Abstract
ABSTRACT: Rhythm disorders in young people are often reported and when they are persistent, repetitive or with a severity degree, an ethiopathgenical assessment of arrhythmogenic risk factors and their implications is required. Purpose: Arrhythmogenic risk factors evaluation and the possibility of determining oxidative stress in the arrhythmic pathology in young people. Material and Methods: The study was conducted on 184 young subjects, aged 16-26 years old; the points of interest were: the presence or absence of cardiac dysrhythmias, the existence of proarrhythmogenic risk factors and determination of oxidative stress status modifications. Results: Of the studied young subjects, 39% presented heart rhythm disturbances, repetitive or persistent (atrial extrasystolic arrhythmia, sinus tachycardia, ventricular extrasystolic arrhythmia, paroxysmal atrial fibrillation, paroxysmal supraventricular tachycardia, associated dysrhythmias, atrial flutter, sinus bradycardia), which have been associated with the following risk factors: coffee consumption 82%, stress 80%, physical effort 72%, energy drinks consumption 72%, hyperlipidic diet 69%, familial predisposition 69%, alcohol intake 53%, frequent sleep deprivation 50%, smoking 31%, overweight 31%. The observed risk factors may be involved in the increasing of oxidative stress level, and, for this reason, the determination of oxidative stress biomarkers is required. The association of arrhythmogenic risk factors, with the expression of oxidative stress markers and the existence of enzymatic genetic polymorphism of redox systems, requires proper monitoring for the further risk of endothelial lesions induction, leading to aterosclerosis. Conclusions: Arrhythmogenic risk factors and biomarkers of oxidative stress are important, especially in young people cases, for monitoring the cardiovascular risk, for primary prevention and early treatment.
Keywords: arrhythmogenic risk factors, young people, oxidative stress
Introduction
Arrhythmias in young people, either functional or pathologic, are frequently described, having a significant impact regarding the quality of life, professional and extra-professional performances.
The multitude of factors favoring the installation of arrhythmias (either paroxysmal, repetitive, persistent or permanent) requires a study of their profile, evaluating their role- assessed in some laboratory or experimental research [1] [3] [5] - in the installation of oxidative stress modifications [2], involved in generating subsequent lesion changes, with pathological induction.
Various exogenous conditions, known through their proarrhythmogenic risks, should be considered, especially in young people, for the early prophylaxis of severe damage to the cardiovascular system.
The often unbalanced diet, poor in antioxidants, stressing metabolic conditions, especially in young persons, and the increased cellular oxidations may determine an oxidant-antioxidant imbalance, with short-term repercussion, such as the occurrence of abnormal heart rhythm or term-long ones, in association with other disorders (hypoxic, hormonal, dyslipidemics, genetic predisposition and others), generating the installation of endothelial injury with early initiation of pathological processes, especially atherosclerosis.
Spectrum, pattern profile, of arrhythmogenic risk elements and disruptive oxidative status, isolated or associated in various combinations, describes the following factors: smoking, drinking coffee and energy drinks consumption, alcohol intake, physical efforts, nutritional, hormonal and psychosocial imbalances, familial predisposition.
Aim and Objectives
The observation of potentially arrhythmogenic risk factors in young persons is important, in order to evaluate trigger conditions and their control. Some of these conditions have an increased risk in generating a disturbance of oxidant-antioxidant balance, with side effects, by creating a high level of oxidative stress that can and may induce metabolic and cardiac disturbances, leading to unfavorable effects on short and long term.
Objectives of the study are to highlight and evaluate the issues related to cardiac rhythm disorders and also their risk in generating oxidative stress.
Material and Methods
The study was conducted on a group of 186 young subjects aged 16 to 26 years (students and resident physicians). Same type research questionnaires were used, aiming: to describe the presence or absence of cardiac rhythm disorders, the existence of arrhythmogenic and metabolic risk conditions and character.
So, answers were requested regarding smoking, alcohol, coffee, energy, diet rich in protein / fat or rich in fruits and vegetables, nutritional status, weight / height / body mass index, physical activity performed, rest and sleep, stress, medication management, family and personal illness history.
