Abstract
Introduction
The mortality rates and Disability Adjusted Life Years lost of burn injuries (including scalds) among children below 15 years of age in Africa are more than ten and 20 times higher, respectively, than in high-income countries. Prevention of injuries and timely optimal management will help to reduce these figures. Management guidelines that are locally relevant to low income settings, incorporating universal principles, are required. We aim to provide a reference guide for the management of paediatric burn injuries in settings with limited resources using a resource-tiered approach. Additionally, we would like to add our voice to the advocacy for improvements in primary, secondary and tertiary prevention.
Methods
A literature review was carried out using Ovid Medline (1946 to present), Embase (1974 to November 2016) and Google Scholar (2012 to present) using the key words and Boolean terms Burn OR Scald, AND Paediatric, AND Management OR Treatment, AND Africa, AND Sub-Saharan Africa. Further references were found from citations.
Results and discussion
In total, 78 papers were included in this review, along with the WHO injury book and the Burns Manual. Comprehensive primary prevention programmes should be set up and adequately funded. Assessment and immediate management of a burn patient should follow the ABCDE approach. Appropriate patients such as those with inhalational injury should be referred early. An escharotomy should be performed without delay at the facility where the patient has presented. Intravenous fluid management must be guideline-based, goal-directed and titrated to effect. Pain management should use multiple modalities including adequate and pre-emptive analgesia. Supplemental nutrition is required in patients with baseline malnutrition and/or burns greater than 10% Total Body Surface Area. Infections such as toxic shock syndrome and tetanus must be managed aggressively.
African relevance
-
•
Burn and scald injuries in Sub-Saharan Africa are very common.
-
•
Prevention strategies are an important aspect of burn management in Sub-Saharan Africa.
-
•
Appropriate treatment reduces the morbidity associated with burn and scald injuries in low resourced settings.
Introduction
Advances in knowledge around the management and prevention of burns has led to a reduction in the mortality of burn and scald injuries in high income countries, with the WHO documenting mortality rates of between 0.2 and 0.6 per 100,000 aged less than 15 years. Disability Adjusted Life Years (DALYs) lost, a measure of overall disease burden, are also estimated to be lower in high-income countries, at around 85,000 [1].
Unfortunately, this benefit is often not translated to low- and middle-income settings such as Africa, where the mortality rate is 6.9 per 100,000 in those aged less than 15 years and the DALYs lost are extremely high (estimated to be over 2 million) [1]. In addition approximately 300,000 new burn cases occur annually in those aged under five in sub-Saharan Africa, calculated from the lowest observed incidence rates which may therefore underplay the genuine burden of these injuries [2], [3]. Furthermore, over 80% of burn and scald injuries are sustained in children younger than ten years, with an average mortality of 17% [2], [3].
The transfer gap can be explained in part by lack of resources and the fact that burn injuries are closely related to social and cultural factors. This means that research around prevention and management in high-income countries is often irrelevant to low- and middle-income settings. Although proposed ‘gold standard’ burn treatment is difficult to translate to low income settings, practitioners often still carry out a high level of burn care by combining lessons learned from high income countries with local knowledge and practices [4]. Nonetheless, everyone involved in the management of these injuries in resource-constrained situations should be an advocate for improvements in primary, secondary and tertiary prevention. Governments are urged by the World Health Assembly (WHA) to support Surgery as a component of Universal Health Coverage, as detailed in the A68/15 WHA Resolution on Strengthening Emergency and Essential Surgical Care and Anaesthesia, passed on the 22nd of May 2015 [5]. Secondary and tertiary prevention can only be effective if health services are made accessible and affordable to all who require them at the appropriate time, at a facility that is suitably equipped and manned with adequate and appropriately trained personnel.
Our aim with this paper is to provide a reference for the management of paediatric burn patients in sub Saharan Africa. We hope to provide an overview for care providers who are faced with the reality of sparse resources, by sharing our local burn care management plan alongside published evidence of good burn care practice throughout the continent and advice for the different levels of resourcefulness. First aid, wound management and rehabilitation have not been discussed.
