Key Points
Question
Is the network structure of emotional and behavioral symptoms among elementary school girls indicative of later anxiety disorder or major depression occurrence?
Findings
In this network analysis of 932 elementary school girls from an ongoing population-based cohort study, bridge symptoms between disruptive and internalizing symptom communities (symptom clusters in networks) were identified. These symptoms exhibited the strongest relationships with anxiety disorders at ages 15 and 22 years.
Meaning
Bridge symptoms appear to play a central role in the developmental process leading to long-term anxiety and have potential relevance as early targets in disease-prevention or health-promotion interventions.
Abstract
Importance
The onset of adult psychopathologic disorders can be traced to behavioral or emotional symptoms observed in childhood, which could be targeted in early interventions to prevent future mental disorders. The network perspective is a novel conceptualization of psychopathologic disorders that could help to identify target symptoms with a distinct role in the emergence of mental illness.
Objective
To assess whether the network structure of emotional and behavioral symptoms among elementary school girls is associated with anxiety disorders or major depression in early adulthood.
Design, Setting, and Participants
The Quebec Longitudinal Study of Kindergarten Children is an ongoing, prospective, population-based study of kindergarten children attending French-speaking state schools in the Canadian province of Quebec in 1986-1988. This study included 932 girls whose parents completed the Social Behavior Questionnaire when the girls were ages 6 (baseline), 8, and 10 years; 780 participants were interviewed to assess the presence of mental disorders at age 15 and/or 22 years. Data analysis was conducted from December 2016 to April 2018.
Main Outcomes and Measures
Gaussian graphical models were estimated for 33 symptoms (eg, internalizing, externalizing, and prosocial behaviors) assessed using the Social Behavior Questionnaire to evaluate the temporal stability of the symptom network through childhood. At follow-up time points, mental disorders were assessed using the DSM-III-R, and symptom networks were reestimated at ages 6 to 10 years, this time including a variable indicative of future diagnosis.
Results
At baseline, the mean (SD) age of the 932 girls was 6.0 (0.3) years. Among the 780 women assessed at follow-up, 270 (34.6%) and 128 (16.4%) had developed anxiety disorders and major depression, respectively. Symptoms clustered in internalizing and externalizing communities. Five symptoms—irritable, blames others, not liked by others, often cries, and solitary—emerged as bridge symptoms between the disruptive and internalizing communities. These symptoms were those that were connected with the highest regularized edge weights (from 0.015 to 0.076) to future anxiety disorders once added to the network. Bootstrapped 95% CIs ranged from (95% CI, −0.063 to 0.068) to (95% CI, 0.561 to 0.701) for positive edges and from (95% CI, −0.156 to 0.027) to (95% CI, −0.081 to 0.078) for negative edges included in the regularized network.
Conclusions and Relevance
Bridge symptoms between disruptive and internalizing communities are identified for the first time in childhood, and these findings suggest that these symptoms could be central in indicating probable later anxiety disorders. The study suggests that bridge symptoms should be investigated further as potential early targets in disease-prevention interventions.
This population-based network analysis examines the association between emotional and behavior symptoms demonstrated by elementary school girls and later diagnoses of anxiety disorder and depression in adolescence and early adulthood.
Introduction
In recent decades, an increasing number of studies from representative birth cohorts have shown that the onset of adult psychopathologic disorders can be traced back to behavioral or emotional symptoms observed in childhood or adolescence.1,2,3 These studies have suggested that targeting early childhood symptoms might be effective in preventing future mental disorders. However, these interventions are challenging to implement because we lack knowledge on which specific childhood symptoms have predictive associations with adult psychopathologic disorders. High levels of childhood emotional and disruptive problems have been associated with depression and anxiety4,5,6 and antisocial7,8,9,10 disorders in adulthood, suggesting homotypic continuity (ie, behaviors predicting future occurrences of the same behaviors). However, some studies have also found evidence for heterotypic continuity.1 For instance, externalizing behaviors in children have been found to be predictive of anxiety disorders5 or depression11 in adulthood, and anxiety to be predictive of disruptive disorders12 in later development.
An approach known as the network perspective has been proposed to investigate and conceptualize mental disorders.13,14 For example, Van Borkulo et al15 found that the symptom network structure in adults diagnosed with major depression was associated with the longitudinal course of the illness (but see also Schweren et al16). From this perspective, symptoms (eg, poor sleep and depressed mood) are not conceptualized as passive consequences of an underlying disorder (eg, depression) as in the common cause model traditionally used in classic psychometrics. Instead, symptoms are conceptualized as distinct entities that can causally influence each other and be self-reinforcing.13,14 Symptoms are thus part of causal chains including feedback loops, which can culminate in disorders. Intersymptom associations reflect the underlying causal links that constitute these chains.13,17
Network analysis is an important statistical tool in the network perspective, focusing on symptoms (nodes) and intersymptom associations (edges) that together constitute a network. When activated, a symptom highly connected to other symptoms is likely to spread activation by them through the network. This property of the nodes highlights one of the fundamental differences between the network perspective and the common cause model: symptoms are not interchangeable or equally reflective of the latent disorder. Quite the opposite, they are constitutive of this disorder and are not necessarily equally involved in its emergence.13,14,18,19
Various criticisms have been leveled against the use of the common cause model in psychology and several are particularly relevant to developmental psychopathologic disorders.20 For example, because symptoms of disorders can vary with the developmental stage, the assumption of symptom interchangeability implied in this model does not hold when disorders are studied over lifetime. Another example concerns the conceptualization of disorders as separate entities in the common cause model. For some disorders, for example, anxiety and depression, there is currently no consensus on how to distinguish between them in early childhood.21,22,23,24,25,26,27,28 In addition, the common cause model treats symptoms as exchangeable indicators of a latent disorder and as such does not naturally accommodate the investigation of specific symptom-level effects. In contrast, because network approaches focus on relationships between individual symptoms, they allow us to focus at the level of symptoms. Therefore, network approaches offer a new developmental perspective in psychopathologic disorders by (1) providing a more detailed picture, which may yield etiologic clues to the development of disorders, and (2) addressing and resolving ambiguous findings regarding long-term indication of the probability of psychopathologic disorders. For example, heterotypic continuity from childhood externalizing behaviors to adult anxiety and depression may reflect contrasting contributions of individuals externalizing symptoms to the development of disorders. Therefore, the network perspective has the potential to provide more clinically useful insights than the classic model regarding the role of early symptoms in the estimation of the probability of later disorders.
