Abstract
Introduction: Complementary and alternative medicine (CAM) use has been increasing in the past decades in tandem with changes regarding the notions of health and illness. Comparing conventional medicine (CM) and CAM in how they address health problems has been a point of focus for both the health sciences and individuals dealing with health problems. Various social, cultural, political, economic, and personal factors play a role in whether different health approaches are integrated or not when addressing illness experiences. Methods: The qualitative study comprised semistructured interviews (N = 9) and participant observation involving 105 patients conducted between January 2015 and May 2017 at 4 clinics of Traditional Chinese Medicine in Budapest, Hungary. Code structures were created inductively with Interpretative Phenomenological Analysis. Results: The mutually exclusive view of CM/CAM use occurred due to loss of trust in the doctor-patient relationship causing problems in communication, and also as a result of the patient espousing certain cultural dispositions. Significant dispositions included a preference for the “natural” and psychologization, the latter often manifested in psychosocial etiology, vitalism, and illness symbolism. Discussion: A polarized choice of therapy may occur as a result of a competitive health care market in which medical modalities and their underlying cultural systems compete within a global milieu of information proliferation and a hybridization of individual worldviews. Through a process of “cultural creolization”, changing concepts of health and illness create varying patient expectations and meanings regarding illness, which in turn affect therapy choice as well. Conclusion: Mirrored in the articulation of an individual’s illness trajectory is a tension that is also reflected in the struggles in the health care system to more adequately understand health/illness processes from a pluralistic perspective. The power relations in the health arena (among CAM/CM practitioners and systems) play a role in legitimizing or undermining different health practices, which as consequence affects the possibility of integrating them into the processes of care. Thus, therapy choice is not only linked to changing notions of health and illness, but also to shifting conceptualizations of self, identity, and the practitioner-patient relationship.
Keywords: qualitative, complementary and alternative medicine use, integration, cultural dispositions, push and pull factors, Traditional Chinese Medicine
Introduction
Complementary and alternative medicine (CAM) is composed of a group of health systems, products, and services not considered to constitute a part of conventional medicine (CM). The diverse medical modalities may be employed simultaneously with (complementary) or instead of (alternative) biomedicine. Most quantitative surveys of CAM use indicate that it is on the rise and that the majority of individuals in Western cultures are using a CAM modality; results vary between 42% and 83% in the United States and may be up to 86% in Europe.1-6
A significant focal point of query is whether patients inform their physician about a complementary therapy or product they are employing. Various studies state that patients predominantly do not disclose this information to their CM practitioners7-9; Adler and Fosket,10 working with a sample of 86 breast cancer patients found that while 72% of them used a CAM modality, only 54% disclosed this to their physician; yet 94% discussed their CM treatment with their CAM practitioner. Illness-specific studies in Hungary and Europe suggest that 20% to 77% of cancer patients and 60% to 80% of emergency and surgical patients do not communicate about using complementary treatments with their physician.11,12 It is argued that this endangers the patient, as the various therapies may exhibit a negative interaction. Furthermore, from the perspective of institutions providing health care services, this affects the possibility of creating an integrative approach to health problems. Based on several studies, Faith et al9 report that “reasons for lack of disclosure include concerns about negative reactions or judgment from providers, perceptions that CAM use is not something about which providers need to know, and providers not initiating discussions about CAM.”
A multitude of studies suggest that CAM use is highest among female cancer patients4,13 and that a frequent employed modality is Traditional Chinese Medicine (TCM). Patients obtain information about TCM through self-help, synthesizing information from various sources, such as family, friends, fellow patients and support groups, which are all instrumental in the decision-making process.14 As with most CAM users, cancer patients employ these treatments for a variety of reasons, such as a need to avoid passivity in coping with feelings of helplessness and hopelessness, assuming control in their well-being and quality of life, and tackling the adverse effects of CM.4,14,15 Because of their prominent role among cancer patients, the use of these modalities requires a deeper understanding regarding their predictors and their mode of usage, that is, as an alternative or a complementary therapy.
Most studies do not measure substituting and augmenting CAM use separately, but those which do assert that patients in the West tend to use CAM as complementary, rather than alternative treatment the latter may only account for about 4.4% of CAM clients,16 or according to other studies this number may be more than 29%.17 A relevant point of inquiry concerning modes of CAM use (integration or mutual exclusion) is whether patients belonging to these 2 groups retain different reasons and motivations regarding their choice of therapy. Astin16 found that dissatisfaction with biomedicine (or a certain hospital/physician) was not a significant predictor of complementary use, while adherence to cultural dispositions, such as “holism” and “spirituality” was; conversely, in alternative CAM use, dissatisfaction with and distrust in CM physicians proved to be a significant factor. Thus, there is a possibility that motivations behind modes of CAM use differ greatly and warrant further analysis.
We can assume that an individual’s help-seeking behavior is congruent with his or her concepts regarding health and illness,18 hence the patient’s interpretations, worldview, and predisposing factors are of pivotal importance. The decision-making process concerning CAM use, which involves factors such as sources of information about said health practices, the perception of their benefits, the congruence in meanings regarding health and illness among practitioners and patients, all affect the likelihood of turning to CAM practices. Nonetheless, the role CM plays in decision making is also vital, particularly in the process of developing an integrative approach to health problems favoring the articulation of CAM and CM, or enforcing a nonintegrative approach to address health, which in some cases could exacerbate the patient’s physical, mental and emotional condition.
Methods
The research is a qualitative, anthropological initiative paying heed to ensure scientific rigor19-21 in the employed methodology and analysis. Central to qualitative standards is maintaining neutrality concerning the topic under scrutiny, as well as retaining a critical stance toward all types and sources of information, that is, contextual interpretation.22,23 Also pivotal in our methodology is ensuring continued reflexivity in all areas of inquiry, that is, with regard to researcher preconceptions (controlled with retaining cultural relativism and a holistic understanding of each cultural phenomenon24); the observer effect brought on by the researcher25 (reduced by prolonged fieldwork and engaged intersubjectivity26,27), and the double hermeneutic28,29 (biases moderated through situated analysis,30,31 respondent validation,26,27 and upholding a constructivist approach32 with a balance of emic and etic viewpoints).31,33 All presently discussed findings are derived from a larger study pertaining to choice of therapy from a sociocultural perspective; the methods for that research project are discussed in the following.
TCM was chosen as a prominent CAM modality, which, lacking current representative studies on CAM use in Hungary, was assumed to be the most popular modality based on permits issued by the National Public Health Service,34 and could thus offer high transferability of findings to CAM phenomena. The employed qualitative methods within the scope of anthropological fieldwork included participant observation and semistructured interviews. Participant observation was conducted at 4 TCM clinics in Budapest, Hungary, between January 2015 and May 2017. The clinics were elected with nonproportional quota sampling based on (1) geographical location of clinic, (2) nationality of practitioner (Hungarian and Chinese; 2 of both), sex of practitioner (male and female; 2 of both). The author conducting fieldwork wore a “student” or “researcher” tag, partook in everyday work at the clinic, and recorded data in a field journal. Patients were involved in the study through observing their admittance to the clinic (N = 49) or through conducting unstructured and informal interviews with them during their ongoing treatment (N = 56). Depending on opportunities and limitations in the interpersonal milieu of the field, unstructured interviews comprised topics such as: reasons behind therapy choice, illness experience, subjective evaluation of therapeutic efficacy.
Semistructured interviews were conducted with patients of TCM (N = 9) between January 2015 and July 2017. The interviews lasted about 1.5 to 2 hours and were arranged at either the TCM clinic, at the interviewee’s home, or at a public location, depending on the interviewee’s preferences. Patients were included via non-proportional quota sampling from the sites of participant observation and other clinics, based on the following criteria: (1) nationality of patient (all Hungarian), (2) sex (two-thirds female), and (3) location of TCM clinic (maximum variety). All interviews comprised the following thematic blocks: concepts of world (ontology and epistemology), relation to majority society and in-groups, concepts of man (constituents and their interplay), concepts of illness (typology, etiology, images), concepts of health (healing process and images of health), the patient journey (from illness onset to present), and therapy choice (reasons for choosing TCM, mode of coming into contact with it, etc). The interviews were sound recorded and transcribed verbatim.
