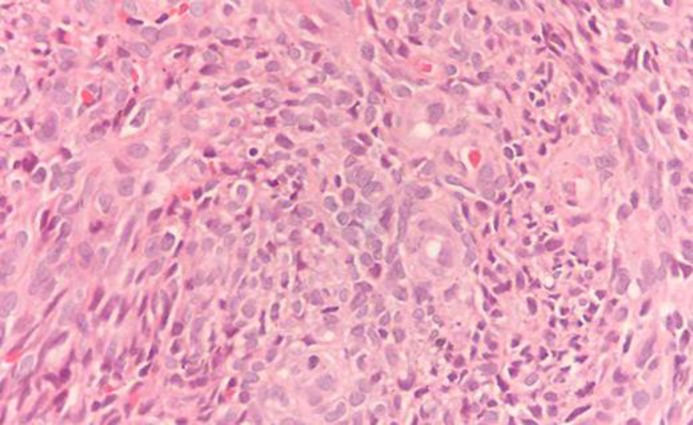
Fig. 5.
Hematoxylin and eosin stain in a sample obtained from the colon. ×40.
Fig. 6.
Tumor cells of the antrum with positive immunoreactivity for HHV8. ×10.
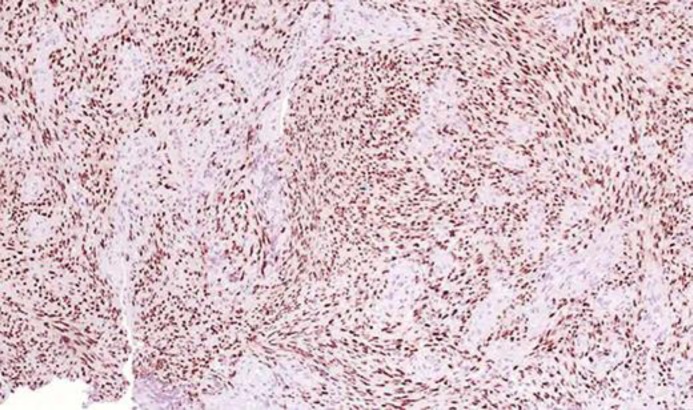
Fig. 7.
Tumor cells of the colon with positive immunoreactivity for HHV8. ×10.
Fig. 8.
CD34-positive marker in tumor cells of the antrum. ×10.
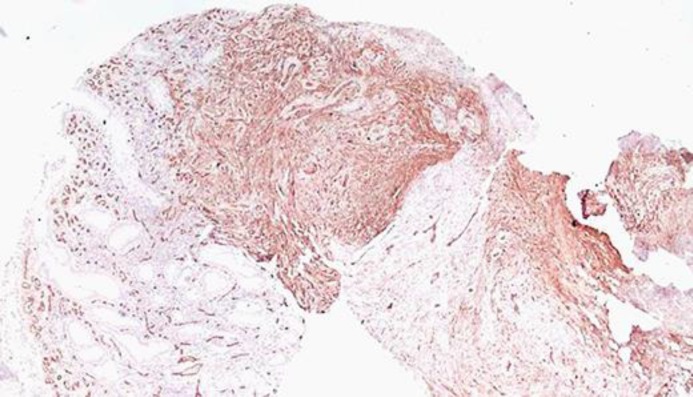
Fig. 9.
CD34-positive marker in colon tumor cells. ×10.
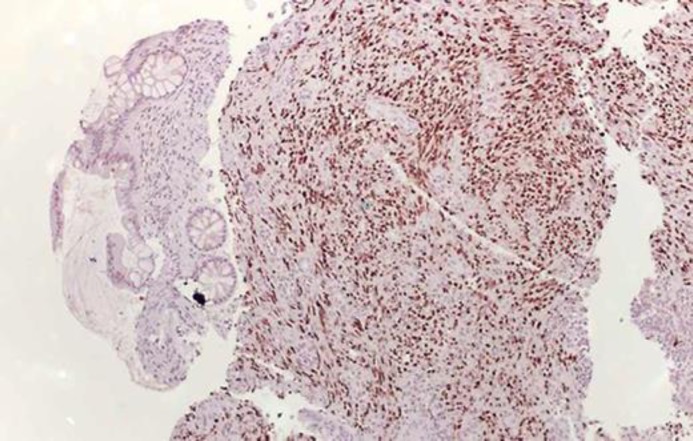
Fig. 10.
Ki67-positive marker in tumor cells located in the colon. ×4.
