Key Points
Question
Is posttraumatic stress disorder (PTSD) associated with incident type 2 diabetes independent of obesity?
Findings
In this cohort study of 2204 patients without PTSD and 3450 patient with PTSD, the association between PTSD and incident type 2 diabetes was not significant after adjusting for obesity. The incidence of type 2 diabetes in patients with PTSD without obesity is similar to that of all adults in the United States.
Meaning
In the absence of obesity, patients with PTSD are not at increased risk of type 2 diabetes.
This cohort study assesses a veteran population with and without posttraumatic stress disorder (PTSD) to determine if obesity can account for the increased risk of incident type 2 diabetes in patients with PTSD.
Abstract
Importance
Posttraumatic stress disorder (PTSD) is associated with an increased risk of type 2 diabetes mellitus (T2DM). Existing literature has adjusted for obesity in combination with other confounders, which does not allow estimating the contribution of obesity alone on the association of PTSD with incident T2DM.
Objective
The current study was designed to determine if obesity accounted for the association between PTSD and incident T2DM.
Design, Setting, and Participants
This cohort study used data from Veterans Health Administration medical records collected from patients with PTSD and without PTSD from 2008 to 2015. Patients were eligible for study inclusion if they were free of prevalent PTSD and T2DM for 12 months prior to index date. To estimate whether the association of PTSD and incident T2DM remained independent of obesity, Cox proportional hazard models were computed before and after adding obesity to the model and then further expanded by adding psychiatric disorders, psychotropic medications, physical conditions, smoking status, and demographics. Additional Cox models were computed to compare the risk of incident T2DM in patients with PTSD with and without obesity. Data analysis was completed from February 2018 to May 2018.
Exposures
Two International Classification of Diseases, Ninth Revision (ICD-9) codes for PTSD in the same 12 months and obesity, defined by a body mass index of 30 or more or an ICD-9 code for obesity.
Main Outcomes and Measures
Incident T2DM, as defined by ICD-9 codes.
Results
Among 2204 patients without PTSD, the mean (SD) age was 47.7 (14.3) years; 1860 (84.4%) were men, 1426 (64.7%) were white, and 956 (43.4%) were married. Among 3450 patients with PTSD, the mean (SD) age was 42.8 (14.2) years; 2983 (86.5%) were men, 2238 (64.9%) were white, and 1525 (44.2%) were married. The age-adjusted association between PTSD and incident T2DM was significant (hazard ratio [HR], 1.33 [95% CI, 1.08-1.64]; P = .01), and after adding obesity to the model, this association was reduced and no longer significant (HR, 1.16 [95% CI, 0.94-1.43]; P = .18). Results of the full model, which included additional covariate adjustment, revealed no association between PTSD and incident T2DM (HR, 0.84 [95% CI, 0.64-1.10]; P = .19). Among patients with PTSD with obesity, the age-adjusted incidence of T2DM was 21.0 per 1000 person-years vs 5.8 per 1000 person-years in patients without obesity. In patients without PTSD, it was 21.2 per 1000 person-years for patients with obesity vs 6.4 per 1000 person-years in those without obesity.
Conclusions and Relevance
In this study of patients who use the Veterans Health Administration for health care, obesity moderated the association between PTSD and incident T2DM. The incidence of T2DM in patients with PTSD who are not obese is similar to the national incidence rate in the United States. These results suggest PTSD is not likely to have a causal association with incident T2DM. Future research is needed to determine if PTSD remission can lead to weight loss and reduced T2DM incidence.
Introduction
Posttraumatic stress disorder (PTSD) is associated with an increased risk of type 2 diabetes mellitus (T2DM).1,2,3,4,5,6 The condition is associated with risk factors for T2DM, such as poor diet, lack of exercise, alcohol abuse, and obesity. These risk factors may interact with hypothalamic-pituitary-adrenal changes to increase risk of T2DM. Alternatively, hypothalamic-pituitary-adrenal dysfunction alone may be in the causal pathway from PTSD to T2DM,7,8 or a common biological mechanism (such as genetic vulnerability) could underlie this association.9
There is no conclusive evidence whether PTSD directly causes T2DM, or whether poor health, such as alcohol use disorder, obesity, or sedentary lifestyle, are either in the causal pathway or moderate the association from PTSD to T2DM.8,9 To help tease apart the multifactorial pathways from PTSD to T2DM, we focus on the role of obesity, which is twice as common in patients with PTSD compared with those without PTSD10,11,12 and accounts for up to 44% of the T2DM burden in the general population.13
In studies of civilian and veteran populations, the risk of self-reported incident diabetes was markedly reduced and no longer significantly associated with PTSD after adjusting for psychiatric comorbidity, body mass index (calculated as weight in kilograms divided by height in meters squared), hypertension, alcohol consumption, physical activity, and cardiovascular disease.4,6 In contrast, over 22 years, the Nurses Health Study5 observed that body mass index accounted for 14% of the association between PTSD and incident diabetes, but even after adjusting for body mass index and other diabetes risk factors, those with PTSD were 30% more likely to report being diagnosed as having T2DM than those without trauma exposure. It is unknown whether PTSD is directly associated with incident T2DM. It is not possible to determine the role of obesity in the association between PTSD and incident T2DM from existing studies, which have either measured body mass index (not obesity) or have simultaneously adjusted for obesity in combination with other T2DM risk factors.
To determine if PTSD remains associated with incident T2DM independent of obesity, we used a large medical record database that permits measuring relevant confounding factors and potential moderators over many years of observation. The current study is designed to (1) determine if the association between PTSD and incident T2DM remains after first controlling for obesity and further adjusting for other potential confounders, (2) determine if patients with PTSD and obesity have a greater risk of incident T2DM compared with patients with PTSD alone, and (3) determine if obesity and PTSD have a combined association with incident T2DM.
Methods
This retrospective cohort study used deidentified Veterans Health Administration (VHA) patient medical record data from fiscal years (FY) 2008 to 2015 (October 1, 2007, to September 30, 2015). Data elements included International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes, vital signs, laboratory results, medications, demographic data, and the type of clinic encounter (eg, primary care, mental health clinic, or PTSD psychotherapy).
The study was approved by the institutional review boards of participating institutions. A waiver of informed consent was obtained because this study used deidentified data.
We initially identified and randomly selected 5916 individuals with PTSD and 5940 control patients without PTSD who were aged 18 to 70 years and had at least 2 visits between FY2008 and FY2012 to 1 of 5 VHA PTSD specialty mental health clinics distributed across the United States. Patients were defined as having PTSD if they had ICD-9 code 309.81 on 2 outpatient visits within a 12-month period or 1 inpatient stay. Requiring 2 diagnoses for PTSD results in good positive predictive value (82%) when compared with a gold standard PTSD Checklist score of 50 or greater.14 This algorithm has good agreement (79.4%) with lifetime diagnoses derived from the Structured Clinical Interview for DSM-IV.15 Control patients without PTSD had no occurrence of a PTSD diagnosis code in FY2008 to FY2012.
