Abstract
The primary romantic relationship may offer critical opportunities for improving HIV care among key populations affected by high rates of HIV infection and low rates of care engagement, such as black men who have sex with men. A conceptual framework is needed to identify dyadic processes involved in addressing challenges in retention in care and adherence to antiretroviral therapy. This study conducted dyadic and individual-level qualitative analyses of individual interviews with men living with HIV from 14 black gay couples (n = 28). Interviews explored each partner's perspectives on challenges to and supportive strategies for retention in care and medication adherence. Findings highlighted challenges at various levels of care engagement and patterns of dyadic interactions that impeded or facilitated HIV care. Couple-level processes (i.e., couple's resilience, interdependence) underlined a joint problem-solving approach toward addressing challenges in care engagement. Findings support a conceptual framework of dyadic HIV care that highlights the impacts of dyadic and individual factors on coordination of care and treatment to influence retention and adherence. The generalizability of study findings is limited by the small sample size. Implications for intervention design include leveraging drivers of partner support, including couples' resilience, in enhancing joint problem-solving in HIV care among black gay couples.
Keywords: : dyadic HIV care, couple's resilience, joint problem-solving, primary relationship, black men who have sex with men, partner support
Introduction
Black men who have sex with men (MSM) represent approximately one quarter of all new HIV infections in the United States.1,2 Recent estimates indicate that 60% of black MSM will be HIV-positive by age 40.3 Stark disparities in retention in care and adherence to antiretroviral therapy (ART; i.e., HIV care) exist among black MSM.2,4–6 Poor HIV care predicts HIV-associated morbidity and mortality, and subsequent viremia can lead to forward transmission.2,7 Engagement in the HIV care continuum is necessary for people living with HIV to fully benefit from advances in ART.8 To achieve the National HIV/AIDS Strategy goals to lower HIV incidence, enhance health outcomes, and reduce health disparities, it is paramount to enhance HIV care and to reduce discontinuity of HIV care among the most underserved and vulnerable populations in the United States.9,10
Black MSM face a wide range of barriers to HIV care at multiple levels and may have few resources with which to address these challenges.2,9,11,12 Challenges and barriers include those at the individual level (e.g., mental illness, substance use),13–16 interpersonal level (e.g., negative relationship dynamics),17,18 social level (e.g., stigmatization associated with HIV, sexual orientation, race/ethnicity),2,19 and structural/systems level (e.g., access to services, patient–provider relationship).12,20 One common resource with which to address challenges in HIV care among black MSM is the primary relationship.21–23 A nationally representative sample of black MSM living with HIV found that almost half were in a primary relationship,24 yet, a preponderance of intervention research with black MSM has focused on individual-level barriers and facilitators, rather than those at the couple-level.25,26
The primary relationship may be a source of both support and challenge in chronic disease management. On the one hand, support from primary partners is associated with favorable HIV care and treatment outcomes.22,27–29 Partner support strategies range from helping one cope with the impact of an HIV diagnosis, reminding about appointments, setting out medication, coaching to build habits around taking medications, and monitoring adherence.18,30–32 According to dyadic models of stress and coping in chronic illness, partners perceive care engagement needs and evaluate appropriate coping strategies in offering support.28,31,33,34 These support strategies can change dynamically depending on the situation and the changing needs of the partner living with HIV.28
On the other hand, the primary partner may also present challenges in one's care engagement. Just as the adaptive, healthy behavior of a primary partner may influence one's own favorable health outcomes, the partner's beliefs and behavior may have negative impacts.35 Indeed, among black MSM, the primary relationship is inconsistently associated with favorable HIV care outcomes.36 Specifically, relative to single men, partnered black MSM were better retained in care but less adherent to ART.36 To understand the role of the primary relationship in care and treatment, more evidence is needed to elucidate dyadic processes in HIV care. Studies with MSM couples have emerged only recently to highlight how couples work together collaboratively to coordinate behaviors around HIV care and treatment activities.21,22,27,33
The goal of this study is to address the current evidence gap by exploring dyadic HIV care among black MSM in couples, using individual-level analyses of qualitative interviews to identify care engagement challenges and forms of partner support, and dyadic analysis to explore couple's dynamics around care engagement. While individual-level analysis of qualitative data allows a review of issues and behaviors across participants, dyadic or couple-level analysis of qualitative data allows exploration and comparison of each partner's perspectives on the same issue in the context of the relationship (e.g., medication adherence), providing a richer understanding of relationship dynamics around HIV care.37 When data from both partners are available, combining both individual- and couple-level qualitative analyses provides complementary information, just as combining both approaches would in the analysis of quantitative data from both members of the couple.
Methods
Recruitment and screening strategy
Purposive sampling was used to recruit black MSM and their primary partner as part of a larger study exploring the use of mobile technology to increase engagement in HIV care and treatment. Trained recruiters visited and distributed study materials at social venues (e.g., local bars, cafes) and AIDS service and community-based organizations serving black MSM in the San Francisco Bay Area. Recruitment materials contained a dedicated study phone number to contact study staff.
Potential participants were screened by phone for eligibility. Individuals were eligible if they identified as black or African American and a cisgender man at the time of the study; had a primary partner of 3 months or longer, a threshold commonly used in relationship research; was currently living with HIV; was between the ages of 18 and 65; owned a personal mobile telephone device; and was a resident of the San Francisco Bay Area. Individuals were excluded if their partner declined to participate. Inclusion criteria for the primary partner were as follows: identified as a cisgender man; reported the referring participant as their primary partner of 3 months or longer; was between the ages of 18 and 65; and resided in the Bay Area. HIV-status was verified by a letter of diagnosis or by a labeled pill bottle of their HIV medicine.
