Abstract
Background
Evidence has suggested a potential link exists between trimethylamine-N-oxide (TMAO), a choline-derived metabolite produced by gut microbiota, and some cancers, but little is known for primary liver cancer (PLC).
Methods
A case-control study was designed including 671 newly diagnosed PLC patients and 671 control subjects frequency-matched by age (±5 years) and sex, in Guangdong province, China. High-performance liquid chromatography with online electrospray ionization tandem mass spectrometry (HPLC-MS/MS) was used to measure serum TMAO and choline. The associations between these biomarkers and PLC risk were evaluated using logistic regression models.
Results
Serum TMAO concentrations were greater in the PLC group than the control group (P = 0.002). Logistic regression analysis showed that the sex- and age-adjusted odds ratio (OR) and (95% confidence interval [CI]) was 3.43 (2.42–4.86) when comparing the top and bottom quartiles (Q4 vs Q1). After further adjusting for more selected confounders, the OR (95% CI) remained significant but was attenuated to 2.85 (1.59–5.11) (Q4 vs Q1). The multivariable-adjusted ORs (95% CIs) across quartiles of choline were 0.35–0.15 (P-trend < 0.001).
Conclusion
Higher serum levels of TMAO were associated with increased PLC risk. The association was stronger in those with lower serum levels of choline. Additional large prospective studies are required to confirm these findings.
Trial registration
This study was registered at clinicaltrials.gov as NCT 03297255.
Keywords: Trimethylamine N-oxide (TMAO), Choline, Gut microbiota metabolite, Liver cancer, Case control study
Background
Primary liver cancer (PLC) is one of the deadliest malignant tumors worldwide [1]. An estimated 0.8 million new diagnoses of liver cancer and deaths occurred worldwide during 2012, with approximately 50% of the total number occurring in China alone [2]. Chronic viral hepatitis B (HBV) and C (HCV) and exposure to aflatoxin are the predominant risk factors for PLC [3]. Since the implementation of the routine infant HBV immunization [4], as well as improvements in hygiene and sanitation [5], infection-related liver cancer rates are decreasing in historically high-risk areas [5]. However, non-infection-related risk factors for PLC such as alcohol abuse, tobacco smoking, non-alcoholic fatty liver disease (NAFLD), obesity, and type 2 diabetes, have raised concern over recent years [5]. In addition, growing evidence suggests that diet plays a crucial role [6–8] in PLC development.
Choline is an essential nutrient in one-carbon metabolism [8], its effect on the level of DNA methylation is postulated to play an important role in tumor development [8–10]. Previous studies have shown that a deficiency in dietary choline may promote the development of liver cancer both in animals and humans [11, 12]. Additionally, circulating choline was also found to be associated with liver cancer risk in a nested case-control study including 297 male liver cancer patients and 631 male matched controls [13].
Trimethylamine N-oxide (TMAO) is a gut microbiota-dependent metabolite of choline that is formed in the liver by the hepatic enzyme flavin-containing monooxygenase-3 (FMO3) [14]. With the development of microbial metabolomics, investigators have demonstrated TMAO as a risk factor for many diseases [15] including cardiovascular disease [14, 16, 17], type 2 diabetes [18, 19] and chronic kidney disease [20]. All of these diseases may increase the risk of PLC [21, 22]. Moreover, some recent studies suggest a link between TMAO and the risk of cancer development, especially colorectal cancer (CRC) [23–25]. Sajin Bae et al. first reported that plasma TMAO was positively associated with rectal cancer in a nested case-control study including 835 matched case-control pairs [23]. Another study revealed a strong genetic link between CRC and TMAO using genome-wide systems analysis to construct chemical-gene, disease-gene, and protein-protein interaction data from multiple large-scale data resources [25]. Furthermore, through the use of systematic disease enrichment analysis, the study also demonstrated that TMAO may be related to other types of cancer, including liver cancer [25]. Since the generation of TMAO involves crosstalk between the gut and liver (dietary choline/betaine/L-carnitine → trimethylamine formed in gut→ TMAO formed in liver) [17], the link between TMAO and CRC suggests that TMAO may also be related to PLC. Although none of the existing studies have assessed the association between TMAO and liver cancer, our previous research demonstrated a significant positive association between serum TMAO and NAFLD [26]. Since NAFLD is a well-established risk factor for PLC, the association supports a possible link between TMAO and PLC.
Collectively, we conducted a case-control study to investigate the association between serum TMAO, a gut microbiota-dependent metabolite of choline, and PLC risk in a large Chinese population.
Methods
Study population
A cross-sectional case-control study was conducted. Recruitment methods for PLC patients have been previously detailed. [6] Newly diagnosed (within one month) adults with PLC from Sun Yat-sen University Cancer Center in the Guangdong province were consecutively enrolled between September 2013 and April 2017. All cases were diagnosed according to the National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology: Hepatobiliary Cancers [27]. PLC patients were excluded if they (1) had no blood samples, (2) had a history of other cancers, or (3) had a history of stroke or chronic kidney disease. Controls meeting the same inclusion and exclusion criteria, with the exception of liver cancer, were concurrently enrolled from local communities in the Guangdong province. A total of 671 eligible PLC patients and 671 controls, frequency-matched by age (±5 years) and sex, were included in the present analyses. Written informed consent was provided by all study participants, and the study protocol was approved by the Ethics Committee of the School of Public Health at Sun Yat-sen University.