For patients with PTSD, the index date was the second visit with a PTSD diagnosis (or inpatient discharge date). For controls, the index date was the date of the second visit to any of the 5 VHA medical centers. From the initial cohort, we selected the 2959 patients without a PTSD diagnosis and 4075 patients with a PTSD diagnosis whose index date occurred in FY2009 to FY2012. The observation period continued until September 30, 2015, which allowed all patients a minimum of 3 years of follow-up time to develop incident T2DM. Patients with and without PTSD whose index date was before 2009 were removed because they did not have a full 1 year of this washout period.
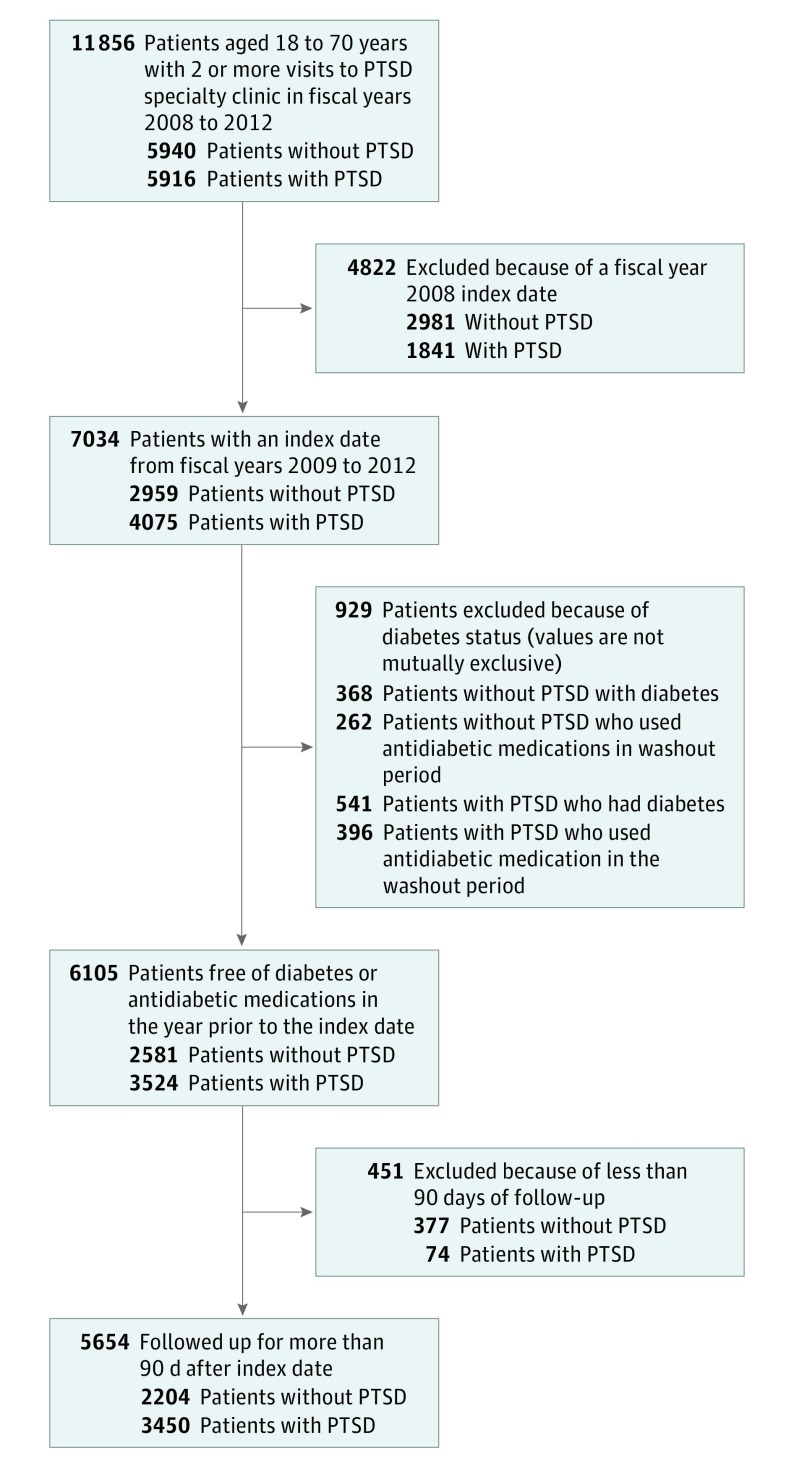
Because we are interested in incident T2DM, we excluded patients who had a diagnosis indicating diabetes (ICD-9 codes 250.x, 357.2, 362.0x, or 366.41; n = 909) or those receiving an antidiabetic medication (n = 658) in the 1-year washout period. In the washout period, we relaxed our diagnostic criteria for T2DM such that patients with a single ICD-9 code for any diabetes (type 1 or 2) were removed. This method was appropriate for maximizing accurate removal of existing cases, while the requirement for 2 ICD-9 codes during follow-up was designed to maximize true positive cases of type 2 diabetes. To allow time for exposures to feasibly contribute to incident T2DM, we excluded patients with 90 days or less of follow-up after the index date. This resulted in a final analytic sample of 3450 patients with PTSD and 2204 patients without PTSD. The Figure illustrates the inclusion and exclusion criteria leading to the analytic sample.
Figure. Study Inclusion Criteria.
PTSD indicates posttraumatic stress disorder.
Outcome Variable
We followed the method used by Miller et al16 for measuring the prevalence of diabetes in the VHA to identify incident T2DM. We defined T2DM by the presence of 2 or more ICD-9 codes (250.x0, 250.x2, 357.2, 362.0x, or 366.41) within a 24-month period. The date of the first code was considered the date of T2DM onset.
Exposure Variables
For our first objective, the exposure was PTSD status at the index date. The presence of PTSD was modeled as a time-invariant variable. For our second objective, obesity among patients with PTSD and patients without PTSD was the main exposure. Obesity was defined as a body mass index of 30 or more or an ICD-9 code for obesity (278.00 or 278.01). Obesity was treated as time dependent, meaning patients could contribute to both nonobese and obese follow-up time.
Covariates
Except for PTSD psychotherapy, which should occur after the PTSD index date, covariates could occur anytime during the observation period prior to study end date. Unless otherwise noted, covariates were treated as time-dependent.
We controlled for time-invariant demographic variables, which included age, sex, race/ethnicity (categorized as white, black, other, or missing data), marital status (married, not married, or missing data) and having both VHA and non-VHA health insurance. We included a missing category for demographic covariates to preserve sample size. To control for detection bias, we adjusted for the volume of primary care health services use by computing the number of primary care clinic visits in the entire VHA system. The distribution of the mean number of visits per month was used to define the top 25th percentile as high use vs all other use levels.