Methods
A literature review was carried out using Ovid Medline (1946 to Present) and Embase (1974 to November 2016, Epub Ahead of Print, In-Process and Other Non-Indexed Citations). The key words and Boolean terms used were Burn OR Scald, AND Paediatric, AND Management OR Treatment, AND Africa, AND Sub-Saharan Africa. This generated 28 papers, which after removal of duplicates and irrelevant papers, left 15 papers. Further papers were identified using Google Scholar with the same key words and Boolean terms. This generated 796 papers since the year 2012. Thirty-six were found to be relevant and not duplicates. As each paper was read, further references were identified from the list of citations. In total, 85 papers were included in this review, along with the WHO injury book and the Burns Manual (2nd edition, 2008) which is the reference manual for the care of burn and scald patients treated in our Burn Unit here at the Queen Elizabeth Central Hospital, Blantyre, Malawi. The last search was undertaken on 5th December 2016. Representative papers are referenced.
Results and discussion
Immediate management of burns and scalds: assessment of the patient
In order not to miss other injuries, patient evaluation must be systematic. The assessment and immediate management of a burn patient follows the ABCDE approach, namely the identification and correction of life-threatening injuries beginning with those that are most rapidly fatal (See Appendix 1). The following conditions are particular to burn injuries and must be noted: inhalational injury; thoracic eschar syndrome; extremity eschar syndrome [6].
Inhalational injury patients must be referred to a Burn Unit without undue delay. See Table 1 for referral criteria. Early intubation is required for those with infraglottic injuries [7]. A bedside escharotomy must be done for the eschar syndromes to improve breathing compliance and limb perfusion. This must be done even at the Primary Health Care level. See Fig. 1. Blood samples are taken including Full Blood Count, Urea, Creatinine and Electrolytes, where resources permit.