Data collection
Information on socio-demographic characteristics and lifestyle habits over the past year was obtained by well-trained research interviewers using a structured questionnaire. Household income was divided into three groups: ≤2000, 2001–6000, and > 6000 Yuan/month/person. Occupation was determined by labor intensity. Participants’ marital status was determined as either married or not married. Education was grouped into three levels: primary school or below, secondary and high school, and college or above. Participants who smoked at least one cigarette per day or drank alcohol at least once a week continuously for at least six months in one’s whole life, were defined as smokers or alcohol drinkers.
Anthropometric data including waist circumference (WC), height (m), and weight (kg) were obtained using standard procedures and measuring equipment. Body mass index (BMI; kg/m2) was calculated. Blood pressure (BP) was measured using a calibrated sphygmomanometer (Hawksley, WA Baum Co, USA). Serostatus of hepatitis B surface antigen was determined by enzyme linked immunosorbent assay. Serum total cholesterol (TC) and triglycerides (TG) were analyzed using enzymatic colorimetric tests; the elective inhibition method was used to measure serum high-density lipoprotein cholesterol (HDL-C). Fasting blood glucose (FBG) was determined using the hexokinase method. All biochemical parameters were determined using commercially available kits on an automatic biochemistry analyzer (Advia1650 Autoanalyzer, Byer Diagnostics, Leverkusen, Germany). Metabolic syndrome (Mets) was diagnosed based on WC, BP, TG, HDL-C and FBG, according to International Diabetes Federation criteria [28].
Laboratory analysis of serum TMAO and choline
Fasting serum samples were isolated and stored at − 80 °C until analysis. Serum TMAO and choline were assessed using high-performance liquid chromatography with online electrospray ionization tandem mass spectrometry (HPLC-MS/MS) (Agilent 6400 Series Triple Quad LCMS; CA, USA) [29], using multi-reaction monitoring (MRM) functions. 100 μl of acetonitrile containing 10 μM of internal standards [d9-TMAO (Toronto Research Chemicals Inc., Toronto, Canada), d9-choline (Sigma-Aldrich, St. Louis, USA)] was added to 60 μl of either the serum sample or standards. The samples were then centrifuged at 13,000×g for 10 min to precipitate the proteins. Finally, the remaining supernatant was injected into a normal-phase silica column (2.1 mm × 100 mm, 5 μM) and equilibrated with 30% solution A (15 mmol/L ammonium formate in water, pH 3.0) and 70% solution B (acetonitrile) under isocratic elution with a flow rate of 0.2 mL/min. Ten pairs of duplicate control samples were randomly interspersed to assess laboratory precision. The coefficients of variation for the between-run assays were 6.0 and 4.9% for TMAO and choline, respectively.
Statistical analysis
Data were analyzed using SPSS version 20.0 for Windows (SPSS Inc., Chicago, IL, USA). P-values were based on two-tailed tests and P < 0.05 was considered to be statistically significant.
All analyses included men and women combined, with the exception of analyses stratified by sex. Differences in socio-demographic characteristics, presence of Mets, serum TMAO, and choline concentrations between patients and controls were compared by t-test, chi-squared test, and Wilcoxon rank-sum test as appropriate. Serum TMAO and choline concentrations were grouped into quartiles (Q1–Q4) based on control subjects, and then the cutoffs were applied to the PLC patients. Logistic regression models were used to calculate odds ratios (ORs) and corresponding 95% confidence intervals (CIs) with the first quartile as the reference. The forward stepwise method was used to select variables included in the multivariable analyses, and only those that were statistically significant (P < 0.10) were included in the final models. Only age and sex were adjusted for in model 1. Further adjustments were made for BMI, household income, occupation, marital status, smoking status, alcohol use, presence of Mets, and HBV infection status in model 2. Linear trends across increasing quartiles were assessed by assigning quartiles as continuous variables in the regression models. To investigate possible associations between various joint effects of serum TMAO and choline with PLC risk, four groups were studied according to combinations of serum TMAO and choline that were stratified based on the study population medians. The group with low-TMAO and high-choline was considered as the reference group (group 1).
In stratified analyses, we divided serum TMAO and choline into quartiles and then combined the second and third quartiles into a middle 50% to examine whether associations between serum TMAO/choline and PLC risk were different in various subgroups (HBV-infected subjects vs non-HBV-infected subjects, alcohol drinkers vs non-alcohol drinkers, smokers vs non-smokers, men vs women, with Mets vs without Mets). Interactions were estimated via multiplicative interaction terms in the multivariate model 2.
Results
Basic characteristics
Basic characteristics of the 671 PLC patients and control pairs (569 male pairs and 102 female pairs) are presented in Table 1. The mean (±S.D.) age of PLC patients and non-PLC controls were 58.6 ± 7.6 years and 58.6 ± 7.5 years, respectively. Compared with controls, PLC patients were more likely to have a lower BMI, lower level of education, lower incidence of Mets, and higher household income. A significantly greater proportion of PLC patients had heavy intensity occupations, were married, were alcohol drinkers, and were infected with HBV (P < 0.05 for all variables). No significant differences were observed in smoking status between patients and controls.
Table 1.
