Abstract
Chicken liver has been implicated in several reported U.S. illness outbreaks, probably caused by inadequate cooking and pathogen contamination. To identify commonalities among these outbreaks that could represent targets for prevention, we describe chicken liver–associated U.S. outbreaks during 2000–2016 reported to the Food Safety and Inspection Service, to the Centers for Disease Control and Prevention, and in published literature. We identified 28 outbreaks (23 [82.1%] were campylobacteriosis only, 3 [10.7%] were salmonellosis only, and 2 [7.1%] were caused by both pathogens), with 18 (64.3%) occurring during 2014–2016. Common outbreak features included blended chicken liver dishes (e.g., pâté; 24 [85.7%]), inadequate cooking (26 [92.8%]), and preparation in foodservice settings (e.g., sit-down restaurants; 25 [89.3%]). The increasing frequency of reported outbreaks highlights chicken liver as an important food safety problem. Public health partners should collaborate on prevention measures, including education on proper foodservice preparation of blended chicken liver dishes.
Keywords: : liver, chicken, infectious disease outbreaks, foodborne diseases, Campylobacter, Salmonella, prevention and control, cooking
Introduction
Campylobacter and Salmonella are the estimated leading causes of bacterial foodborne infections in the United States (Scallan et al., 2011). Infections with these pathogens are rarely fatal but can be associated with severe gastrointestinal symptoms, sometimes requiring hospitalization, and can lead to postinfectious complications, including reactive arthritis, irritable bowel syndrome, and Guillain–Barré syndrome (Nyati and Nyati, 2013; Scallan et al., 2015). Exposure to chicken and other poultry products has been identified as both a common source of campylobacteriosis and salmonellosis outbreaks (Chai et al., 2017) and as a risk factor for sporadic infection with these pathogens (Friedman et al., 2004; Kassenborg et al., 2004; Kimura et al., 2004; Fullerton et al., 2007).
Chicken liver has been recognized as an important vehicle for foodborne infections (Geissler et al., 2017). Like other chicken parts, chicken liver is regulated by the Food Safety and Inspection Service (FSIS). Methods of preparing chicken liver for consumption are numerous and include frying and blending (e.g., for pâté). Recent outbreaks of campylobacteriosis and salmonellosis in the United States have been linked to chicken liver (Tompkins et al., 2013; Hanson et al., 2014; Scott et al., 2015; Glashower et al., 2017). Such outbreaks have also occurred in other countries; reviews of chicken liver–associated outbreaks in the United Kingdom (Little et al., 2010), Australia (Merritt et al., 2011), and New Zealand (NZMPI, 2007, 2013) have been published. These outbreaks may, in large part, be explained by the interplay of two factors: inadequate cooking and pathogen contamination.
FSIS and the Food and Drug Administration (FDA) recommend cooking poultry products to an internal temperature of 165°F (FDA, 2013; FSIS, 2015). However, some food writers recommend using livers that have not been fully cooked (e.g., “still rosy pink inside”) when preparing chicken liver dishes (The Dallas Morning News, 2013; Los Angeles Times, 2015). Recipes that call for the use of partially cooked chicken liver are readily available (The New York Times Company, 2018; Food Network, 2018).
Cooking to recommended internal temperatures is especially important for foods known to contain pathogens. Like other chicken products, chicken liver has been found to be contaminated with Campylobacter (Cox et al., 2009; Noormohamed and Fakhr, 2012; Strachan et al., 2012) and Salmonella (Zdragas et al., 2012; Abd-Elghany et al., 2015). Of particular concern is the evidence that pathogens can exist in internal chicken liver tissues. Among several studies, Campylobacter was recovered from the internal tissues of 10–90% of chicken livers tested after the external surface had been sterilized (Barot et al., 1983; Boukraa et al., 1991; Baumgartner et al., 1995; Whyte et al., 2006; Firlieyanti et al., 2016). In addition, in studies involving specific pathogen–free chickens in experimental conditions, livers tested after oral inoculation yielded Campylobacter (Sanyal et al., 1984; Knudsen et al., 2006; Chaloner et al., 2014) and Salmonella (Borsoi et al., 2009; He et al., 2010; Gast et al., 2013). Pathogens are thought to spread from the gastrointestinal tract to the liver through the biliary, lymphatic, or vascular systems, although the exact route is unclear (Boukraa et al., 1991; Whyte et al., 2006; He et al., 2010; Chaloner et al., 2014; Firlieyanti et al., 2016).
Consumption of inadequately cooked chicken livers contaminated with pathogens can lead to illnesses and outbreaks. To better understand the characteristics of such outbreaks to identify opportunities for prevention, we reviewed and described chicken liver–associated outbreaks in the United States during 2000–2016.
