Abstract
In sub-Saharan Africa, men who have sex with men (MSM) experience high HIV prevalence, in part, due to stigma and discrimination creating barriers to engagement in prevention and care services. We examined the reliability and validity of measures of stigma and satisfaction with healthcare providers, as well as explored whether scores on the factors varied across sociodemographic variables among MSM in western Kenya. A mixed-methods design using a sequential triangulation approach was adopted, involving a survey of 89 MSM and 10 key informant interviews. Reliability and correlation analyses, exploratory factor analyses, t-tests, and ANOVAs (analyses of variances) were conducted to test the scale's psychometric properties and examine differences in mean scores by demographics. Thematic analysis with qualitative data was used to validate the meaning of scales and explore how stigma influences and relates to satisfaction with healthcare providers. Of 89 participants, 50% identified as homosexual, 52% had college degree, 45% were above 25 years, and 72% had ever been married. Three subscales measuring enacted stigma, internalized stigma, and mistrust of healthcare providers showed good reliability (α = 0.80, α = 0.90, and α = 0.90). Men who identified as homosexual reported higher mean scores of enacted stigma and distrust of healthcare providers compared to heterosexual/bisexual identified (p < 0.001). Qualitative data revealed perceptions that healthcare providers were not knowledgeable to handle MSM needs. Study provides preliminary evidence for the reliability and validity of measures of stigma and mistrust of healthcare providers in Kenya. Quantitative and qualitative findings highlight the need for interventions to reduce stigma and create a more inclusive health system.
Keywords: : MSM, healthcare, providers, HIV, stigma, Kenya
Introduction
In sub-Saharan Africa, men who have sex with men (MSM) continue to experience significantly higher prevalence of HIV than other groups.1–3 For example, in Kenya, HIV prevalence among MSM is almost thrice that of the general population, with the most recent national estimates of HIV infection being 18.2% among MSM compared to the general population estimate of 5.9%.4 Yet, despite the high HIV prevalence MSM disproportionately lack access to HIV prevention and treatment services. Consequently, MSM lag behind in benefiting from ongoing advances in HIV treatment, which in turn has an impact on the ability of antiretroviral therapy to prevent incident cases.
Laws criminalizing same sex sexual practices, relationships, and identities, as well as a lack of legal protection for lesbian, homosexual, bisexual, and transgender (LGBT) persons, from discrimination impede access to HIV prevention and treatment services among MSM in sub-Saharan Africa and in Kenya specifically.5–9 Given that many people in Kenya, including healthcare providers, harbor stigmatizing attitudes and beliefs against those infected with HIV, HIV-positive MSM may suffer layered stigma related to their sexuality and their HIV status, which may compromise their ability to seek HIV treatment and care services.10,11 Prior studies have shown that MSM in Sub-Saharan Africa (SSA) who report high levels of stigma are more likely to have poor access to care and health outcomes.9,12,13 Many MSM choose to remain invisible due to their fear of negative reactions from healthcare providers, arrest, or violence.5,6,8,14–19
Healthcare providers acknowledge that they foster negative judgments toward MSM, despite their ethical obligation to care for and treat people impartially.7 Judgmental attitudes toward MSM are particularly present among SSA healthcare providers with conservative cultural and religious beliefs.7,8 Improvements in access to HIV services for MSM in sub-Saharan Africa, alongside antidiscrimination and stigma reduction efforts, can significantly reduce new HIV infections both among MSM and the wider community.2 Current World Health Organization (WHO) guidelines call for the need to “reenergize and strengthen HIV programs so that key populations, including MSM, benefit from ongoing advances in HIV treatment.”20 Despite the large body of research describing forms of stigma related to MSM and HIV-related stigma, as well as the recognized need to develop stigma-reduction interventions in African healthcare settings, there are no known culturally appropriate instruments that have been validated for use among MSM in sub-Saharan African settings.21
A recent systematic review shows that studies measuring MSM-associated stigmas have been conducted predominantly in developed countries, with few studies conducted in low- and middle-income countries, including sub-Saharan Africa.21 To design interventions to improve access and uptake of HIV and other health services among MSM in sub-Saharan Africa, it is necessary to have culturally adequate measures of stigma and related factors among MSM. The aim of this study was to address this gap in the literature using a mixed-methods approach to examine the structure, reliability, and validity of instruments for measurements of stigma and trust in healthcare providers among MSM in Kenya. In addition, we explored whether stigma and distrust in healthcare provider scores varied by sociodemographic variables. This information could ultimately be used to guide the development of tailored interventions targeting demographic groups with higher scores of stigma and distrust of healthcare providers.
Methods
The current study used a mixed-method convergence model design,22 incorporating separate phases of quantitative and qualitative data collection and then triangulating findings from the different sources of data. Based on the procedures of the model, the current analysis used quantitative methodology as the first step and qualitative methodology as the second step. Then, findings from the quantitative and qualitative methodologies were integrated during the final interpretation step to better understand the relationships among the study variables. For this research study, we first administered a structured quantitative survey to assess experiences of stigma and mistrust of healthcare providers among MSM in western Kenya and then conducted qualitative key informant interviews to further understand the meaning of the quantitative analysis. Qualitative data were also used to contextualize the findings to illustrate how stigma influences experiences with healthcare among MSM and trust of healthcare providers.
Study setting
The study was conducted in Eldoret Kenya, the fifth largest city in Kenya with a population of ∼218,446 people.23 Eldoret is home to one of Kenya's largest referral hospitals and is the site of the USAID-Academic Model Providing Access to Healthcare (AMPATH plus) program, the largest HIV clinical care program in Kenya which provides HIV-related services to over 150,000 patients.