Comparison of selected characteristics between PLC cases and controls
| Variables | PLC | Controls | P value |
|---|---|---|---|
| Age (years)a | 58.6 ± 7.6 | 58.6 ± 7.5 | 0.981 |
| Men, n (%) | 569 (84.8) | 569 (84.8) | – |
| BMI (kg/m2) a | 22.8 ± 3.1 | 23.8 ± 3.1 | < 0.001 |
| Household income (Yuan/month/person), n (%) | |||
| ≤2000 | 206 (30.7) | 355 (52.9) | < 0.001 |
| 2001–6000 | 410 (61.1) | 283 (42.2) | |
| > 6000 | 55 (8.2) | 33 (4.9) | |
| Occupation, n (%) | |||
| Light intensity of activity | 246 (36.7) | 365 (54.4) | < 0.001 |
| Moderate intensity of activity | 209 (31.2) | 193 (28.8) | |
| Heavy intensity of activity | 216 (32.2) | 113 (16.8) | |
| Married, n (%) | 658 (98.1) | 643 (95.8) | 0.017 |
| Education level, n (%) | |||
| Primary school or below | 176 (26.2) | 38 (5.7) | < 0.001 |
| Secondary & High school | 387 (57.7) | 409 (61.0) | |
| College or above | 108 (16.1) | 224 (33.4) | |
| Smoker, n (%) | 302 (45.0) | 272 (40.6) | 0.098 |
| Alcohol drinker, n (%) | 186 (27.7) | 85 (12.7) | < 0.001 |
| HBV infection, n (%) | 582 (86.7) | 60 (8.9) | < 0.001 |
| Mets, n (%) | 128 (19.1) | 174 (25.9) | 0.003 |
| Serum choline (μmol/L) a | 12.88 ± 4.53 | 17.33 ± 5.15 | < 0.001 |
| Serum TMAO (μmol/L) b | 2.07 (1.32,3.49) | 1.61 (0.87,2.92) | 0.002 |
Abbreviations: BMI = body mass index, PLC = primary liver cancer, HBV = hepatitis B virus, Mets = Metabolic syndrome, TMAO = trimethylamine N-oxide
aContinuous values are mean ± S.D.
bValue is median (IQR)
Compared with controls, PLC patients had significantly higher serum levels of TMAO (2.07 (1.32, 3.49) μmol/L vs 1.61 (0.87, 2.92) μmol/L)) and lower levels of choline (12.88 ± 4.53 μmol/L vs 17.33 ± 5.15 μmol/L). All P-values were < 0.05.
Associations between serum TMAO, choline, and PLC risk
Associations between serum TMAO, choline and PLC risk are shown in Table 2. In the sex- and age-adjusted analysis, participants with higher serum TMAO had a significantly increased risk of PLC (P-trend < 0.001); the OR (95% CI) was 3.43 (2.42–4.86) when comparing the top and bottom quartiles (Q4 vs Q1). After further adjusting for BMI, household income, occupation, marital status, smoking status, alcohol use, presence of Mets, and HBV infection status, the OR remained significant (P-trend = 0.003) but was attenuated to 2.85. An inverse association between serum choline and PLC risk was found. A higher serum concentration of choline was associated with a significantly lower risk of PLC (P-trend < 0.001). The adjusted OR (95% CI) for Q4 vs Q1 was 0.15 (0.08–0.28) in the multivariate-adjusted model 2.
Table 2.
Odds ratios (ORs) and 95% confidence intervals (CIs) of PLC according to quartiles of serum TMAO and choline levels among controls
| Level (μmol/L) | n (Cases/Controls) | OR1 (95% CI) a | OR2 (95% CI) b | |
|---|---|---|---|---|
| Serum TMAO | ||||
| Q1 | ≤0.87 | 66/168 | 1.00 | 1.00 |
| Q2 | 0.87–1.61 | 167/168 | 2.53 (1.77–3.61) | 2.41 (1.32–4.40) |
| Q3 | 1.61–2.92 | 213/168 | 3.23 (2.28–4.58) | 2.91 (1.62–5.23) |
| Q4 | ≥2.92 | 225/167 | 3.43 (2.42–4.86) | 2.85 (1.59–5.11) |
| P-trend | < 0.001 | 0.003 | ||
| Serum choline | ||||
| Q1 | ≤13.27 | 425/167 | 1.00 | 1.00 |
| Q2 | 13.27–16.95 | 134/168 | 0.29 (0.22–0.39) | 0.35 (0.21–0.57) |
| Q3 | 16.95–21.03 | 68/168 | 0.15 (0.11–0.21) | 0.22 (0.12–0.38) |
| Q4 | ≥21.03 | 44/168 | 0.09 (0.06–0.14) | 0.15 (0.08–0.28) |
| P-trend | < 0.001 | < 0.001 | ||
aAdjusted for age and sex
bFurther adjusted for BMI, household income, occupation, marital status, smoking status, alcohol use, presence of metabolic syndrome, and HBV infection status
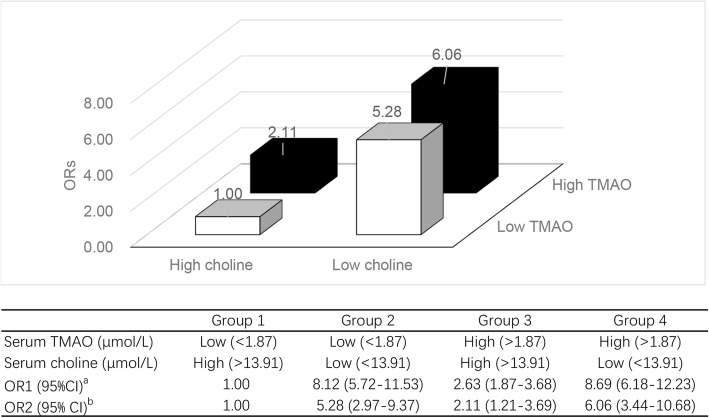
In the four combined groups analyses, median concentrations of the whole study population were 1.87 μmol/L and 13.91 μmol/L for TMAO and choline, respectively. Compared with group 1 (low-TMAO and high-choline), participants with unfavorable factors (high-TMAO, low-choline, or both) all had an increased risk of PLC, those with high-TMAO and low-choline had the highest risk of PLC, the multivariate-adjusted OR (95% CI) for group 4 vs group 1 was 6.06 (3.44–10.68). Data are shown in Fig. 1.