Different aspects of electrocardiographic rhythm disorders were recorded: atrial or ventricular extrasystolic arrhythmia, paroxysmal supraventricular tachycardia, atrial fibrillation, atrial flutter, sinus tachycardia or bradycardia, sustained and persistent. Data related to their character in relation to the installation, duration, impact degree over professional or personal life quality were noted.
The obtained information was selected, highlighting the pre-existing conditions associated to arrhythmias and their type, and then included in databases and processed.
Representation on age groups was approximately equal, 92 teenagers between 16-20 years and 92 adolescents between 21-26 years old. The studied gender group included 128 females and 58 males.
Based on the presence or absence of cardiac rhythm disorders and the assessment of risk factors, subjects were divided into 2 groups, as follows: group I- young subjects with arrhythmias, with risk factors generating oxidative stress; group II- subjects without cardiac rhythm disturbances, but presenting also clinical risk factors. None of the subjects had pre-existing cardiac disease which could have been considered as generator for arrhythmias (determined by clinical examination, electrocardiography and ultrasound investigations).
Statistical calculation allowed us to obtain incidence and risk factors data for each group and mentioned factor. The assessments appreciated their importance and necessity in the determination of oxidative stress biomarkers in young patients with risk factors, especially when they are multiple.
The existence of oxidative stress can be revealed by determining: nitric oxide- NO (Griess colorimetric method), superoxide dismutase activity- SOD, glutathione peroxidase activity- GPx, malondialdehyde activity (thiobarbituric acid), glutathione reductase activity –GR (spectrophotometric measurements). These biochemical determinations are considered as markers of oxidative stress and the interpretation of their variations represents a motivation for further treatment corrections and a method for primary cardiovascular prevention.
Results
Of the total of 186 young subjects aged 16-26 years, 72 showed arrhythmias (group I), representing 39%. A total of 114 subjects (group II) presented no heart rhythm disturbances, namely 61 % (1), (1).
Table 1.
Numeric and procentual group repartition of young subjects
Subjects |
Number |
Percentage |
Total |
186 |
100 |
Group I (Youngs with arrhythmias) |
72 |
39 |
Group II (Youngs without arrhythmias) |
114 |
61 |
Figure 1.
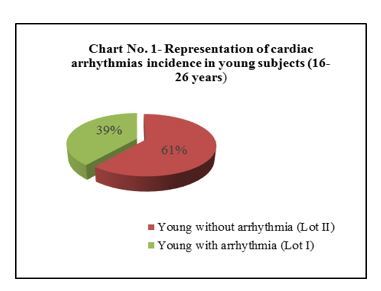
Cardiac arrhythmias frequency in young people
In the total group of young subjects, there were 128 female, 56 of them presenting arrhythmia (44%) and 72 not (56%).
Of all male subjects, a total of 58 men were observed in the study, of which 16, respectively 28 %, showed arrhythmias and 42 (72%) did not (2), (2).
Table 2.
Repartition of studied young subjects by gender, on groups
Gender |
Females |
Males |
||
|
Number |
Percentage |
Number |
Percentage |
Total |
128 |
100 |
58 |
100 |
Group I (Youngs with arrhythmias) |
56 |
44 |
16 |
28 |
Group II (Youngs without arrhythmias) |
72 |
56 |
42 |
72 |
Figure 2.
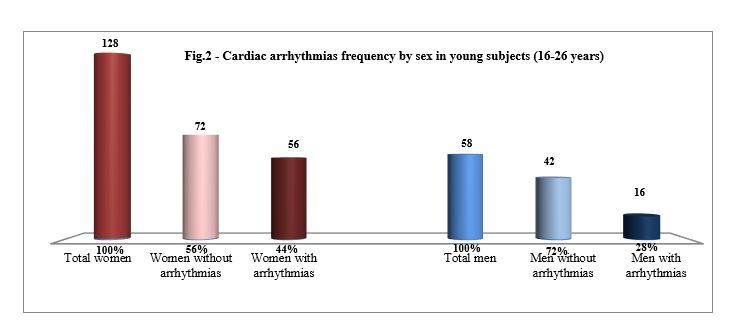
Cardiac arrhythmias frequency by sex in young subjects
Computing the Chi square p value, we obtained p=0.036, meaning there is a statistically significant difference between the percentage of males and females in the two study grups, women being more susceptible in developing arrythmias.
