Abstract
Background
The diagnosis of metastasis by sentinel lymph node biopsy (SLNB) in early breast cancer surgery provides an accurate view of the state of metastases to the axillary lymph nodes, and it has now become the standard procedure. In the present study, whether omission of axillary lymph node dissection (ALND) after neoadjuvant chemotherapy (NAC) is possible by evaluation of tumor-infiltrating lymphocytes (TILs) before NAC in cases without metastasis on diagnostic imaging, but with metastasis on SLNB, was retrospectively investigated.
Methods
A total of 91 patients with resectable, early-stage breast cancer, diagnosed as cT1–2, N0, M0, underwent SLNB and were treated with NAC. A semi-quantitative evaluation of lymphocytes infiltrating the peritumoral stroma as TILs in biopsy specimens of primary tumors prior to treatment was conducted.
Results
In cases with a low number of TILs, estrogen receptor expression was significantly higher (p = 0.044), and human epidermal growth factor receptor 2 (HER2) expression was significantly lower than in other cases (p = 0.019). The number of TILs was significantly lower in cases in which the intrinsic subtype was hormone receptor-positive breast cancer (HRBC) (p = 0.044). Metastasis to axillary lymph nodes was significantly more common in HER2-negative cases and cases with a low number of TILs (p = 0.019, p = 0.005, respectively).
Conclusions
Even if macrometastases are found on SLNB in cN0 patients, it appears that ALND could be avoided after NAC in cases with a good immune tumor microenvironment of the primary tumor.
Electronic supplementary material
The online version of this article (10.1186/s12967-018-1692-3) contains supplementary material, which is available to authorized users.
Keywords: Sentinel lymph node biopsy, Breast cancer, Microenvironment, Neoadjuvant chemotherapy, Tumor-infiltrating lymphocytes
Background
The diagnosis of metastasis by sentinel lymph node biopsy (SLNB) in early breast cancer surgery (BCS) provides an accurate view of the state of metastasis to the axillary lymph nodes, and it has now become the standard procedure [1–5]. However, in cases requiring neoadjuvant chemotherapy (NAC), it has not yet been established whether SLNB should be done before or after NAC. Performing SLNB after NAC, that is, during surgery, means that there is only one surgery, which reduces the burden on patients, but there is an increased chance of false-negative results. Therefore, our institute performs SLNB before NAC, and then NAC is given based on the histologic diagnosis, and BCS is finally performed [6]. Several reports recommend this method [7–10]. In this method, accurate pathological diagnosis can be performed before NAC, while unnecessary axillary lymph node dissection (ALND) can be avoided if there is no metastasis to axillary lymph nodes. However, if the axillary lymph node metastasis disappears following NAC, unnecessary ALND might be performed.
The immune tumor microenvironment (iTME) in cancer is currently thought to be involved in many antitumor treatment effects, and the presence of tumor-infiltrating lymphocytes (TILs) has been shown to be a useful indicator to monitor [11–13]. Similarly, TILs could be useful for predicting the effect of NAC in breast cancer [14]. However, few reports have examined the use of TILs as biomarkers in clinical practice.
In the present study, we hypothesized that ALND after NAC can be avoided by evaluation of the iTME before NAC. Then, whether omission of ALND after NAC is possible by evaluation of TILs before NAC in cases without metastasis on diagnostic imaging, but with metastasis on SLNB, was retrospectively investigated.
Methods
Patient background
A total of 91 patients with resectable, early-stage breast cancer, diagnosed as cT1–2, N0, M0, underwent SLNB and were treated with NAC at Osaka City University Hospital from August 2009 to July 2016. TNM staging was evaluated according to the seventh edition of the American Committee on Cancer staging manual [15]. Breast cancer was diagnosed histologically by core needle biopsy (CNB) or vacuum-assisted biopsy (VAB) and staged with systemic imaging studies, including computed tomography (CT), ultrasonography (US), and bone scintigraphy. Depending on the immunohistochemical expressions of estrogen receptor (ER), progesterone receptor (PgR), human epidermal growth factor receptor 2 (HER2), and Ki67, the breast cancers were categorized into the following immunophenotypes: luminal A (ER+ and/or PgR+, HER2−, Ki67-low); luminal B (ER+ and/or PgR+, HER2+; ER+ and/or PgR+, HER2−, Ki67-high); HER2BC (HER2-enriched breast cancer; ER−, PgR−, and HER2+); and TNBC (triple-negative breast cancer; negative for ER, PgR, and HER2) [16]. In this study, luminal A and luminal B types were considered hormone receptor-positive breast cancer (HRBC). Sentinel lymph nodes (SNs) were identified by a combination of radioisotope and dye methods, for which the detailed methods have been previously reported [6, 17, 18]. Histopathological diagnosis of lymph node metastasis was made by slicing the entire SN into 2-mm-thick sections [19, 20]. A positive diagnosis of SN metastasis as an indication for axillary clearance was defined as macrometastasis in the SN (macrometastasis: tumor diameter > 2 mm). Micrometastasis and isolated tumor cells were considered negative indications for axillary clearance (micrometastasis: tumor diameter > 0.2 mm, ≤ 2 mm or < 200 tumor cells; isolated tumor cells: tumor diameter < 0.2 mm or < 200 tumor cells) [21]. NAC was generally recommended according to the intrinsic subtype of the primary tumor determined from the biopsy sample. ALND was followed by BCS within 4 weeks after the termination of NAC in SN-positive patients, and BCS without ALND was performed in SN-negative patients.