Materials and Methods
We reviewed outbreaks reported to FSIS and the Foodborne Disease Outbreak Surveillance System (FDOSS) of the Centers for Disease Control and Prevention (CDC, 2017a) and in published literature to identify outbreaks of illness associated with chicken liver during 2000–2016 in the United States. An outbreak was defined as the occurrence of two or more cases of similar illness resulting from ingestion of a common food. We included an outbreak in the study if: (1) chicken liver or a food containing chicken liver (e.g., chicken liver pâté) was implicated; and (2) at least one of the case-patients in the outbreak had a laboratory-confirmed foodborne infection. We described outbreaks by several characteristics, including illness-onset dates; etiologies; case-patient demographics; reported illnesses, hospitalizations, and deaths; implicated food vehicles; food-preparation settings; and contributing factors. For outbreaks with incomplete information about certain characteristics, we attempted to obtain the information from relevant state and local health departments. We compared median numbers of illnesses per outbreak using the Wilcoxon rank-sum test in SAS version 9.4 (SAS Institute, Cary, NC).
Results
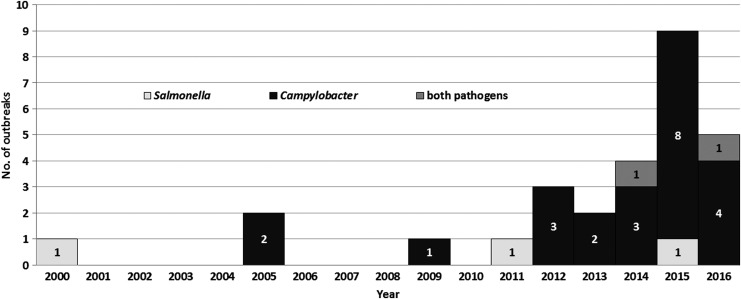
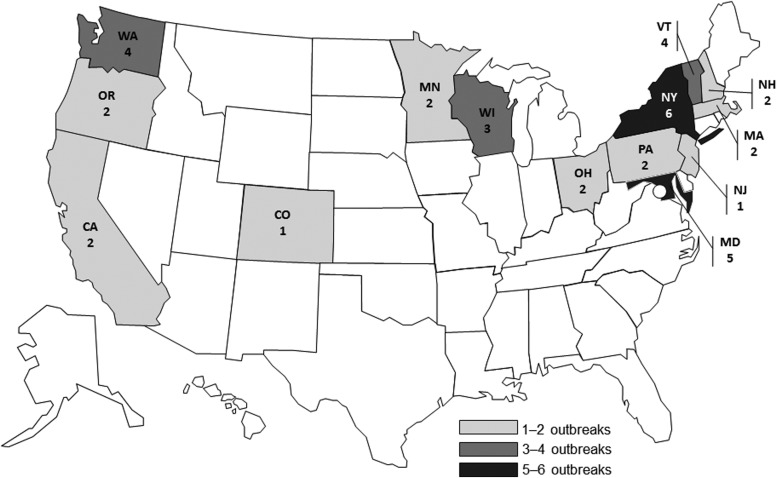
During 2000–2016, a total of 28 reported outbreaks associated with chicken liver were identified (Table 1). The frequency of identified outbreaks increased throughout the study period, particularly during its last few years (Fig. 1); for example, there were 4 (14.3%) outbreaks during 2000–2010, 6 (21.4%) during 2011–2013, and 18 (64.3%) during 2014–2016. The outbreaks were clustered geographically, by state of case-patient residence, in northeastern, western, and upper midwestern states (Fig. 2).
Table 1.
