Key Points
Question
What are the neurocognitive mechanisms that underlie the putative therapeutic effects of cannabidiol in psychosis?
Findings
In this investigation comparing 33 individuals at clinical high risk of psychosis who were part of a double-blind randomized clinical trial and 19 healthy control individuals, a single oral dose of cannabidiol modulated activation in the striatum, medial temporal cortex, and midbrain. In each of these regions, the level of activation following administration of cannabidiol to patients at clinical high risk of psychosis was intermediate between the response in healthy control individuals who did not receive any drug and in patients at clinical high risk receiving placebo.
Meaning
These results suggest that cannabidiol may normalize dysfunction in these brain regions, which are critically implicated in psychosis, and this may underlie its therapeutic effects in psychosis.
This randomized clinical trial investigates the neurocognitive mechanisms that underlie the therapeutic effects of cannabidiol vs placebo in people at clinical high risk of psychosis.
Abstract
Importance
Cannabidiol (CBD) has antipsychotic effects in humans, but how these are mediated in the brain remains unclear.
Objective
To investigate the neurocognitive mechanisms that underlie the therapeutic effects of CBD in psychosis.
Design, Setting, and Participants
In this parallel-group, double-blind, placebo-controlled randomized clinical trial conducted at the South London and Maudsley NHS Foundation Trust in London, United Kingdom, 33 antipsychotic medication–naive participants at clinical high risk (CHR) of psychosis and 19 healthy control participants were studied. Data were collected from July 2013 to October 2016 and analyzed from November 2016 to October 2017.
Interventions
A total of 16 participants at CHR of psychosis received a single oral dose of 600 mg of CBD, and 17 participants at CHR received a placebo. Control participants were not given any drug. All participants were then studied using functional magnetic resonance imaging (fMRI) while performing a verbal learning task.
Main Outcomes and Measures
Brain activation during verbal encoding and recall, indexed using the blood oxygen level–dependent hemodynamic response fMRI signal.
Results
Of the 16 participants in the CBD group, 6 (38%) were female, and the mean (SD) age was 22.43 (4.95) years; of 17 in the placebo group, 10 (59%) were female, and the mean (SD) age was 25.35 (5.24) years; and of 19 in the control group, 8 (42%) were female, and the mean (SD) age was 23.89 (4.14) years. Brain activation (indexed using the median sum of squares ratio of the blood oxygen level–dependent hemodynamic response effects model component to the residual sum of squares) was analyzed in 15 participants in the CBD group, 16 in the placebo group, and 19 in the control group. Participants receiving placebo had reduced activation relative to controls in the right caudate during encoding (placebo: median, −0.027; interquartile range [IQR], −0.041 to −0.016; control: median, 0.020; IQR, −0.022 to 0.056; P < .001) and in the parahippocampal gyrus and midbrain during recall (placebo: median, 0.002; IQR, −0.016 to 0.010; control: median, 0.035; IQR, 0.015 to 0.039; P < .001). Within these 3 regions, activation in the CBD group was greater than in the placebo group but lower than in the control group (parahippocampal gyrus/midbrain: CBD: median, −0.013; IQR, −0.027 to 0.002; placebo: median, −0.007; IQR, −0.019 to 0.008; control: median, 0.034; IQR, 0.005 to 0.059); the level of activation in the CBD group was thus intermediate to that in the other 2 groups. There were no significant group differences in task performance.
Conclusions and Relevance
Cannabidiol may partially normalize alterations in parahippocampal, striatal, and midbrain function associated with the CHR state. As these regions are critical to the pathophysiology of psychosis, the influence of CBD at these sites could underlie its therapeutic effects on psychotic symptoms.