The present study used this new approach to explore the network structure of emotional and behavioral symptoms exhibited during childhood. In addition, we investigated homotypic and heterotypic continuity through life, because this continuity could highlight symptoms with a distinct role in the emergence of mental illness that could be targeted in early interventions. We focused on anxiety disorders and major depression in women, as they are the most prevalent mental disorders in women, about twice as prevalent as in men, whereas, during childhood, girls exhibit fewer disruptive symptoms than boys, but there is no clear sex difference in emotional symptoms.29,30 The 3 main aims were to (1) explore the network structure of these emotional and behavioral symptoms at the age of 6 years, (2) describe the evolution of the network structure through childhood (age 6-10 years), and (3) evaluate links between this network structure in childhood and anxiety disorders and major depression in adolescence or early adulthood.
Methods
Study Sample
The Quebec Longitudinal Study of Kindergarten Children is an ongoing, prospective, population-based study of kindergarten children attending French-speaking state schools in the Canadian province of Quebec in school years 1986-1987 and 1987-1988. At baseline (age 6 years), 1017 children exhibiting disruptive behavior problems and 2000 children representative of the population were enrolled.31 The present study analyzed data for all of the girls (1423) enrolled at baseline. The study was approved by the research ethics boards of the University of Montreal, McGill University, and St Justine Hospital. Written informed consent was provided by the parents; participants received financial compensation.
Childhood Emotional and Behavioral Symptoms
When the girls were ages 6 to 12 years, the Social Behavior Questionnaire (SBQ) was completed yearly by the parent. The 38 items in this questionnaire, presented in the Table, assess a range of behaviors, including internalizing, disruptive, and prosocial behaviors, using a 3-point response scale from 0 (never applies) to 2 (frequently applies).32 We reverse-coded the 10 items assessing prosocial behaviors. Data for ages 6, 8, and 10 years were used.
Table. Items of the Social Behavior Questionnaire, Their Assigned Label, and Community.
| Community (Color) | Label | Meaning |
|---|---|---|
| Attention (light sea green) | At-Conc | Poor concentration |
| At-Give | Gives up quickly | |
| At-Inat | Inattentive | |
| At-Star | Stares into space | |
| Hyperactivity (light green) | Ac-Rest | Restless, always running or jumping |
| Ac-Squi | Squirmy, does not know how to stay still | |
| Disruptive symptoms (green) | D-Blam | Blames others |
| D-Cons | Inconsiderate toward others | |
| D-Dest | Destroys her or someone else’s things | |
| D-Diso | Disobedient | |
| D-Irri | Irritable, loses her temper | |
| D-Kick | Kicks, bites, hits other children | |
| D-Lies | Tells lies | |
| D-Like | Not liked by other children | |
| D-Shar | Does not share toys | |
| Internalizing symptoms (royal blue) | I-Crie | Often cries |
| I-Fear | Fearful | |
| I-Meti | Tends to be very meticulous | |
| I-Sad | Seems sad, unhappy | |
| I-Soli | Tends to play alone, solitary | |
| I-Worr | Worried, many things worry her | |
| None (white) | N-Nail | Bites nails |
| N-Twit | Twitches | |
| Prosocial (violet-red) | P-Byst | Will invite bystanders to join in a game |
| P-Comf | Comforts a child who is crying or upset | |
| P-Diff | Offers to help other children who are having difficulty with a task | |
| P-Hurt | Will try to help someone who has been hurt | |
| P-Mess | Volunteers to help clear up a mess someone else has made | |
| P-Pick | Spontaneously helps to pick up objects that another child has dropped | |
| P-Prai | Takes the opportunity to praise the work of less-able children | |
| P-Quar | If there is a quarrel or dispute, will try to stop it | |
| P-Sick | Helps other children who are not feeling well | |
| P-Symp | Shows sympathy toward someone who has made a mistake | |
| Not used, because highly skewed | Bullies | |
| Fights with other children | ||
| Takes things that do not belong to her | ||
| Speech difficulties | ||
| Stutters |
Disorders Assessed in Adolescence and Adulthood
At ages 15 and 23 years, participants completed the French version of the Diagnostic Interview Schedule to determine DSM-III-R diagnoses of anxiety disorders and major depression.33,34 Participants were classified as having developed anxiety disorders if they exhibited at least 1 of the following diagnoses at any of the follow-up ages: generalized and separation anxiety, agoraphobia, social phobia, overanxious, avoidant, and panic disorder.
