Abstract
Introduction:
The aim of this study was to create an interactive computer-based education program to teach Human Immunodeficiency Virus (HIV) prevention behaviors and raise awareness of Pre-Exposure Prophylaxis (PrEP) among individuals at risk for HIV.
Methods:
An interactive education program was created and delivered to individuals who were at risk of contracting HIV. The content was divided into modules. Within each module, educational material and multiple-choice questions were presented to participants. Participants received immediate feedback for responses and financial incentives for correct responses to multiple choice questions. Mastery criteria required participants to continue in training on each module until they achieved a specified level of speed and accuracy. The modules were divided into three parts: Course 1 (HIV), Course 2 (PrEP usage) and Course 3 (HIV risk behaviors). Tests of content from all three courses were delivered before and after participants completed each course
Results:
Test scores on the content delivered in Courses 1, 2 and 3 improved only after participants completed training on Courses 1, 2 and 3, respectively. Knowledge related to HIV and PrEP was initially low, and increased following the implementation of each part of the education program.
Conclusions:
Delivering HIV prevention education through computer-based training may offer an inexpensive, convenient and effective approach to promoting awareness and knowledge of HIV prevention approaches, including the use of PrEP.
Keywords: Instructional Technology, Education, PrEP, HIV Prevention, Drug Users, Financial Incentives
INTRODUCTION
Human immunodeficiency virus (HIV) prevention strategies are important in decreasing the global incidence and prevalence of the HIV epidemic. The majority of new HIV infections occur through heterosexual contact, among injection drug users (IDUs), and in men who have sex with men (MSM)(CDC, 2016). HIV infections among these populations are transmitted via risky injection practices and sexual behaviours. Individuals who engage in these risk behaviours have been identified by the Centers for Disease Control and Prevention (CDC) as at high risk of HIV infection and in need of a high impact HIV prevention intervention, including daily use of an antiretroviral medication (i.e., Pre-Exposure Prophylaxis; PrEP) (CDC, 2014).
Daily dosing with PrEP, a drug approved by the US Food and Drug Administration and recommended by the CDC as a key factor in a high-impact prevention strategy, is a highly effective HIV prevention intervention (CDC, 2014). The CDC (CDC, 2014) and the World Health Organization (WHO) (WHO, 2017) advise that clinicians should recommend PrEP to HIV-negative adults who; are not in a monogamous relationship with an HIV-negative partner, report sexual activity in the past six months, and also meet criteria based on their specific population (MSM or heterosexually active adults). MSM who report anal sex without a condom, diagnosis of an STD, and/or an HIV-positive sexual partner are eligible for PrEP. Heterosexually active adults who are infrequent condom users with multiple partners of unknown HIV status and/or are men who have sex with men and women are also eligible for PrEP. The CDC also recommends PrEP for individuals with recent (past six month) non-prescribed injection drug use who have shared needles and/or have been in drug treatment in the past six months. Daily PrEP use reduces the risk of sexually acquired HIV by more than 90% and HIV acquired by injection drug use by more than 70% (CDC, 2014). Although the populations targeted for PrEP will change as the incidence of HIV changes and as the cost of PrEP decreases, the CDC estimates that around 1.2 million people in the US should receive PrEP (Smith et al., 2015). This figure includes 24.7% of men who have sex with men, 0.4% of heterosexually active adults, and 18.5% of adults who inject drugs who are at risk for acquiring HIV.
Awareness of PrEP’s efficacy and safety is vital in ensuring PrEP reaches its potential as a highly effective prevention tool in reducing the incidence rates of HIV. However, physicians and those individuals at substantial risk of contracting HIV are generally not aware of the availability or effectiveness of PrEP. Although PrEP awareness among physicians has increased from 24% (2009) to 66% (2015), only 17% reported having read the CDC’s PrEP clinical practice guidelines (Smith, Mendoza, Stryker & Rose., 2016). Furthermore, low awareness of PrEP and lack of knowledge regarding its safety and efficacy has limited its uptake (Smith, Mendoza et al., 2016; Eaton, Driffin, Bauermeister, Smith & Conway-Washington. 2015; Krakower et al., 2012; Mimiaga, Case, Johnson, Safren & Mayer. 1999; Liu et al., 2008; Walters, Reilly, Neaigus & Braunstein., 2017).
Computer-based training is an innovative and relatively inexpensive method that has been used effectively to teach targeted populations about the use of contraception (Reis & Tymchyshyn, 1992) and HIV risk behaviours (Marsch et al., 2011), and could be used to promote awareness of PrEP. Computer-based training allows for measurement and reinforcement of measurable overt responses that could be critical to learning (Silverman, Lindsley & Porter, 1990); feedback for responding, which improves learning and retention of information (Epstein et al., 2002); an efficient way to teach skills to mastery, which can improve learning (Kulik, Kulik & Bangert-Drowns, 1990); and the efficient delivery of financial incentives contingent on responding. Financial incentives appear critical to promoting high rates of responding in training and progress through the training programs for some populations (Koffarnus, DeFulio, Sigurdsson & Silverman, 2013).