Survey methods
Details of the methods of the quantitative survey are provided elsewhere.5 Briefly, the study focused on MSM, a term that refers to cis men who have sex with cis men, regardless of sexual orientation or gender identity, including transgender men, men who identify themselves as homosexual, and those who do not.24 Survey participants included men who were: (1) willing to participate in the survey; (2) ages 18 or more years; (3) reporting having anal or oral sex with a man within the previous 6 months; and (4) residing in Eldoret. The snowball sampling approach began with a set of initial participants recruited with the help of key informants and MSM who have disclosed their sexual orientation. Initial participants then referred members of their peer networks to the study. In total, 95 participants met eligibility criteria, and 89 completed the structured quantitative survey. The survey was administered by an interviewer in a private and secure space. Each questionnaire lasted ∼40 min. Participants received Kshs.150 ($1.50 USD) reimbursement at the end of each interview session. They were also informed about available free care for HIV at Moi Teaching and Referral Hospital and other healthcare facilities in Eldoret. All study procedures were approved by the Moi University College of Health Sciences and Moi Teaching and Referral Hospital Institutional Research and Ethics Committee (IREC Approval No. 0001107). All participants provided written informed consent to participate.
Survey measures
The survey instrument used in this study was adapted from Behavioral Surveillance Surveys for populations with high HIV prevalence.25 The survey assessed a variety of topics; for this analysis, we focused on questions related to enacted stigma, internalized stigma, and perceptions about healthcare providers and sociodemographic characteristics. Demographic characteristics included age, income, education, sexual orientation, and marital status.
Enacted stigma
Enacted stigma was assessed with a 12-item measure that included items about MSM perceptions and experiences of interpersonal negativity and discrimination related to their sexuality, including the experience of being mistreated (e.g., “Someone was unwilling to share a meal with you?”) and the experience of social avoidance by others because of sexual identity (e.g., “Someone was unwilling to be your neighbor?”). Responses were rated on a 4-point frequency scale (“0 = never” to “3 = often”).
Internalized stigma
Participant experiences of internalized stigma were assessed using seven items. Sample items included: “I hang with the wrong crowd because I am a MSM” and “I should be ashamed of being MSM.” Four-point Likert scale response options ranged from “strongly agree” (3) to “strongly disagree” (0).
Mistrust of healthcare providers
Participants completed a seven-item measure that assessed their comfort in accessing healthcare services. Sample items included “I feel comfortable discussing my sexual practices with the healthcare provider” and “I feel safe discussing my sexual orientation with the healthcare provider.” Responses ranged from “strongly agree” (0) to “strongly disagree” (3). One item was reverse-coded “I feel like my healthcare provider does not have adequate knowledge about MSM.”
Quantitative data analysis
Quantitative data were analyzed using exploratory statistical analysis. Initially, we conducted an exploratory factor analysis with all 26 items from the 3 stigma measures. Exploratory factor analysis was completed using maximum likelihood estimation to allow for missing data and Direct Oblimin rotation, an oblique method of rotation that assumed the factors were correlated. The correlation matrix and factor loadings, as well as a scree plot, were used to decide the number of factors and which items to retain. We specified a priori that items with factor loadings of 0.40 or higher and uniqueness values of 0.80 or below would be included. Subsequent analyses were run constraining the model to three factors. The factor structure of the exploratory factor analysis was examined to determine whether factor loadings reflected the unique constructs of enacted stigma, internalized stigma, and dissatisfaction with healthcare provider. Subscale scores were computed by summing up the scores across the items with higher scores indicating higher levels of enacted stigma, internalized stigma, and dissatisfaction with healthcare provider. Internal consistency reliability for each subscale score was evaluated using Cronbach's alpha. We hypothesized that mean stigma and mistrust of healthcare provider scores would be significantly higher among men who identify as homosexual compared to those who identified as heterosexual and bisexual. We also conducted ANOVA (analyses of variance) and t-tests to test differences in mean scores from the resulting subscales by certain sociodemographic factors of interest, including age, sexual orientation, income, marital status, and education. All statistical analyses were performed using STATA, version 14.
Qualitative methods
Qualitative interviews were conducted among 10 key informants with experience working with MSM, but they were not required to be MSM. We purposively selected 10 key informants from Eldoret and its environs. Key informants included MSM activists, healthcare providers providing care to MSM, patrons at gay clubs, MSM peer educators, and MSM advocates. Interview topics included: healthcare access and challenges faced by MSM in Kenya, contextual information on MSM, and HIV-related services for MSM. Participants received 200 Kenya Shillings (approximately $3 USD) compensation. Each interview lasted about an hour, was digitally recorded, and was transcribed verbatim. Interviewers also took detailed notes during each interview and wrote an interview synopsis directly after completing the interview. Qualitative data were analyzed using QSR International's NVivo v.11. Interview transcripts were analyzed using thematic analysis to identify, examine, and record patterns (or themes) within data, based on steps described in Braun and Clarke.26 The coding was performed by two independent coders, and analysis and interpretation were performed by the full study team.
Integration of quantitative and qualitative results (triangulation)
We used a sequential explanatory strategy that first involved analysis of quantitative data followed by analysis of qualitative data to better understand preliminary quantitative results. The final analysis involved integration of both quantitative and qualitative data to identify convergence and divergence of results.
Results
Sample characteristics
Table 1 shows the characteristics of the survey sample. Approximately half (51%) of participants were between the ages of 18 and 24. Approximately one-third of the sample was married, and more than half (60%) had monthly income of less than 5000 Kenyan shillings ($50 USD). Fifty percent self-identified as “homosexual,” while 35% described themselves as “bisexual” and 15% identified as “heterosexual.” The majority of the sample had children (80%) and had at least a university or college degree (58%).
