Abstract
Background
Most liver transplant patients require Intensive Care Unit (ICU) care in the immediate postoperative period and some patients require readmission to the ICU before discharge from the hospital. A retrospective cohort study was conducted to identify risk factors for ICU readmission after liver transplantation.
Material/Methods
Adult patients who underwent living donor or deceased donor liver transplantation at Seoul National University Hospital between 2004 and 2015 were included. A retrospective review of baseline and perioperative factors that may be associated with ICU readmission was performed. Patients requiring ICU readmission during the hospitalization for LT (readmission group) were compared with patients who did not need ICU readmission (control group). A multivariable logistic regression analysis was performed to identify factors associated with ICU readmission after LT.
Results
Of the 1181 patients, 68 patients (5.8%) were readmitted to the ICU during the postoperative period after liver transplantation. Common causes of ICU readmission included postoperative bleeding, pulmonary complications, and sepsis. Multivariate analysis revealed that old age (OR 1.030 95%CI 1.002–1.059, p=0.035), pre-transplant chronic kidney disease (CKD) (OR 4.912 95%CI 2.556–9.439, p<0.001), intraoperative red blood cell (RBC) transfusion (OR 1.029 95%CI 1.008–1.050, p=0.007), new-onset atrial fibrillation in the ICU (OR 2.807 95%CI 1.087–7.249, p=0.033), and transplantation between 2011 and 2015 (vs. 2004–2010) were risk factors for ICU readmission after LT.
Conclusions
Old age, pre-transplant CKD, more intraoperative RBC transfusion, new-onset atrial fibrillation during ICU stay, and transplant period were identified as risk factors for ICU readmission.
MeSH Keywords: Intensive Care Units, Liver Transplantation, Patient Readmission
Background
Liver transplantation (LT) is the treatment of choice for end-stage liver disease [1], with continuously improving post-transplant survival [2]. Most LT patients are closely monitored in the Intensive Care Unit (ICU) for early complications that may occur in the immediate postoperative period. After discharge from the ICU, some LT patients suffer from complications requiring readmission to the ICU before discharge from the hospital [3].
In general, patients who required ICU readmission showed higher mortality and longer hospital length of stay compared to those who did not require ICU readmission [4,5]. Previous studies have shown that factors associated with ICU readmission were difficult to identify and were often unrelated to the initial condition for which the initial ICU admission was required [6–8]. In contrast, risk of ICU readmission after surgery seems to be associated with the underlying disease, the extent of the procedure, and the occurrence of procedure-related complications [9]. LT recipients are at risk of ICU readmission due to not only the complex surgical procedure, but also because of the coexisting morbidities.
The most relevant study regarding factors associated with ICU readmission after LT was reported in 2001 [3]. Older recipient age, pre-transplant hepatic function, and more intraoperative transfusion were associated with ICU readmission. However, the results were unadjusted and there have been significant advances in surgical technique and postoperative care since that time. We conducted a retrospective observational study to identify risk factors for ICU readmission after LT.
Material and Methods
The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (IRB 1609-075-791). Informed consent was waived due to the retrospective cohort study design.
Patient population
Adult patients (age ≥18 years) who underwent living donor or deceased donor LT at Seoul National University Hospital between 2004 and 2015 were included in the study. In patients who underwent re-transplantation during the study period, only the first LT was included for analysis. Patients who required re-transplantation before discharge from the ICU after the first LT and patients who died during the initial ICU stay were excluded.
Study protocol
Patients who required ICU readmission during the hospitalization after LT were identified. LT patient electronic medical records were reviewed and baseline demographic data were recorded. The primary endpoint was readmission to the ICU during the index admission after LT. Perioperative factors with potential association with ICU readmission were also recorded: coexisting liver diseases, comorbidities, donor age, type of donor (living or deceased), operation type (elective or emergency), preoperative laboratory values, preoperative Model for End-Stage Liver Disease Na (MELD-Na), amount of intraoperative transfusion, and postoperative factors during the initial ICU stay. We also investigated transplant year, the ICU and hospital length of stay, the cause of ICU readmission, and in-hospital mortality. Causes of readmission were classified as postoperative bleeding, pulmonary complications, sepsis, neurologic complications, cardiovascular complications, renal complication, and others. LT patients were divided into patients who were readmitted to the ICU (readmission group) and those who were not (control group).