Coding was performed in 3 stages:
Stage 1: Free, inductive, line-by-line coding was performed by one author, the codes were kept dynamic for about one-third of the fieldwork duration, then tentative code systems were developed, and data were coded accordingly.
Stage 2: Post fieldwork, 2 raters, working independently, coded the data inductively; the 2 code systems were triangulated, the few rivaling codes were negotiated until consensus was achieved and the final version of the 2 code systems were drawn up (see below). During stages 1 and 2, all raters employed Interpretative Phenomenological Analysis (IPA) as their analytical method.28,35
Stage 3: Two raters, working independently, performed a deductive recoding of the data with the 2 code systems; the second author cross-checked the coding during the process of analysis.
All coding was performed with Atlas.ti 6.0 software; data from the field journal and the semistructured interviews was pooled into a separate hermeneutic unit used in the process of analysis. Tentative findings were checked for validity via respondent validation with confidants in the field and triangulated19 with various colleagues from multiple disciplines throughout the process of interpretation. In qualitative methods, quantification is rarely an objective,20,36 this stands for the present research as well concerning the coding itself; notwithstanding, quantified information is presented where quantifying proves to be relevant and informative (eg, patient demographics, illness distribution, etc).
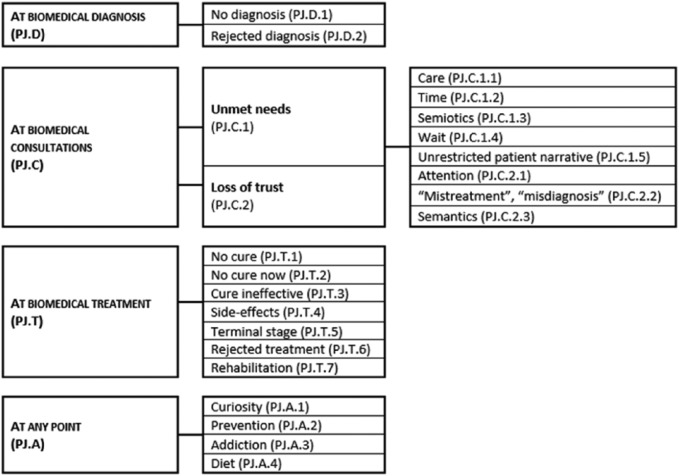
The first code system (Patient Journey or PJ) displays at which point the patient may turn to TCM/CAM with regard to their patient journey and illness trajectory. Master codes were based on the preconception that the patient journey reveals points of entry into CAM and reasons for employing TCM, while also disclosing ways in which the patient remains in dialectic with biomedicine. The PJ code tree (Figure 1) displays the inductively generated code system employed to code the data.
Figure 1.
Patient Journey (PJ) code tree.
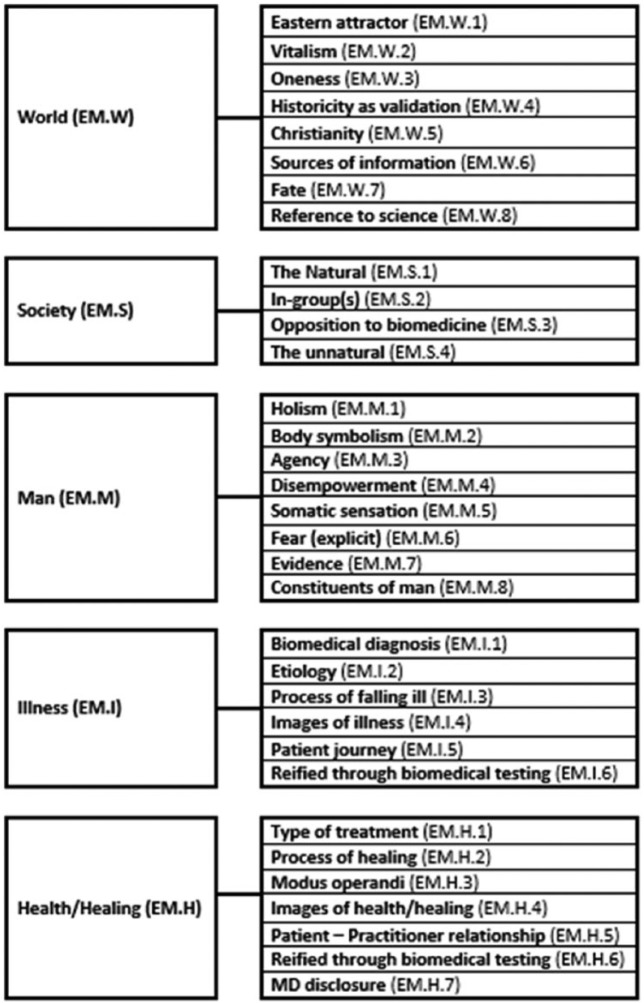
The second code system, Explanatory Model or EM (Figure 2), displays how the individual reflects on their assumptive world and consists of master codes: world (EM.W), society (EM.S), man (EM.M), illness (EM.I), and health (EM.H). EM master codes were created to be compatible with the interview structure and based on the preconception that therapy choice is in interaction with the patient’s explanatory model (concepts of world, society, man, illness, health).
Figure 2.
Explanatory Model (EM) code tree (simplified).*
*The expression “man” in this context connotes “human.”
The results presented below were derived from various codes from both code systems.
Employed Patient Journey (PJ) codes:
At biomedical diagnosis (PJ.D): No diagnosis (PJ.D.1)
At biomedical consultations (PJ.C): Unmet needs (PJ.C.1), Loss of trust (PJ.C.2);
At biomedical treatment (PJ.T): No cure (PJ.T.1), No cure now (PJ.T.2), Cure ineffective (PJ.T.3,) Terminal stage (PJ.T.5) and Rejected treatment (PJ.T.6)
Employed Explanatory Model (EM) codes:
Vitalism (EM.W.2), Oneness (EM.W.3), Fate (EM.W.7), Opposition to biomedicine (EM.S.3), The natural (EM.S.1), In-group(s) (EM.S.2), The unnatural (EM.S.4), Holism (EM.M.1), Body symbolism (EM.M.2), Somatic sensation (EM.M.5), Constituents of man (EM.M.8), Etiology (EM.I.2), Process of falling ill (EM.I.3), Images of illness (EM.I.4), Type of treatment (EM.H.1), Images of health/healing (EM.H.4), MD disclosure (EM.H.7)
For analysis, codes were integrated across various domains to perform cross-sectional interpretations in a systemic approach. The findings below pertain to the circumstances, reasons, and consequences of the nonintegration of CAM and CM, a mutually exclusive therapeutic trajectory. These results are illustrated with narrative elements from patient interviews (aliases: P.J., P.H., P.G.) and the field journal (FJ); all quotes are displayed in italics and encapsulated in quotation marks. It must be stated that the scrutinized narratives are from patients only, exhibiting varying durations between events in the patient journey and their recall; the study’s scope does not extend to the investigation of the original doctor-patient interactions, merely the analysis of said narratives in order to gain a more thorough understanding of patient behavior and decision-making. Approval was gained from the Semmelweis University Regional and Institutional Committee of Science and Research Ethics, reference number: SE TUKEB 6/2015. Individuals in our study provided informed consent to participate anonymously.