Characteristics of Chicken Liver–Associated Campylobacteriosis and Salmonellosis Outbreaks (n = 28), United States, 2000–2016
| Sequential No. | Illness onset date range | Etiology(ies) | State(s) with illness | No. of illnessesa | No. of hospitalizationsb | Implicated chicken liver product(s) | Food preparation setting(s) | Contributing factor(s)c | Data source(s) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | August 2000 | S. Heidelberg | CA | 4 | 1 | Chicken liver (specific dish/preparation method unknown) | Private residence | None identified | FDOSS |
| 2 | August 2005 | Campylobacter (NOS) | WA | 9 | 0 | Chicken liver pâté | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 3 | October 2005 | Campylobacter jejuni | WI | 13 | 2 | Chicken liver pâté | Religious facility | Inadequate cooking; food handler was positive for C. jejuni | FDOSS |
| 4 | August 2009 | C. jejuni | CA | 6 | 0 | Whole chicken livers | Restaurant (sit-down) | Inadequate cooking/not cooking | FDOSS |
| 5 | April to November 2011 | S. Heidelberg | NY, NJ, PA, MD, OH, MN | 190 | 30 | Whole chicken livers; chicken liver spread | Grocery store; school; private residence; assisted living facility | Inadequate cooking; potentially misleading labeling and product appearanced | FSIS; FDOSS; published report 1e |
| 6 | April to May 2012 | C. jejuni and Campylobacter coli | MD, NH | 11 | 2 | Chicken liver pâté | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 7 | April to September 2012 | C. jejuni | VT, NH, NY | 6 | 2 | Chicken liver mousse | Restaurant (sit-down); private residence | Inadequate cooking; occupational exposure at poultry slaughter establishment | FSIS; FDOSS; published report 2f |
| 8 | October 2012 | C. jejuni | OR | 9 | 0 | Chicken liver pâté | Private residence | Inadequate cooking | FSIS; FDOSS |
| 9 | April 2013 | C. jejuni | NY | 20 | 0 | Chicken liver spread | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 10 | December 2013 to January 2014 | C. jejuni | OR, OH, WA | 6 | 0 | Chicken liver pâté; raw, pill-sized chicken liver piecesg | Restaurant (sit-down) | Inadequate cooking | FSIS; FDOSS; published report 3h |
| 11 | May to July 2014 | C. jejuni and C. coli | MD | 4 | 0 | Chicken liver pâté | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 12 | August 2014 | C. jejuni and S. Enteritidis | MA | 5i | 0 | Chicken liver pâté | Restaurant (sit-down) | Inadequate cooking; food handler was positive for Campylobacter (NOS) | FDOSS |
| 13 | September to December 2014 | C. jejuni and C. coli | VT | 4 | 4 | Chicken liver pâté/mousse | Assisted living facility | Inadequate cooking | FDOSS; FSIS |
| 14 | December 2014 | C. jejuni | PA | 3 | 0 | Chicken liver pâté | Private residence | None identified | FDOSS |
| 15 | March to April 2015 | C. jejuni | WA | 2 | 2 | Chicken liver pâté | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 16 | April 2015 | S. Enteritidis | NY | 7 | 1 | Chicken liver butter | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 17 | May to July 2015 | C. jejuni and C. coli | MN | 9 | 0 | Chicken liver mousse | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 18 | June 2015 | C. jejuni | MD | 7 | 1 | Chicken liver mousse | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 19 | July 2015 | C. jejuni | NY | 2 | 0 | Seared chicken liver | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 20 | August 2015 | C. jejuni | MD | 2 | 0 | Whole, fried chicken livers | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 21 | October 2015 | C. jejuni and C. coli | WI | 7 | 0 | Chicken liver pâté/mousse | Restaurant (sit-down) | Inadequate cooking | FSIS |
| 22 | November 2015 | C. jejuni | VT | 3 | 0 | Chicken liver mousse | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 23 | December 2015 | Campylobacter (NOS) | CO | 4 | 0 | Chicken liver pâté | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 24 | January 2016 | C. jejuni | VT | 5 | 0 | Chicken liver mousse | Restaurant (sit-down) | Inadequate cooking | FDOSS; FSIS |
| 25 | April to May 2016 | C. coli and S. Enteritidis | WI | 9j | 0 | Chicken liver pâté | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 26 | July 2016 | C. jejuni | WA | 5 | 0 | Chicken liver mousse | Restaurant (sit-down) | Inadequate cooking; ill food handler | FSIS; published report 4k |
| 27 | August 2016 | C. jejuni | NY | 4 | 0 | Chicken liver mousse | Restaurant (sit-down) | Inadequate cooking | FDOSS |
| 28 | September 2016 | C. jejuni | MA | 5 | 1 | Chicken liver pâté | Banquet facility (for senior citizen housing) | Inadequate cooking | FDOSS |
Includes confirmed and probable/suspect case-patients.
Hospitalization status was not reported for each case-patient. No deaths associated with these outbreaks were reported.
Not all potential contributing factors were known or listed.
Product was labeled “broiled” and appeared, but was not, fully cooked.
Published report 1: Hanson et al. (2014).
Published report 2: Tompkins et al. (2013).
One case-patient in this outbreak consumed raw, pill-sized pieces of chicken liver that had been prescribed by a naturopathic physician.
Published report 3: Scott et al. (2015).
In this outbreak, C. jejuni, S. enterica serovar Enteritidis, or both, respectively, were isolated from two, one, and two case-patients.
In this outbreak, both C. coli and S. Enteritidis were isolated from each of the four confirmed case-patients (the other five were probable illnesses).
Published report 4: Glashower et al. (2017).
FDOSS, Foodborne Disease Outbreak Surveillance System (Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; data received on December 8, 2017); FSIS, United States Department of Agriculture, Food Safety and Inspection Service; NOS, not otherwise specified.
FIG. 1.
Chicken liver–associated campylobacteriosis and salmonellosis outbreaks (n = 28) by year, United States, 2000–2016.
FIG. 2.
Chicken liver–associated campylobacteriosis and salmonellosis outbreaks (n = 28) by state of case-patient residence, United States, 2000–2016 (Four outbreaks included case-patients from multiple states).