A total of 51 individuals were screened. Of these, 23 were ineligible for one of the following reasons: did not identify as black/African American (n = 2), neither partner was HIV-positive (n = 2), single relationship status (n = 2), no-show (n = 2), the relationship ended at the time of screening or interview (n = 4), or primary partner declined to participate (n = 9). One couple (n = 2) was excluded from analyses due to one partner identifying as a trans woman at the interview. A total of 28 men (14 couples) were included in the final analyses.
Individual interviews
Eligible participants were scheduled for an in-person interview with their primary partner. Participants were assigned a unique identification number. Partners were interviewed simultaneously but separately to allow each partner privacy to tell “his side” of the story.38 The study site was centrally located and accessible via public transportation. Informed consent was obtained from the participants before each interview, which lasted approximately 1.5–2 h. Interviews were audiotaped and transcribed for analyses. All study procedures were approved by the University of California San Francisco's Institutional Review Board.
Qualitative analysis
For dyadic analysis, the couple was the unit of analysis. To differentiate the partners from each other, one partner was assigned to be the index. The index referred to the participant living with HIV; among seroconcordant-positive couples, the index was randomly assigned. Among the three serodiscordant couples in the sample, all three HIV-negative partners reported currently being on preexposure prophylaxis (PrEP). Thus, interview topics focused on partner support in care engagement pertained to all couples. Interview topics included how the index engaged in HIV care (e.g., “How often do you see your medical provider for your HIV?”), and how his partner may be involved in his care (e.g., “How does [your significant other] support or not support you in your HIV care and treatment?”).
The first, second, and third authors formed a team-based approach to analyze the narrative data.39 Individual-level analysis was conducted to capture the full range of challenges to care engagement and forms of partner support, while dyadic analysis focused on exploring couple's dynamics based on both partners' narratives. Data were first analyzed at the couple-level using an approach similar to Eisikovits and Koren.37 A codebook was developed by iteratively generating and revising codes based on discussions of major themes that emerged from reading all transcripts. After several sessions of simultaneously applying codes as a team and discussing the coding system, consistency in code application was verified using transcripts from one couple. Thereafter, coders independently coded the remaining 13 transcripts using Dedoose version 7.6.21.40
To analyze the narratives at the couple-level, we compared and contrasted each transcript with that of the partner to discover overlaps between narratives and to identify points of corroboration and contradiction. With the couple as the unit of analysis, important statements were cross-analyzed and themes formulated based on both partners' perspectives on the role that their relationship played in their respective care engagement.37
Discrepancies in partners' accounts were incorporated into the analysis (rather than disregarded) to indicate discord and to signal where closer examination was warranted.37 For example, both partner A and B claimed to be the more supportive partner in the relationship (e.g., “I do more to support him than he does to support me.”). Further exploration of respective narratives found that each man was able to recall instances when his partner was supportive in their HIV care, as his partner had claimed separately. However, because both partners did not attribute those instances to be supportive, the intracouple discrepancy in their narratives was taken to indicate general relationship dissatisfaction in both partners.37,41
Individual-level analysis was conducted by reading a set of six transcripts from three couples, highlighting sections of texts to derive themes based on narratives that described partner support offered or received in the context of HIV care. Specific actions of HIV care and treatment-related support described in the text were marked and developed into index codes. Marker codes were developed to note the presence of specific actions that represented partner support within the dyad. Each marker code was listed under the index code in the codebook and given a definition and an example.
After reviewing the coded transcripts and comparing code application between coders, we applied the codes to the transcripts of one couple to verify code definitions and consistency in code application. The codebook was revised and the process of reviewing the coded transcripts and comparing code application between coders was repeated until reaching 85% agreement.42 Thereafter, we independently coded and created analytic memos based on emergent findings.
Results
A total of 11 seroconcordant-positive and three serodiscordant couples (14 couples; n = 28) participated in the study. The mean age of participants was 48.8 years; intracouple age difference ranged from 0 to 36 years (mean = 10.7 years). The majority of couples comprised partners who both self-identified as black/African American (10 couples); the remaining couples were of interracial. The annual individual income of the sample ranged from <$10K to $55K, with half of the sample (n = 14) reporting an annual personal income of less than $20K. Relationship length ranged from 3 months to over 20 years (mean = 6.6 years). Of the 14 couples, 8 reported cohabitation at the time of the study.
Emergent themes from individual-level analyses focused on facilitators to and challenges in care engagement. Dyadic analysis revealed themes around couple-level characteristics that shaped how partners perceived their significant other's care needs and offered support in response. Individual-level findings are presented first, followed by findings from the dyadic analysis.
Multilevel facilitators and barriers to HIV care
Participants referred to challenges to care engagement at the individual, interpersonal, and social structural levels, while facilitators of care engagement were identified at the interpersonal level.
Individual
Individual-level challenges to engagement in care and medication adherence included medication fatigue and side effects, forgetfulness, and changes to medication regimen. Medication fatigue was common, especially among those who took multiple medications (“I hate taking so many. I'm already taking other different medications, but now the HIV pills, they're just more pills.”). Some men growing tired of taking medications after taking them for a long time and would miss doses on purpose to take a break:
“I purposely missed one this week. Sometimes I just have to ‘air myself out.’ I've spoken to my doctor about this. It's just an instinctual thing. I mean, it's not recommended. But sometimes you just have that feeling. You just need to give your liver a break. And once in a while, once in a while.”