Statistical Analysis
To gain insight into how many symptom clusters are present in the network, we estimated the factor structure of the SBQ using a longitudinal exploratory structural equation model in Mplus software, version 7.4.35 Data analysis was conducted from December 2016 to April 2018.
Emotional and Behavioral Symptom Networks at Age 6 Years
Gaussian graphical models were estimated (based on polychoric correlations) for the SBQ items on pairwise complete observations using the R software package, qgraph.36 A gaussian graphical model is an undirected weighted network in which edge weights can be understood as partial correlation coefficients (ie, controlling for the effects of all other items in the network). A regularization technique, the least absolute shrinkage and selection operator (LASSO) procedure, was used to conservatively identify only the relevant edges among the large number of pairwise associations estimated in the gaussian graphical model.37,38 Layouts for each graph were computed using the Fruchterman-Reingold algorithm, which places nodes with the strongest connections in the center of the network and weakly connected nodes on the periphery. To facilitate visual comparisons, common layouts were established on the data combined over the 3 collection times. Accuracy was evaluated by bootstrapping the edge weights’ 95% CIs using the R package bootnet.39 We computed the node strength centrality index (the sum of the absolute weights of every edge that connects the node to all other nodes in the network) that assesses how strongly connected this node is.40
Changes in Symptom Networks Through Childhood
Using the previously described procedure, symptom networks were reestimated at ages 8 and 10 years. Then, paired networks across ages were compared using the R package network comparison test. Two hypotheses were tested: the global strength invariance test, which states that the overall level of connectivity (weighted absolute sum of all edges in the network) is the same at each collection time, and the network structure invariance test, which investigates whether the structure of the network is identical across collection times.41 Paired tests were 2-sided with a significant threshold set at .05, and a Bonferroni correction was applied to control for multiple testing.
Symptom Networks in Childhood and Anxiety Disorders in Adolescence/Young Adulthood
We reestimated the SBQ network structure using the gaussian graphical model and LASSO regularization. The focus was on hyperactivity, attention, disruptive, and internalizing symptoms at ages 6, 8, and 10 years, including a binary variable that encoded whether women were diagnosed with anxiety disorders or major depression at follow-up.
Results
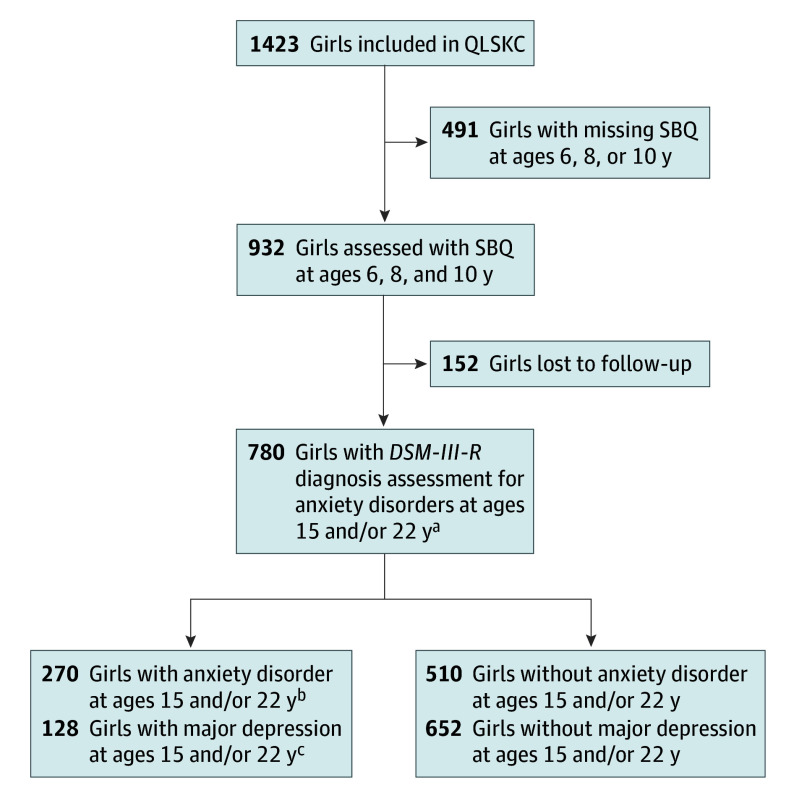
The study flowchart is shown in Figure 1. The network of SBQ items was studied through childhood among 932 girls with a mean (SD) age of 6.0 (0.3) years. Among the 780 women assessed at follow-up, 270 (34.6%) and 128 (16.4%) had developed 1 or more anxiety disorder or major depression. Observed differences owing to attrition concerning the baseline characteristics reported in eTable 1 in the Supplement were statistically significant.
Figure 1. Flowchart of the Girl Sample in the Quebec Longitudinal Study of Kindergarten Children (QLSKC).