Perioperative management
Standard patient monitoring, including noninvasive arterial blood pressure, electrocardiography, and peripheral oxygen saturation, was performed. The right radial artery and femoral artery were cannulated for arterial blood sampling and real-time monitoring of blood pressure. General anesthesia was induced with propofol and rocuronium, maintained using desflurane or sevoflurane throughout the surgery. An advanced venous access catheter and Swan-Ganz catheter were inserted for hemodynamic and mixed venous oxygen saturation monitoring.
After lysis of adhesion and mobilization of the liver, piggyback technique was routinely used for implantation of the graft liver during anhepatic phase in our center. The hepatic and portal vein anastomoses are completed in that order. Hepatic artery and bile duct anastomosis was conducted after reperfusion.
All patients were admitted to the surgical ICU after LT and were closely monitored for 3–4 days. Immune suppression was maintained with tacrolimus, mycophenolate mofetil, and corticosteroids. Patients were discharged from the ICU when they met the discharge criteria: stable vital signs, alert and oriented mental status, and stabilization of laboratory and ultrasound findings.
Statistical analysis
Categorical data were compared using the two-tailed Fisher’s exact test for 2×2 tables and the likelihood ratio chi-square test for larger tables. Continuous data were analyzed using the two-sample t test, or the Mann-Whitney U test when the data were skewed. Variables for which p-value were less than or equal to 0.1 in univariable analysis were incorporated into multivariate analysis using logistic regression to identify risk factors for readmission to the ICU. Variable selection by forward stepwise selection was performed, in which entry and removal were by p≤0.05 and p>0.1, respectively. Clinically relevant variables were also included in the analysis for adjustment. Subgroup analysis by transplant year (early vs. late) and by donor type (living vs. deceased) was performed. Survival analysis was carried out using Kaplan-Meier curves with a log-rank analysis. The statistical analysis was performed using IBM SPSS Statistics software, version 23.0.0 (IBM Corp., Armonk, NY). A p<0.05 was considered statistically significant.
Results
Between 2004 and 2015, 1221 adult patients underwent LT at Seoul National University Hospital. Of the 1221 patients, 40 patients were excluded due to re-transplantation during the same admission (n=12) or death during the initial ICU stay (n=28). A total of 1181 LT patients were included in the study. The vast majority of patients had liver cirrhosis and about half of the patients had hepatitis B virus and/or hepatocellular carcinoma (Table 1).
Table 1.
Risk factors of ICU readmission after liver transplantation.
| Univariable analysis | Multivariable analysis | ||||
|---|---|---|---|---|---|
| Readmission (n=68) | No readmission (n=1113) | p-Value | Odds ratio (95% CI) | p-Value | |
| Age (years) | 56.5±10.5 | 52.7±9.8 | 0.002 | 1.030 (1.002–1.059) | 0.035 |
| Male | 47 (69.1) | 807 (72.5) | 0.577 | ||
| Body mass index (kg/m2) | 23.3±4.2 | 23.4±3.4 | 0.872 | ||
| Coexisting liver diseases | |||||
| Liver cirrhosis | 64 (94.1) | 982 (88.2) | 0.170 | ||
| Hepatitis B virus | 33 (48.5) | 630 (56.6) | 0.209 | ||
| Hepatitis C virus | 12 (17.6) | 116 (10.4) | 0.070 | ||
| Metabolic disease | 0 (0.0) | 12 (1.1) | 1.000 | ||
| Alcoholic | 13 (19.1) | 155 (13.9) | 0.281 | ||
| Hepatocellular carcinoma | 37 (54.4) | 566 (50.9) | 0.618 | ||
| Comorbidity | |||||
| Hypertension | 15 (22.1) | 178 (16.0) | 0.180 | ||
| Diabetes | 21 (30.9) | 296 (26.6) | 0.481 | ||