Fig. 11.
Ki67-positive marker in tumor cells located in the colon. ×10.
Discussion
In 1872, Kaposi's sarcoma (KS) was first seen and described in 5 patients. Dr. Moritz Kaposi described multiple pigmented sarcomas in the skin and gastrointestinal tract of unknown etiology, and one of the lesions in the gastrointestinal tract was associated with bleeding [1, 2]. From that time, it is known that this type of tumor is caused by HHV8 that initially affects the skin, but it can extend to mucous membranes and internal organs. Gastrointestinal KS is the neoplasia most commonly seen and frequent in patients with gastrointestinal neoplasia, occurring in about 40% in the series published [3]. At the beginning of the HIV epidemic, KS was one of the most frequent manifestations seen in immunocompromised patients in up to 50%. However, after the start of highly active antiretroviral therapy (ART), the incidence of this neoplasm decreased to less than 1% of the infected people with HIV [4, 5].
The most common manifestations of this neoplasm include the presence of erythematous, violaceous lesions that are well demarcated and can range from a flat plaque to nodular formation in skin surfaces [6]. Gastrointestinal involvement is less frequent; however, there are already several case reports showing that this tumor can affect any part of the gastrointestinal tract. KS grows from the submucosa, most of the time without any clinical symptoms as we documented in our patient. However, when symptoms develop, abdominal pain, nausea, vomiting, weight loss, gastrointestinal bleeding, intestinal obstruction, and diarrhea may occur, among other manifestations [7, 8]. Endoscopic findings of this type of lesion compromise the submucosa diffusely and with a random pattern, predominance id seen in the antrum and it has an appearance similar to the contoured polyps, with variability in their size that some authors described as target lesions [9].
An HIV patient with gastrointestinal bleeding and no documented skin manifestation as initial manifestation of KS has not been described in series of cases or in individual case reports. In an article published in 2013 by Mansfield et al. [10] and other case reports we reviewed which had symptoms commonly reported as a first manifestation of KS, we found that only 5 patients were HIV positive and only 3 had hematemesis as a first sign [11, 12, 13], and all of them had cutaneous involvement at presentation. Similarly, Carmo et al. [14] in a retrospective study of 9 years in Portugal, described 13 patients with gastrointestinal KS of which 11 were asymptomatic and only 2 had gastrointestinal bleeding (hematochezia). The striking feature of the paper mentioned above was the coinfection with HIV and skin lesions; however, a patient (HIV positive) was identified in their cohort who presented with digestive bleeding without skin lesions and a previous personal history of ulcerative colitis which was a confusing variable that did not allow to discriminate between bleeding from KS gastrointestinal involvement versus autoimmune activity due to a chronic inflammatory intestinal disease.
The diagnostic approach in patients with HIV and gastrointestinal symptoms includes that UGE is not recommended in all patients because it is an invasive and expensive test [15]. Additionally, as previously mentioned, the majority of patients with gastrointestinal KS are asymptomatic. For this reason, we have sought to determine the main risk factors that predict the presence of visceral involvement by KS in HIV-positive patients, finding that CD4 < 100 cells/mm3, viral load > 100,000 copies/mL, no previous use of highly active ART, sexual intercourse among men, and presence of skin lesions are clinical predictors of gastrointestinal involvement by KS [15]. Once patients with high risk are identified, upper gastrointestinal tract endoscopy (UGTE) and/or colonoscopy should be performed. Definitive diagnosis is made by immunohistochemistry, where it is sought to find fusiform cells with irregular vascular bundles in the submucosa layer, extravasation of red blood cells, macrophages with hemosiderin, and lymphoplasmacytic infiltration [1]. Additionally, identification of HHV8 is required by means of markers such as the HHV8 DNA reaching sensitivity and specificity of almost 99 to 100%, respectively. The use of other markers such as CD34 and CD117 is similarly useful; however, they are also positive in patients with GIST, so if they are performed they should always be accompanied by the identification of HHV8, otherwise differentiating GIST from KS is unlikely [16].
Treatment of KS with visceral involvement in patients with HIV differs from classical variables, African endemic, iatrogenic, or related to immunosuppression in terms of prognosis, response, administration form, etc. Pharmacological therapy of gastrointestinal involvement includes as first-line treatment the administration of liposomal doxorubicin, second line with paclitaxel [17], and finally the administration of interferon alpha [1]. In a retrospective study [18] that sought to evaluate the long-term prognosis of HIV-positive patients with KS treated with liposomal doxorubicin and of whom 20/98 had gastrointestinal compromise, a complete response to treatment was observed in 49%, partial response in 28%, and inadequate response in 14.5%. Regarding the risk of recurrence, of the 75 patients who completed this study, 65 attended follow-up after 50 months, of which 8 (13.5%/year) presented tumor relapse. The latter, in comparison with those that had a sustained response to management, had lower levels of CD4 and increase in them was lower compared to the group with an adequate response.
