Abstract
Background
Young adults with type 1 diabetes (T1D) experience a decline in glycemic outcomes and gaps in clinical care. A diabetes education and support program designed for young adults was delivered through group videoconference and mobile Web.
Objective
The objective of our study was to assess the feasibility, acceptability, and preliminary efficacy of the program as measured by attendance and webpage views, satisfaction, and pre- and postintervention psychosocial outcomes, respectively.
Methods
Young adults aged 18-25 years were recruited to attend five 30-minute group diabetes education videoconferences during an 8-week period. Videoconferences included an expert presentation followed by a moderated group discussion. Within 48 hours of each videoconference, participants were sent a link to more information on the study website. Feasibility was assessed using data on videoconference attendance and webpage views. Acceptability was assessed via a Satisfaction Survey completed at the conclusion of the study. Descriptive statistics were generated. Preliminary efficacy was assessed via a survey to measure changes in diabetes-specific self-efficacy and diabetes distress. Pre- and postintervention data were compared using paired samples t tests.
Results
In this study, 20 young adults (mean age 19.2 [SD 1.1] years) attended an average of 5.1 (SD 1.0) videoconferences equivalent to 153 (SD 30.6) minutes of diabetes education per participant during an 8-week period. Average participant satisfaction scores were 62.2 (SD 2.6) out of a possible 65 points. A total of 102 links sent via text message (short message service) or email resulted in 504 webpage views. There was no statistically significant difference between pre- and postintervention diabetes-specific self-efficacy or diabetes-related distress.
Conclusions
Delivery of diabetes education via group videoconference using mobile Web follow-up is feasible and acceptable to young adults with T1D. This model of care delivery has the potential to improve attendance, social support, and patient-reported satisfaction. Nevertheless, further research is required to establish the effect on long-term psychosocial and glycemic outcomes.
Keywords: diabetes education, mobile phone, telehealth, type 1 diabetes, young adult, transition
Introduction
Clinic-based transition support for young adults with type 1 diabetes (T1D) remains inadequate despite expert consensus guidelines published by the American Diabetes Association in 2011 [1-4]. Many young adults with T1D experience gaps in care, have poor glycemic control, and are, thus, at risk for acute and long-term diabetes-related complications. In a large clinical registry based in the United States, only 13% of young adults with T1D achieved the recommended glycated hemoglobin (HbA1c) target of 7%, with HbA1c peaking at an average of 9.2% at the age of 19 years [5,6]. This decline in glycemic control occurs as many young adults move away from home and lose access to their established diabetes support system [7,8]. Recent efforts to provide clinic-based structured transition support for young adults with T1D have been associated with improved glycemic control, reduced hypoglycemia, and improved psychological well-being [9,10]. Telemedicine visits have been successfully used in lieu of in-clinic visits to improve adherence to clinical attendance standards for pediatric patients with diabetes in rural settings [11], and an innovative pilot study found group medical appointments for young adults with T1D conducted using Web-based videoconference technology to be feasible and acceptable [12]. However, the use of Web-based group videoconferences to provide a transition-focused diabetes self-management education and support (DSMES) program has not been studied. The purpose of this pilot study was to test the feasibility, acceptability, and preliminary efficacy of a telehealth transition education program designed for young adults with T1D as a first step in our efforts to evaluate its potential for integration into the clinical care paradigm.
Methods
Following the institutional review board (IRB) approval, participants were recruited via fliers at the University of Florida outpatient diabetes clinic. Upon enrollment, participants completed surveys on paper to obtain demographic data, diabetes history, technology acquisition, and communication preferences. Participants then completed the Problem Areas in Diabetes (PAID) Scale to assess baseline levels of diabetes-specific distress [13,14] and the Confidence in Diabetes Scale (CIDS) to assess baseline levels of diabetes-specific self-efficacy [15]. The PAID Scale consists of 20 items; potential scores range from 0 to 80, with higher scores indicating higher levels of distress. The instrument has demonstrated high internal reliability (Cronbach alpha=.90) as well as reasonable (Spearman ρ=.83) 2-month test-retest reliability and correlates strongly with a wide range of theoretically related psychosocial constructs in diabetes (eg, distress, depression, self-care behaviors, coping, and health beliefs). The CIDS survey has 20 items; potential scores range from 20 to 100, with higher scores indicating higher levels of self-efficacy. The instrument has demonstrated high internal consistency (alpha=.90) and test-retest reliability (ρ=.85, P<.001).