This study involved the development of a novel, computer-based training program to teach adults at risk for HIV infection about PrEP. The first objective was to assess knowledge of PrEP in HIV-negative drug users who were at high risk for HIV because of their risky drug use and sexual behaviours. A rigorous, repeated-measures design was used to evaluate the effectiveness of the course on overall learning and performance across different course content areas. This course was created and delivered using our custom and novel computer-based training authoring and course presentation system called ATTAIN. ATTAIN allows instructional designers to develop courses without the need for computer programming skills. It allows for the presentation of material with audio, visual, and video stimuli. It allows for the presentation of multiple-choice and fill-in-the-blank questions, immediate feedback for responding to those questions, random and repeated presentation of questions, continued presentation of questions until the learner meets criteria based on speed and accuracy of responding, and seamless integration of a system for delivering financial incentives for performance designed to motivate learner engagement and progress through training. Many of these features have been used with considerable effectiveness to teach use of the computer keyboard and numeric keypad (Koffarnus, DeFulio, Sigurdsson & Silverman, 2013).
METHODS
Participants
Participants in the study were HIV-negative drug users who were enrolled in methadone treatment and were at high risk for HIV because of their risky drug use and sexual behaviours. Participants (N=11) were enrolled in a randomized controlled clinical trial between May 2016 and November 2017. The trial evaluated the effectiveness of abstinence-contingent wage supplements in a therapeutic workplace in maintaining abstinence from opiates and cocaine and promoting employment. To be eligible for that trial, applicants had to be: a) ≥18 yrs old; b) unemployed; c) provide an opioid-positive (methadone, buprenorphine, or morphine) urine sample at intake; d) be in methadone or buprenorphine treatment or meet DSM-IV criteria for heroin dependence; and e) express interest in obtaining competitive employment. Participants also had to provide a cocaine positive urine sample at intake, however this criterion was eliminated in March 2016 because it was deemed no longer necessary to achieve the main goals of the trial. All participants, with the exception of P1, were recruited and consented after this change. Applicants were excluded if they reported current suicidal/homicidal ideation or had a severe psychiatric disorder. Table I shows demographic characteristics of participants based on assessments conducted at intake to the study. The Johns Hopkins Medicine Institutional Review Board approved the study and all participants provided written informed consent.
Table I.
Participant Characteristicsa
| P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | Group | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female (1=yes; 0=no) | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 36% |
| Age, years | 48 | 27 | 47 | 50 | 67 | 47 | 50 | 39 | 45 | 40 | 52 | 47 (10)b |
| Black (1=yes; 0=no) | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 45% |
| Education (years) | 11 | 12 | 13 | 10 | 16 | 12 | 12 | 11 | 11 | 14 | 12 | 12 (2)b |
| Cocaine use past 30 days (days) | 20 | 15 | 2 | 13 | 0 | 7 | 30 | 30 | 20 | 5 | 0 | 13 (11)b |
| Married (1=yes; 0=no) | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 18% |
| Felony convictions, lifetime (#) | 3 | 0 | 17 | 22 | 10 | 5 | 10 | 1 | 8 | 2 | 0 | 7 (7)b |
| Drug expense, past 30 days ($) | 1000 | 500 | 300 | 500 | 120 | 300 | 1200 | 600 | 300 | 100 | 50 | 452 (368)b |
Demographic information obtained from Addiction Severity Index Lite (ASI) acquired at intake into the main study.
Mean (SD)
Setting
Participants were enrolled in the therapeutic workplace to establish job skills, initiate drug abstinence, and obtain employment. The therapeutic workplace is located at the Center for Learning and Health in the Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine in Baltimore, Maryland. The therapeutic workplace is an operant intervention that simultaneously targets both unemployment and drug use. The therapeutic workplace arranges high-magnitude reinforcement to promote drug abstinence, engagement in job-skills training, and employment. A number of clinical trials have demonstrated the effectiveness of the therapeutic workplace to initiate and maintain drug abstinence while delivering skills training to socioeconomically disadvantaged individuals to prepare them for employment (Silverman, DeFulio & Sigurdsson, 2012).
The therapeutic workplace is outlined in detail previously (Silverman et al., 2005; Silverman et al., 2007). Briefly, the intervention used in this study consisted of two phases through which participants progressed sequentially. In Phase 1, participants were invited to attend the therapeutic workplace every weekday for four hours each day during which they could engage in training programs to establish basic academic and job skills. In Phase 2, participants sought employment in the community. Participants provided urine samples routinely throughout both phases. To promote and maintain drug abstinence, participants were required to provide drug-free urine samples to maintain maximum pay, which was provided each day on a personalized reloadable credit card (Silverman, Holtyn & Morrison, 2016). Participants were engaged in this study during Phase 1.