The ratio between subjects who described arrhythmias and those who did not, was for women 56/72 (0.78-3/4) and 16/42 (0.38-1/3) for men. This shows that about 3 out of 4 women and 1 in 3 young men presents heart rhythm abnormalities at a young age.
The most frequently observed arrhythmogenic cardiovascular risk factors:
Smoking was present at a number of 22 patients out of 72 with heart rhythm disturbances (31%) and at 15 of the 114 without arrhythmias, accounting for 13%.
Coffee consumption was reported by 59 of the 72 young subjects with heart rhythm disturbances, representing 82 % and by 40 of the 114 without arrhythmias (35%).
Energy drinks consumption was described in 52 of the 72 subjects with arrhythmias (72%) and in 35 of the 114 without (31%).
Alcohol intake was reported by 38 of the 72 patients with arrhythmias (53%) and by 28 of the 114 without arrhythmia, accounting for 24%.
Physical efforts in relation with cardiac disorders installation were reported by 52 subjects in group I (72%) and by 34 in group II (114), representing 30%.
Alimentation rich in proteins/lipids was recorded in 50 of the subjects with cardiac rhythm disturbances, accounting for 69 % and in 32 subjects without (28%).
Alimentation rich in fruits and vegetables was observed in 20 of the subjects presenting dysrhythmia (28%) and in 70 subjects without heart rhythm disorders (61%).
Nutritional status of subjects, calculated based on body mass index (BMI) was assessed for subjects of group I (with dysrhythmias) as: normal weight in 30 subjects (42%), overweight in 22 (31%), underweight in 20 (28 %) and first degree obesity in 2 subjects (3%).
Subjects of group II, without dysrhythmias were: 70-normal weighted (61%), 21- overweighed (18%), 22-underweighted (19%) and 1 subject with first degree obesity (1%).
The presence of stress was observed in 58 (80%) of subjects with heart rhythm disorders, and in 40 of those without (35%).
Frequent sleep deprivation was observed in 36 (50%) of subjects with arrhythmias and in 10 (9%) of those without heart rhythm disturbances.
Family predisposition of cardiovascular diseases was mentioned by 50 subjects (69%) of those who experienced cardiac rhythm disorders and by 25 (22%) of those without arrhythmias.
Extracardiac risk factors found in the 2 groups of young subjects with and without manifest cardiac arrhythmias were ordered in order of incidence as follows:
For group I (the subjects with arrhythmias): coffee consumption-82%, presence of stress-80%, physical effort-72%, consumption of energy drink-72%, diet rich in proteins/ lipids-69%, family predisposition-69%, alcohol intake-53%, frequent sleep deprivation-50%, smoking-31%, diet rich in fruits and vegetables-28%, underweight-28% and first degree obesity-3%.
For group II (subjects without arrhythmias): diet rich in fruits and vegetables-61% , coffee consumption-35%, the presence of stress-35%, consumption of energy drinks-31%, physical efforts-30%, diet rich in proteins/lipids-28%, alcohol intake-24%, familiar predisposition of cardiovascular disease-22%, underweight-19%, overweight-18%, smoking-13%, frequent sleep deprivation-9% and first degree obesity-1% (3).
Table 3.