Results
Demographics
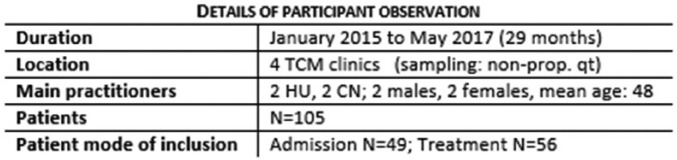
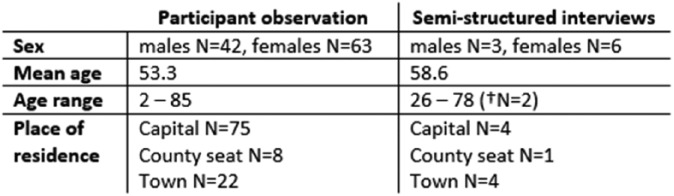
The study involved 105 patients from the 4 sites of participant observation and a further 9 patients were recruited for semistructured interviews; Figure 3 displays the details of participant observation, while Figure 4 shows the demographic information of participants. Patients were included in the study by observing their admittance to the TCM clinic (first consultation and first treatment) or by coming into contact with them during their treatment already in progress. Of the 105 patients under scrutiny, the majority received a biomedical diagnosis prior to entering the TCM clinic (N = 66, 62.8%) and almost all patients arrived with biomedical test results (N = 90, 85.7%). This clearly illustrates that most patients turned to biomedicine before seeking treatment in TCM and the relevant ethnographic data also suggests that those left without a biomedical diagnosis (N = 39, 37.1%) primarily turned to TCM in order to receive a diagnosis of their ailment, albeit a different one than the culturally dominant nosology.
Figure 3.
Details of participant observation. TCM, traditional Chinese medicine; HU, Hungarian; CN, Chinese.
Figure 4.
Patient demographics from fieldwork.
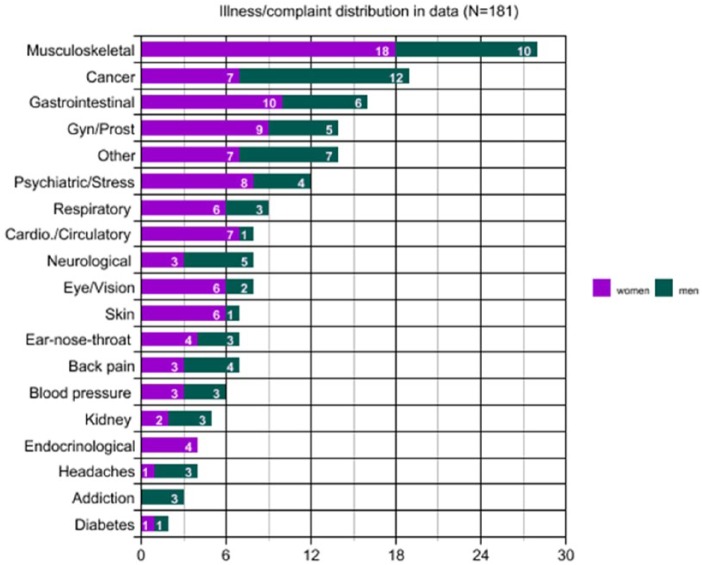
Most patients were suffering from musculoskeletal illnesses (18 females, 10 males), while the second most prominent illness in the sample was cancer, various types treated as one nosological category (7 females, 12 males). Furthermore, gastrointestinal complaints and diseases exhibited a pronounced presence (10 females, 6 males), as well as gynecological and prostate problems (9 females, 5 males). The most common illness type, which women in the sample suffered from was musculoskeletal (N = 18), while for men it was cancer (N = 12). Figure 5 displays the distribution of illness episodes in the sample; the findings are not representative; they reflect illness occurrences in the ethnographic material.
Figure 5.
Distribution of illnesses in the sample.
Patient Journeys and Entry into CAM
Reasons behind employing CAM exhibited a two-fold hermeneutic in patient narratives: on one hand, a dissatisfaction with biomedicine or negatively appraised experiences in conventional treatment, and on the other hand, cultural dispositions underlying decision-making processes related to therapeutic options. Dissatisfaction with biomedicine, the conventional health care system, or a specific physician arose from patient expectations regarding the circumstances of consultation and/or treatment, the doctor-patient relationship, as well as illness interpretation. Cultural dispositions with a marked role in decision making stemmed from broader sociocultural trends, such as a preference for what is “natural” and psychologization (placing a greater emphasis on mind or emotions compared with the body or physiological processes). Aforementioned factors intertwine with patient expectations and goals, and all of these should be viewed in their complex interplay, thus the previously identified codes and themes will be presented below in a situated manner, accentuating cases where CAM and CM were considered mutually exclusive by the patient, that is, CM and TCM were used independently of one another. It is important to note that the ethnographic material does contain patients employing CM and CAM simultaneously, frequently using the latter to manage side effects, but present study focuses on mutual exclusion.
Biomedical Consultation and Loss of Trust
Most commonly patients, entered CAM at the point of biomedical consultations (PJ.C), that is, a patient would rely solely on CM to diagnose their illness (process whereby their complaint-constellation received a nosological label) and offer a treatment for it. Yet in the midst of consultations with one or multiple physicians/specialists, the patient felt that their needs were not met in some way (PJ.C.1) or reported negatively appraised experiences, which led to a loss of trust (PJ.C.2) toward CM. Unmet needs included the patient feeling they did not receive enough attention (PJ.C.2.1) and care (PJ.C.1.1) from the biomedical professional, or did not have enough time (PJ.C.1.2) with the CM practitioner to ask questions and receive information (PJ.C.1.5).
Loss of trust toward a specific physician chiefly occurred due to semantic issues (PJ.C.2.3), the patient felt the doctor phrased information inappropriately. There were many instances also, where the patient felt the prognosis of the disease was conveyed by the doctor without empathy or left no interpretive space for retaining hope in healing. Another reason behind loss of trust was the patient feeling restricted in their narrative, that is, deeming the physician unapproachable, unavailable for questions, or not open to the patient’s illness experience and interpretation. Many patients reported the need for a closer relationship with their healer as a prerequisite for maintaining a relationship with them at all. The co-occurrence of unmet needs and loss of trust frequently resulted in the patient leaving CM, in many cases with no warning at all, and oftentimes in a serious medical condition (EM.H.7).
The vignette below was taken from an interview with a middle-aged female patient whose gallbladder had been surgically removed due to gallstones, but following biopsy she was diagnosed with a tumor, which had spread to nearby lymph nodes as well. Her narrative was recorded after receiving two curative surgical operations and being referred to another for diaphragmatic hernia.
Interviewer: You said you wouldn’t want the operation, why not?
Patient: No, not now [. . .] I wouldn’t know who to go to. I’ll tell you honestly, that doctor may be very-very knowledgeable . . . I’m not doubting him, I’m not the one to speak here, I’m a layperson, but [. . .] when I only see the doctor when he comes into our room with 30 others, they didn’t even fit into the room during the rounds, there were so many of them . . . and aside from these instances, he couldn’t be reached, I didn’t see him. I mean, come on, I want to know what happened during the surgery, how it went! And I had to beg him—after the second operation—to tell me something about how the surgery went.
Interviewer: What happened after the surgery, you woke up and then nothing, no contact . . .?
Patient: No contact, only the next morning during the rounds, but we couldn’t talk then—he just told the others what’s going on with me and then went over to the next bed. And then later, I told him, I would love to know what happened at the operation 3-4 days earlier. All he said was—and this was in the hall of the hospital where I caught him—he says, “I’m very sorry, we couldn’t solve the problem, it’s all scattered . . . and we didn’t want to operate any longer because,” he says, “you would’ve died right there on the operating table,” that’s how he told me.
[. . . The nurses] didn’t even come in, even though I asked them to pay attention to me because, you know, there was a catheter in me, a tube in me, in my nose. Imagine the catheter was in me and the next day I felt like something’s wrong and the tube was all off in every direction [. . .] and the one nurse who was—sorry for saying this—the only normal one, was like “what are 4 cannulas doing here?!” [. . .] I couldn’t even bend my fingers because they had stabbed me with those things so many times . . . they were all over the place, the infusion spilled all over, my hand was swollen . . . (P.G.)
The narrative is explicit in a dissatisfaction with care and attention received from medical personnel and this loss of trust—mostly due to staff not meeting her expectations—leads the patient to question the level of expertise provided by health care workers. The experiences and interpretations above result in the patient rejecting curative procedures and choosing an alternative medical modality with which to treat her initial illness.