Some men mentioned feeling good and thus questioning whether they needed to keep taking medications. Others discussed experiencing side effects such as diarrhea, mood swings, and “crazy dreams.” For one man, these side effects were coupled with a perception that the medications are unnecessary as long as “I'm feeling healthy”:
“I don't really want to take it. I don't really see the point. My T - cells and my viral load are good. I'm feeling healthy. And I actually feel worse taking medicine, in the past. It must have been for about five or six - no - six, seven months. And I was still, like, having symptoms… Right now, I'm just figuring out where I'm going to be in my career and all that - before I can take the medicine.”
Many men mentioned “forgetting” as an ongoing challenge in taking medications or attending appointments. Other personal challenges included mental illness (e.g., depression) and drug use. Approximately one-third of participants discussed having experienced symptoms of depression. These ranged from brief depression after HIV diagnosis to long-term, more serious depression that directly impacted their motivation to live (“[I] didn't want to live, so I didn't care if I take the meds or not.”). Drug use was mentioned as a personal challenge to HIV care:
“Crack, you name it, I was doing it. And I one time got shingles because my immune system was all messed up. I wasn't taking my medication right. And then the stuff doesn't work because you're not using it right.”
Interpersonal
Interpersonal factors such as couple serostatus played a role in how men engaged in care. Men in concordant-positive relationships described that having an HIV-positive partner was helpful to their own care engagement. Some men were comforted by knowing that their partner understood and related to the challenges of living with HIV. Others explained that being with someone who was also HIV-positive destigmatized their HIV-positive status, which increased their capacity for self-care. One man appreciated being in a relationship, in which he did not have to be self-conscious of his status:
“I was too uncomfortable with who I was and probably still am too uncomfortable with somebody who is not positive. I wouldn't even take the chance of being with somebody [who is HIV-negative]…I was very careful and very self-conscious. But with [my partner] it's different…he's just great.”
For HIV-negative partners who were on PrEP, care engagement often was a joint effort. For HIV-positive partners, support revolved around the motivation to help his HIV-negative partner to stay healthy. Reasons for adhering to HIV treatment included not wanting to infect one's partner and feeling responsible for a partner's health:
“Because I don't want to infect nobody, especially him. You know, I wouldn't want that on him, even though he's doing his PrEP, you know, being smart and stuff like that. But I want to make sure he's fine. So, for him to be fine, I have to be okay, have to be good… He keeps me on track, you know, about the medicine and stuff, so, yeah.”
While some interpersonal factors facilitated care engagement, others presented challenges. Some men described negative relationship dynamics such as jealousy and intimate partner violence, but did not specifically refer to them as interfering with their care engagement. In fact, among couples with relationship discord and mutual blame, men nevertheless acknowledged receiving certain tangible benefits in care engagement from their partner. In one example, both men expressed dissatisfaction in their relationship, but each was able to recount instances of support from the partner such as scheduling each other's follow-up appointments and accompanying each other to and from appointments.
Some participants also described that being caregivers to partners, family, or friends detracted from their ability to optimally engage in care. One participant explained that taking care of his ailing grandmother led him to forget to take his own medication at times. Others lamented that caring for their HIV-positive partner can be burdensome when their partner was unappreciative (“[I wish he would say] a simple thank-you to show that he appreciates [what I do for him].”). Partners may also have negative impacts on each other's behavior. For example,
“A couple of months ago because I noticed if I don't take care of myself and then it affects people around me like my partner because then part of me - part of him is like, ‘Well, if he's missing the pills, I could.” So, I notice that we sort of feed off on each other like even our behaviors or patterns are like, “Well, he's drinking whatever. Why can't I?’”
Social structural
Many of the significant challenges to care were social-structural in nature and often interrelated. These included experiences with HIV stigma, incarceration, homophobia, housing, food insecurity, and substance use. One man explained how difficult it was for his partner to stay on track of his care and treatment while living in single-room occupancy (SRO housing):
“There's just a lot of drug people hang out right close to you 24/7. [HIV] is a hard thing to deal with just normally, but if [drug use] is always in your face. I mean, when it comes to SROs, it's crazy. You go up in there, doors are all open, and people doing their shit, and knock on your door at 5:00 in the morning - and you go outside, everything's going on, literally everything. Then the dealer came by, got some stuff. It's a hard thing to be focused and doing your thing.”
Almost all of the HIV-positive men discussed care engagement in the context of coming to terms with their HIV status as a black man, a process that had a profound effect on their self-concept and acceptance. Some discussed the intersecting impacts of HIV stigma, homophobia, and racism that led them to go through periods of denial about their HIV status, during which time they were not engaged in HIV care or on ART. Although several of the men in the study had disclosed their HIV status to close others, discussions around HIV remained taboo. For example,
“Yeah, well, I just shared [my status] with my mom. I told my auntie first, and I told my sister, but it's just something in my family that's not discussed. I cannot have HIV conversation with my sister. I would not dare to. I'm from that family. So, I still feel that it's taboo. We don't discuss this.”
Poverty was described as linked to food insecurity, suboptimal or unstable housing, and challenges to HIV care, such as suboptimal living conditions in SRO housing. Although we did not specifically ask about incarceration history, several men referred to spending time in jail and/or having vicarious (e.g., a relative) encounters with the legal system. In addition, several men also described not adhering to medications due to food insecurity. One such participant was reluctant to take medicines on an empty stomach because there was no food in the house; another missed doses due to believing that he had to take them with meals. One man mentioned selling his HIV medication for food:
“I was selling my pills for grocery. Get pills that come in every month, look at your refrigerator. So, once [my HIV medicine] was a lifesaver, and then it got to be, okay, I can keep food in my house by selling it to other HIV positive people who weren't in the healthcare system.”