Risk factors incidence, on groups, in studied young subjects
Risk factors |
Group I (Youngs with arrhythmias) |
Group II (Youngs without arrhythmias) |
Chi square p value |
Significance |
||
|
Number |
% |
Number |
% |
|
|
Coffee consumption |
59 |
82 |
40 |
35 |
1.9 x 10-10 |
HS |
Stress |
58 |
80 |
40 |
35 |
7.3 x 10-10 |
HS |
Physical effort |
52 |
72 |
34 |
30 |
1.3 x 10-8 |
HS |
Energy drinks consumption |
52 |
72 |
35 |
31 |
2.6 x 10-8 |
HS |
Hyperlipids alimentation |
50 |
69 |
32 |
28 |
2.8 x 10-8 |
HS |
Familiar predisposition |
50 |
69 |
25 |
22 |
1.1 x 10-10 |
HS |
Alcohol intake |
38 |
53 |
28 |
24 |
8.9 x 10-5 |
HS |
Sleep deprivation |
36 |
50 |
10 |
9 |
3.2 x 10-10 |
HS |
Smoking |
22 |
31 |
15 |
13 |
0.0036 |
S |
Overweight |
22 |
31 |
21 |
18 |
0.042 |
S |
Between the 2 groups, were recorded differences regarding arrhythmogenic risk determined by extracardiac factors, the reported percentage being significantly higher in those with cardiac events (3).
Figure 3.
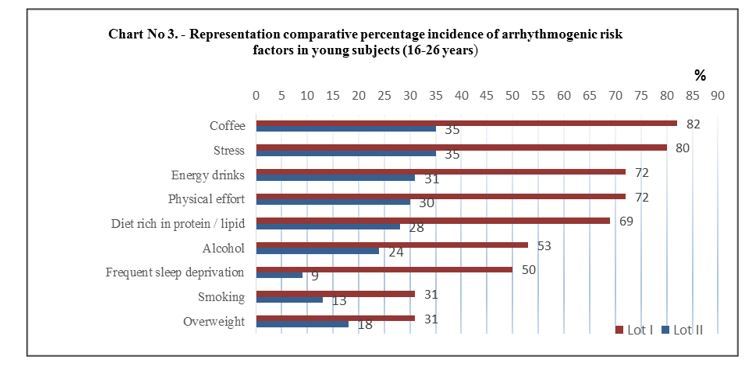
Incidence of arrhythmogenic risk factors in young subjects
There are higly significant differences between the two groups, with p<0.001, regarding risk factors such as: coffee consumption, stress, physical effort, energy drinks consumption, hyperlipids alimentation, familiar predisposition, alcohol intake, sleep deprivation and significant differences, with p<0.05, concerning smoking and overweight.
Young subjects with heart rhythm disorders associated at least: 3 risk factors - a number of 34 (47%), 4 risk factors - 16 subjects (22%), with 5 or more risk factors - 6 people (8%). Addition of risk factors creates preconditions for increased cardiovascular disease and, respectively, they determine an increased arrhythmic risk (4), (4).
Table 4.
Risk factors association, in young subjects with arrhythmias
Number of associated risk factors |
Number of subjects |
Percentage (%) |
1 |
5 |
7 |
2 |
9 |
13 |
3 |
36 |
50 |
4 |
16 |
22 |
≥5 |
6 |
8 |
Figure 4.
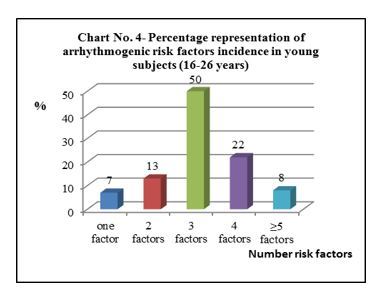
Number of risk factors associations
These extracardiac risk factors may generate arrhythmias on a seemingly normal (healthy) heart and together with the possible induction of oxidative stress (as shown in some studies regarding the described factors) represent favorable conditions for cardiovascular diseases.
The duration of arrhythmias was short, in most cases, up to 10 minutes, but repetitive: daily, at 1-3 days, weekly or sometimes, at several weeks.
The presence of cardiac arrhythmias imposed current activity diminution in a number of 36 subjects (50%) or even cessation in 25 (35%), while a lesser number of subjects, 11 (15%), continued their work, but with anxiety (5).
Figure 5.