Loss of trust also occurred in connection with complementary medicine use and its disclosure to the biomedical professional (EM.H.1, EM.H.7). Patients reported feeling afraid to tell their physician about employing complementary treatments or reluctant to talk about alternative therapies because of prior negative experiences or preconceptions about the doctor’s reaction. A considerable number of patient narratives contained negative remarks made by CM professionals concerning CAM, some patients voiced sentiments of feeling rejected by their CM physician when they divulged their use of CAM. Other narratives contained accounts of the patient not mentioning CAM specifically, merely a nonbiomedical illness interpretation, which was met with tension from the doctor, and left the patient feeling “not understood” (FJ). The latter is an issue of semiotics (PJ.C.1.3), or meanings, which in connection with doctor-patient communication occurred concerning illness interpretation, etiology, prognosis, and treatment (see: a priori rejection of treatment).
Many patient narratives juxtaposed commentary on biomedical consultations/hospital environment with descriptors of TCM/CAM clinics and their sociocultural environment. Frequently, these 2 environments were set in opposition to each other, the hospital described with negative content (no time for patient, little care provided, etc), “full of sick people” and “stressed out staff” (FJ) and the TCM/CAM clinics as a place where they “did not feel sick” and were cared for (FJ). Two of the 4 TCM clinics proved to be places where patients could interact with each other, not only with staff, and reported feeling social support through these interactions (EM.S.2.1, EM.S.2.4), which in their view, contributed to the experience of healing or “not feeling sick” (FJ).
A Posteriori Rejection of Biomedical Treatment
Biomedical treatment was refused by patients in the study in 2 ways: a posteriori (discontinuation after commencing treatment) or a priori (not beginning the treatment at all). While the former was more frequently connected to loss of trust in the doctor-patient relationship, the latter mostly occurred in conjunction with cultural dispositions. In cases of cancer (eg, various metastatic and nonmetastatic carcinomas), a posteriori rejection (discontinuation) of treatments such as chemotherapy and radiation therapy oftentimes transpired because the patient experienced novel somatic sensations (EM.M.5) at the onset of treatment, and due to the perceived nature of the doctor-patient relationship, felt they could not ask about or did not want to report these sensations. In some cases, the patient was asymptomatic at the onset of treatment and thus when they began to experience side effects, instead of initiating a discussion about this with their physician, they interpreted the sensations as therapeutic inefficacy or iatrogenic effect and discontinued CM treatment. In other cases, the patient stated they had attempted to discuss these novel somatic sensations with their doctor, but were refused or the conversation was cut short. Hence, in several instances for varying reasons, patients discontinued their CM treatment and began employing an alternative medical treatment.
Mutual exclusivity in connection with discontinued biomedical treatment either arose from having no prior experience or contact with CAM before “leaving” biomedicine (for reasons elaborated above), or because patients primarily aimed to be treated with conventional methods, but these cures proved to be ineffective. With regard to the latter, the ethnographic material contains instances of patients in the terminal stage of their disease using alternative treatments or patients experiencing relapse, as in the case of a Hodgkin’s lymphoma patient (male, 40s) who entered CAM after 2 unsuccessful treatment cycles in CM (2 episodes of remission-relapse), was treated with acupuncture exclusively for a period of one month, only to return to the hospital for a third round of CM treatment (FJ).
A Priori Rejection of Biomedical Treatment
Whereas the discontinuation of CM treatment was found to be linked to loss of trust in the doctor-patient relationship, the a priori rejection of biomedical treatment strongly correlated with cultural dispositions, that is, underlying preferences, cognitive and behavioral tendencies. These underlying preferences or dispositions affected the perception of etiology, biomedical cures, and treatment efficacy. All dispositions discussed below frequently yielded a therapy choice of employing TCM as an alternative treatment and not considering the utilization of the CM treatment.
The preference for the “natural” was a prominent cultural disposition affecting the perception of illness etiology and treatments. The “natural” was defined in various ways, depending on the context, as well as the explanatory model of the patient, and was delineated using affirmatory (what is “natural”; EM.S.1) and inverse images (what is “unnatural”; EM.S.4) pertaining to medical systems and treatment types (CAM vs CM). Affirmatory images of the “natural” included therapies that were “trustworthy” (through, eg, their “ancient” and/or “traditional” quality), were “pure” or “clean” (considered to be “nonsynthetic,” “nonchemical,” etc), used elements from “nature” (such as phytotherapy, herbal medicine), and mobilized the body’s “self-healing mechanisms” (such as acupuncture or bioenergy). Inverse images comprised therapies that were deemed to be chemical-based (ie, pharmaceuticals), nonselective (eg, radiation therapy), or “permanent” (eg, surgically removing problematic organ, lifelong drug treatment). Patient narratives regarding the “unnatural” also involved treatments or procedures that placed something “synthetic” or “foreign” into the body, such as in the case of cataract surgery (P.J.). The three most frequently cited biomedical treatments characterized by the “unnatural” were chemotherapy, radiation therapy, and steroid treatment; the first 2 in connection with cancerous diseases, the third concerning musculoskeletal illnesses (eg, rheumatoid arthritis).
In the process of decision making vis-à-vis choice of therapy, preferences such as the “natural” often interacted with etiological concepts, as displayed below by a patient who espoused the belief that cancer is caused by fungi:
Simoncini. Dr. Simoncini is his name, he lives in Rome, he’s an oncologist. He discovered that cancer is a type of fungus. [. . .] So fungi cause cancer. And the greatest enemy of fungi is baking soda, so he heals with baking soda. He has a lot of clients from the States as well, and what he does is—as a doctor—he washes the body out with a baking soda solution twice or three times. (P.J.)
If the etiology is deemed to be fungal, the logic of accepting such a cure exhibits an internal consistency; in the narrative the patient goes on to explain that due to a lack of financial resources, he tried a home remedy version of the treatment in order to cure his prostate cancer. Apart from presenting the above argument (etiology and course of action), the interviewee also emphasized that this treatment was developed by a biomedical doctor, thus legitimizing the treatment itself. The patient came across this information first by hearing about it from a peer, and then by searching for a “natural cure” for cancer. These 2 domains frequently co-occurred in the ethnographic data: hearing about the therapy from a friend or family member and performing an Internet search based on previous dispositions that most certainly yielded a reinforcement of those preferences and preconceptions (FJ) by virtue of the keywords and selection mechanisms employed during the search.
Another important disposition in a priori treatment rejection was an understanding of illness experience centered on psychologization, spurring a strong inclination toward psychosocial etiology (EM.I.2.1). Most patients in the sample demonstrated a full or partial commitment to psychosocial etiology, as opposed to espousing other explanatory models, such as taking nutritional (EM.I.2.4), environmental (EM.I.2.2), or genetic factors (EM.I.2.6) into consideration. If the patient favored a psychosocial explanation concerning their illness, they were more likely to choose a type of medicine that addressed the psychosocial domain, such as New German Medicine or Reiki, for example. The lay rationale being that if the problem was successfully resolved in the psychosocial realm, that is, the “root” of their physical illness was attended to, then the “symptom” (physical disease) would be healed as well (EM.I.3, EM.H.4, EM.M.1). In many cases, the patient a priori rejected the biomedical treatment because it was not targeting the “real problem,” as the narrative from the patient in her early 40s, who gives an account of a previous, long-standing gynecological illness:
Precisely because if we think that our thoughts cause illness, then a bad thought [. . .] will make you sick, but . . . if you have a positive attitude and have a realization then . . . then that can heal you. [. . .] And as I understood this and started to deal with it consciously and not . . . not by taking medicine . . . because, you know, you go to the gynecologist and you try everything and nothing works, the problem always comes back. [. . .] And when I understood what could be the cause of this in me, then I decided that I had had enough, I would resolve it and let it go. [. . .] So somehow I clarified things, or had realizations about the root of the problem, I went down there and solved it, and so afterwards everything was okay. (P.H.)