Fig. 1.
ORs and 95% CIs of PLC in four groups: low TMAO/high choline, low TMAO/low choline, high TMAO/high choline, and high TMAO/low choline. Groups were stratified based on the median TMAO and choline concentrations of the entire study population. aAdjusted for age and sex; bFurther adjusted for BMI, household income, occupation, marital status, smoking status, alcohol use, presence of metabolic syndrome, and HBV infection status
Stratified analyses
In risk analyses stratified by HBV infection status, alcohol use, smoking, sex, and presence of Mets, positive associations between TMAO and PLC risk were found only among non-HBV-infected patients (P-trend = 0.006), non-drinkers (P-trend = 0.001), non-smokers (P-trend = 0.001) and participants without Mets (P-trend = 0.006), but not among HBV-infected patients (P-trend = 0.104), alcohol drinkers (P-trend = 0.092), smokers (P-trend = 0.418) and participants with Mets (P-trend = 0.095). However, the P-interaction was only significant between smokers and non-smokers (P-interaction = 0.024).
The inverse associations of choline and PLC risk were not significantly modified, although stronger among non-smokers than smokers (P-trend < 0.001, P-interaction = 0.001), and stronger among women than men (P-trend < 0.001, P-interaction = 0.008). All of the stratified analyses are shown in Table 3.
Table 3.
Associations between serum TMAO and choline levels with PLC risk stratified by selected factors
| Q1 | Combined middle half | Q4 | P -trend | P -interaction | ||
|---|---|---|---|---|---|---|
| Serum TMAO | ||||||
| HBV infectionb | ||||||
| Yes | n (Cases/Controls) | 76/15 | 333/30 | 173/15 | 0.095 | |
| OR (95% CI) a | 1.00 | 1.83 (0.89–3.78) | 2.07 (0.91–4.74) | 0.104 | ||
| No | n (Cases/Controls) | 8/152 | 53/306 | 28/153 | ||
| OR (95% CI) a | 1.00 | 3.82 (1.63–8.94) | 3.73 (1.50–9.30) | 0.006 | ||
| Alcohol usingb | ||||||
| Yes | n (Cases/Controls) | 13/21 | 121/43 | 52/21 | 0.777 | |
| OR (95% CI) a | 1.00 | 2.54 (0.74–8.68) | 3.44 (0.88–13.54) | 0.092 | ||
| No | n (Cases/Controls) | 51/145 | 274/295 | 160/146 | ||
| OR (95% CI) a | 1.00 | 3.10 (1.69–5.67) | 3.57 (1.83–6.96) | 0.001 | ||
| Smokingb | ||||||
| Yes | n (Cases/Controls) | 41/68 | 175/136 | 86/68 | 0.024 | |
| OR (95% CI) a | 1.00 | 1.32 (0.59–2.94) | 1.47 (0.60–3.60) | 0.418 | ||
| No | n (Cases/Controls) | 30/99 | 209/200 | 130/100 | ||
| OR (95% CI) a | 1.00 | 3.92 (1.84–8.35) | 4.88 (2.13–11.19) | 0.001 | ||
| Sexb | ||||||
| Men | n (Cases/Controls) | 74/140 | 312/287 | 183/142 | 0.166 | |
| OR (95% CI) a | 1.00 | 2.04 (1.16–3.60) | 2.28 (1.22–4.26) | 0.016 | ||
| Women | n (Cases/Controls) | 7/25 | 52/52 | 43/25 | ||
| OR (95% CI) a | 1.00 | 1.79 (0.38–8.30) | 5.23 (1.05–26.10) | 0.021 | ||
| Metabolic syndromeb | ||||||
| Yes | n (Cases/Controls) | 14/43 | 75/88 | 39/43 | 0.473 | |
| OR (95% CI) a | 1.00 | 3.04 (0.92–10.01) | 3.45 (0.94–12.65) | 0.095 | ||
| No | n (Cases/Controls) | 50/124 | 307/249 | 186/124 | ||
| OR (95% CI) a | 1.00 | 2.50 (1.35–4.62) | 2.83 (1.44–5.59) | 0.006 | ||
| Serum Choline | ||||||
| HBV infectionb | ||||||
| Yes | n (Cases/Controls) | 368/15 | 151/30 | 63/15 | 0.121 | |
| OR (95% CI) a | 1.00 | 0.22 (0.11–0.46) | 0.22 (0.09–0.50) | < 0.001 | ||
| No | n (Cases/Controls) | 52/152 | 33/306 | 4/153 | ||
| OR (95% CI) a | 1.00 | 0.24 (0.14–0.43) | 0.05 (0.02–0.16) | < 0.001 | ||
| Alcohol usingb | ||||||
| Yes | n (Cases/Controls) | 137/21 | 36/43 | 13/21 | 0.145 | |
| OR (95% CI) a | 1.00 | 0.13 (0.05–0.37) | 0.21 (0.05–0.90) | 0.001 | ||
| No | n (Cases/Controls) | 304/146 | 154/294 | 27/146 | ||
| OR (95% CI) a | 1.00 | 0.34 (0.21–0.56) | 0.13 (0.06–0.27) | < 0.001 | ||
| Smokingb | ||||||
| Yes | n (Cases/Controls) | 200/68 | 69/136 | 33/68 | 0.001 | |
| OR (95% CI) a | 1.00 | 0.16 (0.08–0.34) | 0.21 (0.08–0.53) | < 0.001 | ||
| No | n (Cases/Controls) | 228/98 | 123/201 | 18/100 | ||
| OR (95% CI) a | 1.00 | 0.37 (0.21–0.64) | 0.12 (0.05–0.27) | < 0.001 | ||
| Sexb | ||||||
| Men | n (Cases/Controls) | 361/141 | 161/286 | 47/142 | 0.008 | |
| OR (95% CI) a | 1.00 | 0.23 (0.14–0.38) | 0.20 (0.10–0.38) | < 0.001 | ||
| Women | n (Cases/Controls) | 69/25 | 30/52 | 3/25 | ||
| OR (95% CI) a | 1.00 | 0.34 (0.11–1.10) | 0.01 (0.00–0.08) | < 0.001 | ||
| Metabolic syndromeb | ||||||
| Yes | n (Cases/Controls) | 94/43 | 31/88 | 3/43 | 0.050 | |
| OR (95% CI) a | 1.00 | 0.09 (0.03–0.26) | 0.01 (0.00–0.10) | < 0.001 | ||
| No | n (Cases/Controls) | 329/124 | 169/249 | 45/124 | ||
| OR (95% CI)a | 1.00 | 0.32 (0.19–0.53) | 0.20 (0.10–0.40) | < 0.001 | ||
aAdjusted for age, sex, BMI, household income, occupation, marital status, smoking status, alcohol use, presence of metabolic syndrome, and HBV infection status
bStratified factors were not included in the corresponding model
Discussion
Key findings
To the best of our knowledge, the present study is the first to report on associations between serum TMAO and PLC risk in humans. We found that serum TMAO, a gut flora metabolite of choline, was positively associated with the development of PLC, whereas its precursor choline was inversely associated with PLC risk.
