Introduction
Approximately 3% of patients undergoing screening colonoscopy will have a polyp ≥ 2 cm in diameter (1). Most of these “complex polyps” are too large or too flat to remove with standard polypectomy. Management of challenging lesions may include surgical referral for partial colectomy. This practice, however, is outdated. With recent advances in endoscopic mucosal resection (EMR), over 90% of advanced polyps that lack overt features of cancer can be removed during outpatient colonoscopy, regardless of their size (2).
In principle, all benign polyps should be removed endoscopically, not with colectomy. Colonoscopic resection is recommended as the first-line treatment by societies and guidelines worldwide, including the US Multi-society Task Force on Colorectal Cancer (2–5), and is endorsed by colorectal surgeons (5, 6); it is both more cost-effective than surgery, and associated with lower morbidity and mortality (7, 8). A recent analysis of National Surgical Quality Improvement Program (NSQIP) data found a 30-day mortality of 0.7% for surgical resection of non-malignant polyps, which increased to 3% among patients above age 80 (9). By comparison, the 30-day mortality associated with endoscopic resection was only 0.08% in a review of 6440 patients (10) and zero in a prospective study of 1050 patients (11). In other words, overall surgical mortality for management of benign polyps is nearly 10-fold higher than for endoscopic resection.
Sometimes, colectomy can offer a more definitive solution, such as in patients with numerous polyps or polyps involving the appendiceal orifice or ileocecal valve, suspected Lynch syndrome, or dysplastic colitis associated lesions. However, even these circumstances do not necessarily preclude successful endoscopic management, and consultation with an expert “resectionist” prior to considering colectomy is appropriate.
While endoscopic solutions for patients with non-malignant colorectal polyps have evolved, practice patterns in the US have been slow to follow. In a recent report, nearly one in three elective colon resections had been performed for treatment of benign polyps (12). In order to improve the quality of care for these patients, some significant barriers will need to be addressed.
Presumption of malignancy: All big polyps are not malignant.
“That polyp is huge – it must have cancer in it!”
Endoscopists may falsely presume that an advanced polyp is malignant and unsuitable for endoscopic resection (13). With high-definition endoscopes and skill in visual diagnosis however, endoscopically curable polyps can generally be identified by their appearance. Universal skills in optical diagnosis are key in complex polyp management. Endoscopic training must therefore emphasize lesion characterization by gross morphology and surface features (Paris and Narrow-band imaging International Colorectal Endoscopic (NICE) Classifications), which should be included in procedure reports.
Expectations: All polyps are not the same.
“My patient will be upset if I don’t try to remove this polyp.”
Many endoscopists and patients share a presumption that any polyp discovered at a screening colonoscopy should be removed during the same procedure. A more reasonable expectation would be that certain findings may require treatment at another session. It is usually wisest to treat complex polyps at a dedicated procedure after the plan and risks have been reviewed with the patient, with ample time allotted, with all necessary equipment at hand, and with adequately trained staff present.
Training: Expertise in colonoscopy is not the same as expertise in EMR.
“I doubt that anyone could resect that polyp!”
Performing high quality EMR requires training and high procedural volumes to achieve and maintain competency. In one report, at least 100 colorectal EMR procedures were required to attain adequately high rates of technical success (14). Complex polypectomies performed by specialist endoscopists are associated with better outcomes including a lower risk of incomplete resection (15, 16). However, what constitutes appropriate training in advanced resection techniques is not widely accepted. Currently, there is no formal curriculum for EMR training during fellowship, and most advanced fellowships do not focus on resection techniques. Academic institutions should consider creating tracks dedicated to training advanced mucosal resection experts. Furthermore, as learning opportunities often diminish after entering practice, professional societies should continue to support initiatives such as the Skills Training Assessment Reinforcement (“STAR”) Certificate Program of the American Society of Gastrointestinal Endoscopy (ASGE), which to date has trained members from over 25 US states in lower EMR skills (ASGE, personal communication).