Trial Registration
isrctn.org Identifier: ISRCTN46322781
Introduction
Epidemiological and clinical studies have implicated regular cannabis use as a risk factor for the development of psychosis1 and for poor clinical outcomes after its onset.2,3,4 Psychosis is also associated with alterations in the endocannabinoid system,5,6 independent of exposure to cannabis. The endocannabinoid system thus represents a potential therapeutic target for psychosis.7,8 Its main central receptor, cannabinoid receptor 1 (CB1), is ubiquitous in the brain9,10 and modulates the function of neurotransmitters thought to be critically perturbed in psychosis, including dopamine and glutamate.11 The constituent of cannabis responsible for its short-term psychotomimetic effects12,13,14 and its association with the development and relapse of psychosis is Δ9-tetrahydrocannabinol (THC).1,2,3,4,15,16 In contrast, cannabidiol (CBD), one of the major nonpsychoactive constituents of cannabis, has broadly opposite neural and behavioral effects.17,18,19,20,21,22,23 In particular, we have shown that CBD has opposing effects to THC on activation in the striatum during verbal memory17 and salience processing,18 on amygdala responses during emotional processing,17 and on the functional connectivity of these regions.19 Furthermore, pretreatment with CBD blocks the experimental induction of psychotic symptoms by THC,17,20 and clinical studies24,25 indicate that CBD has antipsychotic and anxiolytic properties in patients with mental disorders.7,8 Cannabidiol was noninferior to antipsychotic medication in a 4-week clinical trial in first-episode psychosis26 and improved psychotic symptoms when used as an adjunct to antipsychotic medication in a 6-week trial in patients with long-term psychosis.27
Although there is good evidence that CBD can have beneficial effects on psychotic symptoms, how these effects are mediated in the brain remains unclear. The present study sought to address this issue by examining the effects of CBD in individuals at clinical high risk (CHR) of psychosis. Individuals at CHR typically experience clinically significant psychotic symptoms that are qualitatively similar to those seen in patients with frank psychosis28 and are associated with high levels of distress.29 Contemporary preclinical models propose that psychosis involves a perturbation of activity in the medial temporal lobe (MTL) that drives subcortical dopamine dysfunction through projections to the striatum and midbrain.30 Moreover, neuroimaging studies in individuals at CHR indicate that the later onset of psychosis is linked to alterations in parahippocampal structure31 and function32,33,34 and to elevated striatal and midbrain dopamine activity.
In the present study, on the basis of previous studies, we expected that participants at CHR would display altered responses in the MTL, midbrain, and striatum relative to healthy control participants. Our main hypothesis was that CBD would attenuate functional abnormalities in this triad of regions. While the MTL is critical for new learning,35 the midbrain36,37,38,39 and striatum39,40,41,42,43 also play a key role in supporting the encoding and updating of contextual information in memory. Therefore, we used the verbal paired associate (VPA) learning task, which engages these processes and brain regions.13,14 Furthermore, transient psychotomimetic effects of THC have been associated with its modulation of striatal13 and midbrain14 function, and CBD17 has been shown to oppose these striatal effects of THC during this task.
Methods
Study Design, Participants, and Procedures
The trial protocol can be found in Supplement 1, and detailed methods can be found in the eMethods and eFigure 1 in Supplement 2. Thirty-three antipsychotic medication–naive participants at CHR28 were recruited from early intervention services in the United Kingdom. Nineteen age-matched (within 3 years) healthy control participants were recruited by local advertisement. Individuals with a history of psychotic or manic episodes, neurological disorders, or a current DSM-IV diagnosis of substance dependence, IQ less than 70, and contraindication to magnetic resonance imaging (MRI) or treatment with CBD were excluded. Psychopathology was measured using Comprehensive Assessment of At-Risk Mental States (positive and negative symptoms)28 and State-Trait Anxiety Inventory–State Subscale44 at baseline before drug administration. Two participants at CHR were excluded, 1 from each of the CBD and placebo groups, after failing to correctly perform the imaging task, resulting in 15 participants in the CBD group and 16 in the placebo group. The study protocol was approved by the National Research Ethics Service Committee of London–Camberwell St Giles. All participants provided written informed consent.
Using a parallel-group, double-blind, placebo-controlled design, participants at CHR were randomized to either CBD or placebo treatment and received a single oral dose of 600 mg of CBD (THC-Pharm), a dose previously effective in established psychosis,26 or an identical placebo capsule, respectively. Three hours after taking the CBD or placebo capsule, participants underwent functional MRI (fMRI) while performing a VPA task that we have previously used in conjunction with fMRI and pharmacological challenge,13,14 including CBD administration17 (eMethods and eFigure 2 in Supplement 2). Control participants were investigated under identical conditions but did not receive any study drug.
All participants were asked to have refrained from consuming cannabis for 96 hours, alcohol for a minimum of 24 hours, and nicotine for 6 hours before scanning as well as any other recreational drugs for 2 weeks before the study day. A urine sample prior to scanning was used to screen for use of illicit drugs.