Table 1.
Referral guidelines [23].
| Level one to two* | Level two to three* | |
|---|---|---|
| Neonates | All | All |
| Elderly patients | All | All |
| Inhalational injury | All | All |
| Electrical injury | All | All |
| Chemical burn | All | All |
| Full thickness burns | All | 10% < TBSA < 50% |
| Partial thickness burns | >5% TBSA in children | >20% TBSA in children |
| >10% TBSA in adults | >30% TBSA in adults | |
| Associated injuries | Minor injuries | Major injuries |
| Primary area burns | All | ≥1% TBSA |
TBSA, Total Body Surface Area.
*Level one is a primary health facility such as a health centre, level two is a secondary health facility such as a district hospital, level three is a tertiary/specialist health facility such as a central hospital.
Fig. 1.
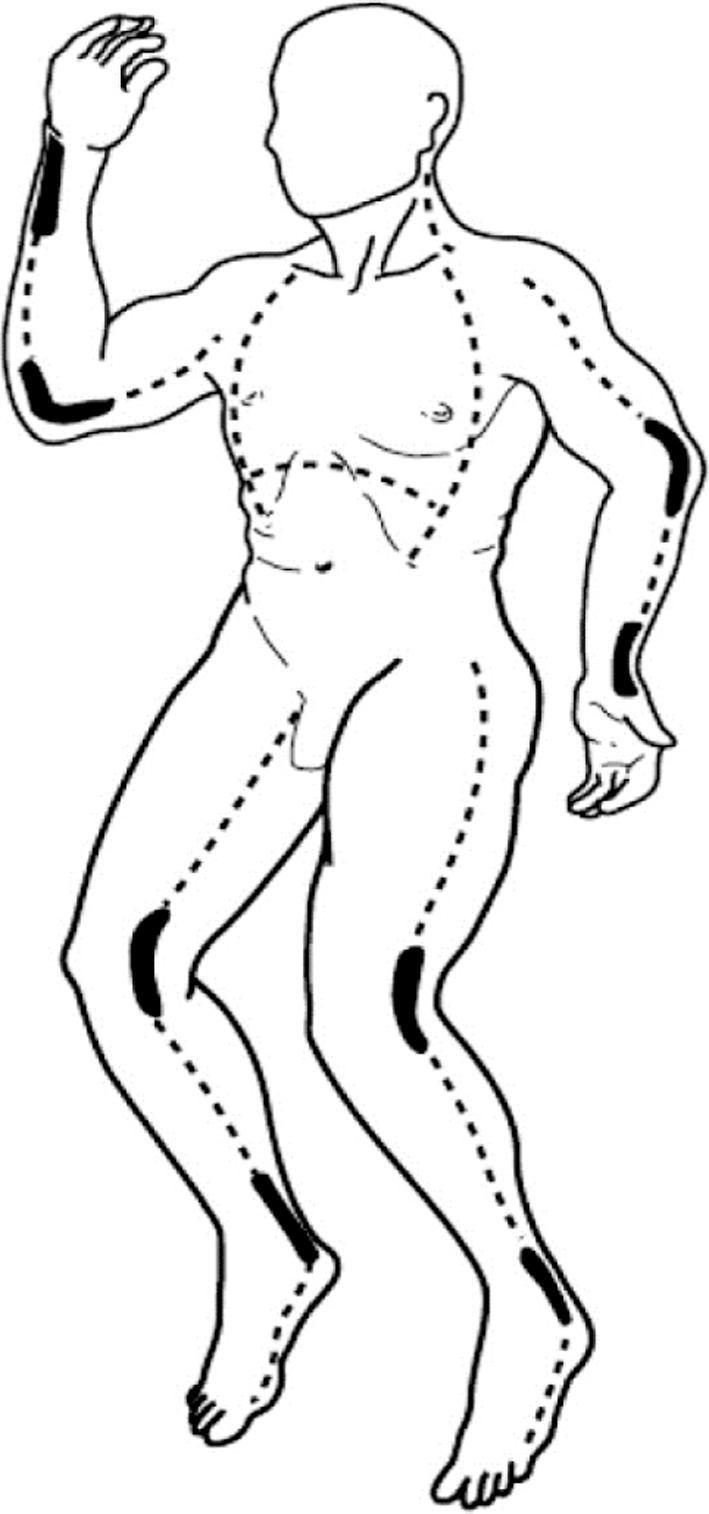
Escharotomy sites [23].
An assessment should be made of the burn size, also known as the percentage of Total Body Surface Area (%TBSA). This is important for calculating the fluid replacement and also for highlighting those patients who are at a greater risk for complications. It is well known that the greater the %TBSA, the higher the mortality rate [8], [9]. Various charts are available to help estimate the %TBSA. Areas of erythema should be excluded as these are only superficial and will usually heal within seven days.
The Lund and Browder Chart [10] is thought to be the most accurate method for calculation as it acknowledges the change in contribution that each body part represents at different ages (Fig. 2). If this is not readily available, the palmar surface of the patient’s hand, from the wrist to the finger tips, which is approximately 1%, may be used to calculate small areas, or the spared areas in large burns. It should be noted that there is controversy regarding the use of the hand versus the palm (excluding fingers) as to which constitutes 1% [11], [12].
Fig. 2.