The narrative expounds a psychosocial etiology, believing that the physical disease was caused by an emotional problem and subsequent to “realizations” and psychological change, the illness went into remission. It is also noteworthy that the narrative gives an account of mutual exclusivity among medical modalities: while previously she had only adhered to medicine prescribed by the gynecologist, later, through a change in etiology and explanatory model, favored only TCM as a means of “going down” to “the root of the problem.”
Aside from a tendency to psychologize the illness experience (eg, adhering to psychosocial etiology), the ethnographic material shows a strong tendency toward vitalism (EM.W.2, EM.W.3, EM.W.7), that is, a belief in “universal energy.” As TCM itself employs this rhetoric (energetic system, meridian, qi, etc)—albeit with various definitions and interpretations—it is logical to assume that the patient either espouses a version of vitalist beliefs prior to using TCM or is encultured into this paradigm during use. According to the data from the participant observation and the semistructured interviews, psychosocial etiology is very much linked to vitalism: not all psychosocial etiologies involve vitalist concepts, but all vitalists are psychosocial as well. In the vitalist worldview health was seen as an unimpeded flow of energy within the body, while illness occurred when the energetic system was inhibited, too much energy, too little energy, or no energy was present (ie, “block” or “blockage”). In most versions of vitalism, blocks in the flow of energy are caused by trauma, fear, and/or negatively appraised emotions, which can be considered a form of psychosocial etiology as well.
Both psychosocial and vitalist etiologies adhere to a disposition toward symbolic illness interpretation (EM.I.4.3), constituting the last discussed disposition affecting a priori treatment rejection. A large portion of patients adhering to psychosocial or vitalist etiologies believed their disease to be symbolic in the sense that it was “not by chance” that the illness occurred where it did (ie, affected body part, organ) and this conviction contributed greatly to their illness interpretation. Many patients retained specific notions on body symbolism (EM.M.2): for example, the right part of the body represents the masculine/the father/the outer world, while the left side represents the feminine/the mother/the inner world. Also, notions regarding organ symbolism, such as: the kidney symbolizes interpersonal relationships and is the “seat of fear,” the throat symbolizes self-expression and self-restraint (especially verbally), the thyroid is the center of self-appraisal, and so on (FJ). These body maps are culturally and subculturally determined and exhibited a strong effect on illness interpretation and therapy choice.
All discussed dispositions of psychologization influencing the a priori rejection of biomedical treatment (psychosocial etiology, vitalism, illness symbolism) are congruent in that they assume an asymmetric interplay among human constituents (EM.M.8). In other words, among a person’s constituents in the patent’s explanatory model (eg, body, mind, soul, consciousness), the body is thought of as most inferior or more the receptive end of a communication, rather than the signal-generating end. The body was frequently described as a mirror to the mind or the soul, serving as a warning mechanism to bring attention to “deeper” psychosocial concerns. Furthermore, the body served not only as a symptom of disease but also as a means of achieving greater well-being—a mirror for both falling ill and healing.
In sum, PJ and EM codes in the collected ethnographic data were analyzed with regard to the reasons and circumstances of mutually exclusive CAM versus CM use, though, it must be emphasized again that not all patients in the study treated therapy choice in such a polarized manner. When the modalities were considered mutually exclusive, it occurred in instances where there was an explicit dissatisfaction with biomedicine or negatively appraised experiences in conventional treatment and/or the patient espoused cultural dispositions that had a strong effect on decision-making processes related to therapeutic options. CM treatments were rejected a posteriori (discontinuation after commencing treatment) or a priori (before commencing treatment). In the former case, oftentimes the perceived inability to discuss novel somatic sensations stemming from biomedical treatments left the patient with a negative interpretation and affected the subjective evaluation of treatment efficacy to an extent where it was discontinued. In case of a priori discontinuation, 2 cultural dispositions played a significant role in the decision: a preference for the “natural” and psychologization (manifesting in psychosocial etiology, vitalism, and illness symbolism). These underlying preferences or dispositions affected the perception of etiology, biomedical cures, and treatment efficacy, assuming an influential role in therapy choice.
Discussion
Many authors working in the field of CAM research suggest analyzing therapy choice with regard to “push factors” (repelling the patient from CM) and “pull factors” (attracting patients to CAM).37-41 Findings of the present study may also be viewed as such: from the patient point of view, lack of attention and care, poor doctor-patient communication constitute one “side” of the individual favoring CAM, while the cultural dispositions comprise another “side” of the same coin. Yet this dichotomy may shroud the true complexity of individual cases, which in this study, were examined via the patient journey and cultural dispositions.
The analysis was focused on instances were CAM and CM were considered by the patient as mutually exclusive strategies in coping with or curing illness, either as part of a patient journey that commenced with the domain of biomedicine and continued on to CAM use or began with an a priori rejection of CM treatment. As the possible sources of such a polarized treatment perspective previous negative experiences and cultural dispositions were discussed, which in many cases worked in tandem to influence patient decision-making processes. Stepping one contextual frame “outward” one finds biomedicine and CAM in the arena of the health care market on a societal level; a scrutiny from this perspective lends to the understanding of polarized therapy choice.
Hungary lacks long-standing social institutions of integration among various medical modalities and has only seen an increase in said treatments since the 1990s. The law divides CAM into 2 groups, one which comprises modalities that necessitate a biomedical diploma in order to be practiced, and the other contains modalities that do not42; TCM belongs to the former group. Such a division among CAM suggests a relatively high degree of state and biomedical control over various medicines, raising the prestige of certain modalities over others, creating the impression of scientific legitimization in some cases. Yet this differentiated treatment of CAM also unveils an intense rivalry within the health care market among various medical systems and the explanatory models (concepts of world, man, health, illness) that they espouse. This rivalry may lend considerably to the polarization patients often exhibit concerning therapy choice. Moreover, this competition not only signifies therapy choice, but also involves existential questions such as: What is illness and how can we judge treatment efficacy? How can health be defined and who can be considered a healer? The consequences of the given answers run far deeper than the employed therapy and permeate issues of professionalization, professional prestige, legal regulation, institutionalization, financial interest, and so on.
The fact that Western concepts of health are changing is accurately mirrored in the transformation of the World Health Organization’s definition departing from health merely regarded as the absence of disease, to describing it as biological, psychological, and social well-being.43 In 1998, an Executive Board Special Group for the review of the Constitution of the World Health Organization, requested an amendment proposing to add spiritual well-being to the definition.44 However, the proposal was not discussed again in subsequent Executive Board meetings; despite the critiques regarding the current definition of health maintained by the constitution, it has not yet been modified to take into account the spiritual dimension.45
The mere fact that a multifaceted definition and even a spiritual dimension is present in scientific discourse suggests a paradigm shift, not only brought about by a more elaborate understanding of biopsychosocial health determinants46,47 but also by a proliferation of information.48,49 Thus, with a changing definition of health and illness come different patient expectations concerning treatments and the doctor-patient relationship, yet also, vice versa: changing concepts of physicians, illness, health, and patient behavior are altering definitions of health. The transformation in the conceptual realm is mirrored and affected by changes in praxis, as in patient information-seeking behavior and illness presentation, for example. The rise of CAM health practices could be related to changes in conceptualizations of health and illness, but also to transformations in the ideas of how health is to be achieved,50 as well as increased consumerism in the health arena48,51 aligned with a preference for engagement and empowerment in the therapeutic process.52
Proliferating information is a phenomenon of our globalizing world, and in this milieu the individual may create a “hybrid” worldview in a process of “cultural creolization”—a melding of various cultural traditions, concepts, practices.49 This “hybridization” occurs concerning concepts of illness and therapy choice as well, hence, as most physicians may verify, the patient frequently arrives to the biomedical consultation with elaborate theories of illness causation and protocol. Furthermore, the patient may go directly to a CAM practitioner if this is what they perceive to be congruent with their worldview and assumed etiology. Consequently, the mode of information seeking and filtering, the way that information is being processed and interpreted, the underlying cultural dispositions affecting these processes all have a strong effect on choice of therapy.53 While seeking help, the patient will look for a therapy/healer congruent with their worldview and with the experiences that peers have shared with them about their own illness trajectory. Subsequently, the subjective evaluation of therapeutic efficacy will be largely dependent on the level of trust the patient feels toward the practitioner.