Conclusion
Heavy gastrointestinal bleeding as the first manifestation of KS in patients with HIV is rare and even more so when there are no cutaneous lesions. This is the most common gastrointestinal tumor that affects patients with HIV, and it is asymptomatic in the majority of cases. Even though ART has reduced its incidence, clinicians should know which are high-risk patients, when to screen for HHV8 infection to timely diagnose, treat, and avoid future complications due to scarce literature and few therapeutic options.
Availability of Data and Materials
All data generated or analyzed during this study are included in this published article.
Statement of Ethics
Written informed consent was obtained from the patient for the publication of this case report. Ethical standards and consent: not applicable.
Disclosure Statement
The authors declare that they have no competing interests.
Author Contributions
M.I. Zapata Laguado, J.E. Aponte Monsalve, J.H. Santos, J. Preciado, A. Mosquera Zamudio, and C. Garza Acosta participated in the recollection of data and writing of the first draft. M.I. Zapata Laguado and J.E. Aponte Monsalve participated in the search of literature and drafted and translated the manuscript. All authors read and approved the final manuscript.
References
- 1.Lee AJ, Brenner L, Mourad B, Monteiro C, Vega KJ, Munoz JC. Gastrointestinal Kaposi's sarcoma: Case report and review of the literature. World J Gastrointest Pharmacol Ther [Internet] 2015 Aug 6 [Cited 2018 Mar 23]6((3)):89. doi: 10.4292/wjgpt.v6.i3.89. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26261737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stănescu L, Foarfă C, Georgescu AC, Georgescu I. Kaposi's sarcoma associated with AIDS. Rom J Morphol Embryol [Internet] 2007 [Cited 2018 Mar 23]48((2)):181–7. Available from: http://www.rjme.ro/RJME/resources/files/480207181187.pdf. [PubMed] [Google Scholar]
- 3.Arora M, Goldberg EM. Kaposi sarcoma involving the gastrointestinal tract. Gastroenterol Hepatol (N Y) [Internet] 2010 Jul [Cited 2018 Mar 23]6((7)):459–62. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20827371. [PMC free article] [PubMed] [Google Scholar]
- 4.Friedman-Kien AE, Saltzman BR. Clinical manifestations of classical, endemic African, and epidemic AIDS-associated Kaposi's sarcoma. J Am Acad Dermatol [Internet] 1990 Jun [Cited 2018 Mar 23]22((6 Pt 2)):1237–50. doi: 10.1016/0190-9622(90)70169-i. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2193952. [DOI] [PubMed] [Google Scholar]
- 5.Rabkin CS. AIDS and cancer in the era of highly active antiretroviral therapy (HAART) Eur J Cancer [Internet] 2001 Jul [Cited 2018 Mar 23]37((10)):1316–9. doi: 10.1016/s0959-8049(01)00104-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11423263. [DOI] [PubMed] [Google Scholar]
- 6.Levine AM, Tulpule A. Clinical aspects and management of AIDS-related Kaposi's sarcoma. Eur J Cancer [Internet] 2001 Jul [Cited 2018 Mar 23]37((10)):1288–95. doi: 10.1016/s0959-8049(01)00109-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11423260. [DOI] [PubMed] [Google Scholar]
- 7.Kibria R, Siraj U, Barde C. Kaposi's sarcoma of the stomach and duodenum in human immunodeficiency virus infection. Dig Endosc [Internet] 2010 Jun 21 [Cited 2018 Mar 21]22((3)):241–2. doi: 10.1111/j.1443-1661.2010.00994.x. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20642618. [DOI] [PubMed] [Google Scholar]
- 8.Lin CH, Hsu CW, Chiang YJ, Ng KF, Chiu CT. Esophageal and gastric Kaposi's sarcomas presenting as upper gastrointestinal bleeding. Chang Gung Med J [Internet] 2002 May [Cited 2018 Mar 21]25((5)):329–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12141706. [PubMed] [Google Scholar]
