Abstract
Background:
Outpatient versus inpatient treatment of deep vein thrombosis (DVT) is believed to result in equivalent outcomes with decreased costs. Little is known about the adoption of outpatient DVT treatment in the United States.
Objective:
Describe the uptake of outpatient DVT treatment in the U.S., and to understand how comorbidities and socio-economic conditions impact the decision to treat as an outpatient.
Design and Setting:
The REasons for Geographic And Racial Differences in Stroke (REGARDS) cohort study recruited 30,329 participants between 2003–2007. DVT events were ascertained through 2011.
Measurements:
Multivariable logistic regression was used to determine the correlates of outpatient treatment of DVT accounting for age, sex, race, education, income, urban / rural residence and region of residence.
Results:
Of 379 venous thromboembolism events, 141 participants had a DVT without diagnosed pulmonary embolism and that did not occur during hospitalization. Overall, 28% (39 of 141) of participants with DVT were treated as an outpatient. In a multivariable model, the odds ratio (OR) for outpatient versus inpatient DVT treatment was 4.16 (95% confidence interval [CI] 1.25–13.79) for urban versus rural dwellers, 3.29 (CI 1.30–8.30) for whites versus blacks, 2.41 (CI 1.06–5.47) for women versus men, and 1.90 (1.19–3.02) for every 10 years younger in age. Living outside the Southeastern U.S., higher education and income, were not statistically significantly associated with outpatient treatment.
Conclusions:
Despite known safety and efficacy, only 28% of participants with DVT received outpatient treatment. This study highlights populations where efforts could be made to reduce hospital admissions.
Introduction
Venous thromboembolism (VTE) is a common medical condition comprising deep vein thrombosis (DVT) and Pulmonary Embolism (PE). Estimates of the incidence of DVT in the United States vary between 0.5 to 1.5 cases per 1,000 person-years1. Left untreated, roughly 50% of DVT patients progress to a PE of whom 10–25% would die within 3 months2.
From the 1990s, multiple randomized controlled studies3–5 demonstrated the safety and efficacy of outpatient treatment for selected DVT patients with low molecular weight heparin and warfarin. The United States Food and Drug Administration approved enoxaparin, a low molecular weight heparin for outpatient use in 19986 and by the end of the decade multiple treatment guidelines for VTE acknowledged the safety of outpatient treatment of DVT with low molecular weight heparin in selected patients7–9. Recently, the approval of direct oral anticoagulants (DOACs) by the Food and Drug Administration allows an all oral treatment regimen for VTE which could further facilitate outpatient treatment of DVT.
Costs associated with treatment of VTE are enormous. For outpatient treatment, studies differ on individual estimates of cost savings associated with outpatient DVT management, but most report a cost savings of several thousand dollars per patient treated as an outpatient compared to an inpatient6,10. Given the incidence of DVT, reducing costs while maintaining a high quality of care in even a small percentage of DVT patients would result in significant healthcare cost savings, as well as increased convenience for patients.
Despite high quality evidence supporting the efficacy and safety or outpatient DVT treatment, little is known about the adoption of outpatient DVT treatment in the United States. Several studies that have been published were limited to single hospitals and were small in size11,12, or limited to a cohort of patients with already diagnosed DVT13.
The purpose of this study was to report the frequency of outpatient treatment of DVT in the United States and to describe patient characteristics associated with outpatient treatment. Information was gathered from the REGARDS study, a contemporary cohort study of over 30,000 patients residing in the contiguous US with racial and geographic diversity. We hypothesized that an individual’s age, sex, race, region of residence, urban/rural residence, education level, and personal income would be associated with outpatient treatment. Results would allow implementation of interventions to promote appropriate use of outpatient treatment in order to reduce healthcare costs and increase patient convenience without compromising safety or efficacy of care.