We adjusted for comorbid psychiatric disorders including depression, any anxiety disorder, alcohol abuse or dependence, and illicit drug abuse or dependence that may confound the association between PTSD and T2DM. Depression was defined by 2 outpatient codes within a 12-month period or a single inpatient diagnosis of ICD-9 codes 296.2x, 296.3x, or 311.17 We used the same algorithm to classify patients as having panic disorder (ICD-9 code 300.01), obsessive-compulsive disorder (300.3), social phobia (300.23), generalized anxiety disorder (300.02), or anxiety not otherwise specified (300.00). We created a composite variable termed any anxiety disorder defined as having any of these disorders. We also adjusted for prescriptions for any antidepressant and atypical antipsychotic medications. Alcohol abuse or dependence was classified by ICD-9 codes 303.9x or 305.0x. Any illicit drug abuse or dependence was defined by an ICD-9 code for any of the following: sedative (304.1x or 305.4x), cocaine (304.2x or 305.6x), cannabis (304.3x or 305.2x), amphetamine (304.4x or 305.7x), hallucinogens (304.5x or 305.3x), other (304.6x, or 305.9x), opioid (304.0x or 305.5x), opioid with other substance use disorder (304.7x), other substance use disorder excluding opioids (304.8x), and unspecified drug use (304.9x).
Comorbid health conditions and health behaviors common in patients with PTSD included sleep disorders, hypertension, hyperlipidemia, obesity, and current smoking.18 Sleep disorders included ICD-9 codes 307.4x, 327.x, 780.5x, and 333.94. Current smoking was identified from health factors data or by an ICD-9 code for nicotine dependence (V15.82 or 305.1). In addition, ICD-9 codes were used to define hypertension (401.x) and hyperlipidemia (272.0, 272.1, 272.2, or 272.4).
Psychotherapy for PTSD was measured by visits to clinics that specialize in PTSD psychotherapy. Psychotherapy was categorized into 0 visits, 1 to 8 visits, and 9 or more visits in any 15 week period, with the last of these representing minimally adequate psychotherapy duration. We did not adjust for psychotherapy for the first objective because the comparison group was patients with PTSD vs patients without PTSD, with the second group not receiving PTSD psychotherapy. We adjusted for PTSD psychotherapy when comparing the combined association of obesity and PTSD on the risk of developing T2DM.
Analytic Approach
Analyses were performed with SAS version 9.4 (SAS Institute) at an α level of .05. Data analysis was completed from February 2018 to May 2018.
Bivariate analyses estimated the association between covariates and PTSD or obesity among those with and without PTSD using χ2 tests for categorical variables or independent samples t tests for continuous variables. Bivariate relationships with marital status included cell sizes with less than 5 patients (eg, missing values); thus, exact P values were computed. Unadjusted cumulative incidence percent and incidence rate (per 1000 person-years) were calculated and compared by PTSD status and among obesity status in groups with and without PTSD using χ2 tests and Poisson regression models. Because older age is positively associated with T2DM,19 we calculated age-adjusted cumulative incidence percents and rates using Poisson regression models.
Cox proportional hazard models were computed to obtain hazard ratios and 95% CIs. For the first objective, models were computed before and after adding obesity to an age-adjusted model to assess the association of PTSD with incident T2DM (model 1 and model 2, respectively). The model was further expanded by adding psychiatric disorders and psychotropic medications (model 3), physical conditions (model 4), smoking status (model 5), and demographic factors (model 6). For the second objective, Cox models were stratified by PTSD status and crude and fully adjusted models for the association of obesity with incident T2DM were computed. The proportional hazard assumption was tested by examining a time-dependent interaction term of PTSD (first objective) or obesity stratified by PTSD (second objective) and log(follow-up time), where a significant test (defined as P < .05) indicates assumption violation and different hazard trends over time. The assumption was met for all outcome models. Follow-up time was measured as days since index date to study end date, which was either the date of T2DM diagnosis or the last clinic encounter, if no T2DM diagnosis occurred.
Results
Overall, the sample (N = 5654) had a mean (SD) age of 44.7 (14.4) years; 4843 participants were men (85.7%), 3664 were white (64.8%), and 2481 were married (43.9%). Among the 2204 patients without PTSD, the mean (SD) age was 47.7 (14.3) years; 1860 were men (84.4%), 1426 were white (64.7%), and 956 were married (43.4%). Among 3450 patients with PTSD, the mean (SD) age was 42.8 (14.2) years, and 2983 were male (86.5%), 2238 were white (64.9%), and 1525 were married (44.2%).
Several conditions were more prevalent among patients with PTSD than in those without PTSD (Table 1): male sex (patients with PTSD: 2983 of 3450 [86.5%]; patients without PTSD: 1860 of 2204 [84.4%]; P = .03), black race (patients with PTSD: 852 [24.7%]; patients without PTSD: 372 [16.9%]; P < .001), and not being married (patients with PTSD: 1921 [55.7%]; patients without PTSD: 1077 [48.9%]; P < .001). Patients with PTSD were less likely to have missing race data (patients with PTSD: 133 [3.9%]; patients without PTSD: 171 [7.8%]; P < .001) and missing marital status data (patients with PTSD: fewer than 5 [less than 0.1%]; patients without PTSD: 171 [7.8%]; P < .001). Access to VHA insurance only was less prevalent in those with PTSD (patients with PTSD: 2210 [64.1%]; patients without PTSD: 1502 [68.2%]; P = .002), and high primary care use was more common among patients with PTSD (patients with PTSD: 1034 [30.0%]; patients without PTSD: 379 [17.2%]; P < .001). Patients with PTSD more often received psychiatric diagnoses than those without PTSD, including depression (patients with PTSD: 2525 [73.2%]; patients without PTSD: 433 [19.7%]; P < .001) and other anxiety disorders (patients with PTSD: 1142 [33.1%]; patients without PTSD: 272 [12.3%]; P < .001). They also more often received diagnoses of sleep disorder (patients with PTSD: 2023 [58.6%]; patients without PTSD: 604 [27.4%]; P < .001), alcohol abuse/dependence (patients with PTSD: 1564 [45.3%]; patients without PTSD: 365 [16.6%]; P < .001), and drug abuse/dependence (patients with PTSD: 1074 [31.1%]; patients without PTSD: 236 [10.7%]; P < .001). Patients with PTSD were more likely to receive prescriptions for psychotropic medications. Specifically, 3087 patients (89.5%) with PTSD and 761 patients (34.5%) without PTSD (P < .001) received an antidepressant, and 1139 patients (33.0%) with PTSD and 125 patients (5.7%) without PTSD (P < .001) received an atypical antipsychotic. Hypertension was significantly more prevalent in patients with PTSD vs those without PTSD (patients with PTSD: 1651 [47.9%]; patients without PTSD: 965 [43.8%]; P = .003), as was hyperlipidemia (patients with PTSD: 1704 [49.4%]; patients without PTSD: 941 [42.7%]; P < .001), obesity (patients with PTSD: 2039 [59.1%]; patients without PTSD: 987 [44.8%]; P < .001), and smoking (patients with PTSD: 1967 [57.0%]; patients without PTSD: 917 [41.6%]; P < .001).