Assessment of Eligibility for PrEP
All participants completed the PrEP Eligibility Assessment, an assessment tool created for this study to determine eligibility for treatment with PrEP. The 18-item assessment was based on the CDC guidelines and recommendations to clinicians about who should consider PrEP, as described previously (CDC, 2014). The items in the PrEP Eligibility Assessment consisted of statements about risky sexual and drug injection behaviors. Participants responded by selecting “Yes” or “No” to each statement. The education program was offered to individuals who were appropriate for PrEP based on CDC guidelines and to individuals who reported engaging in a number of behaviours that may make them at risk for HIV, but were not eligible for PrEP based on the CDC guidelines.
Education Program
Participants were invited to complete a computer-based self-paced HIV prevention education program that was designed to teach them about PrEP. Content was based on information provided by the CDC (CDC, 2014) and included an introduction to HIV, signs and symptoms of HIV, routes of transmission, an introduction to PrEP, HIV risky behaviours, who should use PrEP, and PrEP protection levels. The education program was delivered in ATTAIN, a custom computer-based training and presentation system. One of the authors of this study (Silverman) designed ATTAIN and comissioned a softward developer to create ATTAIN. Access to ATTAIN can be obtained by contacting the corresponding author. The education program was divided into three courses containing a total of 33 modules that participants were required to take and master sequentially. The average Flesch Kincaid Reading Level across education program modules was grade 6.6. To eliminate complications due to reading difficulties, audio of the text played when the text appeared, and participants could replay text audio.
Each module (except the last) included a Presentation Unit and a Mastery Unit. Within each Presentation Unit, material was presented in logical order in presentation screens that displayed the information in text, graphics, and sound. Presentation screens were full screens that trainees read or viewed, but which posed no questions requiring overt responses by the learner. These presentation screens were used to introduce learners to new material. Multiple-choice questions (explained below) were interspersed in between presentation screens. Participants had unlimited time to complete each run of a Presentation Unit and had to respond correctly to all questions in the Presentation Units to pass the module (100% correct). If a participant did not meet the accuracy criterion (i.e., 100% correct), the participant was required to complete the Presentaion Unit again. If the participant responded correctly to all questions in the Presentation Units, the participant progressed to the Mastery Unit of that module.
In each Mastery Unit, there were no presentation screens. Rather, multiple-choice questions about the module content were presented in random order during two-minute timings (speed trials) and participants were required to respond correctly on at least 18 questions with no errors (i.e., 9 correct per minute) to pass the Mastery Unit. The participant continued to practice answering the questions in 2-miniute timings until they met the speed and accuracy criteria set for that unit. If the participant did not meet the speed and accuracy criteria for a Mastery Unit, the participant was required to answer randomly-presented questions in that Mastery Unit again in another 2-minute timing. Once a participant met the speed and accuracy criteria for a Mastery Unit, the participant then progressed to the next module.
As described, participants responded to multiple-choice questions across Presentation and Mastery Units. Questions covered all content from the program, for example; “What is the abbreviation for human immunodeficiency virus?”, “What is the first stage of HIV?”, “Who should take PrEP?”, and a various questions reporting to the degree of risk associated with different sexual behaviours. On each multiple-choice question, participants were presented with a question in the upper part of the screen and two or more answer choices contained within individual choice boxes on the bottom part of the screen. All choice boxes for a given question were of equal size and were presented horizontally across the screen. Text representing each choice was centered in the middle of each box. There was only one correct response per question; therefore, one of the choices in the choice boxes was correct and the remaining choices were incorrect. The location of correct and incorrect choices (e.g., left, middle, or right on trials that included three choices) were presented in random locations across trials. Participants responded by clicking the mouse while the pointer was on a particular choice box. Each response on a multiple-choice question was followed by feedback. When the participant clicked on the correct choice box, the outline of the selected choice box turned green and the word “Correct” appeared on the screen for 1 second. When the participant clicked on the incorrect choice box, the outline of the selected choice box turned red, the word “Incorrect” appeared on the screen for 1 second, and the participant was required to answer the question again.
At the beginning of each Presentation and Mastery Unit, an information screen was displayed stating the minimum number of correct responses required, the maximum number of incorrect responses allowed to pass, and the amount in financial incentives awarded for correct responses. Participants could earn $0.02 for each correct response. Participants were not financially penalised for incorrect responses. Upon completion of a Presentation or Mastery Unit, the total amount earned was displayed on the computer and was automatically added to the participant’s account.
Testing
A 112-item test was created to assess performance prior to and following training. All items on the test were multiple-choice questions. To evaluate the generalization of the material participants had learned, 56 questions were original and taken directly from the education course while the other 56 were novel questions. Novel questions tested the same concepts but differed from original questions in their format and how they were presented. For example, an original question was,” HIV can be controlled without medication” (answer choices: True, False). A novel question testing the same concept in the test was, “You can control HIV with medication” (answer choices: True, False). Participants were only provided with feedback about their overall performance on the test (number of correct/ incorrect responses and amount earned in US dollars) following completion of each test and not following each response as in the rest of the education program. The 112 questions were presented once each and there were no criteria for passing the test.