Although all participants in the study had either private or safety-net health insurance, healthcare access was not without hitches. Affordability posed issues to healthcare access. When explaining why he was not engaged in care, one man explained,
“I need to do some blood work before I go to see my doctor. I know that already. But I owed money so I couldn't do it. I have to figure that out, somehow, with ADAP [AIDS Drug Assistance Program] or something, some way to get that done.”
Some men faced healthcare-related challenges with scheduling appointments, communicating with providers, and organizational issues at clinics (“It's just the communication breakdown: I'll call the front office, and it'll be like, well, [the doctor] is not in today, can they call you back? I'll wait for a call, and they won't call me at all that whole month.”). The task of managing healthcare was perceived as difficult due to inefficiency and long wait times at the clinic. For example,
“It was just like sort of like everybody was running around with their heads cut off…You could never go draw blood because something was wrong with the machines. The new receptionist, she didn't know what she was doing. You get to your appointment, and then you go into that little room to wait for the doctor, 40 minutes to an hour.”
Dyadic processes in HIV care
Several important couple-level processes emerged. Dynamics of couple's resilience, joint problem-solving, and interdependence bolstered the couple's capacity for dyadic HIV care.
Couple's resilience
Some men described couples' resilience as working together to overcome oppression and adversity, a sense of “we-ness” that shaped their approach to problem-solve barriers in care engagement. In the same way, the personal experiences in overcoming adversity can lead to a sense of unity, shared experiences with overcoming adversity related to racism, police brutality, incarceration, substance use, and stigma of being HIV-positive and gay or MSM, served as a powerful bond. This couple-level resilience in turn strengthened the couples' relationship and their ability to address challenges in HIV care as a unit. Specifically:
“If a Black man hooks up with another Black man, they appreciate each other. They got a whole lot of odds that they go through. Racism and homophobia are both seriously strong things to go against. A White gay man, he doesn't have to deal with racism. Racism is so strong…so if I can find a brother who's willing to walk with me through all this madness—a bond is created. That bond is impenetrable. I think what helps a Black couple make it is that a Black male relationship doesn't fit the mold of a lot of things. Like two brothers that hang together for however many years? They done been through dope, death, and a lot of stuff—and then homophobia on top of that? So when you find a brother that's strong enough to come through all of that, you hang on to it.”
Positive relationship dynamics among resilient couples often helped men in overcoming individual or social and structural barriers to care engagement. Another expressed pride in being in a relationship that has stood the test of time despite tremendous strains, giving his relationship meaning within his community, while driving how he and his partner supported each other. For example:
“My friends look up to our relationship and say, ‘I want to be just like you guys.’ We're like a model couple for so many people in our community, because we have been through so much, me and my partner, and we're still together. A lot of younger and even some older people look up to us for still hanging in there because our bond is so strong. [We've been through] domestic violence. We've been through drugs together, breaking up off and on, and just a lot of different stuff that we've been through together.”
Joint problem solving
Many participants described HIV care as a collaborative process, in which partners coordinated with each other to problem-solve the myriad of challenges in HIV care. Partners often traded tips and exchanged knowledge around HIV care. One man explained that seeing how his partner engaged in care and treatment helped him know what to expect in terms of his own HIV care (“He's had HIV longer, so I kind of look to him to know what to expect.”). As some noted, challenges relating to affordability, scheduling appointments, and accessing public benefits can be significant barriers. Some men had skills and knowledge that they used to help their partners get beyond these obstacles. Some played an active part in helping navigate healthcare access and social services (“I know which forms to fill out to qualify for [healthcare] services and I'll tell him to go down to [location].”). Couples problem-solved issues in care engagement together, such as listening and then giving recommendations (“He tells me about [the suboptimal care he received], and I tell him to switch doctors.”).
Partners helped each other coordinate activities and behavior around care and treatment engagement as a part of normal daily routine. Dyadic coordination was evident in giving reminders about scheduled appointments, coattending medical appointments, and communicating with each other's healthcare providers. For example, some couples used a joint calendar to keep track of medical appointments. Consequently, the task of managing HIV care became a collaborative task, in which each partner was aware of the other's appointments:
“I take him to my doctor's appointments, and I go to his doctor's appointments…what I usually do is I find out when my next appointment is and then I just write it down on the calendar. I have two calendars, one in the bathroom and one by the door, and so I just write it down on the calendars. I even write down his appointments all on the calendars to remind us so that every day we know what we have - like, the night before, we look at the calendar at least once or twice a day to see what we have to do the next day.”
Coordinating schedules required joint effort and some men did so only when their schedule allowed or when it was necessary. Nevertheless, some were able to coordinate their schedules so that they attended each other's appointments. One described how he and his partner coordinated their schedules to accompany each other:
“[We coordinated] our routine within our schedules… My last appointment was last month at [name of clinic] and his is coming up next month for his checkup but I know his previous one was probably about three months prior. I went to that doctor's appointment with him.”