Table 1. Sample Characteristics of the Overall Cohort and PTSD and Control Subgroups of Veterans Aged 18 to 70 Years, Who Were Free of Diabetes at Index (N = 5654).
| Variable | No. (%) | P Value | ||
|---|---|---|---|---|
| Overall (N = 5654) | Patients Without PTSD (n = 2204) | Patients With PTSD (n = 3450) | ||
| Age, mean (SD), y | 44.7 (14.4) | 47.7 (14.3) | 42.8 (14.2) | <.001 |
| Male | 4843 (85.7) | 1860 (84.4) | 2983 (86.5) | .03 |
| Race/ethnicity | ||||
| White | 3664 (64.8) | 1426 (64.7) | 2238 (64.9) | <.001 |
| Black | 1224 (21.7) | 372 (16.9) | 852 (24.7) | |
| Other | 352 (6.2) | 125 (5.7) | 227 (6.6) | |
| Missing | 414 (7.3) | 281 (12.8) | 133 (3.9) | |
| Marital status | ||||
| Not married | 2998 (53.0) | 1077 (48.9) | 1921 (55.7) | <.001 |
| Married | 2481 (43.9) | 956 (43.4) | 1525 (44.2) | |
| Missing | 175 (3.1) | 171 (7.8) | <5 (<0.1)a | |
| VHA-only insurance | 3712 (65.7) | 1502 (68.2) | 2210 (64.1) | .002 |
| High primary HCU | 1413 (25.0) | 379 (17.2) | 1034 (30.0) | <.001 |
| Psychiatric conditions and psychotropic medicationsb | ||||
| Depression | 2958 (52.3) | 433 (19.7) | 2525 (73.2) | <.001 |
| Other anxiety disorderc | 1414 (25.0) | 272 (12.3) | 1142 (33.1) | <.001 |
| Sleep disorder | 2627 (46.5) | 604 (27.4) | 2023 (58.6) | <.001 |
| Alcohol abuse or dependence | 1929 (34.1) | 365 (16.6) | 1564 (45.3) | <.001 |
| Drug abuse or dependence | 1310 (23.2) | 236 (10.7) | 1074 (31.1) | <.001 |
| Antidepressant use | 3848 (68.1) | 761 (34.5) | 3087 (89.5) | <.001 |
| Atypical antipsychotic use | 1264 (22.4) | 125 (5.7) | 1139 (33.0) | <.001 |
| Physical conditions | ||||
| Hypertension | 2616 (46.3) | 965 (43.8) | 1651 (47.9) | .003 |
| Hyperlipidemia | 2645 (46.8) | 941 (42.7) | 1704 (49.4) | <.001 |
| Obesityd | 3026 (53.5) | 987 (44.8) | 2039 (59.1) | <.001 |
| Smokinge | 2884 (51.0) | 917 (41.6) | 1967 (57.0) | <.001 |
Abbreviations: ICM-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; HCU, health care use; PTSD, posttraumatic stress disorder; VHA, Veterans Health Administration.
Not included in calculations because of small number in cell.
Comorbidities occur anytime in follow-up (fiscal years 2009 to 2015), prior to either diabetes onset or last visit date.
A composite of panic disorder, obsessive-compulsive disorder, social phobia, generalized anxiety disorder, and anxiety not otherwise specified.
Defined by a body mass index (calculated as weight in kilograms divided by height in meters squared) of 30 or more or ICD-9-CM code.
Current smoker per health factor records or ICD-9-CM code.
The cumulative incidence percent and incidence rates of T2DM by PTSD status are shown in eTable 1 in the Supplement. Prior to adjusting for age, the T2DM cumulative incidence percent and incidence rates were similar in patients with PTSD (252 [7.3%]) and without PTSD (141 [6.4%]; P = .19). After adjusting for age, the cumulative incidence of T2DM was significantly higher in those with PTSD vs those without (patients with PTSD: 6.6%; patients without PTSD: 4.7%; P = .002); the same pattern occurred with respect to incidence rate (patients with PTSD: 15.2 per 1000 person-years; patients without PTSD: 11.4 per 1000 person-years; P = .01).
Results from Cox proportional hazard models estimating the association between PTSD and incident T2DM are shown in Table 2. After adjusting for age in model 2, PTSD was associated with a 33% increased likelihood of incident T2DM (hazard ratio [HR], 1.33; 95% CI, 1.08-1.64; P = .01). After adding obesity (model 3), the association between PTSD and incident T2DM was markedly reduced and no longer statistically significant (HR, 1.16; 95% CI, 0.94-1.43; P = .18). A diagnosis of PTSD remained unassociated with incident T2DM after expanding the model by adjusting for psychiatric, sleep disorders, and psychotropic medications (model 4); hypertension, hyperlipidemia, and smoking (model 5); and demographic and health care use variables (model 6). In the full model (model 6), increased risk of incident T2DM was significantly associated with age (HR, 1.03; 95% CI, 1.02-1.04; P < .001), obesity (HR, 2.68; 95% CI, 2.10-3.43; P < .001), sleep disorder (HR, 1.25; 95% CI, 1.01-1.56; P = .045), atypical antipsychotics (HR, 1.44; 95% CI, 1.12-1.85; P = .004), hypertension (HR, 1.66; 95% CI, 1.28-2.14; P < .001), black race (HR, 1.64; 95% CI, 1.31-2.06; P < .001), and high primary care use (HR, 1.91; 95% CI, 1.55-2.37; P < .001).
Table 2. Results From Cox Proportional Hazards Models Estimating the Association of Posttraumatic Stress Disorder (PTSD) and Patient Characteristics With Incident Type 2 Diabetes in Patients With and Without PTSD (N = 5654)a.
| Characteristic | Hazard Ratio (95% CI) | |||||
|---|---|---|---|---|---|---|
| Model 1 (Crude) | Model 2 (Age-Adjusted) | Model 3 (Obesity-Adjusted) | Model 4 (Psychiatric Diagnosis–Adjusted) | Model 5 (Cardiometabolic Condition–Adjusted) | Model 6 (Demographic Factor–Adjusted) | |
| PTSD | 1.07 (0.87-1.32) | 1.33 (1.08-1.64) | 1.16 (0.94-1.43) | 0.91 (0.69-1.19) | 0.91 (0.70-1.20) | 0.84 (0.64-1.10) |
| Age, y | NA | 1.04 (1.03-1.05) | 1.04 (1.03-1.05) | 1.04 (1.03-1.05) | 1.03 (1.02-1.04) | 1.03 (1.02-1.04) |
| Obesityb | NA | NA | 3.45 (2.72-4.38) | 3.18 (2.50-4.05) | 2.83 (2.21-3.61) | 2.68 (2.10-3.43) |
| Psychiatric conditions and psychotrophic medications | ||||||
| Depression | NA | NA | NA | 0.91 (0.70-1.17) | 0.90 (0.70-1.16) | 0.89 (0.69-1.14) |
| Other anxietyc | NA | NA | NA | 1.13 (0.89-1.44) | 1.11 (0.87-1.41) | 1.11 (0.87-1.42) |
| Sleep disorder | NA | NA | NA | 1.38 (1.12-1.71) | 1.30 (1.05-1.61) | 1.25 (1.01-1.56) |
| Alcohol abuse/dependence | NA | NA | NA | 0.97 (0.75-1.25) | 0.95 (0.73-1.23) | 0.94 (0.72-1.22) |
| Drug abuse/dependence | NA | NA | NA | 0.86 (0.64-1.16) | 0.83 (0.61-1.15) | 0.74 (0.55-1.06) |
| Antidepressant use | NA | NA | NA | 1.22 (0.91-1.64) | 1.16 (0.87-1.56) | 1.10 (0.82-1.47) |
| Atypical antipsychotic use | NA | NA | NA | 1.54 (1.20-1.98) | 1.49 (1.16-1.92) | 1.44 (1.12-1.85) |
| Physical conditions | ||||||
| Hypertension | NA | NA | NA | NA | 1.89 (1.47-2.44) | 1.66 (1.28-2.14) |
| Hyperlipidemia | NA | NA | NA | NA | 1.15 (0.91-1.44) | 1.13 (0.90-1.42) |
| Smokingd | NA | NA | NA | NA | 1.07 (0.86-1.32) | 1.06 (0.85-1.31) |
| Demographic factors | ||||||
| Male | NA | NA | NA | NA | NA | 1.43 (0.98-2.10) |
| Race/ethnicity | ||||||
| White | NA | NA | NA | NA | NA | 1 [Reference] |
| Black | NA | NA | NA | NA | NA | 1.64 (1.31-2.06) |
| Other | NA | NA | NA | NA | NA | 1.18 (0.76-1.84) |
| Marital status | NA | NA | NA | NA | NA | |
| Not married | NA | NA | NA | NA | NA | 1 [Reference] |
| Married | NA | NA | NA | NA | NA | 0.98 (0.79-1.21) |
| VHA-only insurance | NA | NA | NA | NA | NA | 0.99 (0.80-1.22) |
| High primary HCU | NA | NA | NA | NA | NA | 1.91 (1.55-2.37) |
Abbreviations: HCU, health care use; ICM-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; NA, not applicable; VHA, Veterans Health Administration.