Experimental Design
A multiple-probe design was used in this study (Horner & Baer, 1978). The overall education program was divided into three courses consisting of several modules each (7 modules for Course 1, 15 modules for Course 2, and 11 modules for Course 3). Each participant completed the 112-item test described above four times (Test 1, Test 2, Test 3, and Test 4). Participants completed the test prior to beginning the education program, and then again after the participant completed each of the three courses. Participants completed Test 1 prior to taking Course 1, Test 2 after taking Course 1 and prior to taking Course 2, Test 3 after taking Course 2 and prior to taking Course 3, and Test 4 after taking Course 3.
To evaluate the effectiveness of each course, the 112-item test described above was also divided into three parts consisting of test items that corresponded to the material covered in the three Courses. We expected that performance on the test items related to each Course would increase in the testing that followed completion of the relevant course, and that performance on the test items related to the other courses would only improve following their training and not before.
Statistical Analysis
Performance data are presented for individual participants and collapsed across all participants. The mean performance data (percentage of responses correct on the three parts of the 112-item test) were analyzed to determine whether performance on the test items that corresponded to a particular course increased only after participants completed training on that course. Comparisons were made within each set of the test items taught in each of the three courses. Three separate repeated-measures analysis of variance (ANOVA): one for performance on items related to Course 1, one for performance on items related to Course 2, and one for performance on items related to Course 3, tested whether there were any statistically significant differences in course-specific performance during Test 1, Test 2, Test 3, and Test 4. Mauchley’s test confirmed that the sphericity assumption was not violated for each repeated-measures ANOVA (all ps > .05). Tukey’s honest significant difference (HSD) post-hoc tests were used to identify when statistically significant performance improvements (i.e., during which Test), if any, occurred. Values of p ≤ .05 were considered statistically significant.
RESULTS
PrEP Eligibility
Table II shows which risk behaviors each participant engaged in and why some of the participants were appropriate for PrEP based on CDC guidelines. As shown in Table II , four participants were injection drug users who qualified for PrEP due to risky needle sharing, while one participant was a heterosexually active man who qualified for PrEP due to risky sexual behaviors. However, all participants were offered, and agreed, to complete the PrEP education course.
Table II.
PrEP Eligibility Based on Center for Disease Control Guidelines
| PrEP Eligibility | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | Group (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female? | Yes | No | Yes | No | No | No | No | Yes | No | No | Yes | 36% |
| Man who has sex with men? | No | Yes | No | No | No | No | No | No | No | No | No | 9% |
| Not in a monogamous partnership with recently tested HIV-negative partner | Yes | No | No | No | Yes | No | No | No | No | Yes | Yes | 36% |
| Any male sex partners in past 6 months | Yes | Yes | No | No | No | No | No | No | No | No | No | 18% |
| AND at least one of the following | ||||||||||||
| Any anal sex without condoms in past 6 months | No | No | No | Yes | No | Yes | No | No | Yes | No | No | 27% |
| Any STI diagnosed or reported in past 6 months | Yes | No | Yes | No | No | No | No | No | No | No | No | 18% |
| In ongoing sexual relationship with an HIV-positive male partner | No | No | No | No | No | No | No | No | No | No | No | 0% |
| MSM in need of PrEP? | No | No | No | No | No | No | No | No | No | No | No | 0% |
| Heterosexually active man or woman? | Yes | Yes | No | Yes | No | Yes | No | No | Yes | Yes | No | 55% |
| Any sex with opposite sex partners in past 6 months | Yes | Yes | No | Yes | No | Yes | No | No | Yes | Yes | No | 55% |
| Not in a monogamous partnership with recently tested HIV-negative partner | Yes | No | No | No | Yes | No | No | No | No | Yes | Yes | 36% |
| AND at least one of the following | ||||||||||||
| A man who has sex with both women and men? | No | Yes | No | No | No | No | No | No | No | No | No | 9% |
| Infrequently uses condoms with partners of unknown HIV status | No | Yes | No | No | No | No | No | No | No | No | No | 9% |
| Heterosexual in need of PrEP? | No | Yes | No | No | No | No | No | No | No | No | No | 9% |
| Injection drug user? | Yes | No | Yes | No | Yes | Yes | No | No | No | No | No | 36% |
| Injected non-prescribed drugs in past 6 months | Yes | No | Yes | No | Yes | Yes | No | No | No | No | No | 36% |
| AND at least one of the following | ||||||||||||
| Shared injection or drug preparation equipment in past 6 months | Yes | No | Yes | No | Yes | Yes | No | No | No | No | No | 36% |
| In methadone, buprenorphine, or suboxone treatment in past 6 months | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 100% |
| Injection drug user in need of PrEP? | Yes | No | Yes | No | Yes | Yes | No | No | No | No | No | 36% |
| Eligible for PrEP based on CDC guidelines? | Yes | Yes | Yes | No | Yes | Yes | No | No | No | No | No | 45% |
Training Time
Table III shows how long participants took to complete the Presentation Units, the Mastery Units and the total amount of time in training. On average, participants took a little over 5 hours to complete the education program, however there was considerable variability across participants. One participant (P7) took as little as 1.75 hours to complete all courses, whereas two participants (P4 and P9) took over 11 hours. Most of the time was spent in working on the Mastery Units (M=4.38 hours, SD=3.3 hours), probably because participants were required to achieve high levels of speed and accuracy on those units and had to take those units repeatedly until they achieved the required levels of speed and accuracy. Earnings, which were contingent on performance, varied across participants and averaged at $60.