The 28 outbreaks resulted in a total of 361 illnesses, 46 (12.7%) hospitalizations, and no deaths. The median number of illnesses per outbreak was 5.5 overall (range, 2–190). In general, later outbreaks had fewer illnesses per outbreak; for example, the median number of illnesses per outbreak significantly decreased from 9 during 2000–2013 to 4.5 during 2014–2016 (p = 0.002). Among case-patients with available information, 177 (51.2%) of 343 were women and 196 (62.6%) of 313 were ≥20 years of age.
Of the 28 outbreaks, 23 (82.1%) were caused by Campylobacter only and 3 (10.7%) by Salmonella only; in 2 (7.1%) of the outbreaks, both pathogens caused illnesses. Chicken liver pâté or other blended dishes (e.g., spread, mousse, or butter) were implicated in 24 (85.7%). The implicated chicken liver was reported to be inadequately cooked (or raw) in 26 (92.8%). A foodservice venue was identified as a food-preparation setting in 25 (89.3%). Restaurants, specifically sit-down restaurants, were identified in 22 (78.6%) of the 28 total outbreaks and 18 (75%) of the 24 campylobacteriosis outbreaks.
Discussion
The frequency of restaurants as a food-preparation location observed among outbreaks in this study (78.6% of total and 75% of campylobacteriosis) is higher than that among all foodborne outbreaks of campylobacteriosis (142/451 [31.5%]) and salmonellosis (1039/2297 [45.2%]) reported to FDOSS during 2000–2016 (CDC, 2018). The predominance of foodservice preparation settings in reported chicken liver–associated outbreaks indicates there may be value in targeting restaurants, particularly sit-down restaurants, and other places where chicken liver dishes are commercially prepared for prevention efforts, especially with regard to cooking adequacy. FSIS (2016a) encourages cooking of chicken liver dishes to an internal temperature of 165°F, as measured by a food thermometer, before consumption. Assisted living or senior citizen institutions were noted as food-preparation settings among the outbreaks in this study; special care should be taken to not serve inadequately cooked chicken livers to the elderly or other higher risk populations. Food safety partners from local, state, and federal agencies, academia, and industry should collaborate to develop ways to encourage foodservice workers and consumers to properly cook chicken liver.
Establishments that produce chicken liver for human consumption (e.g., chicken slaughter facilities) should address food safety hazards associated with chicken liver through their Hazard Analysis and Critical Control Points (HACCP) systems. Freezing is an intervention that has been shown to reduce, but not eliminate, Campylobacter in chicken liver (Baumgartner et al., 1995; Harrison et al., 2013). Despite potential concerns that freezing may negatively impact palatability, researchers found that consumers in the United Kingdom had an overall sensory preference for chicken liver pâté made from frozen liver versus fresh liver (Hutchinson et al., 2015). In this same study, the researchers demonstrated that organic acid washes reduced Campylobacter contamination on chicken liver. High-pressure processing has been shown to reduce pathogens in other chicken products (Solomon and Hoover, 2004; Jackowska-Tracz and Tracz, 2015) and it may also be effective in chicken liver.
To increase the availability of data on chicken liver–specific prevention strategies, In July 2016, FSIS (2016b) included in its list of food safety research priority items specific to chicken liver. Given that inadequate cooking was a common contributing factor among the outbreaks in this study, an important research need is to develop and validate a method of cooking chicken liver, particularly blended chicken liver (e.g., pâté), that is safe to consume and well accepted by both chefs and consumers. FSIS is collaborating with the Agricultural Research Service and universities on chicken liver–related studies to improve understanding of chicken liver contamination with pathogens and of consumer and chef preferences, practices, and knowledge of risk.
Recent FSIS sampling results are consistent with other data demonstrating pathogen contamination in chicken liver. In November 2016, FSIS (2016c) began sampling and analyzing chicken livers from FSIS-regulated establishments for Campylobacter and Salmonella. For these samples, the livers are rinsed in sterile broth and the rinsate is submitted for analysis. Among chicken liver samples collected by FSIS during November 2016 to November 2017, Campylobacter was isolated from 66/87 (75.9%) samples and Salmonella from 57/85 (67.1%) samples (FSIS, unpublished data). Although the small sample size precludes estimation of prevalence, these results signal opportunities for improved pathogen reduction in this part of the chicken.
The observed predominance of campylobacteriosis over salmonellosis outbreaks is noteworthy. Both Campylobacter and Salmonella have been shown to contaminate chicken liver; indeed, two outbreaks in this study involved both pathogens, suggesting concurrent contamination. In addition, both pathogens have been recovered from chicken livers after experimental oral inoculation. Although several published studies have demonstrated the presence of Campylobacter in the internal tissues of chicken liver, to our knowledge, no such studies for Salmonella have been reported. Although internal Salmonella presence may simply not have been assessed, it is also possible that Campylobacter could more likely be present than Salmonella in internal chicken liver tissues. This would help explain the greater number of campylobacteriosis outbreaks and would further highlight the importance of inadequate cooking as a contributing factor.