| Coronary artery disease | 4 (5.9) | 11 (1.0) | 0.008 | ||
| Chronic kidney disease | 22 (32.4) | 73 (6.6) | <0.001 | 4.912 (2.556–9.439) | <0.001 |
| Donor age (years) | 29.5±11.2 | 32.4±11.5 | 0.115 | ||
| Living donor | 39 (57.4) | 793 (71.2) | 0.019 | ||
| MELD-Na score | 22.4±10.6 | 18.1±11.5 | 0.003 | 1.009 (0.984–1.034) | 0.505 |
| Intraoperative RBC transfusion (unit) | 14.1±14.2 | 9.6±10.0 | 0.015 | 1.029 (1.008–1.050) | 0.007 |
| Elective operation | 38 (55.9) | 752 (67.6) | 0.062 | ||
| Operation time (hours) | 8.2±1.7 | 8.4±1.7 | 0.417 | ||
| During ICU stay | |||||
| APACHE II (admission) | 25.3±6.4 | 23.0±6.4 | 0.005 | 1.019 (0.972–1.069) | 0.436 |
| New-onset atrial fibrillation | 7 (10.3) | 32 (2.9) | 0.005 | 2.807 (1.087–7.249) | 0.033 |
| Length of stay in initial ICU | 5.7 [2.7–31.3] | 4.8 [3.6–139.7] | 0.002 | 1.000 (0.991–1.009) | 0.986 |
| Transplant year | 0.005 | ||||
| 2004–2010 | 18 (26.5) | 487 (43.8) | Reference | ||
| 2011–2015 | 50 (73.5) | 626 (56.2) | 1.899 (1.021–3.530) | 0.043 | |
Categorical data were expressed as number (%) and analyzed using chi-square test. Continuous data were expressed as mean ± standard deviation or median [range] and were analyzed using the two-sample Student’s t-test or the Mann-Whitney U statistic. Multivariable analysis was conducted using logistic regression with forward stepwise selection. Goodness-of-fit test of Hosmer-Lemeshow for Final model: p=0.819. Missing cases due to missing item ‘MELD-Na score’: 4/1181, 0.3%. MELD – Model for End-stage Liver Disease; RBC – red blood Cell; ICU – Intensive Care Unit; APACHE II – Acute Physiology and Chronic Health Evaluation II; CI – confidence interval.
ICU readmissions occurred in 5.8% (68/1181) of patients after their initial discharge from the ICU. Of the 68 ICU readmissions, 25% (17/68) occurred within 48 h of initial ICU discharge. The median duration between initial ICU discharge and ICU readmission was 81.9 (2.8–2072) h. There was an increase in the ICU readmission rate during the study period. The readmission rate was 3.6% between 2004 and 2010 and 7.4% between 2011 and 2015.
Overall, postoperative bleeding was the most common cause of ICU readmission, followed by pulmonary complications (desaturation or tachypnea), and sepsis. Other causes included neurologic complications (seizure, stroke, delirium), cardiovascular complications (arrhythmia or non-sepsis hypotension), and renal complications. Pulmonary complications were the most common cause of ICU readmission beyond 48 h of initial ICU discharge. Causes of ICU readmission within and beyond 48 h were similar (p=0.274) (Table 2).
Table 2.
Causes of ICU readmission after liver transplantation.
| Total (n=68) | Within 48 hours (n=17) | Beyond 48 hours (n=51) | |
|---|---|---|---|
| Postoperative bleeding | 15 (22.1) | 6 (35.3) | 9 (17.6) |
| Pulmonary complications | 13 (19.1) | 3 (17.6) | 10 (19.6) |
| Sepsis | 12 (17.6) | 3 (17.6) | 9 (17.60) |
| Neurologic complications | 10 (14.7) | 3 (17.6) | 7 (13.7) |
| Cardiovascular complications | 8 (11.8) | 2 (11.8) | 6 (11.8) |
| Renal complication | 4 (5.9) | 0 (0) | 4 (7.8) |
| Others | 6 (8.8) | 0 (0) | 6 (11.8) |
Data are expressed as number (%). Distributions of causes of ICU readmission within and beyond 48 hours were similar (likelihood ratio chi-square test, p=0.274).
The initial ICU length of stay (LOS) was longer in the readmission group compared to the control group (5.7 [2.7–31.3] days vs. 4.8 [3.6–139.7] days, p=0.002). The hospital length of stay was also longer in the readmission group compared to the control group (59.9 [12.9–305.5] days vs. 23.6 [10.6–819.7] days, p<0.001).