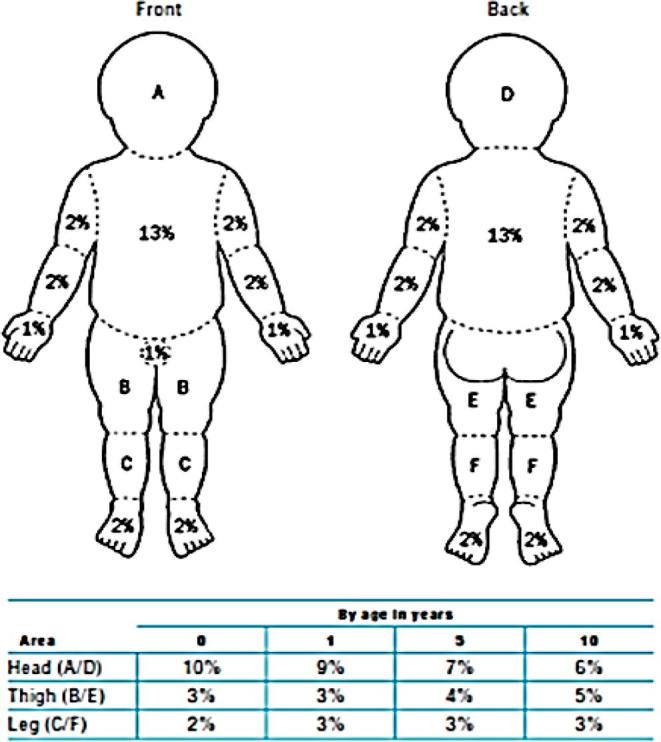
Paediatric Lund and Browder Chart.
Wallace’s rule of nines [13] has been found to be fairly accurate in adults, but not so much in children. If this is used, it is estimated that up to the age of one year the head is 18% and each lower limb is 14%. For each year following, 1% should be subtracted from the head and 0.5% added to each lower limb. By the age of ten years the patient has reached the proportions of an adult. See Fig. 3.
Fig. 3.
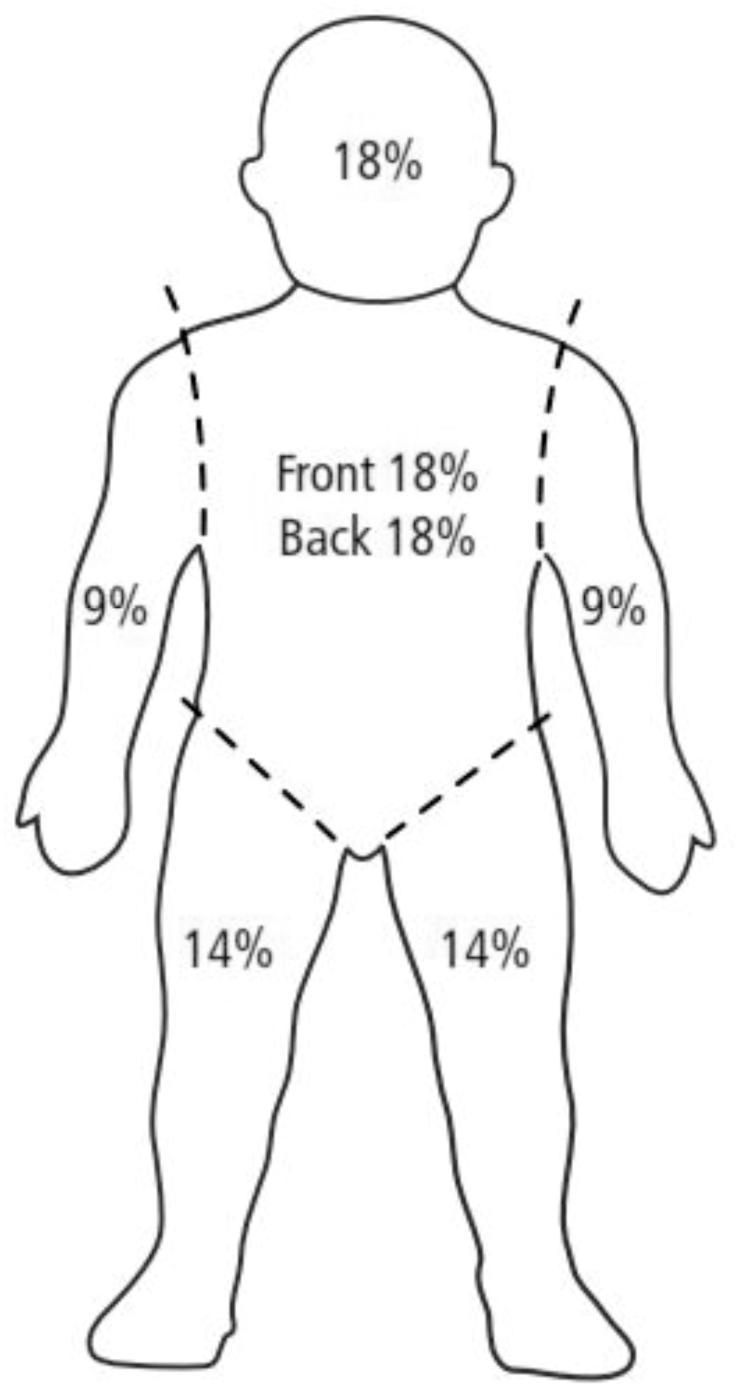
Wallace’s Rule of Nines [23].