A pivotal aspect of the establishment and cultivation of trust is that the patient feels they are understood by the practitioner. As many studies have asserted, medical consultation is the exchange of 2 explanatory models, that of the doctor and that of the patient.54,55 Thus, not only must the medical system and the treatment be congruent with the meaning the patient constructs concerning their illness but also the patient yearns to feel that this meaning is shared by the healer. Because of the “holistic” nature of many CAM treatments, this shared meaning is more easily constructed than in biomedicine. CAM modalities represent one of the earliest manifestations of the increasing significance of “holistic” conceptualizations of personhood.50 These modalities are frequently treatments embedded in a medical system, which in turn is part of a larger cultural system, consequently, the treatment is considered “holistic” because it addresses many (or all perceived) aspects of an individual: biological, psychological, social, and so on, and these realms are interlaced with the same ideology.
Another attribute of such “holism” is that the ideology furnishes the individual with a set of symbols that can be tailored to create personal meaning concerning illness etiology and interpretation. Such an ideology may involve “elements” (eg, 5 elements in TCM), “universal energy” (eg, Reiki), or body/organ symbolism (eg, the kidney is a symbol of interpersonal relationships), for example. On construction of this personal meaning, the patient may feel they have greater agency over their illness, reduced anxiety, and may exhibit a need to see their interpretations mirrored by the healer.48
Biomedical doctors may have trouble identifying with such notions and western medicine in general does not have such a symbolic system that may be personalized in a process of meaning-making. This may lead the patient to feel biomedical explanations are lacking in meaning56 or the doctor is lacking in empathy, when in fact, this situation may also be viewed as a difference in medical subculture and normative beliefs. Furthermore, this may elicit a turn to CAM because many of said modalities are equated with a “holistic” understanding of personhood and well-being, providing the patient with more agency and encouraging personal meaning-making. Some scholars argue that conventional medicine lacks this approach, while “holistic” treatments are exhibiting increasing consumer demand.50
The above description of “holism” and well-being is greatly compatible with Western tendencies of psychologization, which in terms of illness experience and causation signifies that the patient emphasizes psychological aspects rather than the biological domain. The present findings linked psychologization with a belief in psychosocial etiology, vitalism, and the symbolic interpretation of illness, all of which denoted cultural dispositions with the potential of polarizing therapy choice. Many patients espousing these attitudes believe that one either deals with the illness in a “conscious” manner or takes medicine. “Consciously” dealing with physical illness frequently connotes “searching for its real roots,” that is, psychological and/or social problems, while “taking medicine for it” is perceived as only treating the “symptom” and ignoring “the cause.” This polarization occurs because of a conviction concerning etiology and hence acting in a (subjectively) congruent manner concerning therapy choice: if the illness is caused by emotional problems, one needs to treat it with something that employs or has an effect on emotions.57
Psychologization and “holism” can be viewed in a larger context of human tendencies to make sense of their illness experience involving physical ailments by using the same interpretive frame as employed for psychological and social phenomena, as well as life events.55,56 Individuals generally exhibit a need for cognitive consistency58 and such cross-domain ideology may answer this demand, especially in times of physical illness when the need for meaning is increasingly high.31,53 Psychologization may also occur in aspiration for agency: the patients may feel they have more control over their emotion and cognition compared with their physical realm, and thus adhere to the supremacy of the psyche.
Aside from “holism” and psychologization, a preference for the “natural” also plays a vital role in therapy choice59 and in a mutually exclusive view of CM/CAM use. In connection with issues of health care, cultural synonyms for the “natural” include “clean,” “ancient/traditional,” “harmless,” “self-healing,” and “herbal”; while cultural antonyms include “synthetic,” “artificial,” “chemical,” and “drug/medicine.” Thus, a preference for “natural treatments” proves to be a push and a pull factor simultaneously: this disposition may be responsible for creating an anti-drug attitude, especially concerning painkillers and “nonselective treatments,” such as chemotherapy and radiation therapy, but may also create a tendency to choose treatments that employ herbs and/or trigger the “self-healing mechanisms” of the body (as many CAM modalities are conceptualized). Drug treatments may be refused because of their “unnatural” or “chemical” character or for the perceived danger of “getting addicted.”
The preference for the “natural” may be associated with a negative appraisal of humanity and Western values in a general sense, especially phenomena related to modernity. Modern health worries (MHW), that is, perceived detrimental effects on health by modern and/or technological features of daily life, have been found to be significantly associated with CAM use.60,61 Many of these items are related to this sense of “natural versus unnatural” or humanity’s relation to the environment, such as pollution (air, water, earth, etc), radiation (from cell phones, power lines, X-rays, etc), and use of chemicals (food additives, pesticides, hormones, etc). MHW can be linked to the interdisciplinary term “Anthropocene,” demarcating the current era in which humanity has had a major influence on the earth’s ecosystems, climate, and natural resources, characterized by an exponential increase in population, energy production, and so on.62 If the individual exhibits high values in MHW scales, they are more likely to interpret the Anthropocene, the current era, negatively. There is extensive literature not only on the association between MHW and CAM use but also attitudes toward science, Medical Conspiracy Theories (MCT), somatosensory amplification, and so on.61,63,64 All of the aforementioned phenomena are connected to notions of what is “natural” concerning cultural values, medical procedures, and treatments; that which the individual deems to be “natural” will most likely be associated with what is “healthy,” “harmless,” and “trustworthy” as well, hence demonstrating a strong influence on therapy choice. These associations regarding the “natural” and their cultural inverses (chemical, human-made, synthetic, etc) are well-documented in CAM literature around the globe.59,65-68
A mutually exclusive view of conventional medicine and CAM use arose in part from the specific sociocultural circumstances of the location of research: the particulars of Hungarian regulations, processes of institutionalization, competition among market actors and sectors, as well as a lack of social institutions of integration. The health care market, both on a societal and global level, is a competitive arena comprising not only rivaling modes of treatment and medical modalities but also competing worldviews and attitudes. Shifting definitions of illness and health in the West have influenced and mirrored sociocultural changes, which are occurring in a milieu of information production, proliferation, and widespread dissemination, causing “cultural creolization” and hybrid worldviews. Prevailing cultural dispositions in this social environment, such as “holism” and the “natural,” may have a pivotal role in polarizing therapy choice among a portion of individuals inclined to the mutual exclusivity of CM and CAM. Notwithstanding, patients retain a need for constructing meaning with regard to their illness, and both the chosen treatment and the healer-patient interaction must be seen as congruent with this meaning in order to maintain cognitive consistency. Meaning and decision making concerning matters of health care will always be coalesced with previous experiences, preconceptions, associations, and dispositions regarding what is held “true” and “trustworthy.”
Limitations
The study had several limitations, including those stemming from the chosen methods: qualitative research lends a deeper understanding of phenomena but fails to provide accurate information on their prevalence. Although TCM offers highly transferable findings concerning CAM use in Hungary, the level of international transferability is unclear. While the participant observation involved a large sample, unstructured interviews are not highly comparable; semistructured interviews yield strong avenues of comparison, but this study comprised a small sample (albeit an average number for qualitative research). It must also be restated that patient journeys are dependent on a multitude of factors, such as illness type, time of onset, available CM treatments and their appraisal, patient interpretation of illness, severity and interpretation of symptoms, evaluation of available CAM treatments, available sources of information and their interpretation, and so on. As all of these influence patient decision making and choice of therapy, meticulous situated analysis is necessary. Additionally, although nonproportional quota sampling is an adequate mode of qualitative sampling, the designated subgroups may not reflect all possible analytical categories and thus cannot be considered representative of the whole sample (ie, TCM users in Hungary). Further qualitative and quantitative studies are needed to verify findings both on a national and international level. Additional investigations are also needed concerning mutual exclusivity in CAM/CM use conducted in a sample of patients not employing CAM (only CM), as the present study focused on patient journeys dominated by or ending in alternative treatments.