NAC consisted of four courses of FEC100 (500 mg/m2 fluorouracil, 100 mg/m2 epirubicin, and 500 mg/m2 cyclophosphamide) every 3 weeks, followed by 12 courses of 80 mg/m2 paclitaxel administered weekly. Patients with HER2BC were additionally given weekly (2 mg/kg) or tri-weekly (6 mg/kg) trastuzumab during paclitaxel treatment [22–24]. Therapeutic anti-tumor effects were evaluated according to the Response Evaluation Criteria in Solid Tumors [25]. Patients underwent mastectomy or breast-conserving surgery following NAC [26]. In all cases with SN macrometastasis, ALND was performed. The pathological effects of chemotherapy were evaluated in primary tumor resected at the time of BCS. A pathological complete response (pCR) was defined as the complete disappearance of the invasive components of the lesion with or without intraductal components, including within the lymph nodes, according to the National Surgical Adjuvant Breast and Bowel Project B-18 protocol [27].
Histopathological evaluation of TIL status
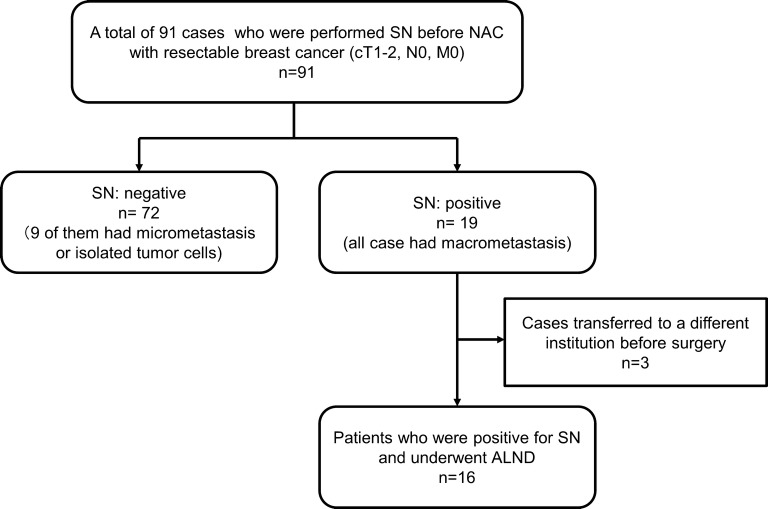
TILs were evaluated on biopsy specimens (CNB or VAB) by measuring the percentage of area occupied by lymphocytes on the hematoxylin and eosin (H&E)-stained tumor section at the time of breast cancer diagnosis [28]. The area of the stroma region with lymphoplasmacytic infiltration was > 50%, > 10–50%, ≤ 10%, or absent, and the corresponding score assigned was 3, 2, 1, or 0, respectively [29] (Fig. 1). TIL status was evaluated as “high” with scores of 2 or more, and “low” with scores of 1 and 0, according to a previous report [29]. The cut-off value of TILs was calculated by receiver operating characteristic (ROC) curve analysis, and the area under the curve (AUC) was 0.719, with a specificity of 0.917 and a sensitivity of 0.750 (Additional file 1: Fig. S1). Histopathological diagnosis was performed by two breast cancer pathologists in blinded fashion.
Fig. 1.
Histopathological evaluation of TILs. TILs were evaluated on biopsy specimens by measuring the percentage of area occupied by lymphocytes on the hematoxylin and eosin (H&E)-stained tumor section at the time of breast cancer diagnosis. The area of the stroma region with lymphoplasmacytic infiltration was > 50%, > 10–50%, ≤ 10%, or absent, and the corresponding score assigned was 3, 2, 1, or 0, respectively (A–D respectively)
Statistical analysis
Statistical analysis was conducted using the JMP software package (SAS, Tokyo, Japan). The relationship between each factor was examined using the Chi squared test (or Fisher’s exact test when necessary). A p value < 0.05 was considered significant.
Ethics statement
This research was conducted at Osaka City University Hospital, Osaka, Japan. Sufficient explanation was provided, and written, informed consent was obtained from all study subjects for their involvement in this study and for the storage and use of their data. This study conformed to the provisions of the Declaration of Helsinki (2013). The study protocol was approved by the Ethics Committee of the Osaka City University (approval number #926).