SBQ indicates Social Behavior Questionnaire.
aA total of 492 participants were assessed at both follow-up points.
bThere were 131 (22.4%) girls with anxiety disorders among the 585 assessed at age 15 years and 188 (27.4%) girls with anxiety disorders among the 686 assessed at age 22 years.
cThere were 53 (9.1%) girls with major depression among the 585 assessed at age 15 years and 76 (11.1%) girls with major depression among the 686 assessed at age 22 years.
Because 5 SBQ items had very low reported rates (eTable 2 in the Supplement), we excluded them from all analyses: stutters, speech difficulties, bullies, takes things that do not belong to her, and fights with other children. Using the 33 remaining items, a 5-factor model provided the best fit to the data; the corresponding dimensions are given in the Table and eTables 2 and 3 in the Supplement: attention (4 items), hyperactivity (2 items), disruptive (9 items), internalizing (6 items), and prosocial (10 items). All factor loadings were under 0.3 for 2 items: bites nails and twitches.
Emotional and Behavioral Symptom Networks at Age 6 Years
The network at age 6 years is shown in Figure 2A and is illustrated in eFigure 1 in the Supplement. Its estimation was fairly accurate, with a noticeable proportion of the strongest edges where 95% CIs did not overlap with those of many others (ie, they were significantly stronger than most; eFigure 2 in the Supplement). Of the 528 possible edges in the network, 329 (62.3%) were not selected by the LASSO procedure.
Figure 2. Networks of the 33 Items in the Social Behavior Questionnaire at Ages 6, 8, and 10 Years.
Positive edges appear blue, negative red, and stronger and saturated represent strong regularized partial correlations. Edges with weight greater than |0.03| are shown; edges are scaled by value of the highest edge weight across all time points (0.65). Colors indicate community: light green, hyperactivity; sea-green, attention; green, disruptive; blue, internalizing; violet-red, prosocial; and white, no community. Item label abbreviations are defined in the Table.
As expected, items that belonged to the same exploratory structural equation model dimension formed communities in the network structure.42 In general, many cross-community associations emerged, except for items in the prosocial community, which rarely related to items in other communities. Four findings appeared to be the most relevant. First, direct associations between items in the disruptive and internalizing communities involved only 3 of the 9 disruptive symptoms (irritable, blames others, and not liked) and only 2 of the 6 internalizing symptoms (often cries and solitary). Second, the hyperactivity and attention communities were mainly connected through the symptom poor concentration. Third, there was no direct association between items in the hyperactivity and internalizing communities. Finally, some items were limited largely to intracommunity associations: destroys, kicks, and tells lies for the disruptive community, and worried for the internalizing community.
The node strength centrality indices for the 33 SBQ items are shown in Figure 3. The 2 items that did not belong to any exploratory structural equation model dimension (twitches and bites nails), as well as the internalizing symptoms, had low node strength indices. The 5 most central symptoms were inattentive, the prosocial symptom helps other children, and the 3 disruptive symptoms disobedient, irritable, and not liked.
Figure 3. Node Strength Centrality Estimates for the 33 Items in the Social Behavior Questionnaire Completed at Ages 6, 8, and 10 Years.
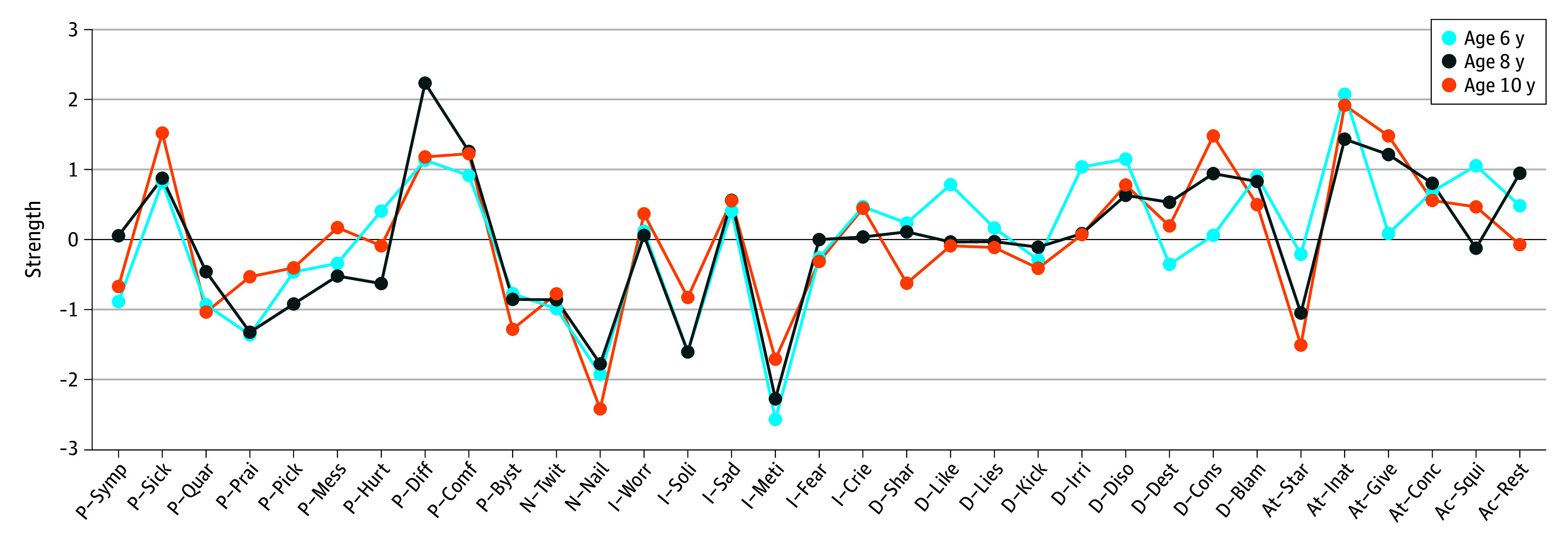
The R package bootnet was used to estimate the centrality stability coefficient (0.67), which should be above 0.5 to consider the order of the centrality index of the nodes as stable.19 Item label abbreviations are defined in the Table.