Conclusions
The relevance of meaning-making in CAM health practices is related to the patient equating the notion of health with well-being. From this perspective, well-being is constructed as something that is available for even those people who may be terminally ill50 but still able to construct personal meaning and a subjective assessment about how they experience and feel. Accordingly, well-being refers not only to biologically defined health, but rather the ability to live a life that is experienced as personally meaningful. Thus, well-being emerges through the process of making sense of difficult situations in a manner that is often felt to be positive, which relates to personal fulfilments and can be characterized as a position where the person feels they have control over their existence, experience, and behavior.50 From this perspective, well-being is also related to agency and the process of dealing with the illness experience in a conscious manner, which in some cases induced the construction of a psychosocial etiology concerning a health problem.
The process of meaning-making and choosing a specific form of treatment that fits those needs, is linked not only to changing notions of health and illness but also to shifting conceptualizations of self, identity, and the practitioner-patient relationship. Mutual exclusivity in CM and CAM use may mirror competition in the health care market on a societal level, as well as reflect loss of trust in the doctor-patient relationship. Global trends in cultural dispositions are also responsible in creating a polarized view of therapy choice, as patients may believe that maintaining congruence with some worldviews, attitudes, or etiologies requires exclusive devotion to one medical modality. Mutual exclusivity can be detrimental to patient well-being insofar as it exacerbates problems in doctor-patient communication or prevents the patient from receiving optimal care for their ailment.
A polarized therapy choice is assumed to be far more frequent in cases where desperation does not characterize the patient’s situation, that is, in cases of chronic or reoccurring illness, or undiagnosed ailments. When the patient is in a state of desperation, it is presumed that integration of medical modalities is preferred because the patient is trying to recover urgently, or at least achieve an experience of well-being by any means possible. Thus, in the cases where polarized therapy choice was exhibited in, for example, the terminal stage of cancer, it either occurred due to biomedicine only offering the prospect of palliative (not curative) care to the patient, or due to a loss of trust in biomedicine because of a series of negatively appraised events/circumstances.
Mirrored in the articulation of an individual’s illness trajectory involving different health practices is a tension that is also reflected in the struggles of the health care system to more adequately understand health/illness processes from a pluralistic perspective. The power relations in the health arena (among CAM/CM practitioners and systems) play a role in legitimizing or undermining different health practices, which as consequence affects the possibility of integrating them into the processes of care. Nonetheless, those persons who formulate their health/illness/care trajectory as an integration of practices from a plural perspective, are transcending health systems in their endeavor to negotiate, resist, and re-create the definitions, categories, and practices that health institutions provide to them.
Acknowledgments
The authors wish to thank co-raters Luca Wilson and Bence Sütő, as well as the Fulbright Association, the Rosztoczy Foundation, and EFOP-3.6.3-VEKOP-16-2017-00009.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report. 2015;(79):1-16. [PMC free article] [PubMed] [Google Scholar]
- 2. Ernst E. Prevalence of use of complementary/alternative medicine: a systematic review. Bull World Health Organ. 2000;78:252-257. [PMC free article] [PubMed] [Google Scholar]
- 3. Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of complementary and alternative medicine (CAM) use by the general population: a systematic review and update. Int J Clin Pract. 2012;66:924-939. [DOI] [PubMed] [Google Scholar]
- 4. Arthur K, Belliard JC, Hardin SB, Knecht K, Chen CS, Montgomery S. Practices, attitudes, and beliefs associated with complementary and alternative medicine (CAM) use among cancer patients. Integr Cancer Ther. 2012;11:232-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Molassiotis A, Fernandez-Ortega P, Pud D, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16:655-663. [DOI] [PubMed] [Google Scholar]
- 6. Eardley S, Bishop FL, Prescott P, et al. A systematic literature review of complementary and alternative medicine prevalence in EU. Forsch Komplementmed. 2012;19(suppl 2):18-28. [DOI] [PubMed] [Google Scholar]
- 7. Söllner W, Maislinger S, DeVries A, Steixner E, Rumpold G, Lukas P. Use of complementary and alternative medicine by cancer patients is not associated with perceived distress or poor compliance with standard treatment but with active coping behavior: a survey. Cancer. 2000;89:873-880. [DOI] [PubMed] [Google Scholar]
- 8. Yates JS, Mustian KM, Morrow GR, et al. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Support Care Cancer. 2005;13:806-811. [DOI] [PubMed] [Google Scholar]
- 9. Faith J, Thorburn S, Tippens KM. Examining CAM use disclosure using the behavioral model of health services use. Complement Ther Med. 2013;21:501-508. [DOI] [PubMed] [Google Scholar]
- 10. Adler SR, Fosket JR. Disclosing complementary and alternative medicine use in the medical encounter: a qualitative study in women with breast cancer. J Fam Pract. 1999;48:453-458. [PubMed] [Google Scholar]
- 11. Davis EL, Oh B, Butow PN, Mullan BA, Clarke S. Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: a systematic review. Oncologist. 2012;17:1475-1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Soós SÁ, Jeszenői N, Darvas K, Harsányi L. Complementary and alternative medicine use in surgical patients [in Hungarian]. Orv Hetil. 2016;157:1483-1488. [DOI] [PubMed] [Google Scholar]
- 13. Bishop FL, Lewith GT. Who uses CAM? A narrative review of demographic characteristics and health factors associated with CAM use. Evid Based Complement Alternat Med. 2010;7:11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Xu W, Towers AD, Li P, Collet JP. Traditional Chinese medicine in cancer care: perspectives and experiences of patients and professionals in China. Eur J Cancer Care (Engl). 2006;15:397-403. [DOI] [PubMed] [Google Scholar]
- 15. Bishop FL, Yardley L, Lewith GT. Why consumers maintain complementary and alternative medicine use: a qualitative study. J Altern Complement Med. 2010;16:175-182. [DOI] [PubMed] [Google Scholar]
- 16. Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548-1553. [DOI] [PubMed] [Google Scholar]
- 17. Hunt KJ, Coelho HF, Wider B, et al. Complementary and alternative medicine use in England: results from a national survey. Int J Clin Pract. 2010;64:1496-1502. [DOI] [PubMed] [Google Scholar]
- 18. Arnault DS. Cultural determinants of help seeking: a model for research and practice. Res Theory Nurs Pract. 2009;23:259-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358:483-488. [DOI] [PubMed] [Google Scholar]
- 20. Green J, Britten N. Qualitative research and evidence based medicine. BMJ. 1998;316:1230-1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chapple A, Rogers A. Explicit guidelines for qualitative research: a step in the right direction, a defence of the ‘soft’ option, or a form of sociological imperialism? Fam Pract. 1998;15:556-561. [DOI] [PubMed] [Google Scholar]
- 22. Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park, CA: Sage; 1985. [Google Scholar]
- 23. Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf. 2004;22:63-75. [Google Scholar]