Results
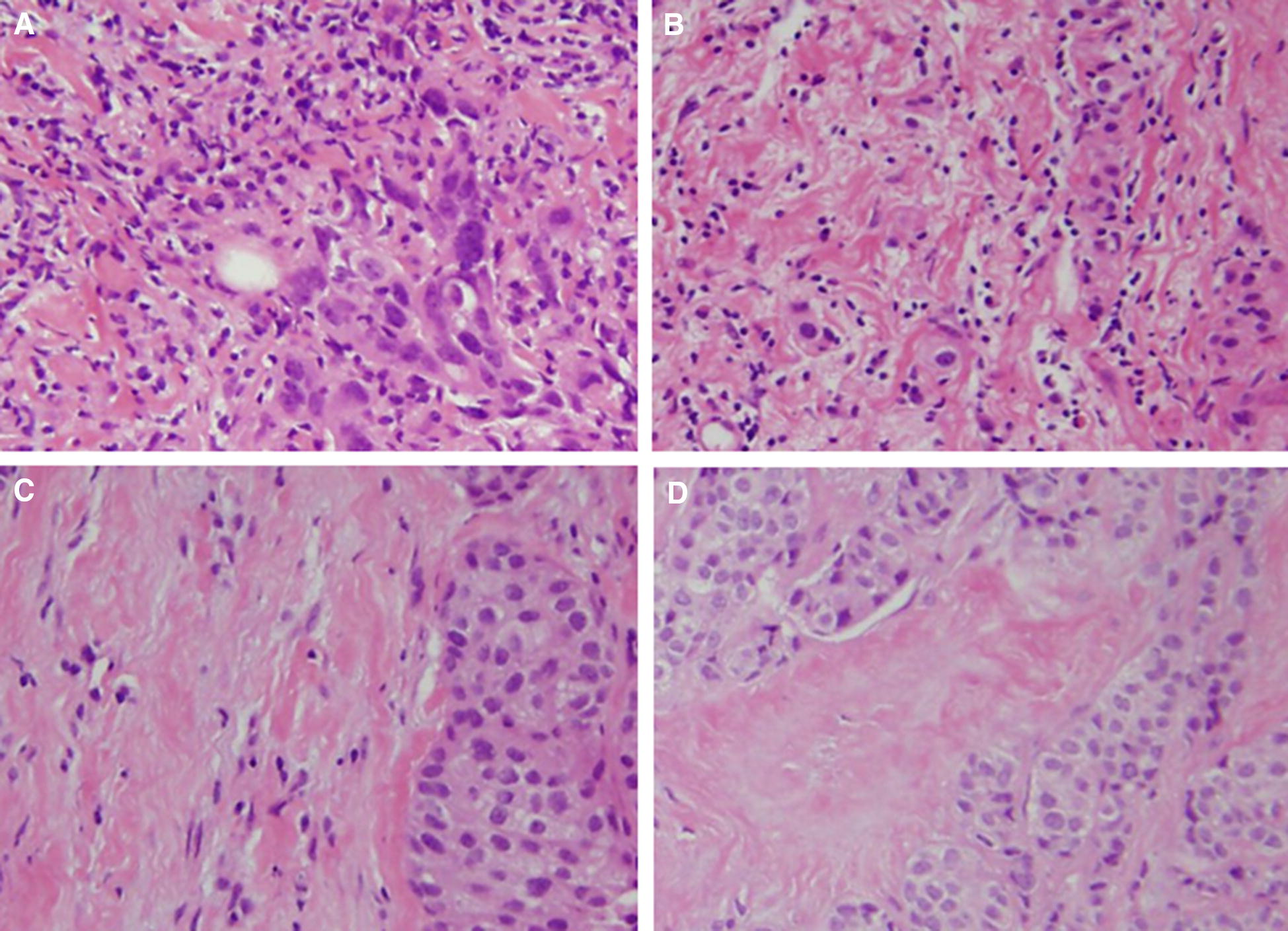
Statistical data of cases that underwent SLNB before NAC and ALND at the time of breast cancer surgery
Nineteen (20.9%) of 91 patients who underwent SLNB before NAC had metastasis, and three of them were transferred to a different institution before surgery. Thus, 16 cases underwent ALND at the time of BCS (Fig. 2). All patients were women, with a median age of 47 years (range 28–72 years). The median tumor size was 25.1 mm (range 18.9–42.0 mm). Regarding intrinsic subtypes, nine cases (56.3%) were HRBC, four (25.0%) were HER2BC, and three (18.7%) were TNBC. Twelve cases (75.0%) had a high number of TILs, and four cases (25.0%) had a low number of TILs at diagnosis of breast cancer. In 13 cases (81.3%), multiple SNs were removed at the time of SLNB. In 12 cases (75.0%), metastasis was found in only one of the SNs. The median metastatic diameter was 3397 µm (range 2108–7281 µm). All cases responded to NAC, and the pCR rate was 31.2%. There were four cases (25.0%) in which metastasis was observed in the axillary lymph node on ALND (Table 1).
Fig. 2.
Consort diagram. A total of 91 patients with resectable, early-stage breast cancer, diagnosed as cT1–2, N0, M0, underwent sentinel lymph node biopsy and were treated with NAC. Nineteen (20.9%) of 91 patients who underwent sentinel lymph node biopsy before NAC had metastasis, and three of them were transferred to a different institution before surgery. Thus, 16 cases underwent axillary lymph node dissection at the time of breast cancer surgery
Table 1.
Statistical data of 16 patients who underwent SNLB before NAC and ALND at the time of breast cancer surgery
| Parameters (n = 16) | Number of patients (%) |
|---|---|
| Age (years old) | 47 (28–72) |
| Tumor size (mm) | 25.1 (18.9–42.0) |
| Estrogen receptor | |
| Negative/positive | 7 (43.8%)/9 (56.2%) |
| Progesterone receptor | |
| Negative/positive | 10 (62.5%)/6 (37.5%) |
| HER2 | |
| Negative/positive | 8 (50.0%)/8 (50.0%) |
| Ki67 | |
| Negative/positive | 4 (25.0%)/12 (75.0%) |
| Intrinsic subtype | |
| HRBC/HER2BC/TNBC | 9 (56.3%)/4 (25.0%)/3 (18.7%) |
| Tumor-infiltrating lymphocytes | |
| Low/high | 4 (25.0%)/12 (75.0%) |
| Number of excised sentinel lymph nodes | |
| 1/2/3 | 3 (18.7%)/6 (37.5%)/7 (43.8%) |
| Number of sentinel lymph nodes with metastasis | |
| 1/2/3 | 12 (75.0%)/1 (6.3%)/3 (18.7%) |
| Size of sentinel lymph node itself (mm) | 12.5 (9.1–26.3) |
| Size of metastatic lesion (μm) | 3397 (2108–7281) |
| Clinical response | |
| cPR/cCR | 14 (87.5%)/2 (12.5%) |
| Pathological complete response | |
| pCR/non-pCR | 5 (31.2%)/11 (68.8%) |
| Number of lymph node dissection | 9 (3–24) |
| Lymph node metastasis | |
| Negative/positive | 12 (75.0%)/4 (25.0%) |
| Number of lymph node metastasis | |
| 1/2/6 | 2 (12.5%)/1 (6.3%)/1 (6.3%) |
SLNB sentinel lymph node biopsy, NAC neoadjuvant chemotherapy, ALND axillary lymph node dissection, BCS breast cancer surgery, HER2 human epidermal growth factor receptor 2, HRBC hormone receptor-positive breast cancer, HER2BC HER2-enriched breast cancer, TNBC triple negative breast cancer, cPR clinical partial response, cCR clinical complete response, pCR pathological complete response
Correlations between clinicopathological features and number of TILs
In cases with a low number of TILs, ER expression was significantly higher (p = 0.044), and HER2 expression was significantly lower than in other cases (p = 0.019). The number of TILs was significantly lower in cases in which the intrinsic subtype was HRBC (p = 0.044). There was no correlation between other clinicopathological features and the number of TILs (Table 2).