Table 1.
Sample Characteristics of the Respondents (N = 89)
| Characteristics | n (%) |
|---|---|
| Age group in years | |
| 18–24 | 46 (51.69) |
| ≥25 | 43 (48.31) |
| Sexual orientation identity | |
| Bisexual | 31 (35.23) |
| Homosexual | 44 (50.00) |
| Heterosexual | 13 (14.77) |
| Income monthly | |
| <5000 | 46 (59.74) |
| ≥5000 | 31 (40.26) |
| Relationship status | |
| Single | 55 (67.9) |
| Married | 28 (33.73) |
| Ever been married to a woman | |
| Yes | 72 (80.9) |
| No | 17 (19.1) |
| Have children | |
| Yes | 67 (79.76) |
| No | 17 (20.24) |
| No. of children, mean (SD) | 1.9 (0.28) |
| Education | |
| No college degree | 37 (41.57) |
| College/university degree | 52 (58.43) |
SD, standard deviation.
Factor structure
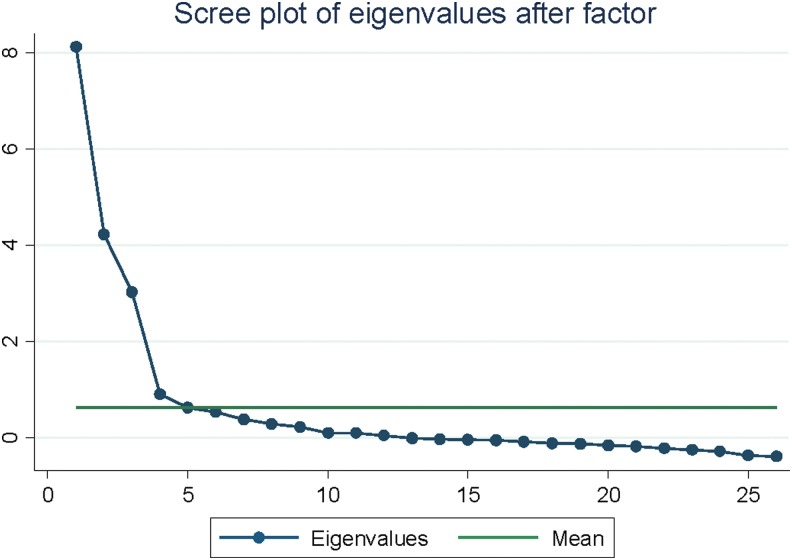
First, we examined the suitability of the survey items for factor analysis. The Kaiser-Meyer-Olkin value of 0.70 was above the recommended value of 0.60 for factor analysis,27 and Bartlett's test of sphericity was significant (χ2 = 1257.8, df = 325, p < 0.001) indicating good sampling adequacy for factor analysis. Table 2 shows all 26 items that were included in the initial assessment of stigma and satisfaction with healthcare provider among MSM. Four items did not load on any factor (factor loading <0.40) and were therefore excluded from future analysis leaving 22 items. These items were as follows: (1) someone considered MSM as people who are unnecessarily draining medical/economic resources in the country, (2) someone at the health facility was unwilling to serve you because you are MSM, (3) I hang with the wrong crowd because I am a MSM, and (4) I am afraid to share my sexual orientation with others. Exploratory factor analysis (EFA) indicated that this model was characterized by three strong factors with factor loadings of 0.40 and above (Fig. 1, scree plot). Therefore, the three-factor model was retained. Ten items that loaded on factor 1 represent enacted stigma. Seven items that loaded on factor 2 represent mistrust of healthcare providers, and finally, five items that loaded on factor 3 represent internalized stigma.
Table 2.
Item Factor Loading Patterns
| Item | Factor 1 | Factor 2 | Factor 3 | Uniqueness |
|---|---|---|---|---|
| Someone was unwilling to share a meal with youa | 0.77 | 0.28 | 0.18 | 0.30 |
| Someone was unwilling to live with youa | 0.79 | 0.21 | 0.16 | 0.31 |
| Someone was unwilling to be your neighbora | 0.65 | 0.25 | 0.39 | 0.35 |
| Someone was unwilling to employ you/have you employeda | 0.60 | 0.24 | 0.07 | 0.57 |
| Someone was unwilling to have you interact with childrena | 0.72 | 0.18 | 0.24 | 0.40 |
| Someone was unwilling to be your frienda | 0.79 | 0.07 | −0.21 | 0.32 |
| Someone was unwilling to socialize with youa | 0.87 | 0.09 | −0.17 | 0.21 |
| Someone has scandalized your physical appearance and dressinga | 0.77 | 0.10 | −0.34 | 0.27 |
| Someone refused to associate with you saying you can corrupt them with your MSM lifestylea | 0.87 | 0.12 | −0.08 | 0.23 |
| Someone expressed doubts regarding your ability to make social contribution as an MSMa | 0.61 | −0.03 | −0.22 | 0.58 |
| Someone considered MSM a people who are unnecessarily draining medical/economic resources in the countrya | 0.33 | −0.19 | −0.27 | 0.78 |
| Someone at the health facility was unwilling to serve you because you are MSMa | 0.40 | 0.28 | −0.07 | 0.75 |
| I hang with the wrong crowd because I am a MSMb | 0.22 | 0.09 | 0.24 | 0.88 |
| I should be ashamed of being a MSMb | 0.02 | 0.13 | 0.82 | 0.32 |
| Being a MSM means I have been irresponsibleb | −0.03 | −0.11 | 0.83 | 0.30 |
| Being a MSM shows I lack self-controlb | −0.10 | −0.05 | 0.82 | 0.31 |
| I should be avoided because I am a MSMb | −0.02 | 0.03 | 0.71 | 0.49 |
| I have poor morals because I am a MSMb | −0.03 | 0.01 | 0.82 | 0.32 |
| I am afraid to share my sexual orientation with othersb | 0.19 | 0.07 | −0.22 | 0.91 |
| I feel comfortable discussing my sexual practices with the healthcare providerc | 0.09 | 0.85 | 0.02 | 0.27 |
| I feel safe discussing my sexual orientation with the healthcare providerc | 0.20 | 0.91 | 0.00 | 0.14 |
| I am comfortable asking the healthcare provider questions about my healthc | 0.19 | 0.81 | 0.01 | 0.31 |
| The healthcare provider understands my problems wellc | 0.31 | 0.83 | 0.11 | 0.20 |
| I feel like my confidence is protected during the meeting with the healthcare providerc | 0.20 | 0.92 | −0.01 | 0.11 |
| I feel like the healthcare provider does not have adequate knowledge about MSMc | −0.05 | 0.40 | −0.08 | 0.84 |
| I feel like the healthcare provider answers my questions wellc | 0.31 | 0.81 | 0.21 | 0.21 |
Table shows the factor loadings of each item. Bold items and numbers indicate items that fall under 0.4.