- 24. Eriksen TH. Small Places, Large Issues: An Introduction to Social and Cultural Anthropology. 2nd ed. London, England: Pluto Press; 2001. [Google Scholar]
- 25. Giorgi A. The role of observation and control in laboratory and field research settings. Phenomenol Pedagogy. 1986;4:22-28. [Google Scholar]
- 26. Spradley JP, Baker K. Participant Observation. New York, NY: Holt, Rinehart & Winston; 1980. [Google Scholar]
- 27. Babbie E. The Practice of Social Research. Belmont, CA: Wadsworth; 2007. [Google Scholar]
- 28. Smith JA, Osborn M. Interpretative phenomenological analysis. In: JA Smith, ed. Qualitative Psychology: A Practical Guide to Research Methods. London, England: Sage; 2008:53-80. [Google Scholar]
- 29. Leder D. Clinical interpretation: the hermeneutics of medicine. Theor Med. 1990;11:9-24. [DOI] [PubMed] [Google Scholar]
- 30. Ryle G. The Concept of Mind. New York, NY: Routledge; 2009. [Google Scholar]
- 31. Geertz C. The Interpretation of Cultures: Selected Essays. New York, NY: Basic Books; 1973. [Google Scholar]
- 32. Berger PL, Luckmann T. The Social Construction of Reality: A Treatise in the Sociology of Knowledge. London, England: Penguin Books; 1966. [Google Scholar]
- 33. Headland TN, Pike K, Harris M. Emics and Etics: The Insider/Outsider Debate (Frontiers of Anthropology). Thousand Oaks, CA: Sage; 1990. [Google Scholar]
- 34. Varga O. Integration of Complementary and Alternative Medicine Into Modern Medicine With Special Emphasis on Medical Education and Legal Regulation in Hungary [in Hungarian] [PhD thesis]. Debrecen, Hungary: Debreceni Egyetem; 2007. https://dea.lib.unideb.hu/dea/bitstream/handle/2437/5384/Varga_Orsolya_ertekezes.pdf?sequence=5. Accessed September 1, 2018. [Google Scholar]
- 35. Rácz J, Kassai S, Pintér J. Az Interpretatív Fenomenológiai Analízis (IPA) mint kvalitatív pszichológiai eszköz bemutatása. Magyar Pszichológiai Szemle. 2016;71:313-336. [Google Scholar]
- 36. Whittaker A. Qualitative methods in general practice research: experience from the Oceanpoint Study. Fam Pract. 1996;13:310-316. [DOI] [PubMed] [Google Scholar]
- 37. Furnham A, Vincent C. Reasons for using CAM. In: M Kelner, B Wellman, B Pescosolido, M Saks, eds. Complementary and Alternative Medicine: Challenge and Change. Amsterdam, the Netherlands: Harwood Academic; 2000:61-78. [Google Scholar]
- 38. Bahall M. Complementary and alternative medicine usage among cardiac patients: a descriptive study. BMC Complement Altern Med. 2015;15:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McLaughlin D, Lui CW, Adams J. Complementary and alternative medicine use among older Australian women—a qualitative analysis. BMC Complement Altern Med. 2012;12:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pawluch D, Cain R, Gillett J. Lay constructions of HIV and complementary therapy use. Soc Sci Med. 2000;51:251-264. [DOI] [PubMed] [Google Scholar]
- 41. Stevinson C, Ernst E. Why patients use complementary and alternative medicine. In: E Ernst, MH Pittler, B Wider, eds. The Desktop Guide to Complementary and Alternative Medicine. An Evidence-Based Approach. London, England: Mosby Elsevier; 2006:501-510. [Google Scholar]
- 42. Ministry of Health, Hungary. Act CLIV of 1997 on health. https://www2.ohchr.org/english/bodies/cescr/docs/E.C.12.HUN.3-Annex10.pdf. Accessed September 1, 2018.
- 43. International Health Conference. Constitution of the World Health Organization. 1946. Bull World Health Organ. 2002;80:983-984. [PMC free article] [PubMed] [Google Scholar]
- 44. World Health Organization. Review of the Constitution of the World Health Organization: report of the Executive Board special group. 101st Session, Agenda item 7.3, EB 101.R2. http://apps.who.int/gb/archive/pdf_files/EB101/pdfangl/angr2.pdf. Accessed September 1, 2018.
- 45. Chirico F. Spiritual well-being in the 21st century: it’s time to review the current WHO’s health definition? J Health Soc Sci. 2016;1:11-16. [Google Scholar]
- 46. Birchera J, Kuruvillab S. Defining health by addressing individual, social, and environmental determinants: new opportunities for health care and public health. J Public Health Policy. 2014;35:363-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Huber M, Knottnerus JA, Green L, et al. How should we define health? BMJ. 2011;343:d4163. [DOI] [PubMed] [Google Scholar]
- 48. Kelner M, Wellman B. Health care and consumer choice: medical and alternative therapies. Soc Sci Med. 1997;45:203-212. [DOI] [PubMed] [Google Scholar]
- 49. Van Wolputte S. Hang on to your self: of bodies, embodiment, and selves. Annu Rev Anthropol. 2004;33:251-269. [Google Scholar]
- 50. Sointu E. The search for wellbeing in alternative and complementary health practices. Sociol Health Illn. 2006;28:330-349. [DOI] [PubMed] [Google Scholar]
- 51. Goldstein M. The emerging socioeconomic and political support for alternative medicine in the United States. Ann Am Acad Pol Soc Sci. 2002;583:44-63. [Google Scholar]
- 52. Hoch D, Ferguson T. What I’ve learned from E-patients. PLoS Med. 2005;2:e206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Verhoef MJ, Mulkins A, Carlson LE, Hilsden RJ, Kania A. Assessing the role of evidence in patients’ evaluation of complementary therapies: a quality study. Integr Cancer Ther. 2007;6:345-353. [DOI] [PubMed] [Google Scholar]
- 54. Helman CG. Culture, Health and Illness. Oxford, England: Butterworth-Heinemann; 1994. [Google Scholar]
- 55. Kleinman A. Patients and Healers in the Context of Culture. Berkeley, CA: University of California Press; 1980. [Google Scholar]
- 56. Stratton TD, McGivern-Snofsky JL. Toward a sociological understanding of complementary and alternative medicine use. J Altern Complement Med. 2008;14:777-783. [DOI] [PubMed] [Google Scholar]
- 57. White M, Verhoef M. Cancer as part of the journey: the role of spirituality in the decision to decline conventional prostate cancer treatment and to use complementary and alternative medicine. Integr Cancer Ther. 2006;5:117-122. [DOI] [PubMed] [Google Scholar]
- 58. Festinger L. A Theory of Cognitive Dissonance. Stanford, CA: Stanford University Press; 1962. [Google Scholar]
- 59. Connor LH. Relief, risk and renewal: mixed therapy regimens in an Australian suburb. Soc Sci Med. 2004;59:1695-1705. [DOI] [PubMed] [Google Scholar]
- 60. Köteles F, Simor P, Czető M, Sárog N, Szemerszky R. Modern health worries—the dark side of spirituality? Scand J Psychol. 2016;57:313-320. [DOI] [PubMed] [Google Scholar]
- 61. Furnham A. Are modern health worries, personality and attitudes to science associated with the use of complementary and alternative medicine? Br J Health Psychol. 2007;12(pt 2):229-243. [DOI] [PubMed] [Google Scholar]
- 62. Zalasiewicz J, Williams M, Haywood A, Ellis M. The Anthropocene: a new epoch of geological time? Philos Trans A Math Phys Eng Sci. 2011;369:835-841. [DOI] [PubMed] [Google Scholar]
- 63. Lahrach Y, Furnham A. Are modern health worries associated with medical conspiracy theories? J Psychosom Res. 2017;99:89-94. [DOI] [PubMed] [Google Scholar]
- 64. Freyler A, Kohegyi Z, Köteles F, Kökönyei G, Bárdos G. Modern health worries, subjective somatic symptoms, somatosensory amplification, and health anxiety in adolescents. J Health Psychol. 2013;18:773-781. [DOI] [PubMed] [Google Scholar]
- 65. Thorne S, Paterson B, Russell C, Schultz A. Complementary/alternative medicine in chronic illness as informed self-care decision making. Int J Nurs Stud. 2002;39:671-683. [DOI] [PubMed] [Google Scholar]
- 66. Harris D. The natural. Salmagundi. 2000;126-127:236-251. [Google Scholar]
- 67. McClean S., Shaw A. From schism to continuum? The problematic relationship between expert and lay knowledge—an exploratory conceptual synthesis of two qualitative studies. Qual Health Res. 2005;15:729-749. [DOI] [PubMed] [Google Scholar]
- 68. Herzlich C. Modern medicine and the quest for meaning. Illness as a social signifier. In: M Augé, C Herzlich, eds. The Meaning of Illness. Luxembourg: Harwood Academic; 1995:151-173. [Google Scholar]