In the US, colonoscopy is performed by gastroenterologists, surgeons, and primary care physicians, and not all are familiar with the spectrum of lesions amenable to EMR or other advanced mucosal resection techniques. Some may lack access to a local EMR expert, or not know how to locate the nearest high-volume center of excellence. Though the availability of endoscopists with EMR expertise is limited in some regions of the US, patients are often motivated to travel a considerable distance to avoid a colectomy and its attendant risks.
GI societies could help identify means for recognizing centers of excellence, and communicate this information as a resource for referring physicians.
Reimbursement: All procedures are not equitably reimbursed.
“Why should I spend my time on that polyp when I won’t get reimbursed for the time, and it will delay the other patients on my schedule? I’ll just refer them to surgery.”
As compared to performing a simple polypectomy, a difficult and time-consuming EMR is often not reimbursed in proportion to the work involved. Thus, for the time-pressured endoscopist, referral to a surgeon is a more cost-effective use of their time than working on a challenging polyp. Insurance companies and regulatory bodies can powerfully influence physician behavior, through compensation schedules and pre-authorizations. However, the current financial climate does not incentivize endoscopic resection over colectomy. Compared to EMR, surgery with a laparoscopic hemicolectomy (CPT44204) generates a 2017 Medicare professional reimbursement nearly five times greater than that for colonic EMR (CPT 45390). Until reimbursement is more proportionate to the time and effort required, advanced endoscopic resection procedures will not reach their full potential in the US. Health systems participating in alternative payment models with downside financial risk (e.g. accountable care organizations) should find EMR financially attractive. Savvy endoscopists working within these systems may be able to negotiate more favorable remuneration for this cost-effective service.
High quality care for patients with complex polyps:
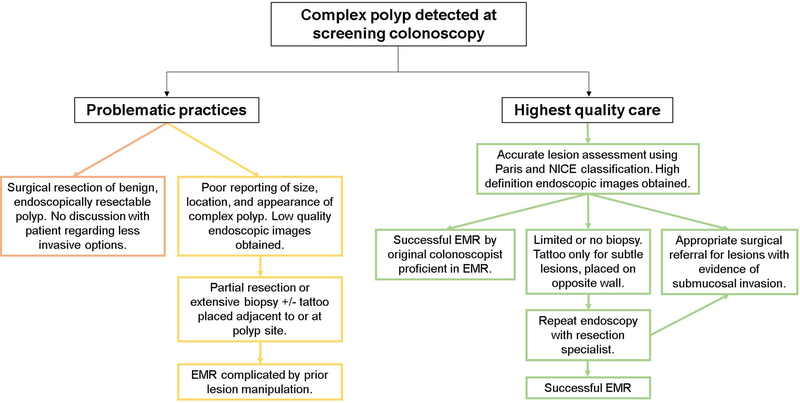
What can referring physicians do to ensure the highest quality of care (Figure 1)?
Carefully assess and characterize lesions (Paris classification, NICE) with high-definition endoscopy. High quality digital images should be provided to the consulting physician to counsel patients and plan their resection procedures (Figure 2).
Avoid attempts at removal when in doubt. The largest contributor to inferior EMR outcomes is the incomplete removal of a lesion prior to referral (Figure 3) (17). Biopsies can be avoided except when signs of invasive cancer are present, such as depressed morphology and loss of regular surface or vascular pattern (Figure 4). Biopsies can cause submucosal fibrosis and subsequent non-lifting properties. Aggressive biopsies and partial removal reduce the chance of a successful one-stage resection, increase risk of bleeding and perforation, and unnecessarily drive up procedure times, costs, and follow-up examinations.
Be cautious placing tattoos near the lesion. An accurate description and high quality photo is preferred over a tattoo. Tattoos may actually complicate resection attempts because the carbon tends to track several centimeters from the injection site and underneath the lesion, leading to submucosal fibrosis (Figure 5). If a tattoo is placed, the marking should be on the opposite wall 5cm distal to the lesion.
Only refer patients for surgical resection when invasive cancer is present. “Intramucosal carcinoma” is not invasive cancer, but rather an endoscopically curable lesion whose misleading name often leads to an unnecessary surgical referral.
Counsel patients about the option of endoscopic resection, even when treatment requires travelling a considerable distance.