Enacted stigma.
Internalized stigma.
Mistrust of healthcare provider.
MSM, men who have sex with men.
FIG. 1.
Scree plot for ML analysis of the scale. ML, maximum likelihood factor.
Internal consistency reliability
Table 3 presents response frequencies for each item within the three subscales and Cronbach's alphas for each subscale. Cronbach's alpha was α = 0.80 for enacted stigma, α = 0.90 for internalized stigma, and α = 0.90 for mistrust of healthcare provider. Overall, the mean scores were 7.0 [standard deviation (SD) = 6.1] for enacted stigma, 3.2 (SD = 3.1) for internalized stigma, and 11.0 (SD = 5.6) for mistrust of healthcare provider.
Table 3.
Response to Items from the Three Subscales (Frequencies), Cronbach's Alpha for Reliability of Subscales, and Mean and Standard Deviation of Total Subscale Scores
| Item | Never | Rarely | Sometimes | Often | α | Mean (SD) |
|---|---|---|---|---|---|---|
| Social stigma | 0.80 | 7.0 (6.1) | ||||
| Someone was unwilling to share a meal with you | 64 | 20 | 12 | 4 | ||
| Someone was unwilling to live with you | 53 | 12 | 30 | 4 | ||
| Someone was unwilling to be your neighbor | 65 | 11 | 22 | 2 | ||
| Someone was unwilling to employ you/have you employed | 74 | 12 | 13 | 1 | ||
| Someone was unwilling to have you interact with children | 65 | 19 | 14 | 2 | ||
| Someone was unwilling to be your friend | 43 | 22 | 32 | 3 | ||
| Someone was unwilling to socialize with you | 42 | 20 | 35 | 3 | ||
| Someone has scandalized your physical appearance and dressing | 49 | 14 | 34 | 2 | ||
| Someone refused to associate with you saying you can corrupt them with your MSM lifestyle | 51 | 22 | 23 | 5 | ||
| Someone expressed doubts regarding your ability to make social contribution as an MSM | 61 | 24 | 11 | 4 | ||
| Strongly disagree | Disagree | Agree | Strongly agree | |||
|---|---|---|---|---|---|---|
| Self-stigma | 0.90 | 3.2 (3.1) | ||||
| I should be ashamed of being a MSM | 47 | 37 | 11 | 5 | ||
| Being a MSM means I have been irresponsible | 44 | 45 | 8 | 3 | ||
| Being a MSM shows I lack self-control | 51 | 38 | 9 | 2 | ||
| I should be avoided because I am a MSM | 54 | 42 | 1 | 3 | ||
| I have poor morals because I am a MSM | 51 | 43 | 3 | 2 |
| Strongly agree | Agree | Disagree | Strongly disagree | |||
|---|---|---|---|---|---|---|
| Mistrust of HCP | 0.90 | 11.0 (5.6) | ||||
| I feel comfortable discussing my sexual practices with the healthcare provider | 22 | 24 | 33 | 21 | ||
| I feel safe discussing my sexual orientation with the healthcare provider | 15 | 26 | 41 | 18 | ||
| I am comfortable asking the healthcare provider questions about my health | 20 | 26 | 36 | 18 | ||
| The healthcare provider understands my problems well | 15 | 29 | 35 | 21 | ||
| I feel like my confidence is protected during the meeting with the healthcare provider | 20 | 30 | 33 | 16 | ||
| I feel like the healthcare provider does not have adequate knowledge about MSMa | 25 | 27 | 35 | 13 | ||
| I feel like the healthcare provider answers my questions well | 18 | 28 | 35 | 19 |
Reverse code.
α, Cronbach's alpha; MSM, men who have sex with men; SD, standard deviation.
Correlations between the subscales
Pearson's correlation showed enacted stigma and distrust of healthcare subscales, which were moderately positively correlated (r = 0.41, p = 0.001). However, internalized stigma was not correlated with enacted stigma or distrust of healthcare providers (r = 0.01, p = 0.98; r = 0.12, p = 0.31).