Changes in the Emotional and Behavioral Symptom Networks During Childhood
Networks at ages 8 and 10 years are shown in Figure 2B and C, respectively, and in eFigure 1 in the Supplement. Statistical comparisons of networks across time points were all nonsignificant for global strength and structure invariance. Thus, the null hypothesis that the networks for the different ages are identical at the population level could not be rejected.
As shown in Figure 3, node strength centrality indices were consistent across the different ages (Spearman correlation coefficients between ages 6 and 8, 6 and 10, and 8 and 10 years were 0.73, 0.77, and 0.85 respectively), also reflecting the strong similarity between the network structures. The stronger nodes were the same at ages 6 and 10 years.
Association With Disorders at Follow-up
Figure 4 presents the network structures we reestimated at ages 6, 8, and 10 years, now including anxiety diagnosis at follow-up ages 15 and 22 years. Bootstrapped 95% CIs ranged from (95% CI, −0.063, to 0.068) to (95% CI, 0.561 to 0.701) for positive edges and from (95% CI, −0.156 to 0.027) to (95% CI, −0.081 to 0.078) for negative edges included in the regularized network. Two, 5 and 8 of these edges involved the anxiety disorders node in the 6, 8, and 10 years networks, respectively. Thus, few items were relevant indicators of the probability of anxiety disorder diagnoses at follow-up. Not liked was the only one consistently connected to anxiety diagnosis across all measurement points with regularized edge weights equal to 0.076, 0.037, and 0.064 in the 6, 8, and 10 years networks respectively. On the right side of Figure 4, we highlight the edges between SBQ items and anxiety diagnosis. Nodes from the internalizing community were progressively involved in association with anxiety diagnosis over time, but nodes that were involved more strongly and sooner were disobedient, irritable, and not liked from the disruptive community. These 3 nodes were also found to be involved in direct relationships between the disruptive and internalized communities in Figure 2, but the kick disruptive symptom, which exhibited negative regularized edge weight equal to −0.066 with anxiety diagnosis at age 10 years, was only involved in intracommunity relationships. Results concerning the links with major depression at follow-up are shown in eFigure 3 in the Supplement. The number of nodes associated with major depression also increased over time, but no node was consistently associated with major depression across all measurement points.
Figure 4. Links Between the Social Behavior Questionnaire (SBQ) Item Network During Childhood and Occurrence of Anxiety Disorders at Follow-up.
A, Network of the 21 items of the hyperactivity (light green), attention (sea green), disruptive (green), and internalizing (blue) communities in the SBQ at age 6 years. The ANX node (red) represents the occurrence of anxiety disorders at follow-up. Each edge corresponds to a partial correlation (positive in blue, negative in red, with an absolute magnitude >0.03) between 2 items, and its thickness corresponds to the absolute magnitude of the correlation. For instance, an edge between ANX and like implies that indication of the like item at age 6 years was indicative of anxiety disorder diagnosis at follow-up (age 15 or 22 years). B-D, All edges are removed except relevant edges involving the ANX node in the network at ages 6, 8, and 10 years, with no minimum absolute weight magnitude appearing in the graph. Item label abbreviations are defined in the Table.
Discussion
For what we believe to be the first time, we adopted the network perspective to investigate longitudinally the network structure among a broad range of symptoms collected in girls (6-10 years) and their role in the emergence of anxiety and depression until age 22 years. Focusing at the symptom level allowed us to reveal information inaccessible to methods traditionally used in classic psychometrics. In particular, we highlighted the central role of bridge symptoms in the developmental process leading to long-term anxiety. Clinicians may wish to focus on these bridge symptoms when assessing patients. The network approach provides a natural language for clinicians and patients to use when discussing symptoms and therapeutic options.43
First, we found that the symptoms irritable, blames others, not liked, often cries, and solitary retained a distinctive position in the network because most of the direct relationships between the disruptive and internalized communities transited through them. These symptoms have been termed bridge symptoms in the network perspective, as they constitute pathways that can connect different disorders.13,14 In clinical practice, irritability is known to characterize both internalizing and externalizing disorders in childhood, and there is a growing number of studies focusing on irritability.30,44,45 The poor concentration symptom has a similar position between the hyperactivity and attention communities. This observed singular position is consistent with the commonly observed comorbidity between hyperactivity disorder and attention-deficit disorder, but the information added here is that pathways between components of the 2 communities seem to be mainly mediated by the poor concentration node. This mediation phenomenon suggests that an intervention targeting this node could reduce attention-deficit symptoms in, for example, hyperactive children; however, as the observational nature of the current data precludes firm causal conclusions, this hypothesis requires experimental testing.14
Second, this study showed that the network structure of SBQ symptoms, including bridge symptoms, was relatively stable over a 5-year developmental period. Results of tests comparing network structure across ages were not significant and the correlations between edge weights were consistently high. This finding challenges recent claims that network analyses do not replicate46 and suggests that, as the importance of bridge symptoms remains similar over time, the symptoms could be seen as providing leverage for altering the network early in childhood.