Figure 1:
Best practices for high quality care of patients with complex polyps
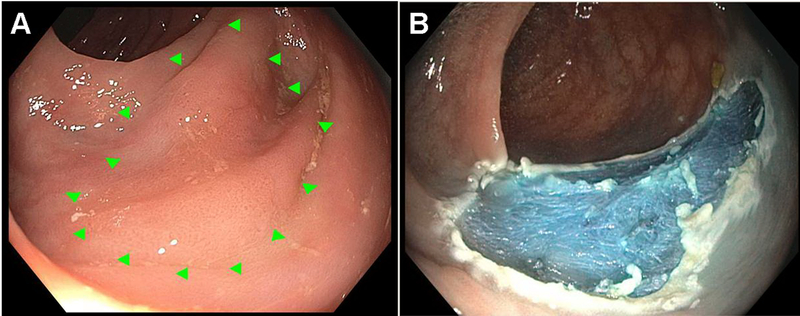
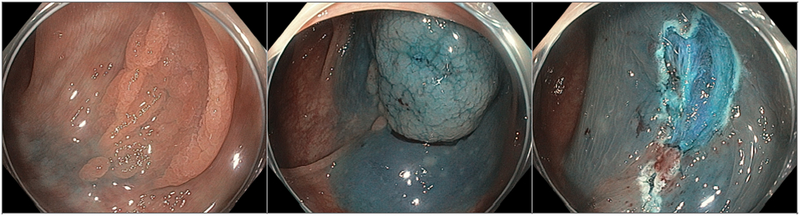
Figure 2:
Example of a 20mm flat (Paris 0-IIb, NICE 2) non-granular laterally spreading lesion referred to a specialized center for EMR. Referring physician described location of polyp in detail, provided high quality endoscopic images (A), avoided biopsy or partial removal during index procedure, and tattooed the opposite wall of the colon to aid the EMR practitioner in locating this subtle polyp. EMR performed 1 month later with excellent results. Histopathology revealed a tubular adenoma without high-grade dysplasia.
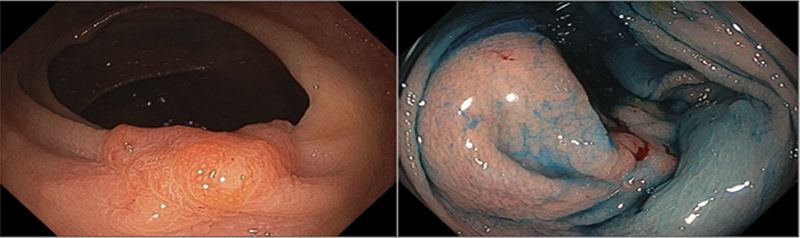
Figure 3:
Paris 0-Is lesion demonstrating non-lifting sign, due to a prior incomplete resection that caused severe submucosal fibrosis.
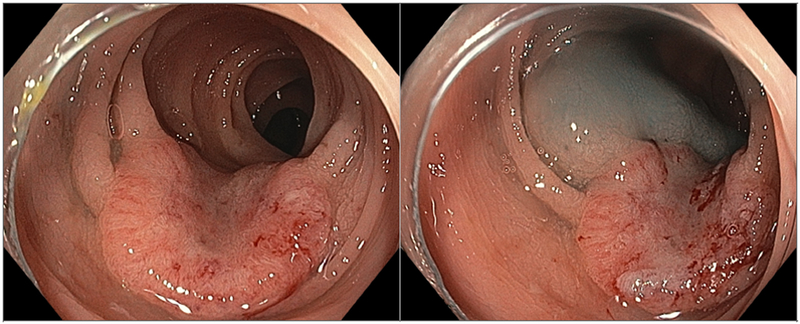
Figure 4:
Deep submucosal invasion, identified by central depression, loss of surface and vascular patterns, and a non-lifting sign. These are the major visible predictors of deep invasion and unresectability.
Figure 5:
Paris 0-IIa lesion with adjacent tattoo, which contributed to non-lifting and suboptimal EMR.