While some men accompanied each other, others even entered the examination room with their partner or communicated directly with the healthcare provider. Attending the primary partner's medical appointments often also meant meeting and communicating with the partner's healthcare provider. This was particularly instrumental in cases where a partner was struggling with depression or substance use:
“…[W]hen he wasn't taking his meds and stuff, the doctor asked me, ‘Why wasn't he taking it? And what can we do to get him back to taking his medicine’ and stuff. I told him the truth. I said, ‘He don't…like taking the medicine because he don't really care to live anymore…’”
Interdependence
All men described some degree of mutual dependence within their relationship with their partner that factored in their care engagement. An interdependent dynamic of accountability was often manifested in everyday interactions between partners, as one man described:
“We both usually know when each other [has] got an appointment. So, just in general conversation we usually throw it out to the other. So, when he says that, ‘oh, I got a dental appointment,’ I'll try to keep him conscious of it, even though he probably remembers. So, we know enough about each other to be conscious of an appointment coming up.”
It was common among couple members to be mutually familiar with each other's preferences for receiving social support, noting respective similarities and differences between themselves and their partner. Partners were adept at balancing between competing needs and preferences in offering their support that required intimate and off-hand knowledge of their partner's goings-on. Men recalled their partner's last medical appointment, the name of his healthcare provider or clinic, and the number of medications he takes and when. Having an intimate knowledge about their partner allowed men to engage in nuanced support strategies that changed dynamically depending on the situation. Although familiarity with each other's habits was more commonly expressed among couples that have been together for some time (e.g., 5+ years), it was not uncommon among shorter relationships (e.g., <1 year).
Many described a mutual sense of responsibility for their partner's health. Partners typically mirrored each other's caregiving values and sense of responsibility or obligation. A few men reported feeling “100% responsible” for their partner's health outcomes, while others emphasized personal responsibility, but all felt some responsibility toward their partner's overall health. Some expressed that they offered support to demonstrate their love for the partner; this often prompted their partner to reciprocate by “trying to be healthy for him.” Some men demonstrated good habits in healthcare as a way of motivating their partner and to illustrate that “life is worth living.” Other men suggested that helping their partner with care engagement further strengthened their beliefs in and resolve to be healthy.
For some couples, medication adherence appears to be a result of mutual influence on each other. Several men described being reminded to take their medicine when they see their primary partner take theirs (e.g., “Usually he kind of reminds me now because…when he gets up and takes his in the morning, I see him taking his. It's kind of a ‘ding, I better take mine.’”). Many described medication adherence as a joint effort (e.g., “I make sure he take his medicine. He make sure I take mine”). Others supported each other by incorporating their partner's medication regimen into their own.
Discussion
HIV care is a complex and dynamic process, and black MSM may draw from various resources, including from their primary relationship, to address a multitude of individual, interpersonal, and social structural or institutional challenges to care.12 Findings showed common challenges to and facilitators of care engagement among black MSM in primary relationships and elucidated couple-level dynamics that appear to support care engagement. Individual-level analyses highlighted challenges to and facilitators of HIV care that were individual, interpersonal, and social structural/institutional in nature.
Individual-level barriers included medication fatigue and side effects, forgetfulness, changes to medication regimen, and mental illness, consistent with the existing literature.15,20 Interpersonal factors included those that presented challenges, such as caregiving burden and negative relationship dynamics, as well as those that facilitated care engagement, such as couple serostatus.36 Specifically, our findings found that having a primary partner who was also HIV-positive may remove some of its stigma, while being in a relationship with an HIV-negative partner may be a motivation to maintain an undetectable viral load and lower transmission risk. Other challenges in care engagement were social structural or institutional in nature, ranging from food insecurity, discrimination, and navigation of healthcare systems.
In response to challenges in HIV care, primary partners often provided tactical, instrumental support that included reminding about medication regimens and accompanying to and from medical appointments.43 Couple-level analyses identified key dynamics of the couple that underlined these supportive strategies in dyadic care engagement. Such dynamics included couple's resilience, a characteristic of the couple based on having overcome adversity together and evidenced by a mutual understanding around shared experiences as black and MSM. To our knowledge, this is the first study to examine couple's resilience in the context of black MSM in couples. Past research has examined couple's resilience using a stress and coping framework to understand how couples adapt to and cope with HIV,34 but has been limited in application to black MSM.
Couple's resilience was evident in how couples approached challenges in care engagement. One such approach was joint problem-solving, evident in how couples drew upon and relied on each other to engage in care and treatment. Joint problem-solving entailed coordinating schedules, attending each other's healthcare appointments, reminding each other to take medications on time, and trading tips and discussing solutions for navigating the healthcare system.
Couples also referred to a sense of obligation to and from their partner, and this dimension of interdependence was key in driving mutual support. Support strategies also appeared to be driven by familiarity with the partner's needs, preferences, and daily goings-on. Findings showed that some men viewed adherence as an individual responsibility, while others viewed it as something that is a collective responsibility that should be integrated into the relationship.27,43
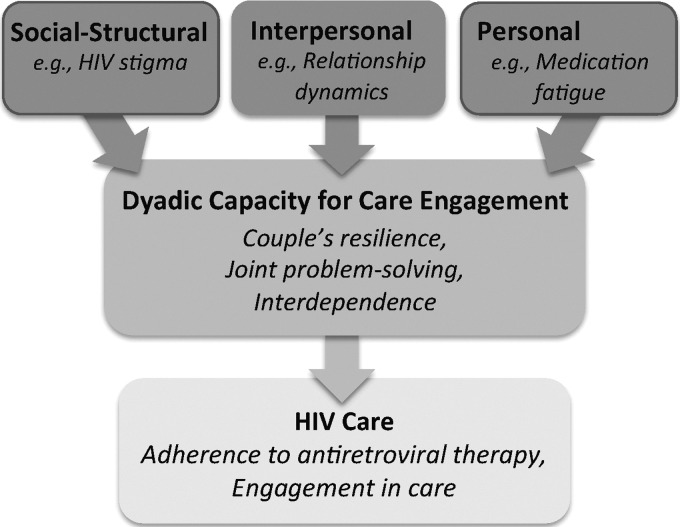
These findings expand on Karney and colleagues' model of dyadic HIV prevention. Our model delineates individual, interpersonal, and social structural factors in HIV care and identifies dyadic processes that bolster the couple's capacity to address multilevel challenges and to coordinate dyadic HIV care (Fig. 1).44 Specifically, dyadic processes of couple's resilience, joint problem-solving, and interdependence bolster the couple's capacity to address multilevel challenges to HIV care.21
FIG. 1.