The VPA task (eMethods in Supplement 2) comprised 3 conditions (encoding, recall, and baseline), with stimuli presented visually in blocks and accuracy of responses recorded online. During encoding, participants were shown word pairs and asked to say yes or no aloud after each pair to indicate whether they went well together. The same word pairs were presented in the encoding condition 4 times so that the associations could be learned over repeated blocks. During recall, 1 of the words from previously presented pairs was shown, and participants were asked to say the word that it had previously been associated with. Participants said “pass” if they could not recall the missing word. During baseline, participants viewed a pair of blank blue rectangles of identical dimensions as in the encoding/recall condition. For each participant, the blood oxygen level–dependent (BOLD) hemodynamic response of the brain during each encoding and recall block, measured using a Signa HDx 3.0-T MRI scanner (General Electric; gradient echo sequence axially; 39 × 3-mm slices; 3.3-mm slice gap; 30-millisecond echo time; compressed acquisition with a 2-second repetition time and 3-second silence), was contrasted with the response during the baseline condition.
Analysis
Functional MRI data were analyzed with XBAM software, version 4.1, using a nonparametric approach to minimize assumptions (https://www.kcl.ac.uk/ioppn/depts/neuroimaging/research/imaginganalysis/Software/XBAM.aspx).45,46 Images were corrected for motion47 and spatially smoothed, and the experimental design was convolved with 2 γ-variate functions to model the BOLD response. Using the constrained BOLD effects model, a best fit between the weighted sum of these convolutions and the change over time at each voxel was computed.48 Following least-squares fitting of this model to the time series at each voxel, a sum of squares (SSQ) ratio statistic (ratio of the model component to the residual sum of squares) was estimated for the encoding and recall conditions relative to baseline. Significance of the estimated SSQ values at each voxel was determined by permutation tesing.49,50 Sum of squares ratio maps for each individual were transformed into standard stereotactic space,45,51 and group activation maps were computed for each group in each drug condition by determining the median SSQ ratio at each voxel (over all individuals) in the observed and permuted data maps. Group activation maps for each condition were compared against each other (placebo vs control and CBD vs placebo) using nonparametric repeated-measure analysis of variance.45 The voxelwise statistical threshold was set at P = .05, and the clusterwise thresholds were adjusted to ensure that the number of false-positive clusters per brain would be less than 1; regions that survived this critical statistical threshold and the corresponding P values are reported.
The BOLD response in each participant was modeled using only trials associated with correct responses in the recall condition. To test the hypothesis that activation in the CBD group would be intermediate between that of the control and placebo groups, we examined whether a linear relationship in brain activation (placebo group activation > CBD group activation > control group activation or placebo group activation < CBD group activation < control group activation) existed within the whole brain.
Recall performance was analyzed using repeated-measures analysis of variance. Correlational analysis between recall score and brain activation was conducted using 2-tailed Pearson test. Significance was set at a P value less than .05.
Results
There were no significant group differences between the placebo and control groups or the placebo and CBD groups in most demographic and clinical variables. However, the placebo group had fewer years of education than the control group (Table 1).
Table 1. Sociodemographic and Clinical Measures at Baseline.
| Characteristic | No. (%) | P Value | |||
|---|---|---|---|---|---|
| CBD (n = 16) | Placebo (n = 17) | Control (n = 19)a | Control vs Placebo | Placebo vs CBD | |
| Age, mean (SD), y | 22.43 (4.95) | 25.35 (5.24) | 23.89 (4.14) | .36 | .11 |
| Female | 6 (38) | 10 (59) | 8 (42) | .50 | .30 |
| Education, mean (SD), y | 14.50 (3.06) | 12.00 (3.69) | 16.94 (1.59) | .01 | .15 |
| CAARMS score, mean (SD) | |||||
| Positive symptoms | 40.19 (20.79) | 42.94 (29.46) | NA | NA | .75 |
| Negative symptoms | 23.25 (16.49) | 28.41 (20.49) | NA | NA | .43 |