Methods
Cohort Characteristics
VTE events were ascertained in the REGARDS cohort, a prospective longitudinal cohort study investigating the causes of racial and geographic disparities in stroke and cognitive decline14. Between 2003 and 2007, 30,239 participants in the contiguous United States aged ≥45 years old enrolled in REGARDS. By design, 55% were female, 41% were black, the mean age was 65, and 56% lived in the Southeastern U.S. Participants were recruited from a commercial list by mail and telephone contact followed by verbal consent. A telephone interview was followed by an in-home examination, including obtaining written informed consent. On study entry, many participants had comorbid conditions, including 8% with reported Atrial Fibrillation, 56% receiving treatment for hypertension, 22% for diabetes, 3.7% taking warfarin and 14% who were actively smoking15,16. Participants were only excluded if they had active cancer, stated a self-reported race other than white or black, were unable to converse in English, had cognitive impairment as judged by the telephone interviewer, or were residing in or on the waiting list for a nursing home. Study methods were reviewed and approved by the institutional review board at each study institution and have been published elsewhere14.
Event ascertainment and definitions
DVT event ascertainment is complete through 2011, with identification by telephone interview, review of reported hospitalizations, and review of deaths17. Questionnaires in similar epidemiological studies have 98% specificity and >70% sensitivity for ascertaining VTE events18. A research nurse reviewed the text recorded each reported hospitalization through 2011. Any report of a blood clot in the legs, arms, or lungs was a potential case for physician review. Medical records were retrieved for up to 1 year before and 1 year after potential events. Retrieved records were used to help guide further record retrieval if they did not contain the primary VTE event. Primary inpatient and outpatient records, including history and physical examinations, discharge summaries, imaging reports (to include limb Ultrasounds, CT scans, MRIs), autopsies and outpatient notes, were retrieved using up to 3 attempts19. Using all available information, characteristics of the VTE event and treatment were systematically recorded. For each potential VTE case, two of three physician reviewers abstracted medical records to validate and classify the event. If the physician reviewers disagreed, the third physician would review the case and if VTE status remained uncertain, cases were discussed and resolved. Race was determined by participant self-report as black or white. Location of residence was defined by geocoding of the address and urban or rural status was defined by United States census tract using Rural-Urban Commuting Area Codes (RUCA, with rural areas being RUCA codes 4–10)20. Other risk factors were obtained through surveys, telephone interviews or an in-home visit14.
Outpatient treatment was defined as receiving a DVT diagnosis in an emergency department or ambulatory clinic, but not receiving an overnight hospitalization. Inpatient treatment was defined as at least one overnight stay in a hospital (but not in an emergency department). Only participants admitted with a primary diagnosis of DVT were included in the analysis. If someone was noted to have a DVT, but was admitted to the hospital for another cause, they were not included in the analysis, and classified as a hospital-associated DVT. A provoked DVT was defined as occurring within 90 days of major trauma, surgery, marked immobility, or associated with active cancer or treatment for cancer (i.e. chemotherapy, radiotherapy, surgical therapy), while an unprovoked DVT was defined as having none of the above provoking factors. A distal DVT was defined as a DVT occurring in the posterior tibial, anterior tibial, peroneal, or soleus sinuses. The primary outcome was DVT treated as an outpatient only without concurrent diagnosis of PE or VTE as a complication of a hospitalization (as these individuals were not eligible for outpatient treatment at the time).
Statistical Analysis
Age, sex, race, region of residence (inside or outside the Southeastern US), education, income (determined as greater or less than $20,000 per year), and urban or rural status of residence were compared between those treated as an outpatient or inpatient using chi-square analysis in DVT patients by inpatient or outpatient treatment. Univariable and multivariable logistic regression was then used to determine the odds ratio (OR) of receiving outpatient DVT treatment by the same variables, with age per 10 year increment. ORs were adjusted for age, sex, race, year of DVT diagnosis, and region of residence as appropriate. Statistical significance was defined as P < 0.05. All statistical analyses were performed by N.A.Z. and conducted with SAS, version 9.3 (SAS Institute, Cary, NC, USA). All authors had access to the primary clinical data.