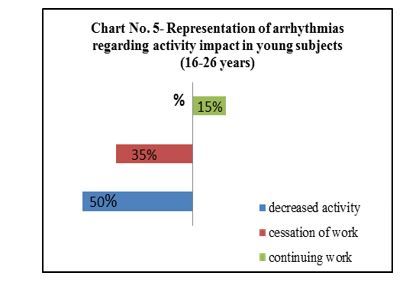
Activity impact
This condition had repercussions and impact over professional performances, leading to installation of attention disorders and decreasing the quality of life in 62 subjects (33% of the entire investigated group of subjects), (6 ).
Figure 6.
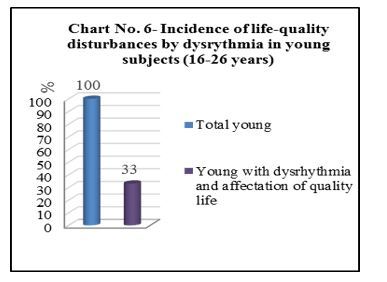
Life-quality disturbances by dysrythmia
Profile of cardiac arrhythmias in the studied young subjects of group I, consisted of the following types: atrial extrasystolic arrhythmia in 13 subjects (representing 18%), ventricular extrasystolic arrhythmia in 12 (17%), sinus tachycardia in 13 (18%), paroxysmal atrial fibrillation in 11 (15%), paroxysmal supraventricular tachycardia in 10 (14%), atrial flutter in 4 (6%), sinus bradycardia in 2 (3%), associated dysrhythmias (for example: atrial and ventricular extrasystolic arrhythmias, extrasystoles with tachycardia or bradycardia) in 7 (10%), (5), (7).
Table 5.
Representation of dysrhythmias aspects in the studied young subjects
Type of arrhythmia |
Number of subjects |
Percentage (%) |
extrasystolicatrialarrhythmia |
13 |
18 |
sinus tachycardia |
13 |
18 |
extrasystolic ventriculararrhythmia |
12 |
16 |
paroxysmal atrial fibrillation |
11 |
15 |
paroxysmal supraventricular tachycardia |
10 |
14 |
atrial flutter |
4 |
6 |
sinus bradycardia |
2 |
3 |
associated dysrhythmias |
7 |
10 |
Figure 7.
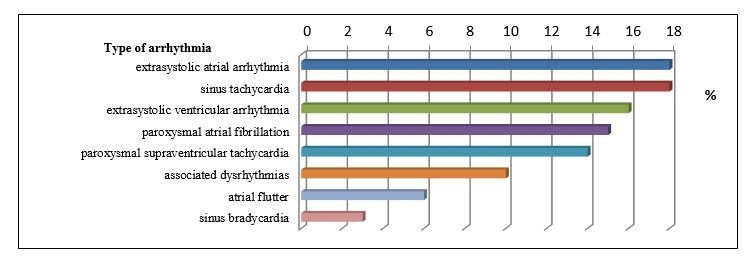
Incidence profile of arrhythmias in the studied young subjects
From seemingly functional arrhythmias, in the presence of risk factors, persistent oxidative modifications may be achieved, which, although clinically inapparent, can determine important cardiac pathologies in future adults and elders.
In the presence of oxidative stress markers positivity, in young persons with cardiovascular risk and family predisposition, recommendations for correcting risk factors, both clinical and biochemical are useful, associated also with proper monitoring of this corrections, for an effective long-term primary prevention.
Discussion
Heart rhythm disturbances in young people are often subject to a number of risk factors that, through their prolonged or repetitive action, may cause modifications of tissue oxidative status and for this reason, the absence or lack of antioxidant preventive measures may lead to further repercussions, by inducing subclinical lesions, especially at the level of endothelium.
Although rhythm disorders causality is sometimes imprecisely etiological defined, arrhythmogenic favoring conditions are important to be studied, especially in situations when they sum (more risk factors) and when they are probably involved in creating a myocardial oxidative status, enabling arrhythmogenic reentry circuits and leading to a modified redox system.