| STAI-S, mean (SD) | 40.31 (9.06) | 38.94 (10.17) | NA | NA | .68 |
| Patients who made a transition to psychosis | 1 (6) | 1 (6) | NA | NA | >.99 |
| Urine drug screen results | NA | .45 | |||
| Clean | 10 (63) | 8 (47) | NAb | ||
| THC | 2 (13) | 5 (29) | NAb | ||
| Morphine | 1 (6) | 0 | NAb | ||
| Benzodiazepines | 0 | 1 (6) | NAb | ||
| PCP | 0 | 1 (6) | NAb | ||
| Missing | 3 (19) | 2 (12) | NAb | ||
| Cannabis use | |||||
| Lifetime use | 15 (94) | 17 (100) | NAc | NA | .48 |
| Current use | 7 (44) | 7 (41) | NAc | NA | >.99 |
| Cannabis use frequency | NA | .38 | |||
| More than once a week | 11 (69) | 12 (71) | NA | ||
| Once/twice monthly | 1 (6) | 3 (18) | NA | ||
| Few times a year | 2 (13) | 0 | NA | ||
| Only once/twice lifetime | 1 (6) | 2 (12) | NA | ||
| Alcohol use | |||||
| Lifetime use | 12 (75) | 13 (76) | NAd | NA | >.99 |
| Current use | 11 (69) | 10 (59) | NAd | NA | .59 |
| Alcohol use frequency | NA | .59 | |||
| Daily | 1 (6) | 2 (12) | NA | ||
| More than once a week | 4 (25) | 4 (24) | NA | ||
| Few times a month | 4 (25) | 3 (18) | NA | ||
| Few times a year | 3 (19) | 2 (12) | NA | ||
| Only once/twice lifetime | 0 | 2 (12) | NA | ||
| Nicotine use | |||||
| Lifetime use | 11 (69) | 7 (41) | NAe | NA | .16 |
| Current use | 9 (56) | 5 (29) | NAe | NA | >.99 |
| Nicotine use frequency | NA | .68 | |||
| Daily | 8 | 6 | NA | ||
| More than once a week | 2 | 1 | NA | ||
| Few times a month | 1 | 0 | NA | ||
| Total recall score, mean (SD) | 28.31 (2.91) | 27.62 (4.42) | 29.74 (2.51) | NAf | NAf |
Abbreviations: CAARMS, Comprehensive Assessment of At-Risk Mental States; CBD, cannabidiol; NA, not applicable; PCP, phencyclidine; STAI-S, State-Trait Anxiety Inventory–State Subscale; THC, Δ9-tetrahydrocannabinol.
Controls were selected to have minimal drug use and hence were not compared with participants at clinical high risk of psychosis on these parameters.
Controls tested negative on urine drug screen for all substances tested.
Cannabis use less than 10 times lifetime (no current users).
Lifetime users: 13; frequency: more than once a week, 5; few times a month, 3; and few times a year, 4.
Lifetime users: 5; current users: 2; frequency: daily, 2; few times a month, 1; few times a year, 1; and only once/twice lifetime, 1.
Analysis of variance: F2,48 = 1.84; P = .17.
fMRI Results
In control participants, relative to the baseline condition, the encoding condition was associated with activation in the left anterior cingulate cortex, the right caudate, the left precentral gyrus, and the cuneus (eTable 1 in Supplement 2). The recall condition relative to the baseline condition was associated with activation in the left parahippocampal and the left transverse temporal gyri and with decreased activation in the left middle occipital, the right lingual, and the inferior frontal gyri (eTable 2 in Supplement 2).
Differences in Activation Associated With the CHR State (Placebo vs Control)
Encoding
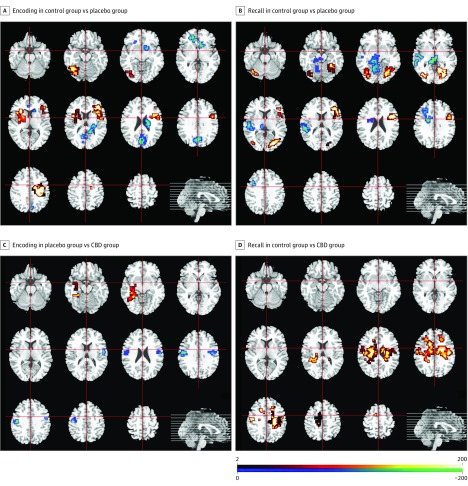
During the encoding condition, participants receiving placebo showed greater activation than control participants in the right middle frontal gyrus and adjacent parts of the inferior frontal gyrus and insula; the left insula/claustrum and the adjacent inferior frontal gyrus and putamen; the right precentral gyrus and the adjacent postcentral gyrus and inferior parietal lobule; and the left cerebellum and the adjacent lingual gyrus (Table 1; Figure 1A). Relative to participants in the placebo group, controls showed greater activation in the right subcallosal gyrus/caudate head; the left anterior cingulate; the right caudate tail extending to the posterior cingulate cortex; and in the right precuneus and cuneus (Table 2; Figure 1A).
Figure 1. Altered Brain Activation in Participants at Clinical High Risk of Psychosis.
A, Clusters showing greater (red/yellow) or reduced (blue/green) activation in participants at clinical high risk receiving placebo compared with healthy controls during the encoding condition. B, Clusters showing greater (red/yellow) or reduced (blue/green) activation in the placebo group compared with the control group during the recall condition. C, Clusters showing greater (red/yellow) or reduced (blue/green) activation in the placebo group compared with participants at clinical high risk receiving cannabidiol (CBD) during verbal encoding. D, Clusters showing greater (red/yellow) activation in the placebo group compared with the CBD group during the recall condition. The right side of the brain is shown on the right of the images.