Results
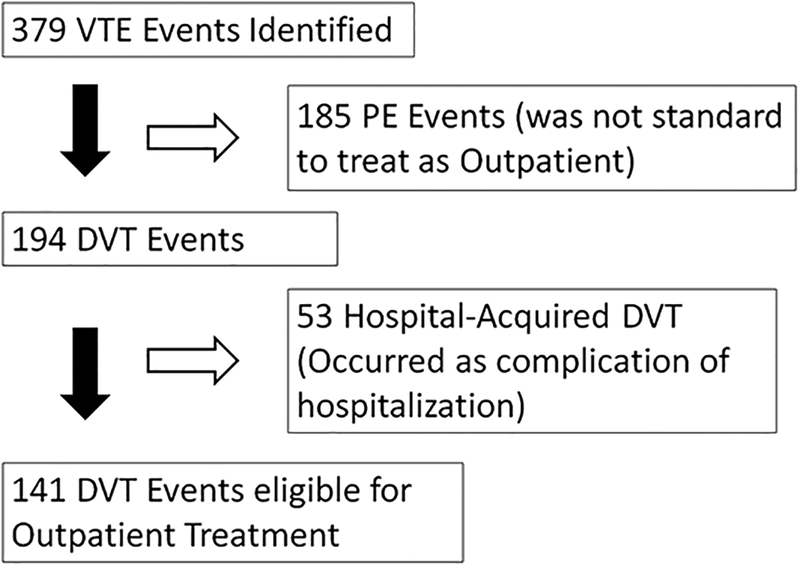
Over a mean of 4.7 years follow-up, 379 VTE events occurred (incident and recurrent); 185 were diagnosed with a PE and 53 occurred as a complication of hospitalization (and not eligible for outpatient treatment) leaving 141 DVT events potentially eligible for outpatient treatment out of a population of 29,556 participants with available records and follow-up in the cohort (figure 1).
Figure 1.
Of 141 DVT events, 39 (28%) were treated as an outpatient. Table 1 presents the characteristics of participants treated as an inpatient and as an outpatient. Factors significantly associated with outpatient DVT treatment were younger age, female sex, white race, residing in an urban area, having a distal DVT only, and having a higher income. In the study, DVT events were recorded between 2003 to 2011, the median year of a diagnosed DVT and treated as an outpatient was 2009, while the median year of inpatient treatment was 2008. Living in the Southeast versus the rest of the country (P= 0.13) and high school education or greater (P= 0.07) were marginally associated with receiving outpatient treatment. In absolute terms, 11% of people living in rural areas and 19% of blacks had outpatient DVT treatment while 33% of the urban dwellers and 32% of whites received outpatient treatment (Table 1). At the time of cohort enrolment, 92% of participants claimed to have insurance, however this did not differentiate between Medicare, Medicaid and private insurance. Only 1 participant diagnosed with a DVT had an estimated glomerular filtration rate (eGFR) < 30, and this individual was admitted for treatment.
Table 1.
Characteristics of Participants with DVT by Treatment Location
| Treated as Outpatient Total: 39 |
Treated as Inpatient Total: 102 |
p | |
|---|---|---|---|
| Median age (interquartile range) | 67 years (60–73) | 70 years (63–76) | 0.02 |
| DVT Year (median) | 2009 | 2008 | 0.02 |
| Female | 23 (59%) | 43 (42%) | 0.03 |
| White | 30 (77%) | 62 (61%) | 0.04 |
| Living outside the southeast | 21 (54%) | 50 (49%) | 0.13 |
| High School Graduate | 38 (97%) | 90 (88%) | 0.07 |
| Yearly Income >$20K | 12 (82%) | 58 (57%) | 0.02 |
| Living in a Urban Area | 35 (90%) | 71 (70%) | 0.01 |
| Provoked event | 10 (26%) | 42 (41%) | 0.09 |
| Body Mass Index ≥30 | 20 (51%) | 47 (47%) | 0.55 |
| Current or former smoker | 17 (44%) | 53 (52%) | 0.45 |
| Proximal DVT | 28 (72%) | 92 (90%) | <0.01 |
| Treated with full dose anticoagulation | 34 (87%) | 89(87%) | 0.99 |
| History of Cancer* | 6 (25%) | 14 (18%) | 0.43 |
| Chronic Kidney Disease (eGFR <60) | 5 (13%) | 19(19%) | 0.46 |
| History of Coronary Artery Disease* | 8 (21%) | 23 (23%) | 0.77 |
| History of Hypertension | 21 (54%) | 70 (69%) | 0.10 |
| History of Diabetes* | 4 (11%) | 21 (22%) | 0.15 |
| History of Hyperlipidemia* | 22 (56%) | 53 (54%) | 0.80 |
Data missing on 38 participants with cancer, 1 participant with coronary artery disease, 7 participants with diabetes, 4 participants with hyperlipidemia