Endoscopic resection techniques have advanced substantially in the last decade. Most complex benign polyps can now be safely resected endoscopically, sparing patients the higher risks and costs of colectomy. Gastroenterologists, surgeons, professional societies, and payers should work together to promote endoscopic resection as the treatment of choice for all benign colorectal polyps.
Table 1:
Barriers and possible solutions to optimize care for patients with complex polyps
| Barriers | Possible solutions |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
Acknowledgments
Financial support: Dr. Crockett’s effort was supported in part by a grant from the NIH (KL2TR001109). Dr. Peery’s effort was also supported in part by a grant from the NIH (K23 DK113225).
REFERENCES
- 1.Ferlitsch M, Reinhart K, Pramhas S, et al. Sex-specific prevalence of adenomas, advanced adenomas, and colorectal cancer in individuals undergoing screening colonoscopy. JAMA 2011;306:1352–8. [DOI] [PubMed] [Google Scholar]
- 2.Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2017;49:270–297. [DOI] [PubMed] [Google Scholar]
- 3.Rex DK, Bond JH, Winawer S, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2002;97:1296–308. [DOI] [PubMed] [Google Scholar]
- 4.Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2015;81:31–53. [DOI] [PubMed] [Google Scholar]
- 5.Rutter MD, Chattree A, Barbour JA, et al. British Society of Gastroenterology/Association of Coloproctologists of Great Britain and Ireland guidelines for the management of large non-pedunculated colorectal polyps. Gut 2015;64:1847–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Church J, Erkan A. Scope or scalpel? A matched study of the treatment of large colorectal polyps. ANZ J Surg 2016. [DOI] [PubMed] [Google Scholar]
- 7.Jayanna M, Burgess NG, Singh R, et al. Cost Analysis of Endoscopic Mucosal Resection vs Surgery for Large Laterally Spreading Colorectal Lesions. Clin Gastroenterol Hepatol 2016;14:271–8 e1–2. [DOI] [PubMed] [Google Scholar]
- 8.Law R, Das A, Gregory D, et al. Endoscopic resection is cost-effective compared with laparoscopic resection in the management of complex colon polyps: an economic analysis. Gastrointest Endosc 2016;83:1248–57. [DOI] [PubMed] [Google Scholar]
- 9.Peery AF, Shaheen NJ, Cools KS, et al. Morbidity and mortality after surgery for nonmalignant colorectal polyps. Gastrointest Endosc 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hassan C, Repici A, Sharma P, et al. Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut 2016;65:806–20. [DOI] [PubMed] [Google Scholar]
- 11.Ahlenstiel G, Hourigan LF, Brown G, et al. Actual endoscopic versus predicted surgical mortality for treatment of advanced mucosal neoplasia of the colon. Gastrointest Endosc 2014;80:668–76. [DOI] [PubMed] [Google Scholar]
- 12.Zogg CK, Najjar P, Diaz AJ, et al. Rethinking Priorities: Cost of Complications After Elective Colectomy. Ann Surg 2016;264:312–22. [DOI] [PubMed] [Google Scholar]
- 13.Aziz Aadam A, Wani S, Kahi C, et al. Physician assessment and management of complex colon polyps: a multicenter video-based survey study. Am J Gastroenterol 2014;109:1312–24. [DOI] [PubMed] [Google Scholar]
- 14.Bhurwal A, Bartel MJ, Heckman MG, et al. Endoscopic mucosal resection: learning curve for large nonpolypoid colorectal neoplasia. Gastrointest Endosc 2016;84:959–968 e7. [DOI] [PubMed] [Google Scholar]
- 15.Tavakkoli A, Law RJ, Bedi AO, et al. Specialist Endoscopists Are Associated with a Decreased Risk of Incomplete Polyp Resection During Endoscopic Mucosal Resection in the Colon. Dig Dis Sci 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brooker JC, Saunders BP, Shah SG, et al. Endoscopic resection of large sessile colonic polyps by specialist and non-specialist endoscopists. Br J Surg 2002;89:1020–4. [DOI] [PubMed] [Google Scholar]
- 17.Moss A, Bourke MJ, Williams SJ, et al. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 2011;140:1909–18. [DOI] [PubMed] [Google Scholar]