Framework of dyadic HIV care.
The present sample of couples was predominantly of the same race (i.e., black), consistent with previous research.45 Our findings with these black MSM couples showed that couple's resilience entailed a shared experience having coped with past adversity, which strengthens the couple's relationship to further adapt to current or future challenges. These challenges may stem from having overcome past adversity related to incarceration, substance use, racism, living with HIV, and being gay or MSM. Black men in this study referenced significant challenges to care, including housing instability, food insecurity, substance use, and interrupted access to the healthcare system.20,46,47
The effects of such challenges required numerous types of resources and concerted efforts from the couple. Some men referred to feeling empowered from being in a relationship that had been resilient in the face of past challenges and adversity.34 These experiences serve as a powerful bond unifying the couple and invoking a sense of “we-ness,” in turn strengthening the couple's relationship and their capacity to adapt to and coordinate HIV effectively as a unit using joint problem-solving approaches.48,49 Joint problem-solving is commonly conceptualized as an “active” task-oriented approach in the stress and coping literature.50 Joint problem-solving required that each partner have the skills to collaboratively derive plans and implement strategies for engaging in care and treatment.51
Interdependence is a broad concept that encapsulates reciprocal dynamics of mutual accountability, influence, and familiarity around healthcare beliefs, preferences, and behaviors.52,53 Thus, in the context of multilevel challenges to retention in care and adherence to treatment, these dyadic processes may increase the couples' capacity to successfully coordinate HIV care. Interventions with black MSM in primary relationships could be developed to promote dyadic coordination in the relationship of HIV care by leveraging these dyadic processes.21
The primary relationship can be a “double-edged sword.” Being in a relationship with an uncaring partner violates transactional expectations of mutual caring, leading to perceived asymmetry in caregiving and resentment in the relationship.54 While the primary relationship served many positive supportive functions in care engagement, our findings also show evidence of potential negative effects of mutual influence on care engagement. We found evidence that being a caregiver can impede some men's own adherence to treatment. Substance use on the part of one's partner may also negatively impact one's care engagement. There was some evidence for negative partner influence (e.g., one's poor adherence affecting the other's adherence), but this seemed more about the perceptions or the potential to affect a partner rather than having actual negative impacts on engagement.
The emphasis on positive impact of partners suggests the need to capitalize on positive aspects of these relationships in an intervention, such as bolstering couple's resilience and strengthening joint problem-solving skills. Future research may address both positive and negative effects of the primary relationship. Interventions may do so by using approaches and strategies that are culturally appropriate for engaging and retaining minority couples, including technology-based approaches55 to HIV care that synchronize dyadic coordination of engagement and adherence between partners.21 HIV providers and clinics may wish to invite the patient's primary partner to be involved in his HIV care. Doing so acknowledges the primary partner's role in the health of the patient and creates an inclusive environment.56
Limitations
As with most qualitative research that uses small sample sizes, we acknowledge the limits to the generalizability of the study findings to other populations (e.g., black MSM couples living in a different geographical region). We focused in the interviews on how relationship dynamics might support HIV care, which may have inadvertently emphasized positive rather than negative relationship dynamics. Similarly, we did not focus the study on relationship conflict and violence, which has been shown to negatively influence HIV care.57 Our findings represent challenges that were perceived by the participants, and we were not able to observe their actual behavior. Experienced challenges to care engagement may not be captured given social desirability bias, as some studies suggest.58 Future research should explore using mixed methods data collection to triangulate potential barriers and support strategies.