Subgroup differences in enacted stigma, internalized stigma, and mistrust of healthcare providers
To examine subgroup differences on the three measures, we examined mean score differences according to sexual identity and sociodemographic factors (Table 4). There were statistically significant mean differences in enacted stigma and mistrust of healthcare provider by sexual orientation identity. Men who identified as homosexual reported higher enacted stigma levels than those who identified as heterosexual and bisexual (10.0 vs. 8.0 vs. 3.0, p < 0.001). In addition, men who had ever been married to a woman reported lower levels of enacted stigma than those who had never married a woman (3.0 vs. 8.0, p < 0.001). We also observed statistically significant differences in mistrust with healthcare providers. Men who identified as homosexual had higher mean scores of mistrust of healthcare providers (15.0 vs. 7.8 vs. 11.2, p < 0.001) than those who self-identify as bisexual and heterosexual, respectively. However, there were no statistically significant mean differences in internalized stigma by any sociodemographic characteristics (age, income, level of education, and relationship status) that we examined.
Table 4.
Summary of Final Subscale Mean Scores by Sociodemographic Characteristics
| Characteristics | Social stigma (n = 10 items), mean (SD) | Internalized stigma (n = 5), mean (SD) | Mistrust of HCPs (n = 7 items), mean (SD) |
|---|---|---|---|
| Age group in years | |||
| 18–24 | 8.0 (6) | 3.2 (3) | 10.0 (5) |
| >25 | 6.0 (6) | 3.0 (2) | 11.5 (5) |
| Sexual orientation identity | |||
| Bisexual | 3.0 (4) | 3.0 (2) | 7.8 (4.2) |
| Homosexual | 10.0 (6)*** | 3.3 (3) | 15.0 (3)*** |
| Heterosexual | 8.0 (5) | 2.7 (2) | 11.2 (6) |
| Income monthly | |||
| <5000 | 8.0 (6) | 3.3 (3) | 10.2 (5) |
| >5000 | 6.0 (5) | 2.7 (2) | 11.0 (5) |
| Relationship status | |||
| Single | 8.0 (6) | 3.2 (3.1) | 11.2 (5) |
| Married | 6.0 (5) | 2.5 (2.7) | 10.0 (5) |
| Ever been married to a woman | |||
| Yes | 3.0 (3)*** | 3.4 (2) | 11.0 (5) |
| No | 8.0 (6) | 3.1 (2) | 11.0 (5) |
| Education | |||
| No college degree | 6.0 (6) | 3.0 (3) | 10.2 (6) |
| University or college | 7.0 (6) | 3.0 (3) | 11.0 (5) |
p < 0.001, **p < 0.01, *p < 0.05.
SD, standard deviation.
Qualitative findings
The quantitative analysis of the survey items resulted in a final scale with three factors: enacted stigma, internalized stigma, and mistrust of healthcare providers. Based on thematic analysis of our qualitative findings, we found convergence across quantitative and qualitative data, such that the primary themes identified through qualitative analysis were consistent with the factors derived through quantitative analysis. Below we present direct quotes illustrating these themes.
Enacted stigma
Participants described stigma as one of the issues that negatively affects the health and well-being of MSM, including health-seeking behaviors. The quantitative analysis showed higher levels of enacted stigma among men who identified as homosexual compared to other groups (heterosexual or bisexual). The qualitative data support this finding. One of the participants noted that discrimination at societal and interpersonal level leads to social exclusion of MSM.
“There was one time [we] were in a pub drinking, then the owner just got in started saying ‘I do not want homosexuals in my pub, if you see them throw them out’.” [Peer leader 1]
Other participants echoed this sentiment by describing MSM experiences of stigma at the interpersonal level:
“There was a guy who told me he had straight friend. Then when they found out that he was homosexual they run away from him.” [Provider 1]
“People will not want to talk to you or walk with you just because you are MSM. They won't even leave you with their children because they think you will influence them. They think that being a MSM is only about sex. People think that we only think about sex and nothing else. We also contribute to the society.” [Peer leader 4]
Mistrust of healthcare provider
The quantitative analysis showed that men who identified as homosexual reported greater mistrust of healthcare providers compared with other sexual identities. This result is supported by several subthemes that emerged in qualitative data. Four themes on healthcare providers were identified as follows: healthcare provider prejudice, lack of knowledge and skills, cultural norms, and heteronormative assumptions.
Healthcare providers' prejudice
Participants described negative experiences between MSM and healthcare providers who expressed judgmental and stigmatizing attitudes and how these encounters discouraged them from seeking healthcare services. In some instances, participants expressed risk that providers would disclose their patients' sexual orientation to others in the community, including to patients' family members.
“I had one client, he told me he went to a certain facility. Then he explained about his situation that he was sick and he was an MSM. The doctor was so shocked and he chased him away. It's kind of embarrassing, you know. So at the end of it, he was scared to access the services.” [Provider 1]
“A large number of MSM have reported to us instances of discrimination or inappropriate reactions by health professionals, either experienced directly or by others they know. This was due to HIV status, sex orientation involvement, or the combination of both. There are instances of over-reaction by health care who even report these people to their parents.” [Peer leader 1]
“There are very few places if any that somebody would walk in and say hi am ‘MSM’ I have anal warts people will look at you like your sick that's a curse and stuff like. Many service providers are not aware of issues with regards to MSM.” [Peer leader 2]
Age of healthcare provider emerged as a determinant of how MSM received care. Participants noted that MSM preferred young healthcare providers than older healthcare providers. Young providers were friendlier compared to older healthcare providers who tend to play parental role and counsel MSM to change their way of life to fit with their beliefs.