The overall in-hospital mortality rate was 1.4% (16/1181). In-hospital mortality was 23.5% (16/68) in the readmission group in contrast to no hospital deaths in the control group. One-year mortality was also significantly lower in the control group (23.5% vs. 0.1%, p<0.001) (Figure 1). The most common cause of in-hospital mortality in the readmission group was septic shock (62.5%, 10/16). Other causes included multiorgan failure, pneumonia, hemorrhage, and arrhythmia.
Figure 1.
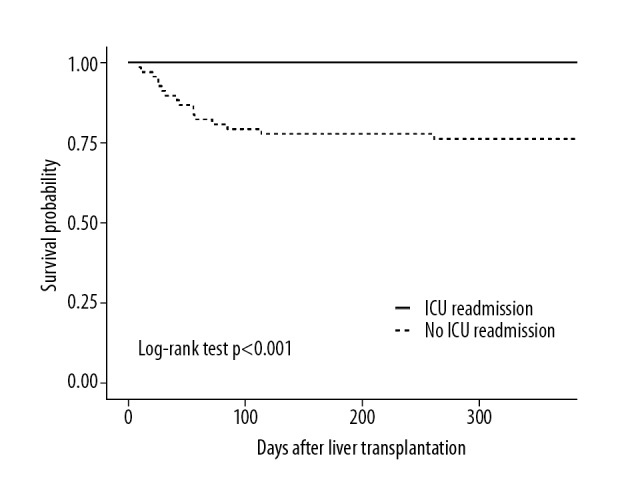
Overall survival of patients in the readmission group and the control group within 1 year after liver transplantation. Survival analysis was carried out using Kaplan-Meier curves with a log-rank analysis. Patients in the readmission group had decreased long-term survival compared with those in the control group within the first year (log-rank test, p<1.001).
Multivariate analysis showed that old age (OR 1.030 95%CI 1.002–1.059, p=0.035), pre-transplant CKD (OR 4.912 95%CI 2.556–9.439, p<0.001), intraoperative red blood cell (RBC) transfusion (OR 1.029 95%CI 1.008–1.050, p=0.007), new-onset atrial fibrillation in the ICU (OR 2.807 95%CI 1.087–7.249, p=0.033), and transplantation between 2011 and 2015 (vs. 2004–2010) were risk factors of ICU readmission after LT (Table 1).
Patients were analyzed depending on the period in which LT was performed (2004–2010 vs. 2011–2015). Patient characteristics in early and late transplant years are summarized in Table 3. Although not included in the analysis, re-transplantation and death during the initial ICU stay were 1.5% (8/524) and 2.1% (11/524) in early transplant years vs. 0.6% (4/697) and 2.4% (17/697) in late transplant years (p=0.141 for re-transplantation, p=0.847 for death during the initial ICU stay).
Table 3.
Comparison of patient characteristics: 2004–10 vs. 2011–15.