Third, our findings have highlighted for what we believe to be the first time the predictive role of bridge symptoms. In particular, the bridge symptoms not liked by other children, disobedient, and irritable were positively related to future diagnoses of anxiety disorders. This relationship is consistent with previous meta-analytic findings on the association of irritability with anxiety in longitudinal studies.47 Conversely, the kicks disruptive symptom, which was only related to other symptoms in the same disruptive community, negatively predicted anxiety disorders at follow-up. This pattern of predictive relationships is consistent with the way in which bridge symptoms have been conceptualized in the literature and offers new ways of investigating heterotypic continuity.13,43,48 Our results suggest that girls may present symptoms, such as kicking, telling lies, and destroying things, but as long as the bridge symptoms such as not liked or irritable are not activated, the risk of later developing anxiety disorders remains stable. From a network perspective, presenting symptoms that connect clusters of problems could lead to the activation of more global patterns of symptom activation throughout the network structure and constitutes a liability for a range of mental disorders. Alternatively, specific patterns of bridge symptoms may be present for different disorders. In this study, we did not find evidence for the specific bridge symptoms linked to anxiety to be also consistently linked with depression. More research is therefore necessary to replicate our findings and investigate whether the bridge symptoms that we identified are also key indicators of other future mental disorders.
Limitations
A first limitation of our study is the sample size of 932 participants, which could be too small to estimate the large number of variables in a 33-node network. However, the LASSO procedure is recognized as a powerful regularization approach to partly circumvent this issue, and bootstrap procedures showed our network estimation to be acceptably accurate. A 45% attrition rate is also responsible for this sample size and may have affected the results. Attrition was more important for participants with adverse family environments because childhood and adulthood symptoms tend to be higher in these settings. The power to detect the associations that we observed would thus have been higher without such attrition with, in addition, possibly stronger effect sizes. Nevertheless, results should be replicated in larger samples and without attrition.
A second limitation is the number of statistical tests performed in the evaluation of whether network connections were invariant over age. The evaluation of whether connections should be included in a given network does not present this problem because of the regularization step of the LASSO. A Bonferroni correction was applied to control for multiple testing, but it implies a loss of power. This implication means that replication of these results is called for. The stability of the emotional and behavioral symptom network observed in this study through childhood proved to be substantial; however, it is possible that the networks were somewhat different at the population level, but that we failed to detect this owing to lack of power.
A third limitation concerns the heterogeneity of the diagnoses identifying women with anxiety disorder at follow-up. More specific links with the childhood symptom network would probably have been evidenced with more homogeneous diagnoses, but fewer women would have been identified with anxiety disorders, thus reducing power. Finally, we decided to focus on girls, but it would be interesting to see whether similar patterns are found in boys, provided sufficiently large samples are available to study anxiety disorders, which are half as prevalent in boys.
Conclusions
In the present study, we identified, for what we believe to be the first time, bridge symptoms between disruptive and internalizing communities in childhood and our findings suggest that these symptoms could be central in the developmental process leading to long-term anxiety. Bridge symptoms should be investigated further as potential early targets in disease-prevention and health-promotion interventions.
eTable 1. Baseline Characteristics of Each Subsample Studied
eTable 2. Frequencies for Each Response to the 38 Items at Each Collection Time for the 932 Girls With Social Behavior Questionnaire Scores at ages 6, 8, and 10
eTable 3. Standardized Loadings From the Longitudinal Exploratory Structural Equation Model on the 33 (Non-Skewed) Items in the Social Behavior Questionnaire (SBQ) With 5 Factors Extracted for the 932 Girls With SBQ Scores at Ages 6, 8 and 10
eFigure 1. Corresponds to Figure 2 With All Edges Shown Including Those With a Weight Over |0.03|
eFigure 2. Bootstrapped 95% Confidence Intervals of the Edge Weights for the Figure 2 Networks
eFigure 3. Links Between SBQ Item Network During Childhood and Occurrence of Major Depression at Follow-up
References
- 1.Rutter M, Kim-Cohen J, Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. J Child Psychol Psychiatry. 2006;47(3-4):276-295. doi: 10.1111/j.1469-7610.2006.01614.x [DOI] [PubMed] [Google Scholar]