Table III.
Training Time across Presentation and Mastery Modules and for All Participants
| Training Timea | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | Group | |
| Presentation Time (hrs) | 0.8 | 1.1 | 0.8 | 1.9 | 1.0 | 0.7 | 0.4 | 0.6 | 1.4 | 0.4 | 1.3 | 0.9 (0.5)b |
| Mastery Time (hrs) | 1.9 | 1.5 | 2.3 | 9.7 | 4.4 | 4.8 | 1.4 | 1.7 | 10.2 | 2.8 | 7.6 | 4.4 (3.3)b |
| Total Time (hrs) | 2.7 | 2.6 | 3.1 | 11.6 | 5.4 | 5.5 | 1.8 | 2.3 | 11.6 | 3.1 | 8.9 | 5.3 (3.7)b |
Time spent training on presentation and mastery modules for each individual participant
Group average and standard deviation for time spent training on presentation and mastery modules.
Evaluation of Course Effectiveness
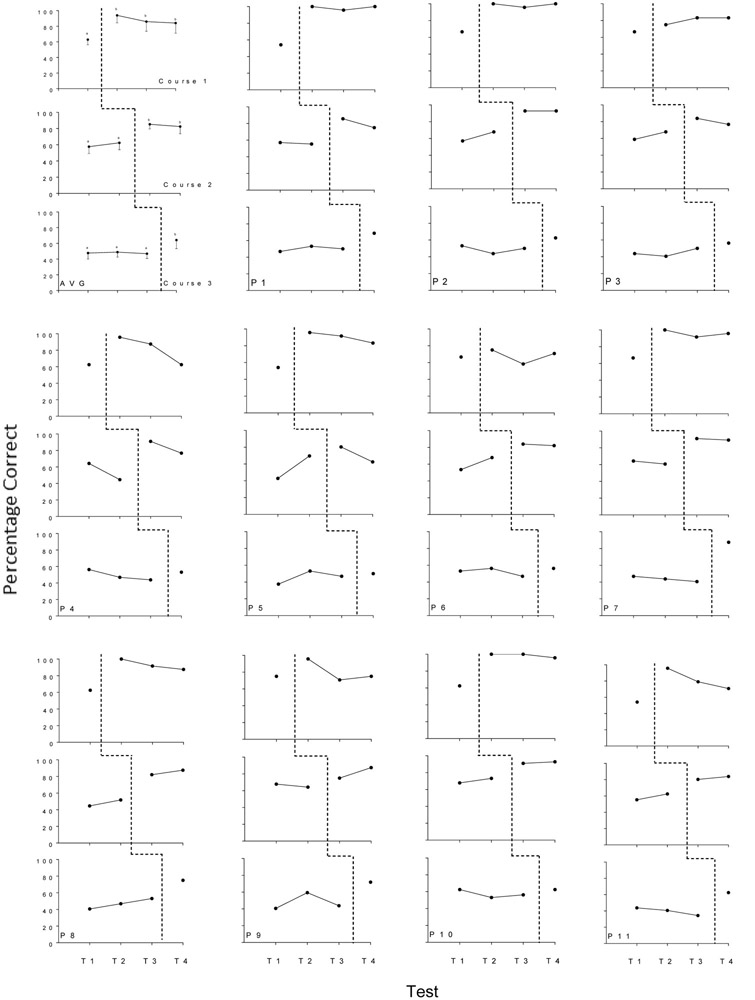
Figure 1 shows performance on Tests 1, 2, 3 and 4 averaged for all participants and for each of the participants. Within each panel, performance on each test is shown separately for the questions associated with each of the three courses (Course 1, Course 2, and Course 3 in the top, middle, and bottom figure of each panel). The dashed lines show when participants completed Courses 1, 2, and 3. The upper left panel of Figure 1 shows the performance data averaged across all 11 participants. Statistical analyses of those data revealed that Course 1 scores (top graph) from Test 1 (prior to training on Course 1) were significantly different for Course 1 scores on Tests 2, 3 and 4 (following training on Course 1) based on a repeated measures ANOVA (F(3, 30) = 23.46, p< .001, ηP2 = 0.70 with 90% CI [0.49,0.77]) and Tukey HSD post-hoc tests (p< .001). Scores on Tests 2, 3, and 4 were not significantly different from each other. Course 2 scores (middle graph) from Test 1 and Test 2 (prior to training on Course 2) were not sigificantly different from each other, but both were significantly different from scores from Tests 3 and 4 (following training on Course 2) based on repeated measures ANOVA(F(3, 30) = 40.87, p< .001, ηP2 = 0.80 with 90% CI [0.66,0.85]) and Tukey HSD post-hoc tests (p< .001). Scores on Tests 3 and 4 were not significantly different from each other. Finally, Course 3 scores from Test 1, 2 and 3 (prior to training Course 3) were not siginficantly different from each other but each were significantly different from Course 3 scores from Test 4 (following training on Course 3) based on repeated measures ANOVA (F(3, 30) = 11.58, p< .001, ηP2 = 0.54 with 90% CI [0.27,0.64]) and Tukey HSD post-hoc tests (p< .001). Taken together, these results confirm that performance on test questions related to Courses 1, 2, and 3 was low and stable prior to completing each course, and increased immediately and significantly after participants completed each course. Individual participant performance data in Figure 1 show that performance by individual participants on test questions related to Courses 1, 2 and 3 increased only after participants completed training on the respective courses, although there was some variability in that pattern.