| 2004–2010 (n=505) | 2011–2015 (n=676) | p-Value | |
|---|---|---|---|
| Age (years) | 51.1±9.5 | 54.2±9.8 | <0.001 |
| Male | 374 (74.5) | 480 (70.7) | 0.131 |
| Body mass index (kg/m2) | 23.2±3.3 | 23.5±3.5 | 0.244 |
| Coexisting liver diseases | |||
| Liver cirrhosis | 458 (90.7) | 588 (87.0) | 0.052 |
| Hepatitis B virus | 254 (50.3) | 409 (60.5) | 0.001 |
| Hepatitis C virus | 50 (9.9) | 78 (11.5) | 0.395 |
| Metabolic disease | 5 (1.0) | 7 (1.0) | 1.000 |
| Alcoholic | 47 (9.3) | 121 (17.9) | <0.001 |
| Hepatocellular carcinoma | 231 (45.7) | 372 (55.0) | 0.002 |
| Comorbidity | |||
| Hypertension | 79 (15.6) | 114 (16.9) | 0.633 |
| Diabetes | 170 (33.7) | 147 (21.7) | <0.001 |
| Coronary artery disease | 3 (0.6) | 12 (1.8) | 0.112 |
| Chronic kidney disease | 24 (4.8) | 71 (10.5) | <0.001 |
| Donor age (years) | 30.3±10.6 | 33.6±11.8 | <0.001 |
| Living donor | 368 (72.9) | 464 (68.6) | 0.122 |
| MELD-Na score | 21.5±10.8 | 16.0±11.4 | <0.001 |
| Intraoperative RBC transfusion (unit) | 12.3±11.3 | 8.0±1.6 | <0.001 |
| Elective operation | 337 (66.7) | 453 (67.0) | 0.950 |
| Operation time (hours) | 8.9±1.7 | 7.9±1.6 | <0.001 |
| During ICU stay | |||
| APACHE II (admission) | 21.6±5.7 | 24.3±5.6 | <0.001 |
| New-onset atrial fibrillation | 12 (2.4) | 27 (4.0) | 0.140 |
| Length of stay in initial ICU | 8.0 [2.2–675.7] | 4.1 [1.6–819.4] | <0.001 |
| In-hospital mortality | 4 (0.8) | 12 (1.8) | 0.204 |
Categorical data were expressed as number (%) and analyzed using chi-square test. Continuous data were expressed as mean ± standard deviation or median [range] and were analyzed using the two-sample Student’s t-test or the Mann-Whitney U statistic.
Subgroup analysis by transplant period showed pre-transplant CKD (OR 9.213 95%CI 2.443–34.750, p=0.001) and intraoperative RBC transfusion (OR 1.036 95%CI 1.006–1.067, p=0.018) as risk factors of ICU readmission in early transplant years (2004–2010), but only pre-transplant CKD (OR 5.556 95%CI 2.855–10.812, p<0.001) in late transplant years (2011–2015) after adjusting for age, APACHE II score at ICU admission, new-onset atrial fibrillation during ICU stay, and length of initial ICU stay (Table 4).
Table 4.
Multivariable analysis of ICU readmission risk factors: 2004–10 vs. 2011–15.
| 2004–2010 | 2011–2015 | |||
|---|---|---|---|---|
| Odds ratio (95% CI) | p-Value | Odds ratio (95% CI) | p-Value | |
| Age (years) | 1.078 (1.011–1.148) | 0.021 | 1.015 (0.985–1.047) | 0.321 |
| Pre-transplant chronic kidney disease | 9.213 (2.443–34.750) | 0.001 | 5.556 (2.855–10.812) | <0.001 |
| Intraoperative RBC transfusion (unit) | 1.036 (1.006–1.067) | 0.018 | ||
| APACHE II (ICU admission) | 1.013 (0.932–1.100) | 0.766 | 1.026 (0.969–1.087) | 0.375 |
| New-onset atrial fibrillation | 4.713 (0.782–28.395) | 0.091 | 2.635 (0.870–7.983) | 0.087 |
| Length of initial ICU stay | 0.996 (0.953–1.041) | 0.864 | 1.000 (0.991–1.009) | 0.994 |
Subgroup analysis by transplant year was adjusted for age, APACHE II score at ICU admission, new-onset atrial fibrillation during ICU stay, and length of initial ICU stay.
Subgroup analysis by donor type showed pre-transplant CKD (OR 10.173 95%CI 4.528–22.859, p<0.001) and intraoperative RBC transfusion (OR 1.050 95%CI 1.019–1.082, p=0.001) as risk factors of ICU readmission in living donor LT. In deceased donor LT patients, pre-transplant CKD (OR 2.649 95%CI 1.020–6.879, p=0.045) and new-onset atrial fibrillation (OR 4.032 95%CI 1.350–12.046, p=0.013) were identified as risk factors of ICU readmission (Table 5).
Table 5.