The observed increase in reported chicken liver–associated outbreaks, particularly campylobacteriosis, is consistent with a concurrent increase in foodborne campylobacteriosis outbreaks overall (CDC, 2018). One explanation for the increase observed in this study is that these outbreaks could actually have begun to occur more frequently. Alternatively, a number of illness surveillance factors might also have promoted outbreak recognition and reporting in the latter years of the study, including: higher index of suspicion for chicken liver as an illness vehicle after published reports of outbreaks since 2011 (Tompkins et al., 2013; Hanson et al., 2014; Scott et al., 2015; Glashower et al., 2017); the addition of chicken liver exposure to campylobacteriosis questionnaires used in the Foodborne Diseases Active Surveillance Network (FoodNet) in 2015 (CDC, unpublished data); and the addition of campylobacteriosis to the U.S. list of nationally notifiable diseases in 2015 (Adams et al., 2017). In addition, in 2017, CDC added chicken liver to the National Hypothesis Generating Questionnaire for enteric illness outbreak investigation (CDC, 2017b). Over time, these factors may have improved the detection of small campylobacteriosis outbreaks associated with chicken liver that is consistent with both the increase in the number of observed outbreaks and the decrease in median outbreak size over the length of the study period.
The geographic outbreak clustering observed in this study may reflect regional differences in consumption of inadequately cooked chicken liver dishes. Data regarding chicken liver consumption and preparation patterns are currently lacking, but may help focus prevention efforts. Another explanation for the observed geographic differences in number of outbreaks is that, because of variability in Campylobacter surveillance, some states may have been more likely to detect and report outbreaks (Geissler et al., 2017). Detection of outbreaks caused by Salmonella and other bacterial foodborne pathogens historically has been greatly enhanced through molecular subtyping by pulsed-field gel electrophoresis (PFGE); however, PFGE is not as consistently used to characterize Campylobacter because of testing limitations, hampering detection of outbreaks (Gerner-Smidt et al., 2006). As campylobacteriosis became nationally notifiable in the United States only recently, national-level information has not been readily available. Our findings highlight the importance of standardizing national surveillance for campylobacteriosis that is important to understand the burden of illness, identify outbreaks, attribute sources of infection, and target measures for prevention and control.
Illnesses associated with reported outbreaks represent only a small proportion of the true illness burden. According to FoodNet data, <1% and 6%, respectively, of reported Campylobacter and Salmonella infections are part of a recognized outbreak (CDC, 2014). Furthermore, it is estimated that for every reported case of Campylobacter or Salmonella infection, there are ∼30 cases undiagnosed or not reported (Scallan et al., 2011). Hence, the actual number of illnesses associated with chicken liver during the study period was likely many times more than the 361 reported here. A case–control study in New Zealand indicated that consumption of chicken liver was a risk factor for sporadic campylobacteriosis (Eberhart-Phillips et al., 1997); to our knowledge, the extent to which chicken liver exposure may be a risk factor for sporadic illness in the United States has not been assessed in a published study.
Conclusions
The increasing numbers of reported outbreaks in recent years highlight chicken liver as an important foodborne illness vehicle. The consumption of inadequately cooked chicken liver dishes noted in this study poses a food safety concern made greater by the strong evidence suggesting the presence of pathogens inside chicken liver. To address this problem, public health officials and stakeholders should collaborate to pursue multipronged prevention strategies, including enhancing illness and outbreak surveillance, pursuing needed research, and encouraging food preparers to fully cook chicken liver dishes.
Acknowledgments
The authors thank the local, state, and federal officials who investigated and reported these outbreaks. The authors completed this study during the course of their employment with the U.S. Federal Government. No other financial support was received for this study.
Disclaimers
The findings and conclusions in this preliminary publication have not been formally disseminated by the U.S. Department of Agriculture and should not be construed to represent any agency determination or policy.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Disclosure Statement
No competing financial interests exist.