Table 2.
Correlations between clinicopathological features and the number of TILs
| Parameters | TILs | p value | |
|---|---|---|---|
| High (n = 12) | Low (n = 4) | ||
| Age | |||
| ≤ 47 | 7 (58.3%) | 1 (25.0%) | |
| > 47 | 5 (41.7%) | 3 (75.0%) | 0.278 |
| Tumor size | |||
| ≤ 25 | 6 (50.0%) | 2 (50.0%) | |
| > 25 | 6 (50.0%) | 2 (50.0%) | 1.000 |
| Estrogen receptor | |||
| Negative | 7 (58.3%) | 0 (0.0%) | |
| Positive | 5 (41.7%) | 4 (100.0%) | 0.044 |
| Progesterone receptor | |||
| Negative | 9 (75.0%) | 1 (25.0%) | |
| Positive | 3 (25.0%) | 3 (75.0%) | 0.082 |
| HER2 | |||
| Negative | 4 (33.3%) | 4 (100.0%) | |
| Positive | 8 (66.7%) | 0 (0.0%) | 0.019 |
| Ki67 | |||
| Negative | 2 (16.7%) | 2 (50.0%) | |
| Positive | 10 (83.3%) | 2 (50.0%) | 0.207 |
| Intrinsic subtype HRBC | |||
| Non-HRBC | 7 (58.3%) | 0 (0.0%) | |
| HRBC | 5 (41.7%) | 4 (100.0%) | 0.044 |
| Intrinsic subtype HER2BC | |||
| Non-HER2BC | 8 (66.7%) | 4 (100.0%) | |
| HER2BC | 4 (33.3%) | 0 (0.0%) | 0.207 |
| Intrinsic subtype TNBC | |||
| Non-TNBC | 9 (75.0%) | 4 (100.0%) | |
| TNBC | 3 (25.0%) | 0 (0.0%) | 0.298 |
| Number of sentinel lymph nodes with metastasis | |||
| 1, 2 | 10 (83.3%) | 3 (75.0%) | |
| 3 | 2 (16.7%) | 1 (25.0%) | 0.734 |
| Size of sentinel lymph node itself (mm) | |||
| ≤ 12.5 | 6 (50.0%) | 2 (50.0%) | |
| > 12.5 | 6 (50.0%) | 2 (50.0%) | 1.000 |
| Size of metastatic lesion | |||
| ≤ 3400 | 5 (41.7%) | 3 (75.0%) | |
| > 3400 | 7 (58.3%) | 1 (25.0%) | 0.278 |
| Clinical response | |||
| cPR | 10 (83.3%) | 4 (100.0%) | |
| cCR | 2 (16.7%) | 0 (0.0%) | 0.417 |
| Pathological complete response | |||
| Non-pCR | 7 (58.3%) | 4 (100.0%) | |
| pCR | 5 (41.7%) | 0 (0.0%) | 0.136 |
TILs tumor-infiltrating lymphocytes, HER2 human epidermal growth factor receptor 2, HRBC hormone receptor-positive breast cancer, HER2BC HER2-enriched breast cancer, TNBC triple negative breast cancer, cPR clinical partial response, cCR clinical complete response, pCR pathological complete response
Correlations between clinicopathological features and metastasis to axillary lymph nodes
Metastasis to axillary lymph nodes was significantly more common in HER2-negative cases and cases with a low number of TILs (p = 0.019, p = 0.005, respectively). However, no correlations were found between other clinicopathological features and axillary lymph node metastasis (Table 3).
Table 3.