Conclusions
This study included participants who are in most need for adherence support and could represent the 10% that get left behind in UNAIDS 90-90-90 goals.59 There are important opportunities to leverage existing forms of relationship dynamics to improve engagement in HIV care and treatment among black MSM. By using individual- and couple-level analyses, the present study identified multilevel barriers to care and the couple-level processes involved in overcoming these challenges. Findings support a conceptual framework of dyadic HIV care that may guide future research with couples. Harnessing the strength of couples (e.g., couple's resilience) while addressing potential negative influences of the partner for HIV care is likely to be a fruitful direction. Dyadic interventions may capitalize on the benefits of primary relationships, such as strengthening joint problem-solving and couple's resilience, in facilitating black MSM in couples to help each other engage in care and treatment.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Sullivan PS, Peterson J, Rosenberg ES, et al. . Understanding racial HIV/STI disparities in black and white men who have sex with men: A multilevel approach. PLoS One 2014;9:e90514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenberg ES, Millett GA, Sullivan PS, del Rio C, Curran JW. Understanding the HIV disparities between black and white men who have sex with men in the USA using the HIV care continuum: A modelling study. Lancet HIV 2014;1:e112–e118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matthews DD, Herrick A, Coulter RW, et al. . Running backwards: Consequences of current HIV incidence rates for the next generation of black MSM in the United States. AIDS Behav 2016;20:7–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Millett GA, Peterson JL, Flores SA, et al. . Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet 2012;380:341–348 [DOI] [PubMed] [Google Scholar]
- 5.Sullivan PS, Rosenberg ES, Sanchez TH, et al. . Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: A prospective observational cohort study. Ann Epidemiol 2015;25:445–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oster AM, Wiegand RE, Sionean C, et al. . Understanding disparities in HIV infection between black and white MSM in the United States. AIDS 2011;25:1103–1112 [DOI] [PubMed] [Google Scholar]
- 7.Hall HI, Holtgrave DR, Tang T, Rhodes P. HIV transmission in the United States: Considerations of viral load, risk behavior, and health disparities. AIDS Behav 2013;17:1632–1636 [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Understanding the HIV care continuum. Available at: www.cdc.gov/hiv/pdf/library/factsheets/cdc-hiv-care-continuum.pdf Published June 2018. Updated 2018 (Last accessed July3, 2018)
- 9.Millett GA, Crowley JS, Koh H, et al. . A way forward: The national HIV/AIDS strategy and reducing HIV incidence in the United States. J Acquir Immune Defic Syndr 2010;55 Suppl 2:S144–S147 [DOI] [PubMed] [Google Scholar]
- 10.Rebeiro PF, Abraham AG, Horberg MA, et al. . Sex, race, and HIV risk disparities in discontinuity of HIV care after antiretroviral therapy initiation in the United States and Canada. AIDS Patient Care STDS 2017;31:129–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hightow-Weidman L, LeGrand S, Choi SK, Egger J, Hurt CB, Muessig KE. Exploring the HIV continuum of care among young black MSM. PLoS One 2017;12:e0179688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Christopoulos KA, Massey AD, Lopez AM, et al. . “Taking a half day at a time”: Patient perspectives and the HIV engagement in care continuum. AIDS Patient Care STDS 2013;27:223–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tobias CR, Cunningham W, Cabral HD, et al. . Living with HIV but without medical care: Barriers to engagement. AIDS Patient Care STDS 2007;21:426–434 [DOI] [PubMed] [Google Scholar]
- 14.Marx KA, Malka ES, Ravishankar J, Schwartz RM. Measurement of retention in care among adults infected with HIV in an urban clinic. AIDS Care 2011;23:1298–1304 [DOI] [PubMed] [Google Scholar]
- 15.Ulett KB, Willig JH, Lin H, et al. . The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS 2009;23:41–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weiss JJ, Stirratt MJ. Psychiatric aspects of care engagement and medication adherence in antiretroviral-based HIV treatment and prevention. In: Comprehensive Textbook of AIDS Psychiatry: A Paradigm for Integrated Care. Cohen MA, Gorman JM, Letendre SL, Jacobson JM, and Volberding P, eds. Oxford, UK: Oxford University Press, 2017:334 [Google Scholar]
- 17.Hatcher AM, Smout EM, Turan JM, Christofides N, Stockl H. Intimate partner violence and engagement in HIV care and treatment among women: A systematic review and meta-analysis. AIDS 2015;29:2183–2194 [DOI] [PubMed] [Google Scholar]
- 18.Conroy A, Leddy A, Johnson M, Ngubane T, van Rooyen H, Darbes L. ‘I told her this is your life’: Relationship dynamics, partner support and adherence to antiretroviral therapy among South African couples. Cult Health Sex 2017;19:1239–1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holtzman CW, Shea JA, Glanz K, et al. . Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen's behavioral model. AIDS Care 2015;27:817–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Remien RH, Bauman LJ, Mantell JE, et al. . Barriers and facilitators to engagement of vulnerable populations in HIV primary care in New York City. J Acquir Immune Defic Syndr 2015;69 Suppl 1:S16–S24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tan JY, Campbell CK, Tabrisky AP, Siedle-Khan R, Conroy AA. A conceptual model of dyadic coordination in HIV care engagement among couples of black men who have sex with men: A qualitative dyadic analysis. AIDS Behav 2018;22:2584–2592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldenberg T, Stephenson R. “The more support you have the better”: Partner support and dyadic HIV care across the continuum for gay and bisexual men. J Acquir Immune Defic Syndr 2015;69 Suppl 1:S73–S79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan JY, Conroy AA, Lee IC, Pratto F. Leveraging power in intimate partner relationships: A power bases perspective. In: Agnew CR, Harman JJ, eds. Power in Close Relationships. Cambridge, UK: Cambridge University Press, 2017 [Google Scholar]