Once the surveys were completed, participants were asked to indicate which 5 group diabetes education videoconferences they preferred to attend over the 8-week study period. Each topic was offered a total of 5 times (5 different dates or times). A maximum of 5 participants per videoconference was set to facilitate dialogue and minimize the risk for technical challenges. After participants indicated topical preferences, a study coordinator contacted them to assist with scheduling. Vidyo software (Vidyo, Inc, Hackensack, NJ, USA) was used as the videoconference platform; it allows end users to participate via a smartphone, tablet, laptop, or desktop. Each 30-minute videoconference included a brief (10-15 minute) expert presentation by a pediatric endocrinologist, nurse practitioner (NP), certified diabetes educator (CDE), psychologist, or registered dietitian (RD). At the beginning of each videoconference, a moderator read a scripted, IRB-approved statement regarding privacy and respecting the privacy of all study participants. Only first names were used during group education sessions. Participants had the option to enable or disable video streaming during all videoconferences. The moderator’s introduction was followed by the expert presentation, and then a moderated discussion among participants to foster peer-learning and social support. Table 1 summarizes the diabetes education topics available during the study.
Table 1.
Diabetes education topics.
| Videoconference topic | Description |
| Pediatric versus Adult Diabetes Clinic | What to expect, how to prepare for transition |
| Say What? | How to have the “Diabetes Talk” |
| Your Rights | Reasonable work and school accommodations |
| Sex, Insulin, and Rock-n-Roll | Exploring “taboo” subjects related to real life with type 1 diabetes |
| Exercise and Nutrition | Optimizing activity and nutrition |
| Diabetes Burnout and Sources of Support | Identifying burnout, burnout versus depression, and how to find help |
| New and Emerging Diabetes Technologies | Insulin pumps, continuous glucose monitors, automated insulin delivery |
Within 48 hours of each videoconference, attendees were sent a link to additional content on a section of the study website specifically for young adults with T1D and their parents (Figure 1). The study website was developed and reviewed by a multidisciplinary team of CDEs, pediatric endocrinologists, NPs, psychologists, RDs, registered nurses, parents, and people with diabetes. The website provides information on basic diabetes management, diabetes technology, and additional content tailored to young adults with T1D. Of note, the website was not publicly available during the study and could only be reached via links sent to participants. Web analytics for the site were monitored and analyzed, with particular attention to relevant page views and increases in website traffic during the 48 hours following the distribution of links via short message service (SMS) text message or email to participants.
Figure 1.
Screenshot of the young adult section of the study website. Source: T1D Toolkit.
At the end of the 8-week study, participants completed the PAID Scale, the CIDS Scale, and a Satisfaction Survey to assess acceptability and usability. The Satisfaction Survey was designed for the study and included 16 questions (13 closed-ended and 3 open-ended) to obtain end-user feedback about the usability and acceptability of the program. Potential scores on the closed-ended questions ranged from 13 to 65, with higher scores indicating higher levels of satisfaction. Answers to open-ended questions were reviewed and coded to inform future iterations of the educational content and clinical model. At the completion of study procedures, a US $75 gift card was provided to participants. Participants were given information about the US $75 gift card at the time of informed consent.
Quantitative data from the Demographic, Communication Preferences, and Satisfaction surveys were analyzed using SPSS, v.25, software (IBM Corp, Armonk, NY) to generate descriptive statistics. Results are expressed as mean (SD) and as frequencies and percentages for categorical variables. Pre- and postintervention scores on the CIDS and PAID scales were analyzed using paired samples t test. A P<.05 was considered statistically significant. Web analytics were reviewed and pageview data were analyzed to describe participant traffic on the study website, T1DToolkit.org.
Results
We approached 21 participants to participate in this study. All enrolled, but 1 participant withdrew immediately following enrollment citing a busy high school sports schedule. Mean age of participants was 19.2 (SD 4.39) years, and 80% (16/21) participants were females. Mean diabetes duration was 10.21 (SD 4.39; range, 2-17) years; mean age at diagnosis was 9 (SD 4.42; range, 3-17) years, and 80% (16/20) participants were insulin pump users. Table 2 provides additional demographic data. All participants had access to a smartphone (20/20, 100%) and most had access to a computer, laptop, or tablet. A majority (9/20, 45%) of participants preferred to receive notifications via both SMS text message and email, with 40% (8/20) preferring SMS text message only and 15% (3/20) email only (Table 3).