Test of proportional hazard, P = .20.
Defined by a body mass index of 30 or more or an ICD-9-CM code for obesity.
A composite of panic disorder, obsessive-compulsive disorder, social phobia, generalized anxiety disorder, and anxiety not otherwise specified.
Current smoker per health factor records or ICD-9-CM code.
The distribution of covariates by obesity status for patients without PTSD and with PTSD are shown in Table 3. Among patients without PTSD, older age was significantly associated with having obesity (patients without obesity without PTSD: mean [SD] age, 46.3 [14.9] years; patients with obesity without PTSD: 49.5 [13.4] years; P < .001). Obesity was slightly more prevalent among white patients (patients with obesity without PTSD: 692 of 987 [70.1%]; patients without obesity without PTSD: 734 of 1217 [60.3%]; P < .001) and black patients (patients with obesity without PTSD: 188 of 987 [19.1%]; patients without obesity without PTSD: 184 of 1217 [15.1%]; P < .001) than among patients in other racial/ethnic categories. Missing race was frequent among patients without PTSD who did not have obesity (patients without obesity without PTSD: 224 of 1217 [18.4%]; patients with obesity without PTSD: 57 of 987 [5.8%]; P < .001). Being married was much more common among patients with obesity (patients with obesity without PTSD: 486 of 987 [49.2%]; patients without obesity without PTSD: 470 of 1217 [38.6%]; P < .001), as was high primary care health services use (patients with obesity without PTSD: 224 of 987 [22.7%]; patients without obesity without PTSD: 155 of 1217 [12.7%]; P < .001). Patients who were not obese more often had VHA health coverage only (patients with obesity without PTSD: 626 of 987 [63.4%]; patients without obesity without PTSD: 876 of 1217 [72.0%]; P < .001). Several health conditions were also more prevalent among those without PTSD who had obesity: comorbid depression (patients with obesity without PTSD: 233 of 987 [23.6%]; patients without obesity without PTSD: 200 of 1217 [16.4%]; P < .001), other anxiety disorders (patients with obesity without PTSD: 138 of 987 [14.0%]; patients without obesity without PTSD: 134 of 1217 [11.0%]; P < .001), sleep disorder (patients with obesity without PTSD: 388 of 987 [39.3%]; patients without obesity without PTSD: 216 of 1217 [17.8%]; P < .001), antidepressant medication use (patients with obesity without PTSD: 397 of 987 [40.2%]; patients without obesity without PTSD: 364 of 1217 [29.9%]; P < .001), atypical antipsychotic medication use (patients with obesity without PTSD: 69 of 987 [7.0%]; patients without obesity without PTSD: 56 of 1217 [4.6%]; P < .001), hypertension (patients with obesity without PTSD: 590 of 987 [59.8%]; patients without obesity without PTSD: 375 of 1217 [30.8%]; P < .001), hyperlipidemia (patients with obesity without PTSD: 564 of 987 [57.1%]; patients without obesity without PTSD: 377 of 1217 [31.0%]; P < .001), and current smoking (patients with obesity without PTSD: 460 of 987 [46.6%]; patients without obesity without PTSD: 457 of 1217 [37.6%]; P < .001).
Table 3. Sample Characteristics Stratified by Posttraumatic Stress Disorder (PTSD) and Obesity, Among Patients Aged 18 to 70 Years Who Were Free of Diabetes at Index (N = 5654).
| Variable | No (%) | |||||
|---|---|---|---|---|---|---|
| Patients Without PTSD (n = 2204) | Patients With PTSD (n = 3450) | |||||
| Without Obesity (n = 1217) | With Obesity (n = 987) | P Value | Without Obesity (n = 1411) | With Obesity (n = 2039) | P Value | |
| Age, mean (SD), y | 46.3 (14.9) | 49.5 (13.4) | <.001 | 42.2 (14.8) | 43.2 (13.7) | .04 |
| Demographic factors | ||||||
| Male | 964 (79.2) | 896 (90.8) | <.001 | 1223 (86.7) | 1760 (86.3) | .76 |
| Race/ethnicity | ||||||
| White | 734 (60.3) | 692 (70.1) | <.001 | 904 (64.1) | 1334 (65.4) | .03 |
| Black | 184 (15.1) | 188 (19.1) | 334 (23.7) | 518 (25.4) | ||
| Other | 75 (6.2) | 50 (5.1) | 111 (7.9) | 116 (5.7) | ||
| Missing | 224 (18.4) | 57 (5.8) | 62 (4.4) | 71 (3.5) | ||
| Marital status | ||||||
| Not married | 588 (48.3) | 489 (49.5) | <.001 | 856 (60.7) | 1065 (52.2) | <.001 |
| Married | 470 (38.6) | 486 (49.2) | 553 (39.2) | 972 (47.7) | ||
| Missing | 159 (13.1) | 12 (1.2) | <5 (<0.4)a | <5 (<0.3)a | ||
| VHA-only insurance | 876 (72.0) | 626 (63.4) | <.001 | 955 (67.7) | 1255 (61.6) | <.001 |
| High primary HCU | 155 (12.7) | 224 (22.7) | <.001 | 327 (23.2) | 707 (34.7) | <.001 |
| Psychiatric conditions and psychotropic medicationsb | ||||||
| Depression | 200 (16.4) | 233 (23.6) | <.001 | 998 (70.7) | 1527 (74.9) | .01 |
| Other anxietyc | 134 (11.0) | 138 (14.0) | .04 | 454 (32.2) | 688 (33.7) | .34 |
| Sleep disorder | 216 (17.8) | 388 (39.3) | <.001 | 690 (48.9) | 1333 (65.4) | <.001 |
| Alcohol abuse/dependence | 211 (17.3) | 154 (15.6) | .28 | 645 (45.7) | 919 (45.1) | .71 |
| Drug abuse/dependence | 132 (10.9) | 104 (10.5) | .82 | 436 (30.9) | 638 (31.3) | .81 |
| Antidepressant use | 364 (29.9) | 397 (40.2) | <.001 | 1214 (86.0) | 1873 (91.9) | <.001 |
| Atypical antipsychotic use | 56 (4.6) | 69 (7.0) | .02 | 406 (28.8) | 733 (36.0) | <.001 |
| Physical Conditions | ||||||
| Hypertension | 375 (30.8) | 590 (59.8) | <.001 | 522 (37.0) | 1129 (55.4) | <.001 |
| Hyperlipidemia | 377 (31.0) | 564 (57.1) | <.001 | 548 (38.8) | 1156 (56.7) | <.001 |
| Smokingd | 457 (37.6) | 460 (46.6) | <.001 | 855 (60.6) | 1112 (54.5) | <.001 |
| PTSD psychotherapy visits per 15 wks | ||||||
| 0 | NA | NA | NA | 431 (30.6) | 600 (29.4) | .47 |
| 1-8 | NA | NA | 413 (29.3) | 577 (28.3) | ||
| ≥9 | NA | NA | 567 (40.2) | 862 (42.3) | ||
Abbreviations: HCU, health care use; ICM-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; NA, not applicable; VHA, Veterans Health Administration.