Immediate management of burns and scalds: fluid management
Oral fluids (oral rehydrate solution) are adequate for most burns of less than 10% total body surface area. Indications for intravenous fluid administration are detailed in Table 2. Intravenous fluid management must be guideline-based, goal-directed and titrated to effect. The fluid requirement is calculated from the time of injury using a formula such as Parkland or Modified Brooke as stipulated in the local guideline. See Table 3. The Parkland formula using Ringer’s lactate is probably the most common practice in Africa [14]. The intravenous fluid giving set should have a burette where possible to avoid infusion of too much fluid Table 4.
Table 2.
Indications for intravenous fluid therapy.
| Indication | Fluid therapy |
|---|---|
| ≥10% TBSA | Full regime (formula plus maintenance) |
| Patient taking inadequate oral fluids | Maintenance fluids only if <10% TBSA |
| Pre-existing fluid deficit with ≥10% TBSA | Fluid repletion plus full regime |
| Pre-existing fluid deficit with <10% TBSA | Fluid repletion plus maintenance |
TBSA, Total Body Surface Area.
Table 3.
Calculations for intravenous fluid therapy.
| Maintenance Fluids | 0.9% NaCl + 5%Dextrose | For the first 10 kg…4 ml/kg/h (100 ml/kg/24 h) For 10–20 kg…2 ml/kg/h (50 ml/kg/24 h) For greater than 20 kg…1 ml/kg/h (25 ml/kg/24 h) |
| Parkland Formula* | Ringers Lactate or 0.9% NaCl | 4 ml × %TBSA × weight (kg) Half the volume is given in the first 8 h, the remainder over the next 16 h^ |
| Modified Brooke Formula* | Ringers Lactate or 0.9% NaCl | 3 ml × %TBSA × weight (kg) Half the volume is given in the first 8 h, the remainder over the next 16 h^ |
TBSA, Total Body Surface Area.
*Either Parkland or modified Brooke formula should be used, and this is in addition to maintenance fluids.
^Note that this is calculated from the time of injury.
Table 4.
Level A, key recommendations regarding the immediate management of burns and scalds.
Assessment of the patient
|
Fluid Management
|
Pain management
|
Nutrition
|
Toxic Shock Syndrome and Tetanus
|
If there are no scales available, the child’s weight can be calculated using the formula (age + 4) × 2 = … kg.
Additional fluids include maintenance, boluses to correct shock, replacement of on-going losses and additional requirements [15]. The maintenance and replacement fluids must have glucose added to them to make at least a 5% solution since children’s liver glycogen stores can be depleted within 14 h of starving. In patients who are in hypovolemic or in burn shock, 10–20 ml/kg fluid boluses should be given [15]. Losses, such as through vomiting and diarrhoea, must be replaced. Myoglobinuria, one of the complications of burns involving muscles, presents with dark coloured urine and requires a urine output of 2 ml/kg/h to be maintained in order to reduce the risk of acute tubular necrosis [15].