“Most of the health care workers, especially the older ones, I think they see the MSM as their sons…You know it reaches a point where someone start to play parent while they are supposed to play nurse so it becomes really hard.” [Peer leader 3]
“If they don't play parent they play the role of a pastor, it never easy (laughs). They will start quoting the Bible or the Quran and tell you- my son this is not right, its un-African, but with younger service provider they are more exposed so it becomes easier to go to them.” [Peer leader 3]
MSM have also encountered discrimination by healthcare providers at clinical settings. For instance, one participant described experiences of MSM in public hospitals.
“Two young men appeared in a voluntary counseling and HIV testing center (VCT) and wanted to be tested as a couple, but they were sent away by the health care provider who wanted to even call the police for them.” [Administrator 1]
Lack of knowledge and skills
In addition to healthcare providers displaying judgmental attitudes, participants shared the view that healthcare providers are not equipped with the knowledge and skills necessary to provide MSM with appropriate services related to HIV, sexually transmitted infections (STIs), and other sexual health issues.
“Healthcare workers have limited information in terms of what are the real issues of HIV and AIDS among [the] MSM population, how can they prevent infection? what puts them at risk of an HIV infection in terms of MSM relations?” [Provider 3]
Another participant agreed with this statement by describing challenges MSM face when they visit healthcare facilities.
“There are very few health care places if any that somebody would walk in and say ‘Hi, I am MSM, I have anal warts…’ people would look at you like you are sick, cursed… many health care workers are not aware of these issues.” [Peer leader 1]
Social norms
One theme that emerged from healthcare provider attitudes toward MSM is related to cultural and social norms in this setting. The narratives from healthcare worker informants suggested that their moralizing, judgmental, and homoprejudicial attitudes are a result of social norms.
Another participant supported this sentiment:
“Moderator: would they find it difficult to be attended to in public facilities?”
“Respondent: it is tricky because we are talking about someone whose sexual behavior is not common in the community so they want to feel comfortable where they know someone understands and supports them.” [Administrator 2]
MSM are viewed as having a psychiatric disorder and the society thinks of them as outcasts largely because their behavior deviates from social norms.
“The society has not accepted MSM. They view them as cursed or morally pervaded beings.”[Peer leader 1]
Healthcare providers also acknowledged that their cultural beliefs and lack of exposure to other cultures influenced how they perceive and treat MSM:
“Most people are guided by those norms, so a health care worker who has travelled out and actually interacted with people from different settings has different views from a person who hasn't left the community.” [Peer leader 2]
Heteronormative assumptions
Heteronormativity emerged as another key barrier for MSM to access care. Many participants described that healthcare and prevention services focused on heterosexual relationships.
“Let me say AIDS messages are all over. The National AIDS Council and the Ministry of Health has put up and used all methods to communicate about HIV and related illness. However, MSM in Eldoret always complain that there is no message that targets them, it is for heterosexual.” [Administrator 2]
Another participant echoed this statement by describing health materials that are mainly targeted to one group—heterosexuals:
“Most of them [MSM] don't use protection and they complain that materials available are for heterosexuals. They are left out and always argue that they are not targeted or valued.” [Peer leader 1]
Discussion
The goals of this mixed-methods research were threefold: to examine the structure, reliability, and validity of measures of stigma and trust in healthcare providers among MSM in western Kenya; to examine subgroup differences among MSM in self-reported stigma and mistrust of healthcare providers; and to contextualize the findings with qualitative research. The final scale consisted of 22 items with 3 separate scales assessing enacted stigma, internalized stigma, and mistrust of healthcare providers. In addition, the scale demonstrated very good reliability.
Our results demonstrated that men who identified as homosexual reported higher mean scores of enacted stigma and mistrust of healthcare providers compared to men who identified as heterosexual/bisexual. However, we did not find any statistical differences in mean scores of internalized stigma by sociodemographic factors. Qualitative results supported these findings and revealed MSM experiences with healthcare providers who were perceived to have inadequate knowledge and competence to handle their healthcare needs. Narratives regarding providers who adopted cultural norms and endorsed enacted stigma directly to MSM were commonly reported as leading to discrimination of MSM. Another subtheme that emerged from the qualitative data included perceptions regarding a biased healthcare system focused exclusively on heterosexual needs. Healthcare providers were perceived by key informants to express bias when their own cultural, moral, or religious leanings conflicted with MSM reported behaviors. However, participants noted that younger healthcare providers demonstrated higher acceptance of MSM, possibly because of the ongoing discussions to protect the rights of LGBT, emergency of LGBT right movements in Kenya, and access to less stigmatizing views of LGBT through social media.