Correlations between clinicopathological features and axillary lymph node metastasis
| Parameters | Axillary lymph node | p value | |
|---|---|---|---|
| Negative (n = 12) | Positive (n = 4) | ||
| Age | |||
| ≤ 47 | 6 (50.0%) | 2 (50.0%) | |
| > 47 | 6 (50.0%) | 2 (50.0%) | 1.000 |
| Tumor size | |||
| ≤ 25 | 7 (58.3%) | 1 (25.0%) | |
| > 25 | 5 (41.7%) | 3 (75.0%) | 0.278 |
| Estrogen receptor | |||
| Negative | 6 (50.0%) | 1 (25.0%) | |
| Positive | 6 (50.0%) | 3 (75.0%) | 0.417 |
| Progesterone receptor | |||
| Negative | 8 (66.7%) | 2 (50.0%) | |
| Positive | 4 (33.3%) | 2 (50.0%) | 0.582 |
| HER2 | |||
| Negative | 4 (33.3%) | 4 (100.0%) | |
| Positive | 8 (66.7%) | 0 (0.0%) | 0.019 |
| Ki67 | |||
| Negative | 3 (25.0%) | 1 (25.0%) | |
| Positive | 9 (75.0%) | 3 (75.0%) | 1.000 |
| Intrinsic subtype HRBC | |||
| Non-HRBC | 6 (50.0%) | 1 (25.0%) | |
| HRBC | 6 (50.0%) | 3 (75.0%) | 0.417 |
| Intrinsic subtype HER2BC | |||
| Non-HER2BC | 8 (66.7%) | 4 (100.0%) | |
| HER2BC | 4 (33.3%) | 0 (0.0%) | 0.207 |
| Intrinsic subtype TNBC | |||
| Non-TNBC | 10 (83.3%) | 3 (75.0%) | |
| TNBC | 2 (16.7%) | 1 (25.0%) | 0.734 |
| TILs | |||
| Low | 1 (8.3%) | 3 (75.0%) | |
| High | 11 (91.7%) | 1 (25.0%) | 0.005 |
| Number of sentinel lymph nodes with metastasis | |||
| 1, 2 | 11 (91.7%) | 2 (50.0%) | |
| 3 | 1 (8.3%) | 2 (50.0%) | 0.071 |
| Size of sentinel lymph node itself (mm) | |||
| ≤ 12.5 | 6 (50.0%) | 2 (50.0%) | |
| > 12.5 | 6 (50.0%) | 2 (50.0%) | 1.000 |
| Size of metastatic lesion | |||
| ≤ 3400 | 6 (50.0%) | 2 (50.0%) | |
| > 3400 | 6 (50.0%) | 2 (50.0%) | 1.000 |
| Clinical response | |||
| cPR | 10 (83.3%) | 4 (100.0%) | |
| cCR | 2 (16.7%) | 0 (0.0%) | 0.417 |
| Pathological complete response | |||
| Non-pCR | 8 (66.7%) | 3 (75.0%) | |
| pCR | 4 (33.3%) | 1 (25.0%) | 0.774 |
TILs tumor-infiltrating lymphocytes, HER2 human epidermal growth factor receptor 2, HRBC hormone receptor-positive breast cancer, HER2BC HER2-enriched breast cancer, TNBC triple negative breast cancer, cPR clinical partial response, cCR clinical complete response, pCR pathological complete response
Discussion
Metastasis to axillary lymph nodes affects prognosis, so evaluation of axillary lymph nodes is important [30]. Currently, it is recognized clinically that SLNB can accurately diagnose the presence or absence of axillary lymph node metastasis in early-stage breast cancer with no axillary lymph node metastasis [31]. Therefore, if the SN is negative, it is standard practice to omit ALND. On the other hand, NAC is a standard initial treatment not only in locally advanced breast cancer, but also early-stage breast cancer, because it improves the breast conservation rate by downstaging [22, 23, 27]. However, the timing of SLNB in patients undergoing NAC has been debated extensively [32–34]. By performing SLNB after NAC, the state of metastasis to the axillary lymph node at the time of BCS can be known, and the axillary preservation rate is increased; however, the false-negative rate increases [35, 36]. This is caused by lymph flow changes and lymph node scarring due to NAC. The false-negative rate is reported as 11–39% [32–34, 37]. Thus, some studies suggested that SLNB after NAC cannot predict the state of the axillary lymph nodes [38, 39]. Some studies recommend SLNB before NAC [7, 9, 10]. However, with this protocol, while the false-negative rates can be reduced by evaluation with H&E staining, unnecessary lymph node dissection may be performed in cases that are downstaged by NAC. Overall, 20–40% of cN+ cases before NAC will downstage to cN0 after NAC [40, 41]. Evaluation of axillary lymph node metastasis after NAC is difficult in cN0 cases in which metastasis to SNs is observed on pathology.
The iTME in cancer is involved in many antitumor treatment effects [42]. The number of TILs is being established as a biomarker for therapeutic effect and prognosis [11–13]. There are reports that the number of TILs is related to the rate of pCR [14]. In breast cancer, the correlation between subtype and TILs was examined, and it is often reported that it is high in TNBC and HER2BC [43, 44]. In the examination of TILs and clinical factors in the present study, the number of TILs was significantly higher in ER-negative cases than in ER-positive cases, and higher in HER2-positive than in HER2-negative cases; that is, the present result was similar to the previous reports. In the high TILs group, a better therapeutic effect was observed, and remnants of metastases to the axillary lymph nodes were significantly decreased.
When the metastasis to the SN is 2 mm or less, there is little metastasis to lymph nodes that are not the SN, and there are no significant differences in disease-free survival and overall survival between the SLNB alone group and the SLNB with complete ALND group [21, 45–47]. However, if the metastasis is 2 mm or more, half of the patients have metastasis to non-sentinel lymph nodes, and there is a difference in prognosis. Although studies are being conducted to identify other new criteria, there are currently no clinically applicable ones [48]. Although methods for reducing the false-negative rate after NAC have also been studied, many of them require additional examinations or other treatment [49]. However, the present method only requires the examination of H&E-stained specimens, and does not require special examinations or other costly tests.
There are many reports on the scoring of TILs as prognostic factors and effect predictors. However, application to clinical practice has not been reported much. Although the present study is limited by its retrospective nature and the low number of cases studied, it does show the possibility of using TILs as a biomarker in the clinical setting. If this method were established clinically, the disadvantage of SLNB before NAC would be reduced, unnecessary surgery could be avoided, and it would be possible to reduce the burden on patients.
Conclusions
Even if macrometastases are found in the SN in cN0 patients, it appears that ALND could be avoided if the iTME is good.
Additional file
Additional file 1: Fig. S1. The cut-off value of TILs was calculated by receiver operating characteristic (ROC) curve analysis, and the area under the curve (AUC) was 0.719, with a specificity of 0.917 and a sensitivity of 0.750.