Table 2.
The description of study participants.
| Characteristics | Values | ||
| Age in years, mean (SD) | 19.2 (4.39) | ||
| Age at diagnosis in years, mean (SD) | 9 (4.42) | ||
| Type 1 diabetes duration in years, mean (SD) | 10.21 (4.39) | ||
| Insulin regimen, n (%) | |||
| Pump | 16 (80) | ||
| Multiple daily injections | 4 (20) | ||
| Gender, n (%) | |||
| Male | 4 (20) | ||
| Female | 16 (80) | ||
| Ethnicity, n (%) | |||
| Asian | 3 (15) | ||
| Hispanic black | 1 (5) | ||
| Non-Hispanic black | 1 (5) | ||
| Hispanic | 1 (5) | ||
| Non-Hispanic white | 14 (70) | ||
| Residence, n (%) | |||
| Independent | 14 (70) | ||
| Parent or guardian | 6 (30) | ||
| Level at school, n (%) | |||
| College | 17 (85) | ||
| High School | 3 (15) | ||
| Employment, n (%) | |||
| Full time | 4 (20) | ||
| Part time | 10 (50) | ||
| None | 6 (30) | ||
Table 3.
Technology acquisition and communication preferences.
| Characteristics | Values | |
| Technology acquisition, n (%) | ||
| Smartphone | 20 (100) | |
| Tablet | 7 (35) | |
| Laptop | 19 (95) | |
| Desktop | 6 (30) | |
| Communication preference, n (%) | ||
| Email only | 3 (15) | |
| Short message service (SMS) text message only | 8 (40) | |
| Email and SMS text message | 9 (45) | |
Mean attendance was 5.1 (SD 1.0; range, 2-7) diabetes education videoconferences per participant, which is equivalent to an average of 153 (SD 30.6; range, 60-210) minutes of diabetes education per participant. The most popular sessions included Diabetes Burnout (n=17), Your Rights (n=15), Diabetes Technologies (n=15), and Exercise and Nutrition (n=15); these were followed by Transition to Adult Clinic (n=14); Sex, Insulin, and Rock-n-Roll (n=14); and Say What? (n=12). A minimum of 2 and a maximum of 5 participants participated in each of the 35 videoconferences offered during the study. The mean score on the Satisfaction Survey was 62.2 (SD 2.6; range, 57-65). Overall, 95% (19/20) participants responded that they would be “extremely interested” or “very interested” in participating in a similar program in the future. Representative positive responses to the open-ended questions included, “I really enjoyed participating in this study. I got to talk about things that I don’t really talk about with my doctor. And the topics that I have discussed with my doctor, it was interesting to hear different opinions.” Suggestions to improve the program included, “Add a better way to manage all questions from larger groups of people” and “Only one session had technical difficulties where no one could log on. It was fixed quickly.”
The mean scores for diabetes-related distress declined; however, there was no statistically significant reduction when comparing the mean baseline (mean 20.4 [SD 15.0]) and postintervention (mean 17.2 [SD 15.3]) scores on the PAID Scale (t19=1.04, P=.09). Mean scores for diabetes-specific self-efficacy increased; however, there was no statistically significant increase when comparing the mean baseline (mean 87.0 [SD 7.4]) and postintervention (mean 88.2 [SD 6.9]) scores on the CIDS Scale (t19=−0.79, P=.44; Table 4).
Table 4.
Psychosocial outcomes.
| Construct | Measure | Mean (SD) | t statistic | dfa | P value | ||||
| Pre | Post | ||||||||
| Diabetes-related distress | Problem areas in Diabetes Scale | 20.4 (15.0) | 17.2 (15.3) | 0.79 | 19 | .09 | |||
| Diabetes-related self-efficacy | Confidence in Diabetes Scale | 87 (7.4) | 88.2 (6.9) | 1.04 | 19 | .44 | |||
adf: degrees of freedom.
A total of 102 emails or SMS text messages with links to the study website were sent to participants, resulting in 504 page views. The timing of website page views was strongly linked to the date the links were pushed to participants; this indicates a high level of engagement in the educational content by participants. Figure 2 provides a sample of the dose-response feedback.
Figure 2.