- 24.Koblin BA, Mayer KH, Eshleman SH, et al. . Correlates of HIV acquisition in a cohort of black men who have sex with men in the United States: HIV prevention trials network (HPTN) 061. PLoS One 2013;8:e70413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mitchell JW. The use of technology to advance HIV prevention for couples. Curr HIV/AIDS Rep 2015;12:516–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell JW. HIV-negative and HIV-discordant gay male couples' use of HIV risk-reduction strategies: Differences by partner type and couples' HIV-status. AIDS Behav 2013;17:1557–1569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldenberg T, Clarke D, Stephenson R. “Working together to reach a goal”: MSM's perceptions of dyadic HIV care for same-sex male couples. J Acquir Immune Defic Syndr 2013;64 Suppl 1:S52–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wrubel J, Stumbo S, Johnson MO. Antiretroviral medication support practices among partners of men who have sex with men: A qualitative study. AIDS Patient Care STDS 2008;22:851–858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stumbo S, Wrubel J, Johnson MO. A qualitative study of HIV treatment adherence support from friends and family among same sex male couples. Psychol Educ 2011;2:318–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Houston E, Osborn A, Lyons T, Masvawure T, Raja S. Exploring perceived social support from peer facilitators in an HIV treatment adherence intervention for African American patients: A content analysis of participant perspectives. J Community Appl Soc Psychol 2015;25:487–501 [Google Scholar]
- 31.Pakenham KI, Dadds MR, Terry DJ. Relationship between adjustment to HIV and both social support and coping. J Consult Clin Psychol 1994;62:1194. [DOI] [PubMed] [Google Scholar]
- 32.Conroy AA, McKenna SA, Leddy A, et al. . “If she is drunk, I don't want her to take it”: Partner beliefs and influence on use of alcohol and antiretroviral therapy in South African couples. AIDS Behav 2017;21:1885–1891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montgomery CM, Watts C, Pool R. HIV and dyadic intervention: An interdependence and communal coping analysis. PLoS One 2012;7:e40661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gamarel KE, Revenson TA. Dyadic adaptation to chronic illness: The importance of considering context in understanding couples' resilience. In: Couple Resilience. Skerrett K, Fergus K, eds. Dordrecht: Springer Netherlands, 2015:83–105 [Google Scholar]
- 35.VanderDrift LE, Ioerger M, Mitzel LD, Vanable PA. Partner support, willingness to sacrifice, and HIV medication self-efficacy. AIDS Behav 2017;21:2519–2525 [DOI] [PubMed] [Google Scholar]
- 36.Tan JY, Pollack L, Rebchook G, et al. . The role of the primary romantic relationship in HIV care engagement outcomes among young HIV-positive black men who have sex with men. AIDS Behav 2018;22:774–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eisikovits Z, Koren C. Approaches to and outcomes of dyadic interview analysis. Qual Health Res 2010;20:1642–1655 [DOI] [PubMed] [Google Scholar]
- 38.Morris SM. Joint and individual interviewing in the context of cancer. Qual Health Res 2001;11:553–567 [DOI] [PubMed] [Google Scholar]
- 39.MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Cult Anthropol Methods 1998;10:31–36 [Google Scholar]
- 40.Lieber E, Weisner T, Taylor J. Dedoose Software. California: Sociocultural Research Consultants, 2011. [Google Scholar]
- 41.Koren C, Eisikovits Z. Life beyond the planned script: Accounts and secrecy of older persons living in second couplehood in old age in a society in transition. J Soc Personal Relat 2011;28:44–63 [Google Scholar]
- 42.Lombard M, Snyder-Duch J, Bracken CC. Content analysis in mass communication: Assessment and reporting of intercoder reliability. Hum Comm Res 2002;28:587–604 [Google Scholar]
- 43.Wrubel J, Stumbo S, Johnson MO. Male same-sex couple dynamics and received social support for HIV medication adherence. J Soc Personal Relat 2010;27:553–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karney BR, Hops H, Redding CA, Reis HT, Rothman AJ, Simpson JA. A framework for incorporating dyads in models of HIV-prevention. AIDS Behav 2010;14:189–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tieu H, Nandi V, Hoover DR, et al. . Do sexual networks of men who have sex with men in New York city differ by race/ethnicity? AIDS Patient Care STDS 2016;30:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weiser SD, Bangsberg DR, Kegeles S, Ragland K, Kushel MB, Frongillo EA. Food insecurity among homeless and marginally housed individuals living with HIV/AIDS in San Francisco. AIDS Behav 2009;13:841–848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weiser SD, Young SL, Cohen CR, et al. . Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr 2011;94:1729S–1739S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gamarel KE, Neilands TB, Golub SA, Johnson MO. An omitted level: An examination of relational orientations and viral suppression among HIV serodiscordant male couples. J Acquir Immune Defic Syndr 2014;66:193–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Revenson TA, Kayser KE, Bodenmann GE. Couples Coping with Stress: Emerging Perspectives on Dyadic Coping. American Psychological Association, Washington, DC, 2005 [Google Scholar]
- 50.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Pub Co, 1984. [Google Scholar]
- 51.Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull 2007;133:920. [DOI] [PubMed] [Google Scholar]
- 52.Thibaut J, Kelley H. The Social Psychology of Groups. New York: Wiley, 1959. [Google Scholar]
- 53.Kelley H, Thibaut J. Interpersonal Relations: A Theory of Interdependence. New York: Wiley-Interscience, 1978. [Google Scholar]
- 54.Kelley HH, Holmes JG, Kerr NL, Reis HT, Rusbult CE, Van Lange PAM. An Atlas of Interpersonal Situations. Cambridge, UK: Cambridge University Press, 2003 [Google Scholar]
- 55.Freese TE, Padwa H, Oeser BT, Rutkowski BA, Schulte MT. Real-world strategies to engage and retain racial–ethnic minority young men who have sex with men in HIV prevention services. AIDS Patient Care STDS 2017;31:275–281 [DOI] [PubMed] [Google Scholar]
- 56.Tan JY, Baig AA, Chin MH. High stakes for the health of sexual and gender minority patients of color. J Gen Intern Med 2017;32:1390–1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schafer KR, Brant J, Gupta S, et al. . Intimate partner violence: A predictor of worse HIV outcomes and engagement in care. AIDS Patient Care STDS 2012;26:356–365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sauceda JA, Neilands TB, Johnson MO, Saberi P. An update on the barriers to adherence and a definition of self-report non-adherence given advancements in antiretroviral therapy (ART). AIDS Behav 2018;22:939–949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Joint United Nations Programme on HIV/AIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic UNAIDS, 2014. 2014. Available at: www.unaids.org/en/resources/documents/2017/90-90-90 (Last accessed August21, 2018)