Our findings align with previous studies in African settings, including Kenya, where enacted stigma and medical mistrust have been described as key barriers to access to care among MSM.1,3,6,8,18 In qualitative studies conducted in the coastal region of Kenya, healthcare workers described their own attitudes toward MSM and demonstrated a lack of relevant knowledge, skills, and training to manage particular health needs of MSM.7,9 One study reported high levels of stigma and discrimination affecting MSM in communities and at healthcare facilities.9 In another study conducted in Kisumu in the western region of Kenya, over 60% of MSM reported discomfort when seeking health services at public hospitals.27 Our results expand on prior research by providing possible explanations for MSM discomfort with healthcare system. For example, MSM encounter healthcare providers who adopt cultural, social, and religious norms resulting in prejudice, discrimination, and judgmental views. In addition, among MSM, healthcare providers are perceived to lack knowledge and skills necessary to provide appropriate care. Unexpectedly our quantitative results found that internalized stigma was low and did not differ by demographic factors; moreover, we found no thematic evidence from qualitative narratives regarding internalized stigma affecting healthcare interactions among MSM. By contrast, other qualitative studies conducted in sub-Saharan Africa, including Kenya, reported on internalized stigma as a concern among MSM.8,9,15,18,28
This is among the first known studies in western Kenya examining stigma, healthcare systems, and health-seeking behaviors on MSM, which has been noted as a gap in the literature.21 As reviewed above, prior studies have documented that stigma and dissatisfaction with healthcare are known to be problems for MSM accessing care,7–9,28 but validated measures do not exist for this specific population. This study provides preliminary evidence for the reliability and validity of measures of stigma and mistrust of healthcare providers among MSM in Kenya. Specifically, this approach is appropriate in cultural settings in which same-sex sexual behavior is highly stigmatized, considering that general quantitative findings were elaborated and confirmed with qualitative findings from key informants who have worked with this population. Our findings fill the gap in literature on the need for additional validated stigma instruments from sub-Saharan Africa.21 We provide preliminary data that enacted stigma, internalized stigma, and mistrust in healthcare providers can be measured, assessed, and targeted as three components of stigmatizing behaviors in highly stigmatized settings. In addition, our qualitative findings showed that enacted stigma does not exist independently of competing contextual concerns, including the role of religious or social norms, HIV status, and sexual identity. Each of these factors has been shown to elicit stigmatizing reactions, including discriminatory behaviors and prejudicial attitudes in healthcare settings.29,30 We suggest further assessment of the intersectionality of stigma to inform future efforts to improve HIV prevention among sexual minority individuals.
There are limitations that should be acknowledged. First, the current analysis is a preliminary validation of stigma and healthcare provider satisfaction and, therefore, requires future validation and additional formative research. Although we provide evidence of content validity and internal consistency of these scales, we were not able to assess other forms of validity. We recommend future work with larger sample sizes to evaluate predictive, construct, concurrent, convergent, and other forms of validity. Second, this study was done in one region of Kenya and, as a result, our data may not be representative for all Kenyan MSM or MSM in sub-Saharan Africa. Therefore, a larger study covering more regions may be needed to further assess and validate these instruments for their representativeness across populations. Third, due to experiences of sexual stigma and discrimination, MSM who want to keep their sexual identities private may have opted not to participate in this study, thereby introducing selection bias. Fourth, more than half of the sample had a college or university degree, which is higher than the general levels of education completion in Kenya. The high levels of education in this sample might have affected findings on internalized stigma, as previous research has shown protective effects of higher education levels with regards to stigma, mental health, and HIV risk.31,32 Therefore, the low levels of internalized stigma found in our sample may not be representative of stigma among MSM in western Kenya. Different recruitment approaches may be needed to confirm and extend the results presented here. Finally, we used UNAIDS definition of the term MSM, which classifies men with differing gender expressions, sexual practices, and identities as one group. Although this grouping fits well in the Kenyan context where MSM have a range of gender expressions, identities, and sexual practices, this grouping is problematic with regard to tailoring interventions. Patient-centered interventions are more likely to be effective than group interventions. In addition, our study survey used “homosexual” as one of the categories of sexual orientation identity, which may not be a term commonly used in the Kenyan setting; we suggest that future surveys use terminology that may be more appropriate to the local language.
Despite these limitations, use of a mixed-methods approach provided contextual meaning of the scales beyond the quantitative findings. In addition, given emerging efforts to develop stigma reduction and healthcare training programs for addressing HIV among MSM in sub-Saharan Africa, this research measure can be used to evaluate effectiveness of HIV prevention and stigma reduction programs in Kenya or other countries in the region.
In conclusion, our findings highlight the need to reduce healthcare providers' stigma and increase their competence in providing care to MSM to address disparities in access to HIV prevention and treatment services. There is need for specific efforts to address judgmental attitudes among healthcare providers, providing them with the skills to provide the necessary support, counseling, and services to MSM population even when there is marked conflict with personally held moral views. In addition, there is need to use validated measures of stigma toward MSM and patients' satisfaction with healthcare providers in highly stigmatized settings in Kenya and elsewhere in sub-Saharan Africa.
Acknowledgments