Fig 1.
Group average and individual performance on Tests 1, 2, 3 and 4. Each test included the same 112 questions, divided into three parts that corresponded to questions in Courses 1 (top figure in each panel), Course 2 (middle figure in each panel) and Course 3 (bottom figure in each panel). Group averages on the tests are shown in the upper left panel (AVG). The remaining panels show data for individual participants. Participant numbers are shown in the bottom figure of each panel (P1-P11). In the group graph, within each course (top, middle and bottom graph), points that do not share a letter in common are significantly different.
Across all tests, performance was similar on the novel and explicitly taught questions. For each individual participant, percentage correct for the 56 novel and 56 original questions were calculated separately and compared using paired-samples Tukey HSD tests. Test 1 novel performance (M=60.4%, SD=9.6%) was signifiantly higher than original performance (M=51.5%, SD=6.9%), t=2.79, p=.01. Test 2 novel performance (M=68.2%, SD= 5.3%) did not differ from original performance (M=62.3%, SD=5.3%), t=4.66, p = .21. Test 3 novel performance (M=75.2%, SD=7.8%) did not differ from original performance (M=73.7%, SD=5.3%), t=0.72, p=.99. Finally, Test 4 novel performance (M=77.8%, SD=10.1%) did not differ from original performance (M=76.0%, SD=9.3%), t=0.79, p = .99.
HIV and PrEP Knowledge
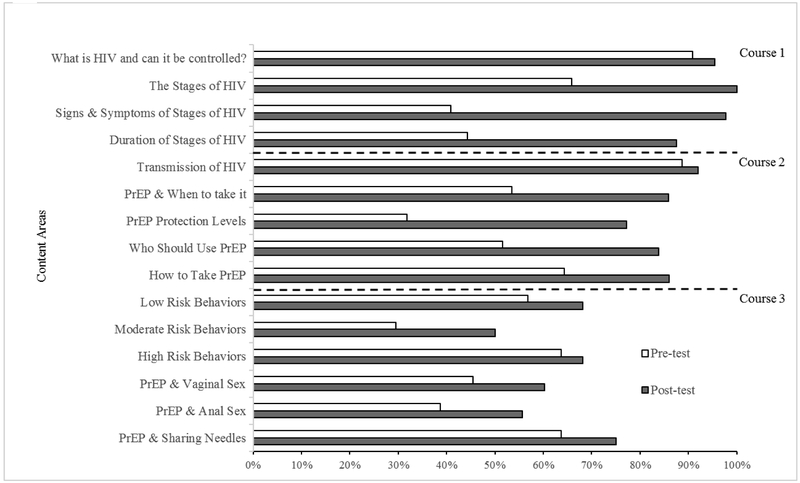
Figure 2 shows what participants knew about different content areas before and after they completed Courses 1, 2 and 3. Specifically, pretest scores are based on a percentage correct average on test 1, prior to completing any training. Averagered percentage correct scores from tests admimistered immediately after taking each Course is termed posttest. Therefore, test 1 and test 2 percentage correct scores for all participants were used to compare knowledge across the four content areas prior to and after training in Course 1. Average percentage correct test scores for all participants from test 1 and test 3 were compared to show changes in knowledge across the five content areas in Course 2, and finally average test scores for all participants from test 1 and test 4 were compared to show changes in knowledge across the six content areas in Course 3. Although there was variability in participant knowledge across content areas, performance on the respective posttests increased from the pretests across all content areas. What’s evident, is that knowledge of Signs & Symptoms of HIV was considerably low initially (M=41%), and only increased following learning on Course 1 (M=98%). Similar trends are also apparent across other content areas; PrEP & when to take it (Pretest M=54%, Posttest M=86%); PrEP Protection Levels (Pretest M=32%, Posttest M=77%); Who should take PrEP (Pretest M=52%, Posttest 84%).