- 9.Santangelo WC, Krejs GJ. Gastrointestinal manifestations of the acquired immunodeficiency syndrome. Am J Med Sci [Internet] 1986 Nov [Cited 2018 Mar 21]292((5)):328–34. doi: 10.1097/00000441-198611000-00016. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3535499. [DOI] [PubMed] [Google Scholar]
- 10.Mansfield SA, Stawicki SP, Forbes RC, Papadimos TJ, Lindsey DE. Acute upper gastrointestinal bleeding secondary to Kaposi sarcoma as initial presentation of HIV infection. J Gastrointestin Liver Dis [Internet] 2013 Dec [Cited 2018 Mar 24]22((4)):441–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24369327. [PMC free article] [PubMed] [Google Scholar]
- 11.Cairncross LL, Davidson A, Millar AJ, Pillay K. Kaposi sarcoma in children with HIV: a clinical series from Red Cross Children's Hospital. J Pediatr Surg [Internet] 2009 Feb [Cited 2018 Mar 25]44((2)):373–6. doi: 10.1016/j.jpedsurg.2008.10.087. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0022346808009512. [DOI] [PubMed] [Google Scholar]
- 12.Yıldız B, Ersoz S, Fıdan E, Fidan S, Ozdemır F, Kavgaci H. Aydın F Classic Kaposi's Sarcoma with Multiple Visceral Organ involvement Presenting with Gastrointestinal Bleeding. HealthMed [Internet] 2010 [Cited 2018 Mar 25]4((2)):1103. Available from: http://connection.ebscohost.com/c/articles/57551318/classic-kaposis-sarcoma-multiple-visceral-organ-involvement-presenting-gastrointestinal-bleeding. [Google Scholar]
- 13.Bello Rodríguez L, Pardeiro Pértega R, Couto Wörner I, Vázquez Rodríguez P, López Calvo S, Castro Iglesias MÁ, et al. Upper gastrointestinal bleeding due to gastric and duodenal Kaposi's sarcoma. Rev Española Enfermedades Dig [Internet] 2012 Jan [Cited 2018 Mar 25]104((1)):33–4. doi: 10.4321/s1130-01082012000100007. Available from: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1130-01082012000100007&lng=en&nrm=iso&tlng=en. [DOI] [PubMed] [Google Scholar]
- 14.Carmo J, Marques SC, Bispo M, Pinto D, Chagas C. Clinical and Endoscopic Features of Gastrointestinal Kaposi Sarcoma: A Single-Center Portuguese Experience over the Last Decade. GE Port J Gastroenterol [Internet] 2017 Sep [Cited 2018 Mar 25]24((5)):219–26. doi: 10.1159/000461592. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29255756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagata N, Shimbo T, Yazaki H, Asayama N, Akiyama J, Teruya K, et al. Predictive Clinical Factors in the Diagnosis of Gastrointestinal Kaposi's Sarcoma and Its Endoscopic Severity. Tang J, editor. PLoS One [Internet] 2012 Nov 30 [Cited 2018 Mar 21]7((11)):e46967. doi: 10.1371/journal.pone.0046967. Available from: http://dx.plos.org/10.1371/journal.pone.0046967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacobson LP, Yamashita TE, Detels R, Margolick JB, Chmiel JS, Kingsley LA, et al. Impact of potent antiretroviral therapy on the incidence of Kaposi's sarcoma and non-Hodgkin's lymphomas among HIV-1-infected individuals. Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr [Internet] 1999 Aug 1 [Cited 2018 Mar 25]21(Suppl 1):S34–41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10430217. [PubMed] [Google Scholar]
- 17.Gill PS, Tulpule A, Espina BM, Cabriales S, Bresnahan J, Ilaw M, et al. Paclitaxel Is Safe and Effective in the Treatment of Advanced AIDS-Related Kaposi's Sarcoma. J Clin Oncol [Internet] 1999 Jun [Cited 2018 Mar 25]17((6)):1876–1876. doi: 10.1200/JCO.1999.17.6.1876. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10561228. [DOI] [PubMed] [Google Scholar]
- 18.Martín‐Carbonero L, Palacios R, Valencia E, Saballs P, Sirera G, Santos I, et al. Long‐Term Prognosis of HIV‐Infected Patients with Kaposi Sarcoma Treated with Pegylated Liposomal Doxorubicin. Clin Infect Dis [Internet] 2008 Aug [Cited 2018 Mar 25]47((3)):410–7. doi: 10.1086/589865. Available from: https://academic.oup.com/cid/article-lookup/doi/10.1086/589865. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.