Not included in calculations because of small number in cell.
Comorbidities occur anytime in follow-up (fiscal years 2009 to 2015), prior to either diabetes onset or the last visit date.
A composite of panic disorder, obsessive-compulsive disorder, social phobia, generalized anxiety disorder, and anxiety not otherwise specified.
Current smoker per health factors records or ICD-9-CM code.
Among patients with PTSD, those with obesity were significantly older (patients without obesity with PTSD: mean [SD] age, 42.2 [14.8] years; patients with obesity with PTSD: 43.2 [13.7] years; P < .04), white race (patients with obesity with PTSD: 1334 of 2039 [65.4%]; patients without obesity with PTSD: 904 of 1411 [64.1%]; P = .03), and black race (patients with obesity with PTSD: 518 of 2039 [25.4%]; patients without obesity with PTSD: 334 of 1411 [23.7%]; P = .03). Among patients with obesity, being married (patients with obesity with PTSD: 972 of 2309 [47.7%]; patients without obesity with PTSD: 553 of 1411 [39.2%]; P < .001) and high primary care health services use (patients with obesity with PTSD: 707 of 2309 [34.7%]; patients with obesity with PTSD: 327 of 1411 [23.2%]; P < .001) were significantly more common, while access to VHA health insurance only was more prevalent among patients with PTSD who were not obese (patients with obesity with PTSD: 1255 of 2309 [61.6%]; patients with obesity with PTSD: 955 of 1411 [67.7%]; P < .001). Among patients with PTSD with obesity vs patients with PTSD without obesity, analysis showed higher prevalences of depression (patients with obesity with PTSD: 1527 of 2309 [74.9%]; patients with obesity with PTSD: 998 of 1411 [70.7%]; P < .001), sleep disorder (patients with obesity with PTSD: 1333 of 2309 [65.4%]; patients with obesity with PTSD: 690 of 1411 [48.9%]; P < .001), antidepressant medication use (patients with obesity with PTSD: 1873 of 2309 [91.9%]; patients with obesity with PTSD: 1214 of 1411 [86.0%]; P < .001), atypical antipsychotic medication use (patients with obesity with PTSD: 733 of 2309 [36.0%]; patients with obesity with PTSD: 406 of 1411 [28.8%]; P < .001), hypertension (patients with obesity with PTSD: 1129 of 2309 [55.4%]; patients with obesity with PTSD: 522 of 1411 [37.0%]; P < .001), and hyperlipidemia (patients with obesity with PTSD: 1156 of 2309 [56.7%]; patients with obesity with PTSD: 548 of 1411 [38.8%]; P < .001). Last, current smoking was more prevalent among patients with PTSD who were not obese (patients with obesity with PTSD: 1112 of 2309 [54.5%]; patients with obesity with PTSD: 855 of 1411 [60.6%]; P < .001).
Among patients with and without PTSD, we observed the T2DM cumulative incidence percent and incidence rate were much higher in patients with obesity than those without, both before and after adjusting for age (eTable 2 in the Supplement). Among patients with PTSD, the age-adjusted T2DM incidence rate was 21.0 per 1000 person-years for patients with obesity compared with 5.8 per 1000 person-years for patients without obesity (P < .001). Among patients without PTSD, the age-adjusted T2DM incidence rate was 21.2 per 1000 person-years for patients with obesity and 6.4 per 1000 person-years for patients without obesity (P < .001).
Results for Cox proportional hazard models estimating the association between obesity and incident T2DM stratified by patients with and without PTSD are shown in Table 4. In patients without PTSD and in those with PTSD, obesity was significantly associated with incident T2DM and the magnitude of association was similar in patients without PTSD (HR, 3.75 [95% CI, 2.60-5.40]; P < .001) and with PTSD (HR, 3.66 [95% CI, 2.67-5.02]; P < .001). The magnitude of association was attenuated after adjusting for all covariates but remained similar in those without PTSD (HR, 2.73 [95% CI, 1.86-4.00]; P < .001) and those with PTSD (HR, 2.72 [95% CI, 1.97-3.77]; P < .001). In patients without PTSD, older age (HR, 1.04 [95% CI, 1.02-1.06]; P < .001), hypertension (HR, 1.68 [95% CI, 1.11-2.54]; P = .01), male sex (HR, 3.76 [95% CI, 1.17-12.05]; P = .03), black race (HR, 1.78 [95% CI, 1.18-2.68]; P = .006), being married (HR, 1.45 [95% CI, 1.01-2.07]; P = .04), and high primary care use (HR, 2.14 [95% CI, 1.47-3.10]; P < .001) were positively associated with incident T2DM. In patients with PTSD, older age (HR, 1.03 [95% CI, 1.01-1.04]; P < .001), sleep disorder (HR, 1.39 [95% CI, 1.06-1.83]; P = .02), atypical antipsychotic medications (HR, 1.44 [95% CI, 1.10-1.89]; P = .01), hypertension (HR, 1.69 [95% CI, 1.23-2.34]; P = .001), hyperlipidemia (HR, 1.42 [95% CI, 1.06-1.90]; P = .02), black race (HR, 1.60 [95% CI, 1.23-2.10]; P < .001), and high primary care use (HR, 1.83 [95% CI, 1.41-2.38]; P < .001) were all significantly associated with increased risk of incident T2DM while drug abuse/dependence diagnosis was significantly associated with a lower risk of incident T2DM.