Fig 2.
Changes in HIV prevention and PrEP knowledge across content areas of the education course from pretest (open bars) to posttest (shaded bars). Data are based on performance on the 112 item test. Data are grouped by the areas covered by the questions. Pretest scores are based on a percentage correct average on test 1, prior to completing any training. Averagered percentage correct scores from tests admimistered immediately after taking each course is termed posttest. Therefore, test 1 and test 2 percentage correct scores for all participants were used to compare knowledge across the four content areas prior to and after training in Course 1. Average percentage correct test scores for all participants from test 1 and test 3 were compared to show changes in knowledge across the five content areas in Course 2, and finally average test scores for all participants from test 1 and test 4 were compared to show changes in knowledge across the six content areas in Course 3.
DISCUSSION
HIV infections among drug users are typically transmitted by risky injection practices and sexual behaviours. Some drug users have been identified by the CDC as being at high risk of contracting HIV and in need of a high impact HIV prevention intervention, including PrEP (CDC, 2014). However, many people who are at risk for HIV are not aware of the availability and potential utility of PrEP. This study was designed to assess the effectiveness of a computer program aimed at promoting HIV awareness and teaching HIV prevention methods including the use of PrEP. The study showed that the essential components of HIV risk reduction techniques, including awareness and the potential utility of PrEP, can be taught effectively through a computerised education course.
Performance on the initial test (Test 1), which was conducted prior to any training, shows that participants had relatively limited knowledge of HIV and the use of PrEP medication in HIV prevention. Although participants were aware of HIV and what the abbreviation stands for, as shown in Figure 2, participants had limited knowledge of the following topics: signs and symptoms of HIV, the progression of HIV, PrEP as a HIV preventative measure and the protection offered by PrEP, and the risk associated with sexual behaviours. This lack of PrEP awareness is consistent across literature (Smith et al., 2015). The computer-based training course was effective in teaching participants about HIV and the use of PrEP in HIV prevention.
Following completion of each part of the overall course (i.e., Course 1, Course 2, Course 3), performance on the test items covered in each course increased immediately after participants completed each course and not before. However, this increase in performance was not maintained by all participants. For example, participants P4, P5, P6, P9 and P11 had declines in performance course-specific items over time (see Figure 1). These participants also spent longer than average completing the program. In order to confirm which factors are critical to ensuring the retention of taught material, future research must be conducted. Performance across novel and explicitly trained questions was measured to determine the transfer of learning from the education course to novel questions. There were no substantial differences across performance on novel and explicitly trained questions after participants completed the course, suggesting successful generalisation of learned material.
The computer-based training program was delivered using ATTAIN and included many features that may have contributed to the effectiveness of the training. Specifically, participants were required to answer questions that were presented repeatedly in random order, received immediate feedback for each response, received financial incentives for correct responses, and were required to continue in training on a particular unit until they achieved a specified level of speed and accuracy. We cannot know from this study if any single feature was necessary or sufficient in producing the training outcomes. Although there is good evidence that financial incentives for correct responses are both effective and attractive to participants (Silverman et al., 2005), future research will have to be conducted to determine which of these features are critical to the training outcomes.
Delivering HIV prevention education through computer-based training may offer an inexpensive and convenient approach to promoting awareness and knowledge of HIV prevention approaches, including the use of PrEP. Computerized methods may be acceptable and appealing to individuals who feel embarrassed or intimidated discussing issues of a personal nature, such as risky sexual behaviors, with professionals. A sense of anonymity may be more encouraging for many, making them more inclined to participate. Based on feedback from participants, the course was well received and valuable to participants. Although this study was conducted within a clinical setting with few participants, the course has the potential to be accessed online, therefore reaching a widespread audience. The cost benefits to both participants and staff could make this method an attractive approach, and reduce implementation costs including staff training and supervision.
This study did not determine if increased knowledge and awareness of HIV and HIV prevention approaches, including the use of PrEP, increased HIV prevention behaviors. However, now that we have experimentally shown that the training program can increase PrEP knowledge, future research could determine if computer-based training of the type provided in this study actually increases the use of PrEP and other HIV prevention behaviors.
This study demonstrated the feasibility and effectiveness of delivering HIV awareness and prevention education via a computer-based program. Integrating this program with mobile technology could provide access to participants in geographic areas who could benefit from PrEP education. The use of computer-based training could be an important element in a larger initiative that can reduce the transmission of HIV, and increase awareness about PrEP among at-risk individuals and health care professionals. Further implementation of this computer-based training program with a larger sample size would be worthwhile.