- 2.Lewis AJ, Galbally M, Gannon T, Symeonides C. Early life programming as a target for prevention of child and adolescent mental disorders. BMC Med. 2014;12:33. doi: 10.1186/1741-7015-12-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pine DS, Fox NA. Childhood antecedents and risk for adult mental disorders. Annu Rev Psychol. 2015;66(1):459-485. doi: 10.1146/annurev-psych-010814-015038 [DOI] [PubMed] [Google Scholar]
- 4.Dekker MC, Ferdinand RF, van Lang NDJ, Bongers IL, van der Ende J, Verhulst FC. Developmental trajectories of depressive symptoms from early childhood to late adolescence: gender differences and adult outcome. J Child Psychol Psychiatry. 2007;48(7):657-666. doi: 10.1111/j.1469-7610.2007.01742.x [DOI] [PubMed] [Google Scholar]
- 5.Roza SJ, Hofstra MB, van der Ende J, Verhulst FC. Stable prediction of mood and anxiety disorders based on behavioral and emotional problems in childhood: a 14-year follow-up during childhood, adolescence, and young adulthood. Am J Psychiatry. 2003;160(12):2116-2121. doi: 10.1176/appi.ajp.160.12.2116 [DOI] [PubMed] [Google Scholar]
- 6.Côté SM, Boivin M, Liu X, Nagin DS, Zoccolillo M, Tremblay RE. Depression and anxiety symptoms: onset, developmental course and risk factors during early childhood. J Child Psychol Psychiatry. 2009;50(10):1201-1208. doi: 10.1111/j.1469-7610.2009.02099.x [DOI] [PubMed] [Google Scholar]
- 7.Reef J, Diamantopoulou S, van Meurs I, Verhulst FC, van der Ende J. Developmental trajectories of child to adolescent externalizing behavior and adult DSM-IV disorder: results of a 24-year longitudinal study. Soc Psychiatry Psychiatr Epidemiol. 2011;46(12):1233-1241. doi: 10.1007/s00127-010-0297-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Broidy LM, Nagin DS, Tremblay RE, et al. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: a six-site, cross-national study. Dev Psychol. 2003;39(2):222-245. doi: 10.1037/0012-1649.39.2.222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Copeland WE, Miller-Johnson S, Keeler G, Angold A, Costello EJ. Childhood psychiatric disorders and young adult crime: a prospective, population-based study. Am J Psychiatry. 2007;164(11):1668-1675. doi: 10.1176/appi.ajp.2007.06122026 [DOI] [PubMed] [Google Scholar]
- 10.Simonoff E, Elander J, Holmshaw J, Pickles A, Murray R, Rutter M. Predictors of antisocial personality: continuities from childhood to adult life. Br J Psychiatry. 2004;184(2):118-127. doi: 10.1192/bjp.184.2.118 [DOI] [PubMed] [Google Scholar]
- 11.Loth AK, Drabick DAG, Leibenluft E, Hulvershorn LA. Do childhood externalizing disorders predict adult depression? a meta-analysis. J Abnorm Child Psychol. 2014;42(7):1103-1113. doi: 10.1007/s10802-014-9867-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict? J Child Psychol Psychiatry. 2007;48(12):1174-1183. doi: 10.1111/j.1469-7610.2007.01812.x [DOI] [PubMed] [Google Scholar]
- 13.Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. 2010;33(2-3):137-150. doi: 10.1017/S0140525X09991567 [DOI] [PubMed] [Google Scholar]
- 14.Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91-121. doi: 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 15.van Borkulo C, Boschloo L, Borsboom D, Penninx BWJH, Waldorp LJ, Schoevers RA. Association of symptom network structure with the course of depression. JAMA Psychiatry. 2015;72(12):1219-1226. doi: 10.1001/jamapsychiatry.2015.2079 [DOI] [PubMed] [Google Scholar]
- 16.Schweren L, van Borkulo CD, Fried E, Goodyer IM. Assessment of symptom network density as a prognostic marker of treatment response in adolescent depression. JAMA Psychiatry. 2018;75(1):98-100. doi: 10.1001/jamapsychiatry.2017.3561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cramer AOJ, van der Sluis S, Noordhof A, et al. Dimensions of normal personality as networks in search of equilibrium: you can’t like parties if you don’t like people. Eur J Pers. 2012;26(4):414-431. doi: 10.1002/per.1866 [DOI] [Google Scholar]
- 18.Fried EI, Bockting C, Arjadi R, et al. From loss to loneliness: the relationship between bereavement and depressive symptoms. J Abnorm Psychol. 2015;124(2):256-265. doi: 10.1037/abn0000028 [DOI] [PubMed] [Google Scholar]
- 19.Armour C, Fried EI, Deserno MK, Tsai J, Pietrzak RH. A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. J Anxiety Disord. 2017;45:49-59. doi: 10.1016/j.janxdis.2016.11.008 [DOI] [PubMed] [Google Scholar]
- 20.Borsboom D. Psychometric perspectives on diagnostic systems. J Clin Psychol. 2008;64(9):1089-1108. doi: 10.1002/jclp.20503 [DOI] [PubMed] [Google Scholar]
- 21.Nuijten MB, Deserno MK, Cramer AOJ, Borsboom D. Mental disorders as complex networks. Clin Neuropsychiatry. 2016;13(4/5):68-76. [Google Scholar]
- 22.Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA. The network structure of symptoms of the Diagnostic and Statistical Manual of Mental Disorders. PLoS One. 2015;10(9):e0137621. doi: 10.1371/journal.pone.0137621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borsboom D, Cramer AOJ, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS One. 2011;6(11):e27407. doi: 10.1371/journal.pone.0027407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borsboom D. Measuring the Mind: Conceptual Issues in Contemporary Psychometrics. Cambridge, UK: Cambridge University Press; 2005. doi: 10.1017/CBO9780511490026 [DOI] [Google Scholar]
- 25.Caron C, Rutter M. Comorbidity in child psychopathology: concepts, issues and research strategies. J Child Psychol Psychiatry. 1991;32(7):1063-1080. doi: 10.1111/j.1469-7610.1991.tb00350.x [DOI] [PubMed] [Google Scholar]