Authors’ contributions
All authors were involved in the preparation of this manuscript. K Takada collected the data and wrote the manuscript. SK, WG, YA, K Takahashi, and TT performed the surgeries and designed the study. K Takada, SK, and ST summarized the data and revised the manuscript. HF, KH, and MO made substantial contributions to study design, performed the surgeries, and revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank Yayoi Matsukiyo and Tomomi Okawa (Department of Surgical Oncology, Osaka City University Graduate School of Medicine) for helpful advice regarding data management.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Written, informed consent was obtained from all subjects. This research conformed to the provisions of the Declaration of Helsinki of 2013. All patients were informed of the investigational nature of this study and provided their written, informed consent. The study protocol was approved by the Ethics Committee of Osaka City University (#926).
Funding
This study was supported in part by Grants-in-Aid for Scientific Research (KAKENHI, Nos. 25461992, 26461957, and 17K10559) from the Ministry of Education, Science, Sports, Culture and Technology of Japan.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- SLNB
sentinel lymph node biopsy
- BCS
breast cancer surgery
- ALND
axillary lymph node dissection
- NAC
neoadjuvant chemotherapy
- TILs
tumor-infiltrating lymphocytes
- ER
estrogen receptor
- HER2
human epidermal growth factor receptor 2
- HRBC
hormone receptor-positive breast cancer
- iTME
immune tumor microenvironment
- CNB
core needle biopsy
- VAB
vacuum-assisted biopsy
- CT
computed tomography
- US
ultrasonography
- SN
sentinel lymph node
- pCR
pathological complete response
- H&E
hematoxylin and eosin
Contributor Information
Koji Takada, Email: taka.cl22.kou.sp@gmail.com.
Shinichiro Kashiwagi, Phone: (+81) 6-6645-3838, Email: spqv9ke9@view.ocn.ne.jp.
Wataru Goto, Email: saraikazemaru@gmail.com.
Yuka Asano, Email: asnyk0325@yahoo.co.jp.
Katsuyuki Takahashi, Email: k.taka@med.osaka-cu.ac.jp.
Hisakazu Fujita, Email: hifujita@med.osaka-cu.ac.jp.
Tsutomu Takashima, Email: tsutomu-@rd5.so-net.ne.jp.
Shuhei Tomita, Email: tomita.shuhei@med.osaka-cu.ac.jp.
Kosei Hirakawa, Email: hirakawa@med.osaka-cu.ac.jp.
Masaichi Ohira, Email: masaichi@med.osaka-cu.ac.jp.
References
- 1.Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, Aguilar M, Marubini E. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347(16):1227–1232. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 2.Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–1241. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz GF, Giuliano AE, Veronesi U, Consensus Conference C Proceedings of the consensus conference on the role of sentinel lymph node biopsy in carcinoma of the breast April 19 to 22, 2001, Philadelphia. Hum Pathol. 2002;33(6):579–589. doi: 10.1053/hupa.2002.124117. [DOI] [PubMed] [Google Scholar]
- 4.Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, Intra M, Veronesi P, Robertson C, Maisonneuve P, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003;349(6):546–553. doi: 10.1056/NEJMoa012782. [DOI] [PubMed] [Google Scholar]
- 5.Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, Intra M, Veronesi P, Maisonneuve P, Gatti G, et al. Sentinel-lymph-node biopsy as a staging procedure in breast cancer: update of a randomised controlled study. Lancet Oncol. 2006;7(12):983–990. doi: 10.1016/S1470-2045(06)70947-0. [DOI] [PubMed] [Google Scholar]
- 6.Kashiwagi S, Onoda N, Asano Y, Kurata K, Noda S, Kawajiri H, Takashima T, Ohsawa M, Kitagawa S, Hirakawa K. Ambulatory sentinel lymph node biopsy preceding neoadjuvant therapy in patients with operable breast cancer: a preliminary study. World J Surg Oncol. 2015;13:53. doi: 10.1186/s12957-015-0471-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breslin TM, Cohen L, Sahin A, Fleming JB, Kuerer HM, Newman LA, Delpassand ES, House R, Ames FC, Feig BW, et al. Sentinel lymph node biopsy is accurate after neoadjuvant chemotherapy for breast cancer. J Clin Oncol. 2000;18(20):3480–3486. doi: 10.1200/JCO.2000.18.20.3480. [DOI] [PubMed] [Google Scholar]
- 8.Mamounas EP, Brown A, Anderson S, Smith R, Julian T, Miller B, Bear HD, Caldwell CB, Walker AP, Mikkelson WM, et al. Sentinel node biopsy after neoadjuvant chemotherapy in breast cancer: results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2005;23(12):2694–2702. doi: 10.1200/JCO.2005.05.188. [DOI] [PubMed] [Google Scholar]
- 9.Newman EA, Sabel MS, Nees AV, Schott A, Diehl KM, Cimmino VM, Chang AE, Kleer C, Hayes DF, Newman LA. Sentinel lymph node biopsy performed after neoadjuvant chemotherapy is accurate in patients with documented node-positive breast cancer at presentation. Ann Surg Oncol. 2007;14(10):2946–2952. doi: 10.1245/s10434-007-9403-y. [DOI] [PubMed] [Google Scholar]
- 10.Tausch C, Konstantiniuk P, Kugler F, Reitsamer R, Roka S, Postlberger S, Haid A, Austrian Sentinel Node Study G Sentinel lymph node biopsy after preoperative chemotherapy for breast cancer: findings from the Austrian Sentinel Node Study Group. Ann Surg Oncol. 2008;15(12):3378–3383. doi: 10.1245/s10434-008-0041-9. [DOI] [PubMed] [Google Scholar]