Table 2 reports the multivariable adjusted odds ratio (OR) for outpatient treatment of DVT adjusted for age, sex, race, region and year of DVT diagnosis. Outpatient treatment of VTE was associated with younger age (OR of 1.90 [95% CI 1.19–3.02] for every 10 years younger in age), female sex (OR of 2.41 [95% CI 1.06–5.47]), and white race (OR of 3.29 [1.30–8.30]). For each progressive calendar year in which the diagnosis was made, individuals had a 1.35-fold increased odds (95% CI 1.03–1.77) of receiving outpatient treatment. Individuals living in urban areas were 4.16 (95% CI 1.25, 13.79) times more likely to receive outpatient treatment than those in rural areas. Living outside of the southeastern US, and having an income over $20,000 per year had an increased, but non-significant odds of being treated as an outpatient (Table 2).
Table 2.
Likelihood of receiving outpatient treatment for DVT (odds ratios, 95% CI)
| Variable | Adjusted Odds Ratio (95% CI)* |
|---|---|
| Age (per 10 years younger) | 1.90 (1.19, 3.02) |
| Year of DVT diagnosis (per 1 year later) | 1.35 (1.03–1.77) |
| Sex (Female vs. Male) | 2.41 (1.06, 5.47) |
| Race (White vs. Black) | 3.29 (1.30, 8.30) |
| Region (Outside the southeast vs. southeast) | 2.00 (0.87, 4.63) |
| Education (High School Graduate vs. No) | 4.51 (0.52, 38.82) |
| Income >$20,000 (Yes vs. No) | 2.63 (0.87, 7.94) |
| Living in an Urban Area (Yes vs. No) | 4.16 (1.25, 13.79) |
Adjusted for age, sex, race, VTE event year, and region
Discussion
In this national prospective observational cohort study, only 28% of participants diagnosed with a DVT were treated as an outpatient versus hospitalized. Urban area of residence, white race, female sex, and younger age were significantly associated with an increased odds of outpatient treatment. Groups that had particularly low outpatient treatment rates were rural dwellers and blacks, who had outpatient treatment rates of 11 and 19% respectively. The odds of receiving outpatient treatment did improve over the course of the study, but in the last year of VTE assessment, outpatient treatment remained at 40%, but this was quite variable over the study years (being 8% 2 years prior).
The feasibility of treating DVTs as an outpatient requires a coordinated health care system and patient support to ensure education and appropriate anticoagulation monitoring. While not all DVTs should be treated as an outpatient, differences in treatment location by sex, race, and residence point to potential health care disparities which increase the burden on patients and increase health care costs. Other studies have documented low outpatient treatment rates of DVTs (20% in one U.S. multicenter DVT registry) but have not discussed the associations of outpatient versus inpatient treatment13. Outpatient treatment also appears underutilized in other developed countries; in the European VTE REITE registry only 31% of DVT patients were treated on an outpatient basis between 2001–201121. To our knowledge, this is the first study to document the uptake of outpatient DVT treatment in the United States across multiple states, regions and health systems well after the safety and efficacy of outpatient treatment of DVT was established randomized controlled trials3–5.