References
- Abd-Elghany SM, Sallam KI, Abd-Elkhalek A, Tamura T. Occurrence, genetic characterization and antimicrobial resistance of Salmonella isolated from chicken meat and giblets. Epidemiol Infect 2015;143:997–1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams DA, Thomas KR, Jajosky RA, Foster L, Baroi G, Sharp P, Onweh DH, Schley AW, Anderson WJ; Nationally Notifiable Infectious Conditions Group. Summary of notifiable infectious diseases and conditions—United States, 2015. MMWR Morb Mortal Wkly Rep 2017;64:1–143 [DOI] [PubMed] [Google Scholar]
- Barot MS, Mosenthal AC, Bokkenheuser VD. Location of Campylobacter jejuni in infected chicken livers. J Clin Microbiol 1983;17:921–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner A, Grand M, Liniger M, Simmen A. Campylobacter contaminations of poultry liver—Consequences for food handlers and consumers. Arch Lebensm Hyg 1995;46:11–12 [Google Scholar]
- Borsoi A, Santin E, Santos LR, Salle CTP, Moraes HLS, Nascimento VP. Inoculation of newly hatched broiler chicks with two Brazilian isolates of Salmonella Heidelberg strains with different virulence gene profiles, antimicrobial resistance, and pulsed field gel electrophoresis patterns to intestinal changes evaluation. Poult Sci 2009;88:750–758 [DOI] [PubMed] [Google Scholar]
- Boukraa L, Messier S, Robinson Y. Isolation of Campylobacter from livers of broiler chickens with and without necrotic hepatitis lesions. Avian Dis 1991;35:714–717 [PubMed] [Google Scholar]
- [CDC] The Centers for Disease Control and Prevention. Foodborne Diseases Active Surveillance Network (FoodNet): FoodNet Surveillance Report for 2014 (Final Report). Atlanta, GA: US Department of Health and Human Services, CDC, 2014. Available at: www.cdc.gov/foodnet/pdfs/2014-foodnet-surveillance-report.pdf, accessed April20, 2018
- [CDC] The Centers for Disease Control and Prevention. Foodborne Disease Outbreak Reporting System. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, 2017a. Available at: https://www.cdc.gov/fdoss/index.html accessed August10, 2018 [Google Scholar]
- [CDC] The Centers for Disease Control and Prevention. Foodborne Disease Outbreak Investigation and Surveillance Tools. 2017b. Available at: www.cdc.gov/foodsafety/outbreaks/surveillance-reporting/investigation-toolkit.html, accessed January2, 2018
- [CDC] The Centers for Disease Control and Prevention. National Outbreak Reporting System (NORS)—NORS Dashboard. 2018. Available at: wwwn.cdc.gov/norsdashboard, accessed March23, 2018
- Chai SJ, Cole D, Nisler A, Mahon BE. Poultry: The most common food in outbreaks with known pathogens, United States, 1998–2012. Epidemiol Infect 2017;145:316–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaloner G, Wigley P, Humphrey S, Kemmett K, Lacharme-Lora L, Humphrey T, Williams N. Dynamics of dual infection with Campylobacter jejuni strains in chickens reveals distinct strain-to-strain variation in infection ecology. Appl Environ Microbiol 2014;80:6366–6372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox NA, Richardson LJ, Buhr RJ, Fedorka-Cray PJ. Campylobacter species occurrence within internal organs and tissues of commercial caged Leghorn laying hens. Poult Sci 2009;88:2449–2456 [DOI] [PubMed] [Google Scholar]
- The Dallas Morning News, Inc. Chicken Livers Rule the Roost as an Unexpected, Exciting Ingredient. 2013. Available at: www.dallasnews.com/life/life/2013/02/19/chicken-livers-rule-the-roost-as-an-unexpected-exciting-ingredient, accessed April20, 2018
- Eberhart-Phillips J, Walker N, Garrett N, Bell D, Sinclair D, Rainger W, Bates M. Campylobacteriosis in New Zealand: Results of a case-control study. J Epidemiol Community Health 1997;51:686–691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [FDA] Food and Drug Administration. Food Code. 2013. Available at: www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf, accessed January17, 2018
- Firlieyanti AS, Connerton PL, Connerton IF. Campylobacters and their bacteriophages from chicken liver: The prospect for phage biocontrol. Int J Food Microbiol 2016;237:121–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food Network (Scripps Networks LLC; online recipe courtesy of Alton Brown). Chicken Liver Mousse. Available at: www.foodnetwork.com/recipes/alton-brown/chicken-liver-mousse-recipe-1940241, accessed April20, 2018