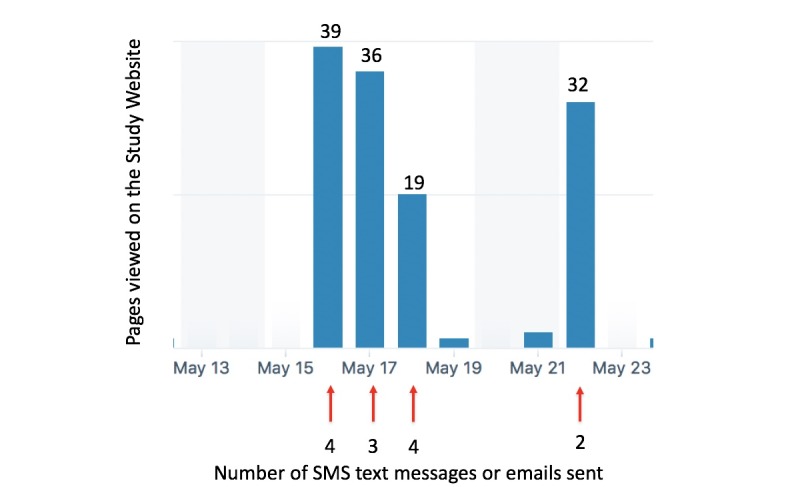
Dose-response example of pushed links and website page views. SMS: short message service.
Discussion
This pilot study with young adults with T1D demonstrated high feasibility for providing diabetes education and support via group videoconference and strong participant engagement in Web-based follow-up. Participants reported high levels of acceptability as measured by user satisfaction. In terms of the preliminary efficacy, there was no statistical difference in pre- and postintervention psychosocial outcomes; however, on average, we observed improved scores for both diabetes-related self-efficacy and diabetes-related distress. The findings support results from previous studies that have demonstrated high attendance and satisfaction with individual clinic visits and group medical appointments provided via telehealth to youth and young adults with T1D [11,12].
The implications of these results should be considered in the context of the study’s limitations. Owing to the brief duration of and limited funding for the study, other efficacy-related outcome measures including glycemic control and diabetes knowledge attainment were not assessed. Recruitment took place at a university-based diabetes clinic, where patients may be more highly motivated to attend diabetes education visits. In addition, despite the ubiquity of mobile technology, patients with limited data plans or access to wireless networks may not find participation as feasible without financial support to cover the cost of a mobile data plan.
Nonetheless, the outcomes suggest that this delivery model for diabetes education and support has the potential to increase contact with the clinic, improve access to diabetes education, and provide peer and social support for young adults who have become disconnected from their diabetes network. Future randomized studies that include a control group should explore the intermediate and longitudinal effect of the model on glycemic control, diabetes knowledge attainment, clinic attendance, and psychosocial outcomes. In addition, future studies should measure provider satisfaction and explore the feasibility of reimbursement for telehealth group videoconference education sessions. Convenient, comprehensive, yet tailored diabetes care, education, and support is required to keep young adults engaged in their diabetes management to reduce gaps in care and to mitigate the decline in glycemic control commonly experienced by this patient population. As T1D management becomes more technically complex, videoconference and Web-based models of diabetes care and education delivery can be leveraged to connect patients to providers and educators at a reduced cost with improved convenience and without a decline in patient satisfaction.
Acknowledgments
This project was funded by the University of South Florida’s “Bringing Science Home” Initiative (University of Florida Agreement #6401-1028-00-O).
Abbreviations
- CDE
certified diabetes educator
- CIDS
Confidence in Diabetes Scale
- DSMES
diabetes self-management education and support
- HbA1c
glycated hemoglobin
- IRB
Institutional Review Board
- NP
nurse practitioner
- PAID
Problem Areas in Diabetes Scale
- RD
registered dietitian
- SMS
short message service
- T1D
type 1 diabetes
Footnotes
Conflicts of Interest: None declared.
Authors' Contributions: AAO, NT, and MJH designed the study. AAO, GB, MJH, SCW, and NT enrolled subjects and delivered the educational content. AAO, GB, and NT collected the data. AAO and MJH designed and performed the analysis. AAO, NT, and MJH wrote the manuscript. SCW, NJ, and DS reviewed and edited the manuscript.