Urine output must be monitored hourly for those requiring intravenous fluids. Fluids are titrated to maintain an adequate urine output of 1 ml/kg/hour in children. If it is low, increase the maintenance fluid rate by 20% [6]. If this needs to be repeated, do so, but re-evaluate for other pathology such as blood loss and arrange for transfer to a facility with an intensive care unit. Conversely, decrease fluids by 20% if the urine output is high. Over-hydration may lead to resuscitation morbidity in the form of compartment syndromes (extremities, abdominal and cerebral) and pulmonary oedema among others. In the absence of a urethral catheter, older children can be asked to pass urine into a urinal, while a feeding tube may be used in the younger children. Alternatively, the diaper or equivalent can be weighed before and after the child passes urine. Children who require monitoring of their urine output should be referred to a tertiary/specialist facility or a Burns Unit.
Immediate management of burns and scalds: pain management
Adequate and pre-emptive analgesia is essential for patient comfort, to avoid complications such as atelectasis and to facilitate rehabilitation. Background and procedural pain must both be addressed. Formal pain assessment must be undertaken where the normal analgesia is inadequate. Most centres in Africa use Paracetamol and Ibuprofen [16], which are adequate for most small burns. Ibuprofen should not be given to children younger than 3 months of age [16]. Morphine is appropriate for procedural analgesia in patients with small burns, but may be used even for background pain in large burns. Analgesia should be complemented with anxiolytics such as a short-acting benzodiazepine and non-pharmacological techniques such as distraction therapy. In our institution, a portable DVD player is used during dressing changes. Red Cross Memorial Hospital in Cape Town has documented the benefits of aromatherapy massage as a non-pharmacological adjunct to pain management [17]. Ketamine is a dissociative anaesthetic agent which has been demonstrated to have good analgesic properties [18], [19]. In addition it also provides sedation and amnesia, whilst still maintaining the protective airway reflexes, which has led to its recognition within burn management as an ideal agent for dressing changes [20]. A versatile compound, it has been administered orally (5–10 mg/kg) [18], [20], intravenously (0.5–4 mg/kg) [19] or intramuscularly (2–5 mg/kg) [21]. Reported side effects include respiratory depression, laryngospasm, tachycardia and hypertension. [21] Close monitoring of the patient, including continuous oxygen saturation, non-invasive blood pressure and temperature is recommended, with reference to guidelines and safety check lists [19], [21], [22].
Immediate management of burns and scalds: nutrition
The importance of appropriate nutrition in burn injuries cannot be over emphasised. The hypermetabolic response to burn injury requires a high calorie intake in order to encourage optimal healing and there is also an increase in protein requirements. Enteral nutrition should be encouraged and commenced early as it has been shown to have a protective role in the gastrointestinal system, with reduction in the risk of bacterial translocation and stress ulceration [23], [24].
The European Society for Clinical Nutrition and Metabolism (ESPEN) have endorsed guidelines relating to nutrition therapy in relation to major burns [25]. They found strong evidence to support the initiation of early enteral feeding (within 12 h of injury) and to set the protein requirements in children to between 1.5 and 3 g/kg/day. They also recommended supplementation of micronutrients, with strong evidence to suggest a substitution of zinc, copper, selenium and Vitamins B1, C, D and E would be beneficial.
We would recommend supplemental nutrition in patients with baseline malnutrition and/or burns greater than 10% TBSA [23]. The Curreri formula for children has been designed to calculate the protein and calorie requirements and in the absence of a nutritionist, a tailor-made protocol may be adopted such as that proposed by van Hasselt [23] (See Appendix 2).
It may be difficult for the child to manage oral intake, either because of the sheer volume of calorific requirement, or due to difficulty physically managing the intake, for example, due to a reduced appetite (caused by pain and anxiety) or difficulty feeding (due to facial or hand burns). In this situation a nasogastric tube, if available, should be encouraged. It is recognised that a nasogastric tube may be negatively viewed by parents or guardians, and to encourage compliance, it is important to educate as to the reasons behind its use. The authors designed a poster which was used in our Burn Unit and translated into the local language; this could be referenced by the nursing and medical staff to encourage a visual explanation to relatives [26].