TMAO and PLC
In recent years, many studies have reported associations between TMAO and chronic diseases. In both animals and humans, harmful effects of TMAO have been related to cardiovascular diseases (atherosclerosis [16, 17], thrombosis [30], hypertension [31]), chronic kidney disease [20], and NAFLD [26]. The contributions of TMAO in the development of these chronic diseases have brought attention to its potential role in carcinogenesis, as these diseases are all cancer risk factors. However, existing literature on associations between circulating TMAO and cancer is limited, and results have been inconclusive. Significant positive associations between TMAO and colorectal cancer were first reported in the Women’s Health Initiative Observational Study [23]. Liu et al. suggested a possible prognostic value of preoperative serum TMAO level in 108 colorectal cancer patients [24]. Additionally, Oellgaard et al. reported TMAO as a promising potential therapeutic target for gastrointestinal cancer [32]. Interestingly, divergent results were reported in male participants in the alpha-tocopherol and beta-carotene study, in which the association between TMAO and prostate cancer was positive [33], but null between TMAO and colorectal cancer [34].
Existing data on TMAO in relation to PLC risk is sparse. To our knowledge, the present study is the first to report on associations between serum TMAO and PLC risk in humans. Consistent with most of the previous findings, the present study found a significant association between serum TMAO and risk of PLC. We hypothesize two possible mechanisms. First, TMAO may contribute to liver injury by decreasing the total bile acid pool size and affecting hepatic TG levels [16], which may lead to the development of PLC. Second, TMAO may be an indirect risk factor by participating in the etiology of several chronic diseases, including atherosclerosis [16, 17], thrombosis [30], hypertension [31] and chronic kidney disease [20], which are all potential risk factors for PLC.
However, it is hard to determine from current literature whether serum TMAO is a risk factor or rather a biomarker for PLC status. Increasing evidence suggests the bacterial microbiome plays a key role in promoting liver cancer through the intestinal microbiota–liver axis [35]. Given that TMAO is a gut flora-dependent metabolite, elevated circulating TMAO concentrations may simply be a biomarker of gut microbiota composition fluctuation in PLC patients. Limited by the case-control design, this study could not definitively conclude whether elevated serum TMAO was involved in liver carcinogenesis, or if liver cancer caused the elevation in serum TMAO. Rong Xu et al. previously revealed a link between TMAO and colorectal cancer using a genome-wide systems analysis, and suggested a potential genetic link with other cancers [25]. These connections could be used in future studies of TMAO to better understand its role in PLC.
In the stratified analysis, we noted that the positive association between serum TMAO and PLC risk became insignificant among the HBV-infected patients, alcohol drinkers, smokers and participants with Mets, although the P-interaction was only significant between smokers and non-smokers. A possible explanation would be that HBV, alcohol consumption, smoking and presence of Mets induced changes in gut flora composition and normal function [36–38], which consequently affected the generation of TMAO. In addition, HBV infection, alcohol drinking, smoking and presence of Mets are well-established PLC risk factors [5], their effects on PLC were much greater than TMAO, which may cover the risk effect of TMAO on PLC.
Choline and PLC
The present study showed a robustly favorable relationship between serum choline and PLC. This was consistent with several previous studies [39–43] and with our previous case-control study, which reported an inverse association between dietary choline intake and PLC risk [11]. To date, only one case-control study, including 297 male HCC patients and 631 male matched controls, has reported on the relationship between serum choline and HCC risk [13], in which the favorable role of choline was also found. There are at least two potential mechanisms to explain the inverse associations between high serum choline and decreased PLC risk. First, choline is an important methyl donor in one-carbon metabolism, which can affect DNA methylation levels. Methyl donor deficiency could impair DNA methylation and further induce liver carcinogenesis [8, 44]. Animal models fed a choline-deficient diet have demonstrated an increased risk of liver cancer [44, 45]. Second, choline is necessary for normal lipid and TG transport from the liver, while defective VLDL secretion and fat accumulation may cause chronic liver diseases such as NAFLD or liver cancer [26].