Table 4. Results From Cox proportional Hazards Models Estimating the Association of Obesity With Incident Type 2 Diabetes, Stratified by Posttraumatic Stress Disorder Status (PTSD) (N = 5654)a.
| Characteristic | Hazard Ratio (95% CI) | |
|---|---|---|
| Patients Without PTSD (n = 2204) | Patients With PTSD (n = 3450) | |
| Obesity | ||
| Crude | 3.75 (2.60-5.40) | 3.66 (2.67-5.02) |
| Adjusted | 2.73 (1.86-4.00) | 2.72 (1.97-3.77) |
| Age, y | 1.04 (1.02-1.06) | 1.03 (1.01-1.04) |
| Psychiatric conditions and psychotropic medications | ||
| Depression | 1.03 (0.60-1.76) | 0.83 (0.62-1.12) |
| Other anxiety disorderb | 1.13 (0.64-1.97) | 1.08 (0.82-1.43) |
| Sleep disorder | 0.99 (0.67-1.48) | 1.39 (1.06-1.83) |
| Alcohol abuse/ dependence | 0.89 (0.50-1.57) | 0.94 (0.70-1.27) |
| Drug abuse/ dependence | 0.87 (0.43-1.75) | 0.69 (0.49-0.97) |
| Antidepressant use | 1.12 (0.72-1.75) | 1.21 (0.76-1.92) |
| Atypical antipsychotic use | 1.19 (0.55-2.56) | 1.44 (1.10-1.89) |
| Physical conditions | ||
| Hypertension | 1.68 (1.11-2.54) | 1.69 (1.23-2.34) |
| Hyperlipidemia | 0.74 (0.51-1.07) | 1.42 (1.06-1.90) |
| Smokingc | 1.11 (0.78-1.59) | 1.06 (0.80-1.39) |
| PTSD psychotherapy visits per 15 wks | ||
| 0 | NA | 1 [Reference] |
| 1-8 | NA | 0.84 (0.59-1.19) |
| ≥9 | NA | 1.11 (0.82-1.49) |
| Demographic factors | ||
| Male | 3.76 (1.17-12.05) | 1.22 (0.80-1.85) |
| Race/ethnicity | ||
| White | 1 [Reference] | 1 [Reference] |
| Black | 1.78 (1.18-2.68) | 1.60 (1.23-2.10) |
| Other | 1.70 (0.84-3.45) | 1.01 (0.57-1.79) |
| Marital status | ||
| Not married | 1 [Reference] | 1 [Reference] |
| Married | 1.45 (1.01-2.07) | 0.79 (0.60-1.04) |
| VHA-only insurance | 0.99 (0.69-1.42) | 0.99 (0.76-1.30) |
| High primary HCU | 2.14 (1.47-3.10) | 1.83 (1.41-2.38) |
Abbreviations: HCU, healthcare use; ICM-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; NA, not applicable; T2DM, type 2 diabetes mellitus; VHA, Veterans Health Administration.
Test of proportional hazard: patients without PTSD, P = .41; patients with PTSD, P = .57.
A composite of panic disorder, obsessive compulsive disorder, social phobia, generalized anxiety disorder, and anxiety not otherwise specified.
Current smoker per health factors records or ICD-9-CM code.
Discussion
In a large cohort of VHA patients with PTSD who were free of T2DM at baseline, we observed that obesity largely accounted for the association between PTSD and incident T2DM. While age-adjusted models indicated a significant association between PTSD and incident T2DM (HR, 1.33 [95% CI, 1.08-1.64]; P = .01), after adjusting for obesity, the risk was reduced by nearly 50% (HR, 1.16 [95% CI, 0.94-1.43]; P = .18). In fully adjusted models, PTSD had no association with incident T2DM and obesity remained the strongest predictor of new onset T2DM (HR, 2.68 [95% CI, 2.10-3.43]; P < .001). To our knowledge, these results are the first to focus on the contribution of obesity by itself on the association between PTSD and T2DM.
The incidence of T2DM was nearly identical in patients with and without obesity in both those with PTSD and without PTSD. From survival models, we observed that before and after adjusting for covariates, the association between obesity and incident T2DM was similar in patients with and without PTSD. In adjusted analysis, patients without PTSD who had obesity were 2.73 times more likely to develop T2DM, and obesity was associated with 2.72 times increased risk of T2DM in those with PTSD. The age-adjusted incidence rate of T2DM in patients without PTSD or obesity (6.4 per 1000 person-years) was similar to that observed in patients with PTSD who did not have obesity (5.8 per 1000 person-years). This is nearly equal to the unadjusted incidence rate of 6.7 per 1000 person-years for adults living in the United States in 2015.19 Overall, we did not observe evidence of a combined association of PTSD and obesity with incident T2DM. In this study, it seems unlikely that PTSD has a causal association with T2DM.
These results are consistent with previous research demonstrating that psychiatric disorders,1 metabolic conditions, and demographic factors attenuate the association between PTSD and T2DM.4 However, others have found PTSD remains significantly associated with incident T2DM when adjusting for various combinations of these covariates.2,5,6
The current study advances existing research, which has relied mostly on self-reported T2DM. Our results are responsive to the call by Koenen et al9 to establish evidence for whether PTSD has a causal relationship with cardiometabolic disease. Based on the present study, reducing body mass index to within a normal range and limiting exposure to atypical antipsychotic medications in patients with PTSD, and in those without PTSD, may reduce the risk of T2DM.
While we observed obesity in 59.1% of those with PTSD compared with 44.8% of patients without PTSD, others have reported that PTSD is associated with nearly a 2-fold likelihood of becoming obese compared with patients without PTSD.10,11,12,20 Persons with PTSD were observed to be less likely to engage in weight loss programs21 and more likely to persistently gain weight.22 Johannessen and Berntsen23 observed a decrease in PTSD symptoms with weight loss. We observed no association between the number of PTSD psychotherapy visits and prevalence of obesity in patients with PTSD; however, we recognize that the number of visits is an imperfect measure of effective treatment and that additional research is warranted.
Sedentary lifestyle, poor diet, and heavy alcohol consumption are likely to lead to obesity and T2DM. Other mechanisms proposed for the PTSD–metabolic disease association include altered hypothalamic-pituitary-adrenal axis7 and chronic high levels of stress hormones that contribute to central adiposity and stress hormones that regulate appetite.24 Functional magnetic resonance imaging has revealed altered brain activity that correlates with cues to eating and consumption of high-calorie, high-fat foods.24
Limitations
Our results were obtained from a cohort of veterans who used 1 of 5 Veterans Administration Medical Centers, and it is possible that the findings may not generalize to all regions of the US or to civilians. The follow-up time for some patients was only 3 years, and the total number of new T2DM diagnoses may be conservative in this relatively young-to-middle-aged patient population. In addition, misclassification is always a limitation in retrospective cohort designs using medical record data. Our diagnostic algorithms are designed to correctly classify true cases; however, we may have misclassified patients with PTSD as noncases, which would result in conservative risk estimates.
Conclusions
Our findings suggest that PTSD does not directly lead to T2DM. Instead, obesity accounts for much of the increased risk of T2DM in patients with PTSD. Epidemiological and neurophysiological evidence has established PSTD as an independent risk factor for obesity.24 Thus, as with the general population, reducing the burden of morbidity in persons with PTSD may hinge on addressing weight.
eTable 1. Type 2 Diabetes outcome FY 2009 to 2015, cumulative incidence % and incidence rate per 1000 person-years. Overall and by PTSD case vs. control.
eTable 2. Type 2 Diabetes outcome FY 2009 to 2015, stratified by PTSD status, cumulative incidence % and incidence rate per 1000 person-years by obesity.