The study of clinical factors in young patients with arrhythmias, precedes imaging and biochemical determinations and is useful for creating a risk score and its grading (outline of a risk orientation map). In the case of an increased risk, with cumulative factors, it is desirable, at these patients, in addition to the careful investigation of the nature and mechanism for the production of arrhythmias, to determine the biochemical and metabolic markers of oxidative stress. They could determine, on one side, the involvement of clinical risk factors and, on the other side, the establishment of therapeutic dietary, medical or behavior measures, in order to reduce cardiovascular risk.
Arrhythmogenic risk, as shown by the study, is influenced by a number of clinical factors such as, in order of incidence: coffee consumption, the presence of stress, physical effort, energy drinks comsumption, high-fat diet, hereditary predisposition, alcohol intake, sleep deprivation, smoking, overweight, diet rich in fruits/vegetables, underweight, diet poor in antioxidants and with multiple oxidative and metabolic action, including at cardiovascular system level.
Activity influence of young people by the appearance of arrhythmias requires proper evaluation, initially clinical and further, targeted in all aspects, including data related to oxidative stress and modulation possibilities.
A number of studies demonstrate the causal relationship between some risk factors and the occurrence of oxidative stress [11], [2], [3], [8].
Treatment through a well balanced diet, rich in antioxidants or through medication is useful in young subjects, in the presence of cardiac rhythm disturbances and arrhythmia risk factors generating oxidative stress, demonstrated by specific biomarkers. The recording of oxidative stress markers variation in subjects with proarrhythmic risk factors and various arrhythmias, especially in a demonstrably frame through genetic polymorphism, justifies the investigational, diagnostic, therapeutic and evolution management.
Conclusion
1. Heart rhythm disorders are present in 39 % of the studied young people aged 16-26 years, 3 out of 4 women and 1 out of 3 males presenting arrhythmias, the quality of life being also affected in 33% of them.
2. Risk factors predisposing to arrhythmias, observed in the studied young subjects were, in order of incidence: coffee consumption- 82%, presence of stress- 80%, physical effort- 72%, consumption of energy drinks-72%, diet rich in proteins/ lipids- 69%, hereditary predisposition- 69%, alcohol intake-53%, frequent sleep deprivation- 50%, smoking- 31%.
3. In young subjects, the association of dysrhythmias with oxidative status modifying condition was observed.
4. Clinical aspects promote cardiac arrhythmias and at the same time lead to oxidative imbalances, causing endothelial modifications and early development of atherosclerotic lesions.
5. In the presence of arrhythmias and clinical risk factors, determination of oxidative stress biomarkers and genetic polymorphisms of involved enzymes is important and useful in order to establish the justified necessary of antioxidants supply and the primary prevention of future cardiovascular diseases.
Acknowledgments
This paper was published under the frame of European Social Found, Human Resources Development Operational Programme 2007-2013, project no. POSDRU/159/1.5/S/136893.