In this study, we noted that serum TMAO and its precursor choline had opposite associations with PLC risk. One of the most likely reasons is that choline is not the only precursor of TMAO. For example, L-carnitine, a nutrient rich in red meat, could also be metabolized to TMAO [16]. In our previous study investigating the association of dietary choline intake and PLC risk, we found that red meat was an important source of dietary choline [11], which implied high dietary L-carnitine intake of the participants.
Strengths and limitations
The present study had several strengths. First, this is the first study to report on associations between serum TMAO and PLC risk in humans. Moreover, the sample size (671 PLC patients and 671 matched controls) is relatively large, compared with the only existing serum choline and HCC risk case-control study (297 HCC patients and 631 matched controls) [13]. Second, only newly diagnosed PLC patients were included with comparable age- and sex-matched to minimize recall bias. Third, multiple confounding factors, including well-established risk factors for PLC, (i.e., HBV infection, alcohol use, smoking) were included in the analyses to reduce residual confounding.
However, several limitations warrant consideration. First, the blood samples were collected at the time point when the participants were diagnosed, a single measurement may not fully reflect the body’s long-term concentrations of choline or its metabolite TMAO. We cannot exclude the possibility that the development of PLC may itself affect concentrations of serum choline and TMAO, even though we recruited only newly diagnosed patients and conducted blood collection as soon as possible. Second, limited by the case-control design, this study could not definitively conclude whether elevated serum TMAO was involved in the liver carcinogenesis, or if liver cancer caused the serum TMAO elevations. More prospective studies are needed to verify the causality between TMAO and PLC. Third, despite the relatively large numbers of participants in the present study, sample size may have played a role in the questionably strong associations seen in women participants, considering the much smaller female sample size. Since liver cancer is much more common in men than in women [2], it was difficult to recruit an equal number of female PLC patients in the present study. Thus, the results from women should be interpreted with caution and need to be confirmed by studies with larger female sample sizes.
Conclusions
In conclusion, the present study revealed opposing associations between serum trimethylamine N-oxide (adverse) and its precursor choline (inverse) with the risk of PLC. We suggest that higher TMAO concentrations are associated with increased risk of PLC, while higher serum choline levels are associated with reduced risk of PLC. However, these results should be interpreted with caution and should be confirmed by large prospective studies in the future.
Acknowledgements
We thank all the participants and researchers for their contributions to this study.
Funding
This study was jointly supported by the National Natural Science Foundation of China (NO. 81773415 and NO. 81472966) and Key Project of Science and Technology Program of Guangzhou, China (NO. 201704020035).
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to privacy protection of the participants but are available from the corresponding author on reasonable request.
Abbreviations
- BMI
Body mass index
- BP
Blood pressure
- CI
Confidence interval
- CRC
Colorectal cancer
- FBG
Fasting blood glucose
- FMO3
Flavin-containing monooxygenase-3
- HDL-C
High-density lipoprotein cholesterol
- Mets
Metabolic syndrome
- NAFLD
Non-alcoholic fatty liver disease
- OR
Odds ratio
- PLC
Primary liver cancer
- TC
total cholesterol
- TG
Triglycerides
- TMAO
Trimethylamine-N-oxide
- WC
Waist circumference
Authors’ contributions
ZYL and HLZ participated in study design and draft the manuscript. HLZ and APF administrated the project. QJL, PYC, XYW, DMZ, YL, JAL and RHZ collected the data and blood samples. XYT and GCL conducted the TMAO and choline analysis. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Written informed consent was provided by all study participants, and the study protocol was approved by the Ethics Committee of the School of Public Health at Sun Yat-sen University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zhao-Yan Liu, Email: liuzhy69@mail2.sysu.edu.cn.
Xu-Ying Tan, Email: tanxy5@mail2.sysu.edu.cn.
Qi-Jiong Li, Email: liqj@sysucc.org.cn.
Gong-Cheng Liao, Email: liaogch3@mail2.sysu.edu.cn.
Ai-Ping Fang, Email: fangaip@mail.sysu.edu.cn.
Dao-Ming Zhang, Email: zhangdm3@mail2.sysu.edu.cn.
Pei-Yan Chen, Email: chpyan@mail2.sysu.edu.cn.
Xiao-Yan Wang, Email: wangxy277@mail2.sysu.edu.cn.
Yun Luo, Email: luoy226@mail2.sysu.edu.cn.
Jing-An Long, Email: longjan@mail2.sysu.edu.cn.
Rong-Huan Zhong, Email: zhongrh6@mail2.sysu.edu.cn.
Hui-Lian Zhu, Phone: +86-20-8733-1811, Email: zhuhl@mail.sysu.edu.cn.