Immediate management of burns and scalds: toxic shock syndrome and tetanus
A septic screen (full clinical evaluation and acquisition of appropriate microbiological specimens) must be done in a child with fever if the wound is unlikely to be the cause, such as in a small fresh burn [27]. Toxic shock syndrome should be suspected if there is concomitant vomiting and/or diarrhoea. This typically occurs within 48 h of injury, as opposed to burn sepsis which occurs later (See Appendix 3). Remember also to check for Malaria parasites. Although antibiotic prophylaxis should not be given in all settings, it may be appropriate in children if the number of burn patients who present with features of TSS are significant.
Tetanus is an important infection in settings where soil and other traditional concoctions are applied on burn wounds; even more so, if immunisation coverage in the general under-five population is suboptimal (See Appendix 4). Patients suspected of these infections must be referred urgently after gaining venous access, starting antibiotics and debriding the wounds.
Conclusion
Primary, secondary and tertiary prevention of burn injuries and their sequelae must be intensified with the support of governments of low and middle-income countries to reduce the mortality rates and DALYs lost. We have provided a resource-tiered reference guide for resource-constrained settings based on available evidence (Table 3).
Conflicts of interest
The authors declare no conflicts of interest.
Author contribution
EBo conceived the original idea. TC and EBr drafted the manuscript and TC, EBo and EBr revised it. TC, EBr and EBo approved the final version that was accepted for publication.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.afjem.2017.06.004.
Appendix A. Supplementary data
References
- 1.WHO Report: The Global Burden of Disease: 2004 Update.
- 2.Hyder A.A., Kashyap K.S., Fishman S., Wali S.A. Review of Childhood Burn Injuries in Sub-Saharan Africa: A Forgotten Public Health Challenge. Afr Saf Promot. 2004;2(2):43–58. [Google Scholar]
- 3.Nthumba P.M. Burns in Sub-Saharan Africa: A review. Burns. 2016;42:258–266. doi: 10.1016/j.burns.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 4.Albertyn R., Bicklerb S.W., Rode H. Paediatric burn injuries in Sub Saharan Africa—an overview. Burns. 2006;32:605–612. doi: 10.1016/j.burns.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Price R., Makasa E., Hollands M. World Health Assembly Resolution WHA68.15:“Strengthening Emergency and Essential Surgical Care and Anesthesia as a Component of Universal Health Coverage”—Addressing the Public Health Gaps Arising from Lack of Safe, Affordable and Accessible Surgical and Anesthetic Services. World J Surg. 2015;39:2115–2125. doi: 10.1007/s00268-015-3153-y. [DOI] [PubMed] [Google Scholar]
- 6.Cancio L.C. Initial Assessment and Fluid Resuscitation of Burn Patients. Surg Clin N Am. 2014;94:741–754. doi: 10.1016/j.suc.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Thomas J, Karpelowsky J. The Burn Injury. In Thomas J, Rode H, Eds. A Practical Guide To Paediatric Burns. SAMA Health and Medical Publishing Group. 2006. Chapter 2.
- 8.Rode H., Cox S.G., Numanoglu A., BergBurn A.M. Care in South Africa: a micro cosmos of Africa. Pediatr Surg Int. 2014;30:699–706. doi: 10.1007/s00383-014-3519-5. [DOI] [PubMed] [Google Scholar]
- 9.Jugmohan B., Loveland J., Doedens L., Moore R.L., Welthagen A., Westgarth-Taylor C.J. Mortality in paediatric burns victims: A retrospective review from 2009 to 2012 in a single centre. S Afr Med J. 2016;106(2):189–192. doi: 10.7196/SAMJ.2016.v106i2.8942. [DOI] [PubMed] [Google Scholar]
- 10.Lund C.C., Browder N.C. The estimation of areas of burns. Surg Gynecol Obstet. 1944;79:352–358. [Google Scholar]
- 11.Rossiter N.D., Chapman P., Haywood I.A. How big is a hand? Burns. 1996;22(3):230–231. doi: 10.1016/0305-4179(95)00118-2. [DOI] [PubMed] [Google Scholar]
- 12.Nagel T.R., Schunk J.E. Using the hand to estimate the surface area of a burn in children. Pediatr Emerg Care. 1997;13:254–255. doi: 10.1097/00006565-199708000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Knaysi G.A., Crikelair G.F., Cosman B. The rule of nines: its history and accuracy. Plast Reconstr Surg. 1968;41(6):560–563. [PubMed] [Google Scholar]
- 14.Rode H., Rogers A.D., Cox S.G., Allorto N.L., Stefani F., Bosco A. Burn resuscitation on the African continent. Burns. 2014;40:1283–1291. doi: 10.1016/j.burns.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Thomas J, Karpelowsky J. Resuscitation & Fluid Management. In Thomas J, Rode H, Eds. A Practical Guide To Paediatric Burns. SAMA Health and Medical Publishing Group. 2006. Chapter 5.