- Friedman CR, Hoekstra RM, Samuel M, Marcus R, Bender J, Shiferaw B, Reddy S, Ahuja SD, Helfrick DL, Hardnett F, Carter M, Anderson B, Tauxe RV; Emerging Infections Program FoodNet Working Group. Risk factors for sporadic Campylobacter infection in the United States: A case-control study in FoodNet sites. Clin Infect Dis 2004;38(Suppl 3):S285–S296 [DOI] [PubMed] [Google Scholar]
- [FSIS] Food Safety and Inspection Service. Safe Minimum Internal Temperature Chart. 2015. Available at: www.fsis.usda.gov/wps/portal/fsis/topics/food-safety-education/get-answers/food-safety-fact-sheets/safe-food-handling/safe-minimum-internal-temperature-chart/ct_index, accessed February21, 2018
- [FSIS] Food Safety and Inspection Service. (Foodsafety.gov blog by Adam Gehring FSIS). Winner Winner Chicken Liver. 2016a. Available at: www.foodsafety.gov/blog/2016/03/chicken-liver.html, accessed April20, 2018
- [FSIS] Food Safety and Inspection Service. Food Safety Research Studies. 2016b. Available at: www.fsis.usda.gov/wps/portal/fsis/topics/science/food-safety-research-priorities/food-safety-research-studies, accessed December21, 2016
- [FSIS] Food Safety and Inspection Service. FSIS Notice 72-16: Other Raw Chicken Parts Sampling Project. 2016c. Available at: www.fsis.usda.gov/wps/wcm/connect/5ef0f371-0ce7-4eaf-9cdc-3fe618356d56/72-16.pdf?MOD=AJPERES&CONVERT_TO=url&CACHEID=5ef0f371-0ce7-4eaf-9cdc-3fe618356d56, accessed April20, 2018
- Fullerton KE, Ingram LA, Jones TF, Anderson BJ, McCarthy PV, Hurd S, Shiferaw B, Vugia D, Haubert N, Hayes T, Wedel S, Scallan E, Henao O, Angulo FJ. Sporadic campylobacter infection in infants: A population-based surveillance case-control study. Pediatr Infect Dis J 2007;26:19–24 [DOI] [PubMed] [Google Scholar]
- Gast RK, Guraya R, Jones DR, Anderson KE. Colonization of internal organs by Salmonella Enteritidis in experimentally infected laying hens housed in conventional or enriched cages. Poult Sci 2013;92:468–473 [DOI] [PubMed] [Google Scholar]
- Geissler AL, Carrillo FB, Swanson K, Patrick ME, Fullerton KE, Bennett C, Barrett K, Mahon BE. Increasing Campylobacter infections, outbreaks, and antimicrobial resistance in the United States, 2004–2012. Clin Infect Dis 2017;65:1624–1631 [DOI] [PubMed] [Google Scholar]
- Gerner-Smidt P, Hise K, Kincaid J, Hunter S, Rolando S, Hyytiä-Trees E, Ribot EM, Swaminathan B; PulseNet Taskforce. PulseNet USA: A five-year update. Foodborne Pathog Dis 2006;3:9–19 [DOI] [PubMed] [Google Scholar]
- Glashower D, Snyder J, Welch D, McCarthy S. Notes from the field: Outbreak of Campylobacter jejuni associated with consuming undercooked chicken liver mousse—Clark County, Washington, 2016. MMWR Morb Mortal Wkly Rep 2017;66:1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson H, Hancock WT, Harrison C, Kornstein L, Waechter H, Reddy V, Luker J, Malavet M, Huth P, Gieraltowski L, Balter S. Creating student sleuths: How a team of graduate students helped solve an outbreak of Salmonella Heidelberg infections associated with kosher broiled chicken livers. J Food Prot 2014;77:1390–1393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison D, Corry JEL, Tchórzewska MA, Morris VK, Hutchison ML. Freezing as an intervention to reduce the numbers of campylobacters isolated from chicken livers. Lett Appl Microbiol 2013;57:206–213 [DOI] [PubMed] [Google Scholar]
- He GZ, Tian WY, Qian N, Cheng C, Deng SX. Quantitative studies of the distribution pattern for Salmonella Enteritidis in the internal organs of chicken after oral challenge by a real-time PCR. Vet Res Commun 2010;34:669–676 [DOI] [PubMed] [Google Scholar]
- Hutchinson M, Harrison D, Richardson I, Tchórzewska M. A method for the preparation of chicken liver pâté that reliably destroys campylobacters. Int J Environ Res Public Health 2015;12:4652–4669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackowska-Tracz A, Tracz M. Effects of high hydrostatic pressure on Campylobacter jejuni in poultry meat. Pol J Vet Sci 2015;18:261–266 [DOI] [PubMed] [Google Scholar]
- Kassenborg HD, Smith KE, Vugia DJ, Rabatsky-Ehr T, Bates MR, Carter MA, Dumas NB, Cassidy MP, Marano N, Tauxe RV, Angulo FJ; Emerging Infections Program FoodNet Working Group. Fluoroquinolone-resistant Campylobacter infections: Eating poultry outside of the home and foreign travel are risk factors. Clin Infect Dis 2004;38(Suppl 3):S279–S284 [DOI] [PubMed] [Google Scholar]