Multivariable analysis of ICU readmission risk factors: living donor LT vs. deceased donor LT.
| Living donor LT | Deceased donor LT | |||
|---|---|---|---|---|
| Odds ratio (95% CI) | p-Value | Odds ratio (95% CI) | p-Value | |
| Age (years) | 1.046 (1.003–1.091) | 0.035 | 1.019 (0.982–1.057) | 0.318 |
| Pre-transplant chronic kidney disease | 10.173 (4.528–22.859) | <0.001 | 2.649 (1.020–6.879) | 0.045 |
| Intraoperative RBC transfusion (unit) | 1.050 (1.019–1.082) | 0.001 | ||
| APACHE II (ICU admission) | 1.022 (0.950–1.099) | 0.557 | 1.005 (0.943–1.072) | 0.879 |
| New-onset atrial fibrillation | 0.755 (0.073–7.759) | 0.813 | 4.032 (1.350–12.046) | 0.013 |
| Length of initial ICU stay | 0.998 (0.968–1.029) | 0.900 | 1.001 (0.993–1.009) | 0.756 |
| Transplant year (recent) | 2.032 (0.887–4.654) | 0.094 | 1.605 (0.634–4.063) | 0.318 |
Subgroup analysis by donor type was adjusted for age, APACHE II score at ICU admission, new-onset atrial fibrillation during ICU stay, length of initial ICU stay, and transplant year.
Discussion
Our study showed that 5.8% of adult living or deceased donor LT patients required readmission to the ICU before discharge after LT. Identified risk factors of ICU readmission included old age, pre-transplant CKD, intraoperative RBC transfusion, new-onset atrial fibrillation, and transplant period. The ICU readmission rate of our study is similar to that of a previous study of medical and surgical ICU patients, which showed ICU readmission rates between 4% and 10% [5]. In other high-risk surgical populations, ICU readmission rates were 3.3% after lung resection [10] and 3.6% after cardiac surgery [11].
The readmission rate in our study was lower compared to the sole previous study regarding ICU readmission after liver transplantation (5.8% vs. 19%) [3]. The discrepancy in ICU readmission rates may be due to differences in the LT population (predominantly living donor LT vs. predominantly deceased donor LT) and the study period (2004–2015 vs. 1984–1996). The decreasing trend in MELD scores of LT patients at the time of transplant is in sharp contrast to LT centers where the majority of LTs are deceased donor LTs [12]. The tendency for an earlier decision to transplant seems to be fueled by excellent outcome after living donor LT and the availability of liver donors. Another difference may be the longer initial ICU length of stay (median 4.1 days in the more recent period). While this likely represents local practice patterns, many patients in Western LT centers are placed on “fast track” and are discharged from the hospital in 5–7 days [13]. In addition to the lower severity of disease, the potentially earlier detection of postoperative complications due to the longer hospital length of stay may have influenced the lower incidence of ICU readmission. Causes of ICU readmission were also different, with more postoperative bleeding and less allograft dysfunction in our study compared to the previous report [3]. Advances in immunosuppression and differences in patient populations may also have played a role. In addition, patients who underwent re-transplantation before ICU discharge after the initial LT had been excluded from the analysis, which may have reduced the chance of ICU readmission due to allograft dysfunction.
ICU readmission has been associated with increased in-hospital mortality of up to 10 times [5,6] and longer hospital length of stay compared to patients who did not require ICU readmission [5]. Our study also demonstrated higher in-hospital and 1-year mortality, as well as prolonged hospitalization, in LT patients requiring ICU readmission.
In the LT population, old recipient age, impaired pre-transplant hepatic function (prothrombin time, albumin, bilirubin levels), and higher intraoperative transfusion requirements have been suggested as factors related to ICU readmission after LT [3]. Similarly, pre-transplant CKD and more intraoperative red blood cell (RBC) transfusion were identified as independent predictors of ICU readmission in our study. Of note, postoperative variables were not considered in the study by Levy et al. [3] with no adjustment for relevant factors, whereas all potentially relevant variables were included for multivariable analysis in our study.