References
- 1.Agyemang C, Goosen S, Anujuo K, Ogedegbe G. Relationship between post-traumatic stress disorder and diabetes among 105,180 asylum seekers in the Netherlands. Eur J Public Health. 2012;22(5):658-662. doi: 10.1093/eurpub/ckr138 [DOI] [PubMed] [Google Scholar]
- 2.Boyko EJ, Jacobson IG, Smith B, et al. ; Millennium Cohort Study Team . Risk of diabetes in U.S. military service members in relation to combat deployment and mental health. Diabetes Care. 2010;33(8):1771-1777. doi: 10.2337/dc10-0296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boscarino JA. Posttraumatic stress disorder and physical illness: results from clinical and epidemiologic studies. Ann N Y Acad Sci. 2004;1032:141-153. doi: 10.1196/annals.1314.011 [DOI] [PubMed] [Google Scholar]
- 4.Vaccarino V, Goldberg J, Magruder KM, et al. . Posttraumatic stress disorder and incidence of type-2 diabetes: a prospective twin study. J Psychiatr Res. 2014;56:158-164. doi: 10.1016/j.jpsychires.2014.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts AL, Agnew-Blais JC, Spiegelman D, et al. . Posttraumatic stress disorder and incidence of type 2 diabetes mellitus in a sample of women: a 22-year longitudinal study. JAMA Psychiatry. 2015;72(3):203-210. doi: 10.1001/jamapsychiatry.2014.2632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller-Archie SA, Jordan HT, Ruff RR, et al. . Posttraumatic stress disorder and new-onset diabetes among adult survivors of the World Trade Center disaster. Prev Med. 2014;66:34-38. doi: 10.1016/j.ypmed.2014.05.016 [DOI] [PubMed] [Google Scholar]
- 7.Schnurr PP, Jankowski MK. Physical health and post-traumatic stress disorder: review and synthesis. Semin Clin Neuropsychiatry. 1999;4(4):295-304. [DOI] [PubMed] [Google Scholar]
- 8.Schnurr PP, Spiro A III. Combat exposure, posttraumatic stress disorder symptoms, and health behaviors as predictors of self-reported physical health in older veterans. J Nerv Ment Dis. 1999;187(6):353-359. doi: 10.1097/00005053-199906000-00004 [DOI] [PubMed] [Google Scholar]
- 9.Koenen KC, Sumner JA, Gilsanz P, et al. . Post-traumatic stress disorder and cardiometabolic disease: improving causal inference to inform practice. Psychol Med. 2017;47(2):209-225. doi: 10.1017/S0033291716002294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suliman S, Anthonissen L, Carr J, et al. . Posttraumatic stress disorder, overweight, and obesity: a systematic review and meta-analysis. Harv Rev Psychiatry. 2016;24(4):271-293. doi: 10.1097/HRP.0000000000000106 [DOI] [PubMed] [Google Scholar]
- 11.Bartoli F, Crocamo C, Alamia A, et al. . Posttraumatic stress disorder and risk of obesity: systematic review and meta-analysis. J Clin Psychiatry. 2015;76(10):e1253-e1261. doi: 10.4088/JCP.14r09199 [DOI] [PubMed] [Google Scholar]
- 12.van den Berk-Clark C, Secrest S, Walls J, et al. . Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occuring smoking: a systematic review and meta-analysis. Health Psychol. 2018;37(5):407-416. doi: 10.1037/hea0000593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Obesity facts and figures: fact sheet no.311. http://www.wpro.who.int/mediacentre/factsheets/obesity/en/. Published August 2014. Accessed June 21, 2018.
- 14.Gravely AA, Cutting A, Nugent S, Grill J, Carlson K, Spoont M. Validity of PTSD diagnoses in VA administrative data: comparison of VA administrative PTSD diagnoses to self-reported PTSD Checklist scores. J Rehabil Res Dev. 2011;48(1):21-30. doi: 10.1682/JRRD.2009.08.0116 [DOI] [PubMed] [Google Scholar]
- 15.Holowka DW, Marx BP, Gates MA, et al. . PTSD diagnostic validity in Veterans Affairs electronic records of Iraq and Afghanistan veterans. J Consult Clin Psychol. 2014;82(4):569-579. doi: 10.1037/a0036347 [DOI] [PubMed] [Google Scholar]
- 16.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(suppl 2):B10-B21. doi: 10.2337/diacare.27.suppl_2.B10 [DOI] [PubMed] [Google Scholar]
- 17.Frayne SM, Miller DR, Sharkansky EJ, et al. . Using administrative data to identify mental illness: what approach is best? Am J Med Qual. 2010;25(1):42-50. doi: 10.1177/1062860609346347 [DOI] [PubMed] [Google Scholar]
- 18.Coughlin SS. Post-traumatic Stress Disorder and Chronic Health Conditions. Washington, DC: American Public Health Association; 2013. doi: 10.2105/9780875530161 [DOI] [Google Scholar]
- 19.Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion Division of Diabetes Translation National diabetes statistics report: estimates of diabetes and its burden in the United States. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Published 2017. Accessed June 21, 2018.
- 20.Cohen BE, Marmar C, Ren L, Bertenthal D, Seal KH. Association of cardiovascular risk factors with mental health diagnoses in Iraq and Afghanistan war veterans using VA health care. JAMA. 2009;302(5):489-492. doi: 10.1001/jama.2009.1084 [DOI] [PubMed] [Google Scholar]
- 21.Maguen S, Hoerster KD, Littman AJ, et al. . Iraq and Afghanistan veterans with PTSD participate less in VA’s weight loss program than those without PTSD. J Affect Disord. 2016;193:289-294. doi: 10.1016/j.jad.2015.12.078 [DOI] [PubMed] [Google Scholar]
- 22.Maguen S, Madden E, Cohen B, et al. . The relationship between body mass index and mental health among Iraq and Afghanistan veterans. J Gen Intern Med. 2013;28(suppl 2):S563-S570. doi: 10.1007/s11606-013-2374-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johannessen KB, Berntsen D. Losing the symptoms: weight loss and decrease in posttraumatic stress disorder symptoms. J Clin Psychol. 2013;69(6):655-660. doi: 10.1002/jclp.21962 [DOI] [PubMed] [Google Scholar]
- 24.Farr OM, Sloan DM, Keane TM, Mantzoros CS. Stress- and PTSD-associated obesity and metabolic dysfunction: a growing problem requiring further research and novel treatments. Metabolism. 2014;63(12):1463-1468. doi: 10.1016/j.metabol.2014.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Type 2 Diabetes outcome FY 2009 to 2015, cumulative incidence % and incidence rate per 1000 person-years. Overall and by PTSD case vs. control.
eTable 2. Type 2 Diabetes outcome FY 2009 to 2015, stratified by PTSD status, cumulative incidence % and incidence rate per 1000 person-years by obesity.