References
- 1.Bohm M, Reil JC, Deedwania P, et al. Resting Heart Rate: Risk Indicator and Emerging Risk Factor in Cardiovascular Disease. Am J Med. 2015;128:219–219. doi: 10.1016/j.amjmed.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 2.Bonilla IM, Sridhar A, Gyorke S, Cardounel AJ, Carnes CA. Nitric oxide synthases and atrial fibrillation. Front Physiol. 2012;3:105–105. doi: 10.3389/fphys.2012.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dilaveris P, Pantazis A, Gialafos E, Triposkiadis F, Gialafos J. The effects of cigarette smoking on the heterogeneity of ventricular repolarization. Am Heart J. 2001;142:833–837. doi: 10.1067/mhj.2001.118737. [DOI] [PubMed] [Google Scholar]
- 4.Dhingra R, Sullivan LM, Fox CS, et al. Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med. 2007;167:879–879. doi: 10.1001/archinte.167.9.879. [DOI] [PubMed] [Google Scholar]
- 5.Ekelund LG, Haskell WL, Johnson JL, et al. Physical fitness as a predictor of cardiovascular mortality in asymptomatic North American men. The Lipid Research Clinics Mortality Follow-up Study. N Engl J Med. 1988;319:1379–1379. doi: 10.1056/NEJM198811243192104. [DOI] [PubMed] [Google Scholar]
- 6.Foley RN, Collins AJ, Herzog CA, et al. Serum phosphorus levels associate with coronary atherosclerosis in young adults. J Am Soc Nephrol. 2009;20:397–397. doi: 10.1681/ASN.2008020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–89. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 8.Wilson WF, Cannon CP, Downey BC FACC. Overview of the possible risk factors for cardiovascular disease [Google Scholar]
- 9.Hackam DG, Anand SS. Emerging risk factors for atherosclerotic vascular disease: a critical review of the evidence. JAMA. 2003;290:932–932. doi: 10.1001/jama.290.7.932. [DOI] [PubMed] [Google Scholar]
- 10.Heitzer T, Schlinzig T, Krohn K, et al. Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation. 2001;104:2673–2673. doi: 10.1161/hc4601.099485. [DOI] [PubMed] [Google Scholar]
- 11.Hill JM, Zalos G, Halcox JP, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348:593–593. doi: 10.1056/NEJMoa022287. [DOI] [PubMed] [Google Scholar]
- 12.Ho JE, Larson MG, Ghorbani A, et al. Long-term cardiovascular risks associated with an elevated heart rate: the Framingham Heart Study. J Am Heart Assoc. 2014;3:e000668–e000668. doi: 10.1161/JAHA.113.000668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeong EM, Liu M, Sturdy M, et al. Metabolic stress, reactive oxygen species, and arrhythmia. J Mol Cell Cardiol. 2012;52:454–463. doi: 10.1016/j.yjmcc.2011.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kannel WB, Kannel C, Paffenbarger RS Jr, Cupples LA. Heart rate and cardiovascular mortality: the Framingham Study. Am Heart J. 1987;113:1489–1489. doi: 10.1016/0002-8703(87)90666-1. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1973. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 16.Khan AM, Lubitz SA, Sullivan LM, et al. Low serum magnesium and the development of atrial fibrillation in the community: the Framingham Heart Study. Circulation. 2013;127:33–33. doi: 10.1161/CIRCULATIONAHA.111.082511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–2024. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 18.Marcus BH, Albrecht AE, King TK, et al. The efficacy of exercise as an aid for smoking cessation in women: a randomized controlled trial. Arch Intern Med. 1999;159:1229–1229. doi: 10.1001/archinte.159.11.1229. [DOI] [PubMed] [Google Scholar]
- 19.Rennison JH, Van Wagoner DR. Impact of dietary fatty acids on cardiac arrhythmogenesis. Arrhythm Electrophysiol. 2009;2:460–469. doi: 10.1161/CIRCEP.109.880773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schmidt-Lucke C, Rossig L, Fichtlscherer S, et al. Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation. 2005;111:2981–2981. doi: 10.1161/CIRCULATIONAHA.104.504340. [DOI] [PubMed] [Google Scholar]
- 21.Song Y, Manson JE, Cook NR, et al. Dietary magnesium intake and risk of cardiovascular disease among women. Am J Cardiol. 2005;96:1135–1135. doi: 10.1016/j.amjcard.2005.06.045. [DOI] [PubMed] [Google Scholar]
- 22.Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341–1341. doi: 10.1056/NEJMra0912063. [DOI] [PubMed] [Google Scholar]
- 23.Werner N, Kosiol S, Schiegl T, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005;353:999–999. doi: 10.1056/NEJMoa043814. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Post WS, Dalal D, Blasco-Colmenares E, Tomaselli GF, et al. Coffee, Alcohol, Smoking, Physical Activity and QT Interval Duration: Results from the Third National Health and Nutrition Examination Survey. PLoS ONE. 2011;6(2):e17584–e17584. doi: 10.1371/journal.pone.0017584. [DOI] [PMC free article] [PubMed] [Google Scholar]