- Kimura AC, Reddy V, Marcus R, Cieslak PR, Mohle-Boetani JC, Kassenborg HD, Segler SD, Hardnett FP, Barrett T, Swerdlow DL; Emerging Infections Program FoodNet Working Group. Chicken consumption is a newly identified risk factor for sporadic Salmonella enterica serotype Enteritidis infections in the United States: A case-control study in FoodNet sites. Clin Infect Dis 2004;38(Suppl 3):S244–S252 [DOI] [PubMed] [Google Scholar]
- Knudsen KN, Bang DD, Andresen LO, Madsen M. Campylobacter jejuni strains of human and chicken origin are invasive in chickens after oral challenge. Avian Dis 2006;50:10–14 [DOI] [PubMed] [Google Scholar]
- Little CL, Gormley FJ, Rawal N, Richardson JF. A recipe for disaster: Outbreaks of campylobacteriosis associated with poultry liver pâté in England and Wales. Epidemiol Infect 2010;138:1691–1694 [DOI] [PubMed] [Google Scholar]
- Los Angeles Times. Chicken Livers Can Give You a Rich Foie Gras Taste on a Budget. 2015. Available at: www.latimes.com/food/la-fo-calcook-chicken-livers-20150221-story.html, accessed April20, 2018
- Merritt T, Combs B, Pingault N. Campylobacter outbreaks associated with poultry liver dishes. Commun Dis Intell Q Rep 2011;35:299–300 [PubMed] [Google Scholar]
- The New York Times Company (online recipe by Bittman M). Chicken Livers with Caramelized Onions and Mushrooms. Available at: https://cooking.nytimes.com/recipes/1012527-chicken-livers-with-caramelized-onions-and-mushrooms?mcubz=1, accessed April20, 2018
- Noormohamed A, Fakhr MK. Incidence and antimicrobial resistance profiling of Campylobacter in retail chicken livers and gizzards. Foodborne Pathog Dis 2012;9:617–624 [DOI] [PubMed] [Google Scholar]
- Nyati KK, Nyati R. Role of Campylobacter jejuni infection in the pathogenesis of Guillain-Barré syndrome: An update. Biomed Res Int 2013;2013:Article ID 852195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [NZMPI] New Zealand Ministry of Primary Industries. Risk Profile: Campylobacter jejuni/coli in Mammalian and Poultry Offals. 2007. Available at: www.mpi.govt.nz/food-safety/food-safety-and-suitability-research/food-risk-assessment/food-risk-profiles/, accessed April20, 2018
- [NZMPI] New Zealand Ministry of Primary Industries. Risk Profile: Campylobacter jejuni/coli in Poultry (Whole and Pieces). 2013. Available at: www.mpi.govt.nz/food-safety/food-safety-and-suitability-research/food-risk-assessment/food-risk-profiles, accessed April20, 2018
- Sanyal SC, Islam KM, Neogy PK, Islam M, Speelman P, Huq MI. Campylobacter jejuni diarrhea model in infant chickens. Infect Immun 1984;43:931–936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson M, Roy SL, Jones JL, Griffin PM. Foodborne illness acquired in the United States—Major pathogens. Emerg Infect Dis 2011;17:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scallan E, Hoekstra RM, Mahon BE, Jones TF, Griffin PM. An assessment of the human health impact of seven leading foodborne pathogens in the United States using disability adjusted life years. Epidemiol Infect 2015;143:2795–2804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott MK, Geissler A, Poissant T, DeBess E, Melius B, Eckmann K, Salehi E, Cieslak PR. Notes from the field: Campylobacteriosis outbreak associated with consuming undercooked chicken liver pâté—Ohio and Oregon, December 2013–January 2014. MMWR Morb Mortal Wkly Rep 2015;64:399. [PMC free article] [PubMed] [Google Scholar]
- Solomon EB, Hoover DG. Inactivation of Campylobacter jejuni by high hydrostatic pressure. Lett Appl Microbiol 2004;38:505–509 [DOI] [PubMed] [Google Scholar]
- Strachan NJC, MacRae M, Thomson A, Rotariu O, Ogden ID, Forbes KJ. Source attribution, prevalence and enumeration of Campylobacter spp. from retail liver. Int J Food Microbiol 2012;153:234–236 [DOI] [PubMed] [Google Scholar]
- Tompkins BJ, Wirsing E, Devlin V, Kamhi L, Temple B, Weening K, Cavallo S, Allen L, Brinig P, Goode B, Fitzgerald C, Heiman K, Stroika S, Mahon B. Multistate outbreak of Campylobacter jejuni infections associated with undercooked chicken livers—Northeastern United States, 2012. MMWR Morb Mortal Wkly Rep 2013;62:874–876 [PMC free article] [PubMed] [Google Scholar]
- Whyte R, Hudson JA, Graham C. Campylobacter in chicken livers and their destruction by pan frying. Lett Appl Microbiol 2006;43:591–595 [DOI] [PubMed] [Google Scholar]
- Zdragas A, Mazaraki K, Vafeas G, Giantzi V, Papdopoulos T, Ekateriniadou L. Prevalence, seasonal occurrence and antimicrobial resistance of Salmonella in poultry retail products in Greece. Lett Appl Microbiol 2012;55:308–313 [DOI] [PubMed] [Google Scholar]