References
- 1.Garvey KC, Beste MG, Luff D, Atakov-Castillo A, Wolpert HA, Ritholz MD. Experiences of health care transition voiced by young adults with type 1 diabetes: a qualitative study. Adolesc Health Med Ther. 2014;5:191–8. doi: 10.2147/AHMT.S67943. doi: 10.2147/AHMT.S67943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hilliard ME, Perlus JG, Clark LM, Haynie DL, Plotnick LP, Guttmann-Bauman I, Iannotti RJ. Perspectives from before and after the pediatric to adult care transition: a mixed-methods study in type 1 diabetes. Diabetes Care. 2014 Feb;37(2):346–54. doi: 10.2337/dc13-1346. http://europepmc.org/abstract/MED/24089544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peters A, Laffel L, American Diabetes Association Transitions Working Group Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society) Diabetes Care. 2011 Nov;34(11):2477–85. doi: 10.2337/dc11-1723. http://europepmc.org/abstract/MED/22025785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agarwal S, Garvey KC, Raymond JK, Schutta MH. Perspectives on care for young adults with type 1 diabetes transitioning from pediatric to adult health systems: A national survey of pediatric endocrinologists. Pediatr Diabetes. 2017 Nov;18(7):524–531. doi: 10.1111/pedi.12436. http://europepmc.org/abstract/MED/27578432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood JR, Miller KM, Maahs DM, Beck RW, DiMeglio LA, Libman IM, Quinn M, Tamborlane WV, Woerner SE, T1 DCN. Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care. 2013 Jul;36(7):2035–7. doi: 10.2337/dc12-1959. http://europepmc.org/abstract/MED/23340893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, Maahs DM, Tamborlane WV, T1 DCN. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015 Jun;38(6):971–8. doi: 10.2337/dc15-0078. [DOI] [PubMed] [Google Scholar]
- 7.Ramchandani N, Cantey-Kiser JM, Alter CA, Brink SJ, Yeager SD, Tamborlane WV, Chipkin SR. Self-reported factors that affect glycemic control in college students with type 1 diabetes. Diabetes Educ. 2000;26(4):656–66. doi: 10.1177/014572170002600413. [DOI] [PubMed] [Google Scholar]
- 8.Monaghan M, Helgeson V, Wiebe D. Type 1 diabetes in young adulthood. Curr Diabetes Rev. 2015;11(4):239–50. doi: 10.2174/1573399811666150421114957. http://europepmc.org/abstract/MED/25901502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sequeira PA, Pyatak EA, Weigensberg MJ, Vigen CP, Wood JR, Ruelas V, Montoya L, Cohen M, Speer H, Clark S, Peters AL. Let's Empower and Prepare (LEAP): Evaluation of a Structured Transition Program for Young Adults With Type 1 Diabetes. Diabetes Care. 2015 Aug;38(8):1412–9. doi: 10.2337/dc14-2577. http://europepmc.org/abstract/MED/25906787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Markowitz JT, Laffel LMB. Transitions in care: support group for young adults with Type 1 diabetes. Diabet Med. 2012 Apr;29(4):522–5. doi: 10.1111/j.1464-5491.2011.03537.x. http://europepmc.org/abstract/MED/22150392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raymond JK, Berget CL, Driscoll KA, Ketchum K, Cain C, Fred TJF. CoYoT1 Clinic: Innovative Telemedicine Care Model for Young Adults with Type 1 Diabetes. Diabetes Technol Ther. 2016 Dec;18(6):385–90. doi: 10.1089/dia.2015.0425. http://europepmc.org/abstract/MED/27196443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wood CL, Clements SA, McFann K, Slover R, Thomas JF, Wadwa RP. Use of Telemedicine to Improve Adherence to American Diabetes Association Standards in Pediatric Type 1 Diabetes. Diabetes Technol Ther. 2016 Jan;18(1):7–14. doi: 10.1089/dia.2015.0123. [DOI] [PubMed] [Google Scholar]
- 13.Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care. 1997 May;20(5):760–6. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 14.Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, Schwartz CE. Assessment of diabetes-related distress. Diabetes Care. 1995 Jun;18(6):754–60. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 15.Van Der Ven NCW, Weinger K, Yi J, Pouwer F, Adèr H, Van Der Ploeg HM, Snoek FJ. The confidence in diabetes self-care scale: psychometric properties of a new measure of diabetes-specific self-efficacy in Dutch and US patients with type 1 diabetes. Diabetes Care. 2003 Mar;26(3):713–8. doi: 10.2337/diacare.26.3.713. http://europepmc.org/abstract/MED/12610027. [DOI] [PMC free article] [PubMed] [Google Scholar]