- 26.Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol Bull. 2014;140(3):816-845. doi: 10.1037/a0034733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stringaris A, Maughan B, Copeland WS, Costello EJ, Angold A. Irritable mood as a symptom of depression in youth: prevalence, developmental, and clinical correlates in the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2013;52(8):831-840. doi: 10.1016/j.jaac.2013.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boylan KR, Miller JL, Vaillancourt T, Szatmari P. Confirmatory factor structure of anxiety and depression: evidence of item variance across childhood. Int J Methods Psychiatr Res. 2011;20(4):194-202. doi: 10.1002/mpr.349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015;17(3):327-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zahn-Waxler C, Klimes-Dougan B, Slattery MJ. Internalizing problems of childhood and adolescence: prospects, pitfalls, and progress in understanding the development of anxiety and depression. Dev Psychopathol. 2000;12(3):443-466. doi: 10.1017/S0954579400003102 [DOI] [PubMed] [Google Scholar]
- 31.Rouquette A, Côté SM, Pryor LE, Carbonneau R, Vitaro F, Tremblay RE. Cohort profile: the Quebec Longitudinal Study of Kindergarten Children (QLSKC). Int J Epidemiol. 2014;43(1):23-33. doi: 10.1093/ije/dys177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tremblay RE, Vitaro F, Gagnon C, Piché C, Royer N. A prosocial scale for the Preschool Behaviour Questionnaire: concurrent and predictive correlates. Int J Behav Dev. 1992;15(2):227-245. doi: 10.1177/016502549201500204 [DOI] [Google Scholar]
- 33.Breton JJ, Bergeron L, Valla JP, Berthiaume C, St-Georges M. Diagnostic Interview Schedule for Children (DISC-2.25) in Quebec: reliability findings in light of the MECA study. J Am Acad Child Adolesc Psychiatry. 1998;37(11):1167-1174. doi: 10.1097/00004583-199811000-00016 [DOI] [PubMed] [Google Scholar]
- 34.Robins L, Cottler L, Bucholz K, Compton W. The Diagnostic Interview Schedule, Version IV. St Louis, MO: Washington University; 1995. [Google Scholar]
- 35.Muthén LK, Muthén BO. MPlus Statistical Analysis With Latent Variables User’s Guide. 7th ed. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- 36.Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. Qgraph: network visualizations of relationships in psychometric data. J Stat Softw. 2012;48(4):1-18. doi: 10.18637/jss.v048.i04 [DOI] [Google Scholar]
- 37.Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc B. 1996;58(1):267-288. doi: 10.1111/j.1467-9868.2011.00771.x [DOI] [Google Scholar]
- 38.Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. ArXiv160701367 Stat. July 2016. http://arxiv.org/abs/1607.01367. Accessed November 7, 2017. [DOI] [PubMed]
- 39.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50(1):195-212. doi: 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths. Soc Netw. 2010;32(3):245-251. doi: 10.1016/j.socnet.2010.03.006 [DOI] [Google Scholar]
- 41.van Borkulo CD, Epskamp S, Millner A. Statistical comparison of two networks with respect to global strength. 2015. https://github.com/cvborkulo/NetworkComparisonTest.
- 42.Kruis J, Maris G. Three representations of the Ising model. Sci Rep. 2016;6:34175. doi: 10.1038/srep34175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5-13. doi: 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wakschlag LS, Estabrook R, Petitclerc A, et al. Clinical implications of a dimensional approach: the normal:abnormal spectrum of early irritability. J Am Acad Child Adolesc Psychiatry. 2015;54(8):626-634. doi: 10.1016/j.jaac.2015.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dougherty LR, Smith VC, Bufferd SJ, et al. DSM-5 disruptive mood dysregulation disorder: correlates and predictors in young children. Psychol Med. 2014;44(11):2339-2350. doi: 10.1017/S0033291713003115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Forbes MK, Wright AGC, Markon KE, Krueger RF. Evidence that psychopathology symptom networks have limited replicability. J Abnorm Psychol. 2017;126(7):969-988. doi: 10.1037/abn0000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, Stringaris A. The status of irritability in psychiatry: a conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry. 2016;55(7):556-570. doi: 10.1016/j.jaac.2016.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fried EI, van Borkulo CD, Cramer AOJ, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insights. Soc Psychiatry Psychiatr Epidemiol. 2017;52(1):1-10. doi: 10.1007/s00127-016-1319-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Baseline Characteristics of Each Subsample Studied
eTable 2. Frequencies for Each Response to the 38 Items at Each Collection Time for the 932 Girls With Social Behavior Questionnaire Scores at ages 6, 8, and 10
eTable 3. Standardized Loadings From the Longitudinal Exploratory Structural Equation Model on the 33 (Non-Skewed) Items in the Social Behavior Questionnaire (SBQ) With 5 Factors Extracted for the 932 Girls With SBQ Scores at Ages 6, 8 and 10
eFigure 1. Corresponds to Figure 2 With All Edges Shown Including Those With a Weight Over |0.03|
eFigure 2. Bootstrapped 95% Confidence Intervals of the Edge Weights for the Figure 2 Networks
eFigure 3. Links Between SBQ Item Network During Childhood and Occurrence of Major Depression at Follow-up