References
- 1.Broutier L, Mastrogiovanni G, Verstegen MM, Francies HE, Gavarro LM, Bradshaw CR, et al. Human primary liver cancer-derived organoid cultures for disease modeling and drug screening. Nat Med. 2017;23:1424–1435. doi: 10.1038/nm.4438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Zhu RX, Seto WK, Lai CL, Yuen MF. Epidemiology of hepatocellular carcinoma in the Asia-Pacific region. Gut and Liver. 2016;10:332–339. doi: 10.5009/gnl15257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang YT, Chen TY, Zhu J, Jiao YC, Qu CF. Primary prevention by hepatitis B vaccine on liver cancer in high incidence area of China. Zhonghua Yu Fang Yi Xue Za Zhi. 2018;52:402–408. doi: 10.3760/cma.j.issn.0253-9624.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 6.Lan Qiu-Ye, Zhang Yao-Jun, Liao Gong-Cheng, Zhou Rui-Fen, Zhou Zhong-Guo, Chen Yu-Ming, Zhu Hui-Lian. The Association between Dietary Vitamin A and Carotenes and the Risk of Primary Liver Cancer: A Case–Control Study. Nutrients. 2016;8(10):624. doi: 10.3390/nu8100624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Budhathoki S, Hidaka A, Yamaji T, Sawada N, Tanaka-Mizuno S, Kuchiba A, et al. Plasma 25-hydroxyvitamin D concentration and subsequent risk of total and site specific cancers in Japanese population: large case-cohort study within Japan public health center-based prospective study cohort. The BMJ. 2018;360:k671. doi: 10.1136/bmj.k671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newman AC, Maddocks ODK. One-carbon metabolism in cancer. Br J Cancer. 2017;116:1499–1504. doi: 10.1038/bjc.2017.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ueland PM. Choline and betaine in health and disease. J Inherit Metab Dis. 2011;34:3–15. doi: 10.1007/s10545-010-9088-4. [DOI] [PubMed] [Google Scholar]
- 10.Richman EL, Kenfield SA, Stampfer MJ, Giovannucci EL, Zeisel SH, Willett WC, Chan JM. Choline intake and risk of lethal prostate cancer: incidence and survival. Am J Clin Nutr. 2012;96:855–863. doi: 10.3945/ajcn.112.039784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu HL, Huang J, Xu M, Fang YJ, Lu MS, Pan ZZ, et al. Higher dietary intakes of choline and betaine are associated with a lower risk of primary liver cancer: a case-control study. Sci Rep. 2017;117:839–850. doi: 10.1038/s41598-017-00773-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brunaud L, Alberto JM, Ayav A, Gerard P, Namour F, Antunes L, et al. Effects of vitamin B12 and folate deficiencies on DNA methylation and carcinogenesis in rat liver. Clin Chem Lab Med. 2003;41:1012–1019. doi: 10.1515/CCLM.2003.155. [DOI] [PubMed] [Google Scholar]
- 13.Butler LM, Arning E, Wang R, Bottiglieri T, Govindarajan S, Gao YT, Yuan JM. Prediagnostic levels of serum one-carbon metabolites and risk of hepatocellular carcinoma. Cancer Epidemiol Biomark Prev. 2013;22:1884–1893. doi: 10.1158/1055-9965.EPI-13-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368:1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Velasquez MT, Ramezani A, Manal A, Raj DS. Trimethylamine N-oxide: the good, the bad and the unknown. Toxins (Basel). 2016;8. [DOI] [PMC free article] [PubMed]
- 16.Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19:576–585. doi: 10.1038/nm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472:57–63. doi: 10.1038/nature09922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim Y, Keogh J, Clifton P. A review of potential metabolic etiologies of the observed association between red meat consumption and development of type 2 diabetes mellitus. Metabolism. 2015;64:768–779. doi: 10.1016/j.metabol.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Dambrova M, Latkovskis G, Kuka J, Strele I, Konrade I, Grinberga S, et al. Diabetes is associated with higher trimethylamine N-oxide plasma levels. Exp Clin Endocrinol Diabetes. 2016;124:251–256. doi: 10.1055/s-0035-1569330. [DOI] [PubMed] [Google Scholar]
- 20.Tang WH, Wang Z, Kennedy DJ, Wu Y, Buffa JA, Agatisa-Boyle B, et al. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ Res. 2015;116:448–455. doi: 10.1161/CIRCRESAHA.116.305360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Welzel TM, Graubard BI, Zeuzem S, El-Serag HB, Davila JA, McGlynn KA. Metabolic syndrome increases the risk of primary liver cancer in the United States: a study in the SEER-Medicare database. Hepatology. 2011;54:463–471. doi: 10.1002/hep.24397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yuan JM, Govindarajan S, Arakawa K, Yu MC. Synergism of alcohol, diabetes, and viral hepatitis on the risk of hepatocellular carcinoma in blacks and whites in the U.S. Cancer. 2004;101:1009–1017. doi: 10.1002/cncr.20427. [DOI] [PubMed] [Google Scholar]
- 23.Bae S, Ulrich CM, Neuhouser ML, Malysheva O, Bailey LB, Xiao L, et al. Plasma choline metabolites and colorectal cancer risk in the Women’s Health Initiative observational study. Cancer Res. 2014;74:7442–7452. doi: 10.1158/0008-5472.CAN-14-1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu X, Liu H, Yuan C, Zhang Y, Wang W, Hu S, et al. Preoperative serum TMAO level is a new prognostic marker for colorectal cancer. Biomark Med. 2017;11:443–447. doi: 10.2217/bmm-2016-0262. [DOI] [PubMed] [Google Scholar]