Pre-transplant CKD showed a strong association with ICU readmission after LT in our study. Since the introduction of the model for end-stage liver disease for the allocation of organs for liver transplantation in 2002, the heavy weighting of serum creatinine in the model for end-stage liver disease score has resulted in an increased incidence of renal dysfunction seen among patients undergoing liver transplantation [14]. In our center, the overall prevalence of preoperative CKD in LT patients was 8.0%, increasing during the study period (4.8% in early transplant years and 10.5% in late transplant years; Table 3). Pre-existing renal dysfunction has been a predisposing factor for the development of acute kidney injury after LT associated with poor outcomes such as longer time to extubation, longer ICU length of stay, and a lower 90-day patient survival [15,16]. Our study results, which showed pre-existing CKD to be a risk factor for ICU readmission, are in accordance with the previous studies that reported poor outcomes in patients with acute kidney injury
A previous study on blood transfusion in adult living or deceased donor LT patients suggested that intraoperative RBC transfusion may be influenced by severity of liver dysfunction, especially the degree of coagulopathy and, more importantly, the complexity of the surgical procedure [17]. Postoperative bleeding, the most common cause of ICU readmission in our study, may be linked closely with intraoperative RBC requirement, which may reflect the technical difficulty and/or the degree of coagulopathy. The proportion of postoperative bleeding as a cause of ICU readmission after LT in our study was slightly higher compared to the abdominal complication proportion in the study by Levy et al. (22.1% vs. 16.3%) [3]. Again, the differences in patient population (living donor LT vs. deceased donor LT) and study period (2004–2015 vs. 1984–1996) may also have played a role.
Respiratory failure was reported as the most frequent cause for ICU readmission within the initial hospital stay after LT [18]. Respiratory rate at discharge from first ICU stay was identified as an independent risk factor of ICU readmission with a cutoff point of more than 20 breaths/min that predicted ICU readmission with a specificity of 90% and a positive predictive value of 80%. In our study, respiratory complication manifesting desaturation or tachypnea was the second most frequent cause of ICU readmission. The underlying causes of respiratory complications in our data were infection (aspiration, pneumonia), bleeding complication (hemoptysis, hemothorax), and respiratory failure with unknown etiology. We attempted to collect and analyze respiratory rate at discharge but found some of the data to be unreliable, so we excluded it from analysis.
ICU readmissions that occur within 48 h from discharge are often considered as premature discharges from ICU and are frequently used as a quality of care indicator [19]. A strategy to reduce premature discharges in patients at high risk of in-hospital death have been shown to significantly reduce post-ICU mortality [20]. Our study showed that frequent causes of ICU readmission were postoperative bleeding and respiratory complications, for both within and beyond 48 hours after initial discharge from the ICU after LT.
There are some limitations to our study. In addition to the shortcomings of a retrospective observational study design, the patient population was from a single center and predominantly consisted of living donor LT patients. Caution should be taken when extrapolating our results to other LT patient populations. Second, 3.3% (40/1221) of LT patients were not included in the analysis due to death during the initial ICU admission or re-transplantation during the same hospitalization. It may be argued that the sickest patients were excluded from the analysis; hence, the lower ICU readmission rate. However, in-hospital mortality was 4.6% (56/1221) after considering the patients excluded due to death during the initial ICU admission. As noted in the discussion, the discrepancy from the previous study seems most likely to stem from the differences in patient population and study period. However, efforts should be made to improve supportive care so that adverse effects from complications or comorbidities may be attenuated.
Conclusions
In summary, old age, pre-transplant CKD, more intraoperative RBC transfusion, new-onset atrial fibrillation during ICU stay, and transplant period were identified as risk factors of ICU readmission. Careful optimization of these high-risk patients before ICU discharge may help reduce the rate of ICU readmission and potentially increase survival.
Footnotes
Conflicts of interest
None.