- 11.Zitvogel L, Kepp O, Kroemer G. Immune parameters affecting the efficacy of chemotherapeutic regimens. Nat Rev Clin Oncol. 2011;8(3):151–160. doi: 10.1038/nrclinonc.2010.223. [DOI] [PubMed] [Google Scholar]
- 12.Fridman WH, Pages F, Sautes-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12(4):298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 13.Couzin-Frankel J. Breakthrough of the year 2013. Cancer immunotherapy. Science. 2013;342(6165):1432–1433. doi: 10.1126/science.342.6165.1432. [DOI] [PubMed] [Google Scholar]
- 14.Denkert C, von Minckwitz G, Brase JC, Sinn BV, Gade S, Kronenwett R, Pfitzner BM, Salat C, Loi S, Schmitt WD, et al. Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol. 2015;33(9):983–991. doi: 10.1200/JCO.2014.58.1967. [DOI] [PubMed] [Google Scholar]
- 15.Greene FL, Sobin LH. A worldwide approach to the TNM staging system: collaborative efforts of the AJCC and UICC. J Surg Oncol. 2009;99(5):269–272. doi: 10.1002/jso.21237. [DOI] [PubMed] [Google Scholar]
- 16.Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ, Panel M. Strategies for subtypes–dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22(8):1736–1747. doi: 10.1093/annonc/mdr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kashiwagi S, Onoda N, Asano Y, Noda S, Kawajiri H, Takashima T, Ohsawa M, Kitagawa S, Hirakawa K. Adjunctive imprint cytology of core needle biopsy specimens improved diagnostic accuracy for breast cancer. Springerplus. 2013;2:372. doi: 10.1186/2193-1801-2-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McMasters KM, Tuttle TM, Carlson DJ, Brown CM, Noyes RD, Glaser RL, Vennekotter DJ, Turk PS, Tate PS, Sardi A, et al. Sentinel lymph node biopsy for breast cancer: a suitable alternative to routine axillary dissection in multi-institutional practice when optimal technique is used. J Clin Oncol. 2000;18(13):2560–2566. doi: 10.1200/JCO.2000.18.13.2560. [DOI] [PubMed] [Google Scholar]
- 19.Lee A, Krishnamurthy S, Sahin A, Symmans WF, Hunt K, Sneige N. Intraoperative touch imprint of sentinel lymph nodes in breast carcinoma patients. Cancer. 2002;96(4):225–231. doi: 10.1002/cncr.10721. [DOI] [PubMed] [Google Scholar]
- 20.Khanna R, Bhadani S, Khanna S, Pandey M, Kumar M. Touch imprint cytology evaluation of sentinel lymph node in breast cancer. World J Surg. 2011;35(6):1254–1259. doi: 10.1007/s00268-011-1094-7. [DOI] [PubMed] [Google Scholar]
- 21.Houvenaeghel G, Nos C, Mignotte H, Classe JM, Giard S, Rouanet P, Lorca FP, Jacquemier J, Bardou VJ, Groupe des Chirurgiens de la Federation des Centres de Lutte Contre le C Micrometastases in sentinel lymph node in a multicentric study: predictive factors of nonsentinel lymph node involvement–Groupe des Chirurgiens de la Federation des Centres de Lutte Contre le Cancer. J Clin Oncol. 2006;24(12):1814–1822. doi: 10.1200/JCO.2005.03.3225. [DOI] [PubMed] [Google Scholar]
- 22.Mauri D, Pavlidis N, Ioannidis JP. Neoadjuvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. J Natl Cancer Inst. 2005;97(3):188–194. doi: 10.1093/jnci/dji021. [DOI] [PubMed] [Google Scholar]
- 23.Mieog JS, van der Hage JA, van de Velde CJ. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007;2:CD005002. doi: 10.1002/14651858.CD005002.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kawajiri H, Takashima T, Onoda N, Kashiwagi S, Noda S, Ishikawa T, Wakasa K, Hirakawa K. Efficacy and feasibility of neoadjuvant chemotherapy with FEC 100 followed by weekly paclitaxel for operable breast cancer. Oncol Lett. 2012;4(4):612–616. doi: 10.3892/ol.2012.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 26.Kashiwagi S, Onoda N, Asano Y, Kurata K, Morisaki T, Noda S, Kawajiri H, Takashima T, Hirakawa K. Partial mastectomy using manual blunt dissection (MBD) in early breast cancer. BMC Surg. 2015;15:117. doi: 10.1186/s12893-015-0102-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;30:96–102. doi: 10.1093/oxfordjournals.jncimonographs.a003469. [DOI] [PubMed] [Google Scholar]
- 28.Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL, Penault-Llorca F, et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol. 2015;26(2):259–271. doi: 10.1093/annonc/mdu450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kashiwagi S, Asano Y, Goto W, Takada K, Takahashi K, Noda S, Takashima T, Onoda N, Tomita S, Ohsawa M, et al. Use of Tumor-infiltrating lymphocytes (TILs) to predict the treatment response to eribulin chemotherapy in breast cancer. PLoS ONE. 2017;12(2):e0170634. doi: 10.1371/journal.pone.0170634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orr RK. The impact of prophylactic axillary node dissection on breast cancer survival—a Bayesian meta-analysis. Ann Surg Oncol. 1999;6(1):109–116. doi: 10.1007/s10434-999-0109-1. [DOI] [PubMed] [Google Scholar]
- 31.Lyman GH, Temin S, Edge SB, Newman LA, Turner RR, Weaver DL, Benson AB, 3rd, Bosserman LD, Burstein HJ, Cody H, 3rd, et al. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2014;32(13):1365–1383. doi: 10.1200/JCO.2013.54.1177. [DOI] [PubMed] [Google Scholar]
- 32.Xing Y, Foy M, Cox DD, Kuerer HM, Hunt KK, Cormier JN. Meta-analysis of sentinel lymph node biopsy after preoperative chemotherapy in patients with breast cancer. Br J Surg. 2006;93(5):539–546. doi: 10.1002/bjs.5209. [DOI] [PubMed] [Google Scholar]