- 16.Madadi P., Enato E.F.O., Fulga S., Umeoduagu C.C., MacLeod S.M., Koren G. Patterns of paediatric analgesic use in Africa: a systematic review. Arch Dis Child. 2012;97:1086–1091. doi: 10.1136/archdischild-2012-302386. [DOI] [PubMed] [Google Scholar]
- 17.O’Flahertya L.A., vanDijk M., Albertyn R., Millar A., Rode H. Aromatherapy massage seems to enhance relaxation in children with burns: An observational pilot study. Burns. 2012;38:840–845. doi: 10.1016/j.burns.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Norambuenaa C., Yañezb J., Floresc V., Puentesd P., Carrascoc P., Villenae R. Oral ketamine and midazolam for pediatric burn patients: A prospective, randomized, double-blind study. J Ped Surg. 2013;48:629–634. doi: 10.1016/j.jpedsurg.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 19.Owens V.F., Palmieri T.L., Comroe C.M., Conroy J.M., Scavone J.A., Greenhalgh D.G. Ketamine: A Safe and Effective Agent for Painful Procedures in the Pediatric Burn Patient. J Burn Care Res. 2006;27:211–216. doi: 10.1097/01.BCR.0000204310.67594.A1. [DOI] [PubMed] [Google Scholar]
- 20.O’Hara D., Kirubalini G., Gerrish H., Richardson P. A 2 year experience of nurse led conscious sedation in paediatric burns. Burns. 2014;40:48–53. doi: 10.1016/j.burns.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 21.Green S.M., Krauss B. Clinical Practice Guideline for Emergency Department Ketamine Dissociative Sedation in Children. Ann Emerg Med. 2004;44:460–471. doi: 10.1016/S0196064404006365. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz K.R., Fredricks K., Al Tawil Z., Kandler T., Odenyo S.A., Imbamba J. An innovative safe anesthesia and analgesia package for emergency pediatric procedures and surgeries when no anesthetist is available. Intl J Em Med. 2016;9:16. doi: 10.1186/s12245-016-0113-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Hasselt EJ. Burns Manual: A manual for health workers. 2nd ed. Nederlandse Brandwonden Stichting; 2008.
- 24.Prelack K., Dylewski M., Sheridan R.L. Practical guidelines for nutritional management of burn injury and recovery. Burns. 2007;33:14–24. doi: 10.1016/j.burns.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Rousseau A.F., Losser M.R., Ichai C., Berger M.M. ESPEN endorsed recommendations: Nutritional therapy in major burns. Clin Nut. 2013;32:497–502. doi: 10.1016/j.clnu.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 26.www.rebas.org/nutrition.
- 27.White M.C., Thorton K., Young A.E.R. Early diagnosis of toxic shock syndrome in paediatric burns. Burns. 2005;31:193–197. doi: 10.1016/j.burns.2004.09.017. [DOI] [PubMed] [Google Scholar]
Recommended reading
- 28.Potokar T (Ed). Setting Standards for Burn Care services in Low and Middle Income Countries. Interburns Publication. 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