Source of support: Departmental sources
References
- 1.Goldstein R, Solomon H, Holman M, et al. Liver transplantation, 1990: A Dallas perspective. Clin Transpl. 1990:123–33. [PubMed] [Google Scholar]
- 2.Jain A, Reyes J, Kashyap R, et al. Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg. 2000;232(4):490–500. doi: 10.1097/00000658-200010000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levy MF, Greene L, Ramsay MA, et al. Readmission to the Intensive Care Unit after liver transplantation. Crit Care Med. 2001;29(1):18–24. doi: 10.1097/00003246-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Rosenberg AL, Hofer TP, Hayward RA, et al. Who bounces back? Physiologic and other predictors of Intensive Care Unit readmission. Crit Care Med. 2001;29(3):511–18. doi: 10.1097/00003246-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg AL, Watts C. Patients readmitted to ICUs*: A systematic review of risk factors and outcomes. Chest. 2000;118(2):492–502. doi: 10.1378/chest.118.2.492. [DOI] [PubMed] [Google Scholar]
- 6.Alban RF, Nisim AA, Ho J, et al. Readmission to surgical intensive care increases severity-adjusted patient mortality. J Trauma. 2006;60(5):1027–31. doi: 10.1097/01.ta.0000218217.42861.b7. [DOI] [PubMed] [Google Scholar]
- 7.Cohn WE, Sellke FW, Sirois C, et al. Surgical ICU recidivism after cardiac operations. Chest. 1999;116(3):688–92. doi: 10.1378/chest.116.3.688. [DOI] [PubMed] [Google Scholar]
- 8.Metnitz PG, Fieux F, Jordan B, et al. Critically ill patients readmitted to Intensive Care Units – lessons to learn? Intensive Care Med. 2003;29(2):241–48. doi: 10.1007/s00134-002-1584-z. [DOI] [PubMed] [Google Scholar]
- 9.Snow N, Bergin KT, Horrigan TP. Readmission of patients to the surgical Intensive Care Unit: Patient profiles and possibilities for prevention. Crit Care Med. 1985;13(11):961–64. doi: 10.1097/00003246-198511000-00037. [DOI] [PubMed] [Google Scholar]
- 10.Jung JJ, Cho JH, Hong TH, et al. Intensive Care Unit (ICU) readmission after major lung resection: Prevalence, patterns, and mortality. Thorac Cancer. 2017;8(1):33–39. doi: 10.1111/1759-7714.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bardell T, Legare J, Buth K, et al. ICU readmission after cardiac surgery. Eur J Cardiothorac Surg. 2003;23(3):354–59. doi: 10.1016/s1010-7940(02)00767-4. [DOI] [PubMed] [Google Scholar]
- 12.Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124(1):91–96. doi: 10.1053/gast.2003.50016. [DOI] [PubMed] [Google Scholar]
- 13.Taner CB, Willingham DL, Bulatao IG, et al. Is a mandatory Intensive Care Unit stay needed after liver transplantation? Feasibility of fast-tracking to the surgical ward after liver transplantation. Liver Transpl. 2012;18(3):361–69. doi: 10.1002/lt.22459. [DOI] [PubMed] [Google Scholar]
- 14.Chava SP, Singh B, Zaman MB, et al. Current indications for combined liver and kidney transplantation in adults. Transplant Rev (Orlando) 2009;23(2):111–19. doi: 10.1016/j.trre.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Yalavarthy R, Edelstein CL, Teitelbaum I. Acute renal failure and chronic kidney disease following liver transplantation. Hemodial Int. 2007;11(Suppl 3):S7–12. doi: 10.1111/j.1542-4758.2007.00223.x. [DOI] [PubMed] [Google Scholar]
- 16.Hilmi IA, Damian D, Al-Khafaji A, et al. Acute kidney injury following orthotopic liver transplantation: Incidence, risk factors, and effects on patient and graft outcomes. Br J Anaesth. 2015;114(6):919–26. doi: 10.1093/bja/aeu556. [DOI] [PubMed] [Google Scholar]
- 17.Deakin M, Gunson BK, Dunn JA, et al. Factors influencing blood transfusion during adult liver transplantation. Ann R Coll Surg Engl. 1993;75(5):339–44. [PMC free article] [PubMed] [Google Scholar]
- 18.Cardoso FS, Karvellas CJ, Kneteman NM, et al. Respiratory rate at Intensive Care Unit discharge after liver transplant is an independent risk factor for Intensive Care Unit readmission within the same hospital stay: A nested case-control study. J Crit Care. 2014;29(5):791–96. doi: 10.1016/j.jcrc.2014.03.038. [DOI] [PubMed] [Google Scholar]
- 19.Angus DC. Grappling with Intensive Care Unit quality – does the readmission rate tell us anything? Crit Care Med. 1998;26(11):1779–80. doi: 10.1097/00003246-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Daly K, Beale R, Chang R. Reduction in mortality after inappropriate early discharge from Intensive Care Unit: Logistic regression triage model. BMJ. 2001;322(7297):1274–76. doi: 10.1136/bmj.322.7297.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]