The strengths of this study are that these data are derived from a contemporary cohort with a large geographic and racial distribution in the U.S., and are well characterized with a mean of 4.6 years follow up19. We are limited by a relatively small number of DVT events eligible for outpatient treatment (n=141) and so may miss modest associations. Further, while the geographic scope of the cohort is a tremendous strength of our study, we may have missed some events and did not have complete record retrieval of reported events and could not assess access to healthcare in detail. These data were recorded before the use of DOACs became common. DOACs are an effective and safe alternative to conventional anticoagulation treatment for acute DVT22. Their use might result in increased outpatient treatment as they are not parenteral, however cost considerations (~$400.00 / month) especially with high deductible insurance plans may limit their impact on VTE treatment location23. This study cannot account for why the racial, sex, and urban/rural differences exist, and by extension if hospitalization rates differ due to associated comorbidities or if this represents a healthcare disparity. While it is reasonable from a health care perspective that younger individuals would more likely be treated as an outpatient, there is no data to suggest that differences in DVT by sex, race, and residential location support decreased outpatient treatment. Due to the age of the cohort, most individuals had some form of insurance and a primary care provider. We were however unable to assess the quality of insurance and the ease of access to their primary care providers. More research is needed to determine whether patients were hospitalized on medical grounds or because of a lack of coordinated health care systems to care for them as an outpatient.
In conclusion, only a minority of patients potentially eligible for outpatient DVT treatment (28%) were treated as an outpatient in this study and there were significant racial and socio-economic differences in who received inpatient and outpatient treatment. While outpatient treatment rates were below 40% in all groups, we identified groups with especially low likelihoods of receiving outpatient treatment. While all eligible individuals should be offered outpatient DVT treatment, these data highlight the need for specific efforts to overcome barriers to outpatient treatment in the elderly, rural areas, blacks, and men. Even modest increases in the rate of outpatient DVT treatment could result in substantial cost savings and increased patient convenience without compromising the efficacy or safety of medical care.
Acknowledgements:
We thank the staff and participants of REGARDS for their important contributions. The Executive Committee of REGARDS reviewed and approved this manuscript for publication. This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org Additional funding was provided by an investigator-initiated grant-in-aid from the American Recovery and Reinvestment Act grant RC1HL099460 from the National Heart, Lung, and Blood Institute. Work for the manuscript was supported in part by the Lake Champlain Cancer Research Organization, Burlington, Vermont.
Footnotes
Summary of all relevant conflict of interest statements: Neither my co-authors nor I have any conflicts of interest to report.
References
- 1.Raskob GE, Angchaisuksiri P, Blanco a N, et al. Thrombosis : A major contributor to global disease burden ☆ ISTH Steering Committee for World Thrombosis Day The members of the ISTH Steering Committee for World Thrombosis Day : Thromb Res. 2014;134(5):931–938. doi:10.1016/j.thromres.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Kearon C Natural history of venous thromboembolism. Circulation. 2003;107(SUPPL. 23):22–31. doi:10.1161/01.CIR.0000078464.82671.78. [DOI] [PubMed] [Google Scholar]
- 3.Koopman MM, Prandoni P, Piovella F, et al. Treatment of venous thrombosis with intravenous unfractionated heparin administered in the hospital as compared with subcutaneous low-molecular-weight heparin administered at home. The Tasman Study Group. N Engl J Med. 1996;334(11):682–687. doi:10.1056/NEJM199603143341102. [DOI] [PubMed] [Google Scholar]