This work was supported by the Moi University and VLIR-UOS University Development Cooperation and National Institute of Health (NIH) grant, Award Number NIH-NICHD R24-HD077976. The authors gratefully acknowledge all the study participants for taking part in the study. The authors also thank all the data entry personnel and administrative staff for the project facilitation and data management.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ayala G, Santos GM. Will the global HIV response fail gay and bisexual men and other men who have sex with men? J Int AIDS Soc 2016;19:21098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gall J, Sabin K, Frescoral L, Sabin ML, Erkkola T, Toskin I. Global trends of monitoring and data collection on the HIV response among key populations since the 2001 Declaration of Commitment on HIV/AIDS. AIDS Behav 2017;21:34–43 [DOI] [PubMed] [Google Scholar]
- 3.Smith AD, Tapsoba P, Peshu N, Sanders EJ, Jaffe HW. Men who have sex with men and HIV/AIDS in sub-Saharan Africa. Lancet 2009;374:416–422 [DOI] [PubMed] [Google Scholar]
- 4.National AIDS Control Council. Kenya AIDS Response Progress Report. 2016. Available at: http://nacc.or.ke/wp-content/uploads/2016/11/Kenya-AIDS-Progress-Report_web.pdf (Last accessed July5, 2018)
- 5.Shangani S, Naanyu V, Mwangi A, et al. . Factors associated with HIV testing among men who have sex with men in Western Kenya: A cross-sectional study. Int J STD AIDS 2017;28:179–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fay H, Baral SD, Trapence G, et al. . Stigma, health care access, and HIV knowledge among men who have sex with men in Malawi, Namibia, and Botswana. AIDS Behav 2011;15:1088–1097 [DOI] [PubMed] [Google Scholar]
- 7.van der Elst EM, Gichuru E, Omar A, et al. . Experiences of Kenyan healthcare workers providing services to men who have sex with men: Qualitative findings from a sensitivity training programme. J Int AIDS Soc 2013;16(Suppl 3):18741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duby Z, Nkosi B, Scheibe A, Brown B, Bekker L-G. ‘Scared of going to the clinic’: Contextualising healthcare access for men who have sex with men, female sex workers and people who use drugs in two South African cities. South Afr J HIV Med 2018;19:701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Micheni M, Kombo BK, Secor A, et al. . Health provider views on improving antiretroviral therapy adherence among men who have sex with men in coastal Kenya. AIDS Patient Care STDS 2017;31:113–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nyblade L, Reddy A, Mbote D, et al. . The relationship between health worker stigma and uptake of HIV counseling and testing and utilization of non-HIV health services: The experience of male and female sex workers in Kenya. AIDS Care 2017;29:1364–1372 [DOI] [PubMed] [Google Scholar]
- 11.Goyette M, Wamuti BM, Owuor M, et al. . Understanding barriers to scaling up HIV-assisted partner services in Kenya. AIDS Patient Care STDS 2016;30:506–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson CA. Off the Map. How HIV/AIDS Programming Is Failing Same-Sex Practicing People in Africa. New York: New York International Gay and Lesbian Human Rights Commission, 2007. [Google Scholar]
- 13.Stahlman S, Bechtold K, Sweitzer S, et al. . Sexual identity stigma and social support among men who have sex with men in Lesotho: A qualitative analysis. Reprod Health Matters 2015;23:127–135 [DOI] [PubMed] [Google Scholar]
- 14.Eaton LA, Driffin DD, Kegler C, et al. . The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health 2015;105:e75–e82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogunbajo A, Kershaw T, Kushwaha S, Boakye F, Wallace-Atiapah ND, Nelson LE. Barriers, motivators, and facilitators to engagement in HIV care among HIV-infected Ghanaian men who have sex with men (MSM). AIDS Behav 2018;22:829–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maleke K, Daniels J, Lane T, Struthers H, McIntyre J, Coates T. How social stigma sustains the HIV treatment gap for MSM in Mpumalanga, South Africa. Glob Health Promot 2017. [Epub ahead of print]; DOI: 10.1177/1757975917737509 [DOI] [PubMed] [Google Scholar]
- 17.Wirtz AL, Kamba D, Jumbe V, et al. . A qualitative assessment of health seeking practices among and provision practices for men who have sex with men in Malawi. BMC Int Health Hum Rights 2014;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kushwaha S, Lalani Y, Maina G, et al. . “But the moment they find out that you are MSM…”: A qualitative investigation of HIV prevention experiences among men who have sex with men (MSM) in Ghana's health care system. BMC Public Health 2017;17:770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wanyenze RK, Musinguzi G, Matovu JK, et al. . “If You Tell People That You Had Sex with a Fellow Man, It Is Hard to Be Helped and Treated”: Barriers and opportunities for increasing access to HIV services among men who have sex with men in Uganda. PLoS One 2016;11:e0147714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO. UNAIDS. Global Update on HIV Treatment 2013: Results, Impact and Opportunities. Geneva: World Health Organization, 2013. [Google Scholar]
- 21.Fitzgerald-Husek A, Van Wert MJ, Ewing WF, et al. . Measuring stigma affecting sex workers (SW) and men who have sex with men (MSM): A systematic review. PLoS One 2017;12:e0188393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage Publications, 2017 [Google Scholar]
- 23.World Population View. Population of Cities in Kenya. 2018. Available at: http://worldpopulationreview.com/countries/kenya-population/cities (Last accessed March19, 2018)
- 24.UNAIDS. UNAIDS Terminology Guidelines. 2015. Available at: www.unaids.org/sites/default/files/media_asset/2015_terminology_guidelines_en.pdf (Last accessed July30, 2018)
- 25.Amon J, Brown T, Hogle J, et al. . Behavioral Surveillance Surveys, BSS. Guidelines for Repeated Behavioral Surveys in Populations at Risk of HIV. Arlington, Virginia: Family Health International (FHI), 2000 [Google Scholar]
- 26.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. Taylor & Francis 2006;3:77–101 [Google Scholar]
- 27.Tabachnick BG, Fidell LS. Using Multivariate Statistics. Boston, MA: Allyn & Bacon/Pearson Education, 2007 [Google Scholar]
- 28.Okall DO, Ondenge K, Nyambura M, et al. . Men who have sex with men in Kisumu, Kenya: Comfort in accessing health services and willingness to participate in HIV prevention studies. J Homosex 2014;61:1712–1726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stahlman S, Hargreaves JR, Sprague L, Stangl AL, Baral SD. Measuring sexual behavior stigma to inform effective HIV prevention and treatment programs for key populations. JMIR Public Health Surveill 2017;3:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson Shen M, Freeman R, Karpiak S, Brennan-Ing M, Seidel L, Siegler EL. The intersectionality of stigmas among key populations of older adults affected by HIV: A thematic analysis. Clin Gerontol 2018. [Epub ahead of print]; DOI: 10.1080/07317115.2018.1456500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andu E, Wagenaar BH, Kemp CG, et al. . Risk and protective factors of posttraumatic stress disorder among African American women living with HIV. AIDS Care 2018. [Epub ahead of print]; DOI: 10.1080/09540121.2018.1466981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cianelli R, Villlegas N, De Oliveira G, et al. . Predictors of HIV enacted stigma among Chilean women. J Clin Nurs 2015;24:2392–2401 [DOI] [PMC free article] [PubMed] [Google Scholar]