ACKNOWLEDGEMENTS
The preparation of this publication was supported by the National Institute on Drug Abuse and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Numbers R01DA037314, R01AI117065 and T32DA07209. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- Centers for Disease Control and Prevention. (2014). Preexposure prophylaxis for the prevention of HIV infection in the United States-2014: a clinical practice guideline. Atlanta: Centers for Disease Control and Prevention, 67. [Google Scholar]
- Centers for Disease Control and Prevention. (2016). CDC fact sheet: New HIV infections in the United States. Atlanta: Available from: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508 [Google Scholar]
- Eaton LA, Driffin DD, Bauermeister J, Smith H, & Conway-Washington C (2015). Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS patient care and STDs, 29(8), 423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein ML, Lazarus AD, Calvano TB, Matthews KA, Hendel RA, Epstein BB, & Brosvic GM (2002). Immediate feedback assessment technique promotes learning and corrects inaccurate first responses. The Psychological Record, 52(2), 187–201. [Google Scholar]
- Horner RD, & Baer DM (1978). Multiple‐probe technique: a variation of the multiple baseline. Journal of applied behavior analysis, 11(1), 189–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, DeFulio A, Sigurdsson SO, & Silverman K (2013). PERFORMANCE PAY IMPROVES ENGAGEMENT, PROGRESS, AND SATISFACTION IN COMPUTER‐BASED JOB SKILLS TRAINING OF LOW‐INCOME ADULTS. Journal of applied behavior analysis, 46(2), 395–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakower DS, Mimiaga MJ, Rosenberger JG, Novak DS, Mitty JA, White JM, & Mayer KH (2012). Limited awareness and low immediate uptake of pre-exposure prophylaxis among men who have sex with men using an internet social networking site. PloS one, 7(3), e33119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulik CLC, Kulik JA, & Bangert-Drowns RL (1990). Effectiveness of mastery learning programs: A meta-analysis. Review of educational research, 60(2), 265–299. [Google Scholar]
- Liu AY, Kittredge PV, Vittinghoff E, Raymond HF, Ahrens K, Matheson T, Hecht J, Klausner JD, & Buchbinder SP (2008). Limited knowledge and use of HIV post-and pre-exposure prophylaxis among gay and bisexual men. JAIDS Journal of Acquired Immune Deficiency Syndromes, 47(2), 241–247. [PubMed] [Google Scholar]
- Marsch LA, Grabinski MJ, Bickel WK, Desrosiers A, Guarino H, Muehlbach B, Solhkhah R, Taufique S, & Acosta M (2011). Computer-assisted HIV prevention for youth with substance use disorders. Substance use & misuse, 46(1), 46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Case P, Johnson CV, Safren SA, & Mayer KH (2009). Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. Journal of acquired immune deficiency syndromes (1999), 50(1), 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis J, & Tymchyshyn P (1992). A longitudinal evaluation of computer-assisted instruction on contraception for college students. Adolescence, 27(108), 803. [PubMed] [Google Scholar]
- Silverman K, DeFulio A, & Sigurdsson SO (2012). Maintenance of reinforcement to address the chronic nature of drug addiction. Preventive medicine, 55, S46–S53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Holtyn AF, & Morrison R (2016). The therapeutic utility of employment in treating drug addiction: Science to application. Translational issues in psychological science, 2(2), 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Lindsley OR, & Porter KL (1990). Overt responding in computer-based training. Current Psychology, 9(4), 373–384. [Google Scholar]
- Silverman K, Wong CJ, Grabinski MJ, Hampton J, Sylvest CE, Dillon EM, & Wentland RD (2005). A web-based therapeutic workplace for the treatment of drug addiction and chronic unemployment. Behavior Modification, 29(2), 417–463. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Grabinski MJ, Hampton J, Sylvest CE, Dillon EM, & Wentland RD (2005). A web-based therapeutic workplace for the treatment of drug addiction and chronic unemployment. Behavior Modification, 29(2), 417–463. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Needham M, Diemer KN, Knealing T, Crone‐Todd D, Fingerhood M, Nuzzo P, & Kolodner K (2007). A randomized trial of employment‐based reinforcement of cocaine abstinence in injection drug users. Journal of applied behavior analysis, 40(3), 387–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Mendoza MC, Stryker JE, & Rose CE (2016). PrEP awareness and attitudes in a national survey of primary care clinicians in the United States, 2009–2015. PloS one, 11(6), e0156592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Van Handel M, Wolitski RJ, Stryker JE, Hall HI, Prejean J, Koenig LJ, & Valleroy LA (2015). Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition—United States, 2015. MMWR Morb Mortal Wkly Rep, 64(46), 1291–5. [DOI] [PubMed] [Google Scholar]
- Walters SM, Reilly KH, Neaigus A, & Braunstein S (2017). Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm reduction journal, 14(1), 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. HIV/AIDS fact sheet (cited October 2017). Available from: http://www.who.int/mediacentre/factsheets/fs360/en/