- 33.Kelly AM, Dwamena B, Cronin P, Carlos RC. Breast cancer sentinel node identification and classification after neoadjuvant chemotherapy—systematic review and meta analysis. Acad Radiol. 2009;16(5):551–563. doi: 10.1016/j.acra.2009.01.026. [DOI] [PubMed] [Google Scholar]
- 34.van Deurzen CH, Vriens BE, Tjan-Heijnen VC, van der Wall E, Albregts M, van Hilligersberg R, Monninkhof EM, van Diest PJ. Accuracy of sentinel node biopsy after neoadjuvant chemotherapy in breast cancer patients: a systematic review. Eur J Cancer. 2009;45(18):3124–3130. doi: 10.1016/j.ejca.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 35.Lee S, Kim EY, Kang SH, Kim SW, Kim SK, Kang KW, Kwon Y, Shin KH, Kang HS, Ro J, et al. Sentinel node identification rate, but not accuracy, is significantly decreased after pre-operative chemotherapy in axillary node-positive breast cancer patients. Breast Cancer Res Treat. 2007;102(3):283–288. doi: 10.1007/s10549-006-9330-9. [DOI] [PubMed] [Google Scholar]
- 36.Shen J, Gilcrease MZ, Babiera GV, Ross MI, Meric-Bernstam F, Feig BW, Kuerer HM, Francis A, Ames FC, Hunt KK. Feasibility and accuracy of sentinel lymph node biopsy after preoperative chemotherapy in breast cancer patients with documented axillary metastases. Cancer. 2007;109(7):1255–1263. doi: 10.1002/cncr.22540. [DOI] [PubMed] [Google Scholar]
- 37.Rubio IT. Sentinel lymph node biopsy after neoadjuvant treatment in breast cancer: work in progress. Eur J Surg Oncol. 2016;42(3):326–332. doi: 10.1016/j.ejso.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 38.Boughey JC, Suman VJ, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, Leitch AM, Kuerer HM, Bowling M, Flippo-Morton TS, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310(14):1455–1461. doi: 10.1001/jama.2013.278932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G, Lebeau A, Liedtke C, von Minckwitz G, Nekljudova V, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol. 2013;14(7):609–618. doi: 10.1016/S1470-2045(13)70166-9. [DOI] [PubMed] [Google Scholar]
- 40.Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, Cruz AB, Jr, Fisher ER, Wickerham DL, Wolmark N, et al. Effect of preoperative chemotherapy on local–regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15(7):2483–2493. doi: 10.1200/JCO.1997.15.7.2483. [DOI] [PubMed] [Google Scholar]
- 41.Kuerer HM, Sahin AA, Hunt KK, Newman LA, Breslin TM, Ames FC, Ross MI, Buzdar AU, Hortobagyi GN, Singletary SE. Incidence and impact of documented eradication of breast cancer axillary lymph node metastases before surgery in patients treated with neoadjuvant chemotherapy. Ann Surg. 1999;230(1):72–78. doi: 10.1097/00000658-199907000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 43.Ohtani H, Mori-Shiraishi K, Nakajima M, Ueki H. Defining lymphocyte-predominant breast cancer by the proportion of lymphocyte-rich stroma and its significance in routine histopathological diagnosis. Pathol Int. 2015;65(12):644–651. doi: 10.1111/pin.12355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stanton SE, Adams S, Disis ML. Variation in the incidence and magnitude of tumor-infiltrating lymphocytes in breast cancer subtypes: a systematic review. JAMA Oncol. 2016;2(10):1354–1360. doi: 10.1001/jamaoncol.2016.1061. [DOI] [PubMed] [Google Scholar]
- 45.Dabbs DJ, Fung M, Landsittel D, McManus K, Johnson R. Sentinel lymph node micrometastasis as a predictor of axillary tumor burden. Breast J. 2004;10(2):101–105. doi: 10.1111/j.1075-122X.2004.21280.x. [DOI] [PubMed] [Google Scholar]
- 46.Yi M, Giordano SH, Meric-Bernstam F, Mittendorf EA, Kuerer HM, Hwang RF, Bedrosian I, Rourke L. Hunt KK: Trends in and outcomes from sentinel lymph node biopsy (SLNB) alone vs. SLNB with axillary lymph node dissection for node-positive breast cancer patients: experience from the SEER database. Ann Surg Oncol. 2010;17(Suppl 3):343–351. doi: 10.1245/s10434-010-1253-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Galimberti V, Cole BF, Zurrida S, Viale G, Luini A, Veronesi P, Baratella P, Chifu C, Sargenti M, Intra M, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol. 2013;14(4):297–305. doi: 10.1016/S1470-2045(13)70035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Coutant C, Olivier C, Lambaudie E, Fondrinier E, Marchal F, Guillemin F, Seince N, Thomas V, Leveque J, Barranger E, et al. Comparison of models to predict nonsentinel lymph node status in breast cancer patients with metastatic sentinel lymph nodes: a prospective multicenter study. J Clin Oncol. 2009;27(17):2800–2808. doi: 10.1200/JCO.2008.19.7418. [DOI] [PubMed] [Google Scholar]
- 49.Zahoor S, Haji A, Battoo A, Qurieshi M, Mir W, Shah M. Sentinel lymph node biopsy in breast cancer: a clinical review and update. J Breast Cancer. 2017;20(3):217–227. doi: 10.4048/jbc.2017.20.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Fig. S1. The cut-off value of TILs was calculated by receiver operating characteristic (ROC) curve analysis, and the area under the curve (AUC) was 0.719, with a specificity of 0.917 and a sensitivity of 0.750.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article.