- 4.Prandoni P, Lensing a W, Büller HR, et al. Comparison of subcutaneous low-molecular-weight heparin with intravenous standard heparin in proximal deep-vein thrombosis. Lancet. 1992;339(8791):441–445. doi:10.1016/S0196-0644(05)81047-9. [DOI] [PubMed] [Google Scholar]
- 5.Levine M, Gent M, Hirsh J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med. 1996;334(11):677–681. doi:10.1056/NEJM199603143341101. [DOI] [PubMed] [Google Scholar]
- 6.Segal JB, Bolger DT, Jenckes MW, et al. Outpatient therapy with low molecular weight heparin for the treatment of venous thromboembolism: a review of efficacy, safety, and costs. Am J Med. 2003;115(4):298–308. doi:10.1016/S0002-9343(03)00326-7. [DOI] [PubMed] [Google Scholar]
- 7.Hyers TM, Agnelli G, Hull RD, et al. Antithrombotic therapy for venous thromboembolic disease. Chest. 2001;119(1 Suppl):176S–193S. [DOI] [PubMed] [Google Scholar]
- 8.Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996;93(12):2212–2245. [DOI] [PubMed] [Google Scholar]
- 9.Dunn AS, Coller B. Outpatient treatment of deep vein thrombosis: translating clinical trials into practice. Am J Med. 1999;106(6):660–669. [DOI] [PubMed] [Google Scholar]
- 10.Spyropoulos AC, Lin J. Direct medical costs of venous thromboembolism and subsequent hospital readmission rates: an administrative claims analysis from 30 managed care organizations. J Manag Care Pharm. 2007;13(6):475–486. doi:2007(13)6: 475–486 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee M, Pao D, Hsu T, Sonderskov A. Cost savings and effectiveness of outpatient treatment with low molecular weight heparin of deep vein thrombosis in a community hospital. Can J Clin Pharmacol. 2004;11(1):e17–e27. [PubMed] [Google Scholar]
- 12.Pearson SD, Blair R, Halpert A, Eddy E, Mckean S. An outpatient program to treat deep venous thrombosis with low-molecular-weight heparin. Eff Clin Pract. 1999;2(5):210–217. [PubMed] [Google Scholar]
- 13.Goldhaber SZ, Tapson VF. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004;93(2):259–262. doi:10.1016/j.amjcard.2003.09.057. [DOI] [PubMed] [Google Scholar]
- 14.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25(3):135–143. doi:10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 15.Meschia JF, Merrill P, Soliman EZ, et al. Racial disparities in awareness and treatment of atrial fibrillation: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2010;41(4):581–587. doi:10.1161/STROKEAHA.109.573907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cushman M, Cantrell RA, McClure LA, et al. Estimated 10-year stroke risk by region and race in the United States: geographic and racial differences in stroke risk. Ann Neurol. 2008;64(5):507–513. doi:10.1002/ana.21493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wojcik NC, Huebner WW, Jorgensen G. Strategies for using the National Death Index and the Social Security Administration for death ascertainment in large occupational cohort mortality studies. Am J Epidemiol. 2010;172(4):469–477. doi:10.1093/aje/kwq130. [DOI] [PubMed] [Google Scholar]
- 18.Frezzato M, Tosetto A, Rodeghiero F. Validated questionnaire for the identification of previous personal or familial venous thromboembolism. Am J Epidemiol. 1996;143(12):1257–1265. [DOI] [PubMed] [Google Scholar]
- 19.Zakai N a., McClure L a., Judd SE, et al. Racial and regional differences in venous thromboembolism in the United States in 3 cohorts. Circulation. 2014;129:1502–1509. doi:10.1161/CIRCULATIONAHA.113.006472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morrill R, Cromartie J, Hart G. Metropolitan, Urban, and Rural Commuting Areas: Toward a Better Depiction of the United States Settlement System. Urban Geogr. 1999;20(8):727–748. doi:10.2747/0272-3638.20.8.727. [Google Scholar]
- 21.Lozano F, Trujillo-Santos J, Barrón M, et al. Home versus in-hospital treatment of outpatients with acute deep venous thrombosis of the lower limbs. J Vasc Surg. 2014;59(5):1362–1367.e1. doi:10.1016/j.jvs.2013.11.091. [DOI] [PubMed] [Google Scholar]
- 22.Robertson L, Kesteven P, McCaslin JE. Oral direct thrombin inhibitors or oral factor Xa inhibitors for the treatment of deep vein thrombosis. Cochrane database Syst Rev. 2015;6:CD010956. doi:10.1002/14651858.CD010956.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Cushman M Treating Acute Venous Thromboembolism — Shift with Care A New Era in the Treatment of Amyloidosis ? N Engl J Med. 2013:29–30. doi:10.1056/NEJMe1307413. [DOI] [PubMed] [Google Scholar]