- 25.Xu R, Wang Q, Li L. A genome-wide systems analysis reveals strong link between colorectal cancer and trimethylamine N-oxide (TMAO), a gut microbial metabolite of dietary meat and fat. BMC Genomics. 2015;16(Suppl 7):S4. doi: 10.1186/1471-2164-16-S7-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen YM, Liu Y, Zhou RF, Chen XL, Wang C, Tan XY, et al. Associations of gut-flora-dependent metabolite trimethylamine-N-oxide, betaine and choline with non-alcoholic fatty liver disease in adults. Sci Rep. 2016;6:19076. doi: 10.1038/srep19076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.III ABB, Abrams TA, Ben-Josef E, Bloomston PM, Botha JF, Clary BM, Covey A. Hepatobiliary cancers: clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2009;7:350–391. doi: 10.6004/jnccn.2009.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med. 2006;23:469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 29.Holm PI, Ueland PM, Kvalheim G, Lien EA. Determination of choline, betaine, and dimethylglycine in plasma by a high-throughput method based on normal-phase chromatography-tandem mass spectrometry. Clin Chem. 2003;49:286–294. doi: 10.1373/49.2.286. [DOI] [PubMed] [Google Scholar]
- 30.Zhu W, Gregory JC, Org E, Buffa JA, Gupta N, Wang Z, et al. Gut microbial metabolite TMAO enhances platelet Hyperreactivity and thrombosis risk. Cell. 2016;165:111–124. doi: 10.1016/j.cell.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ufnal M, Jazwiec R, Dadlez M, Drapala A, Sikora M, Skrzypecki J. Trimethylamine-N-oxide: a carnitine-derived metabolite that prolongs the hypertensive effect of angiotensin II in rats. Can J Cardiol. 2014;30:1700–1705. doi: 10.1016/j.cjca.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 32.Oellgaard J, Winther SA, Hansen TS, Rossing P, von Scholten BJ. Trimethylamine N-oxide (TMAO) as a new potential therapeutic target for insulin resistance and Cancer. Curr Pharm Des. 2017;23:3699–3712. doi: 10.2174/1381612823666170622095324. [DOI] [PubMed] [Google Scholar]
- 33.Mondul AM, Moore SC, Weinstein SJ, Karoly ED, Sampson JN, Albanes D. Metabolomic analysis of prostate cancer risk in a prospective cohort: the alpha-tocolpherol, beta-carotene cancer prevention (ATBC) study. Int J Cancer. 2015;137:2124–2132. doi: 10.1002/ijc.29576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guertin KA, Li XS, Graubard BI, Albanes D, Weinstein SJ, Goedert JJ, et al. Serum trimethylamine N-oxide, carnitine, choline, and betaine in relation to colorectal Cancer risk in the alpha tocopherol, Beta carotene Cancer prevention study. Cancer Epidemiol Biomark Prev. 2017;26:945–952. doi: 10.1158/1055-9965.EPI-16-0948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu LX, Schwabe RF. The gut microbiome and liver cancer: mechanisms and clinical translation. Nat Rev Gastroenterol Hepatol. 2017;14:527–539. doi: 10.1038/nrgastro.2017.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Engen PA, Green SJ, Voigt RM, Forsyth CB, Keshavarzian A. The gastrointestinal microbiome: alcohol effects on the composition of intestinal microbiota. Alcohol Res. 2015;37:223–236. [PMC free article] [PubMed] [Google Scholar]
- 37.Savin Z, Kivity S, Yonath H, Yehuda S. Smoking and the intestinal microbiome. Arch Microbiol. 2018;200:677–684. doi: 10.1007/s00203-018-1506-2. [DOI] [PubMed] [Google Scholar]
- 38.Wang J, Wang Y, Zhang X, Liu J, Zhang Q, Zhao Y, et al. Gut microbial Dysbiosis is associated with altered hepatic functions and serum metabolites in chronic hepatitis B patients. Front Microbiol. 2017;8:2222. doi: 10.3389/fmicb.2017.02222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang Joyce, Butler Lesley, Midttun Øivind, Wang Renwei, Jin Aizhen, Gao Yu-Tang, Ueland Per, Koh Woon-Puay, Yuan Jian-Min. Abstract 2273: Serum choline, methionine, betaine, dimethylglycine, and trimethylamine-N-oxide in relation to pancreatic cancer risk in two nested case-control studies in Asian populations. Cancer Research. 2017;77(13 Supplement):2273–2273. doi: 10.1158/1538-7445.AM2017-2273. [DOI] [Google Scholar]
- 40.Zeng FF, Xu CH, Liu YT, Fan YY, Lin XL, Lu YK, et al. Choline and betaine intakes are associated with reduced risk of nasopharyngeal carcinoma in adults: a case-control study. Br J Cancer. 2014;110:808–816. doi: 10.1038/bjc.2013.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nitter M, Norgard B, de Vogel S, Eussen SJ, Meyer K, Ulvik A, et al. Plasma methionine, choline, betaine, and dimethylglycine in relation to colorectal cancer risk in the European prospective investigation into Cancer and nutrition (EPIC) Ann Oncol. 2014;25:1609–1615. doi: 10.1093/annonc/mdu185. [DOI] [PubMed] [Google Scholar]
- 42.Lu MS, Fang YJ, Pan ZZ, Zhong X, Zheng MC, Chen YM, Zhang CX. Choline and betaine intake and colorectal cancer risk in Chinese population: a case-control study. PLoS One. 2015;10:e0118661. doi: 10.1371/journal.pone.0118661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Du YF, Luo WP, Lin FY, Lian ZQ, Mo XF, Yan B, et al. Dietary choline and betaine intake, choline-metabolising genetic polymorphisms and breast cancer risk: a case-control study in China. Br J Nutr. 2016;116:961–968. doi: 10.1017/S0007114516002956. [DOI] [PubMed] [Google Scholar]
- 44.Pogribny IP, James SJ, Beland FA. Molecular alterations in hepatocarcinogenesis induced by dietary methyl deficiency. Mol Nutr Food Res. 2012;56:116–125. doi: 10.1002/mnfr.201100524. [DOI] [PubMed] [Google Scholar]
- 45.Ikawa-Yoshida A, Matsuo S, Kato A, Ohmori Y, Higashida A, Kaneko E, Matsumoto M. Hepatocellular carcinoma in a mouse model fed a choline-deficient, L-amino acid-defined, high-fat diet. Int J Exp Pathol. 2017;98:221–233. doi: 10.1111/iep.12240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to privacy protection of the participants but are available from the corresponding author on reasonable request.