Table 2. Differences in Activation Between 16 Participants at Clinical High Risk of Psychosis Receiving Placebo, 19 Healthy Controls, and 15 Participants Receiving Cannabidiol (CBD).
| Region | Coordinates of Peak (TAL) | Cluster Size, No. of Voxels | P Valuea | ||
|---|---|---|---|---|---|
| X | Y | Z | |||
| Verbal Encoding | |||||
| Placebo > control | |||||
| Middle frontal gyrus extending to inferior frontal gyrus and insula | 36 | 37 | 10 | 165 | <.001 |
| Claustrum/insula extending to inferior frontal gyrus and putamen |
−25 | 26 | 3 | 96 | .001 |
| Precentral gyrus extending to postcentral gyrus and inferior parietal lobule | 40 | −7 | 36 | 134 | <.001 |
| Left cerebellum extending to lingual gyrus | −40 | −67 | −16 | 77 | .001 |
| Placebo < control | |||||
| Subcallosal gyrus/caudate head | 14 | 11 | −10 | 72 | <.001 |
| Anterior cingulate | −4 | 41 | 0 | 18 | <.001 |
| Caudate tail extending to posterior cingulate cortex | 18 | −33 | 16 | 28 | <.001 |
| Precuneus extending to cuneus | 4 | −63 | 30 | 156 | <.001 |
| Placebo > CBD | |||||
| Parahippocampal gyrus extending to superior temporal gyrus and cerebellum | −29 | −30 | −13 | 75 | .003 |
| Placebo < CBD | |||||
| Precentral gyrus | 43 | −7 | 30 | 40 | .003 |
| Precentral gyrus | −40 | −11 | 36 | 72 | .001 |
| Verbal Recall | |||||
| Placebo > control | |||||
| Inferior frontal gyrus extending to middle frontal gyrus, insula, and precentral gyrus | 47 | 11 | 23 | 146 | <.001 |
| Cuneus extending to fusiform gyrus, lingual gyrus, and posterior cingulate cortex | 29 | −74 | 7 | 196 | <.001 |
| Cerebellum extending to middle occipital gyrus and fusiform gyrus | −36 | −63 | −13 | 83 | .002 |
| Placebo < control | |||||
| Parahippocampal gyrus extending to midbrain, cerebellum, and thalamus | −18 | −26 | −13 | 131 | <.001 |
| Superior temporal gyrus extending to the middle temporal gyrus | −50 | −18 | 0 | 80 | <.001 |
| Superior temporal gyrus extending to the transverse temporal gyrus | −50 | −30 | 13 | 33 | .003 |
| Middle frontal gyrus | −25 | 11 | 33 | 57 | .003 |
| Placebo < CBD | |||||
| Cingulate gyrus extending to body of caudate | −14 | 15 | 30 | 365 | <.001 |
| Precentral gyrus extending to cingulate gyrus | 43 | −18 | 33 | 362 | <.001 |
| Medial frontal gyrus | −7 | 0 | 49 | 61 | .002 |
Abbreviation: TAL, Talairach coordinate system.
Corrected for less than 1 false-positive cluster.
Recall
During the recall condition, participants receiving placebo showed greater activation than controls in clusters encompassing the right inferior frontal, middle frontal, and precentral gyri and the insula; the right cuneus, fusiform, and lingual gyri and the posterior cingulate gyri; and the left cerebellum and middle occipital and fusiform gyri (Table 2; Figure 1B). Controls showed greater activation in 4 clusters in the left hemisphere. These involved the parahippocampal gyrus, the midbrain, the cerebellum, and the thalamus; the superior temporal and middle temporal gyri; the superior and transverse temporal gyri; and the middle frontal gyrus (Table 2; Figure 1B).
Effect of CBD on Activation in Participants at CHR (CBD vs Placebo)
Encoding
During the encoding condition, participants at CHR in the placebo group showed greater activation than those in the CBD group in a cluster in the left parahippocampal gyrus that extended into the superior temporal gyrus and the cerebellum. However, participants in the placebo group showed less activation than those in the CBD group in the precentral gyri (Table 2; Figure 1C).
Recall
During the recall condition, participants in the placebo group showed less activation than those in the CBD group in 3 clusters, with foci in the left cingulate gyrus and the adjacent body of caudate; the right precentral gyrus extending to the cingulate gyrus; and in the medial frontal gyrus (Table 2; Figure 1D). There were no clusters of greater activation in the placebo group compared with the CBD group.
Between-Group Linear Analysis
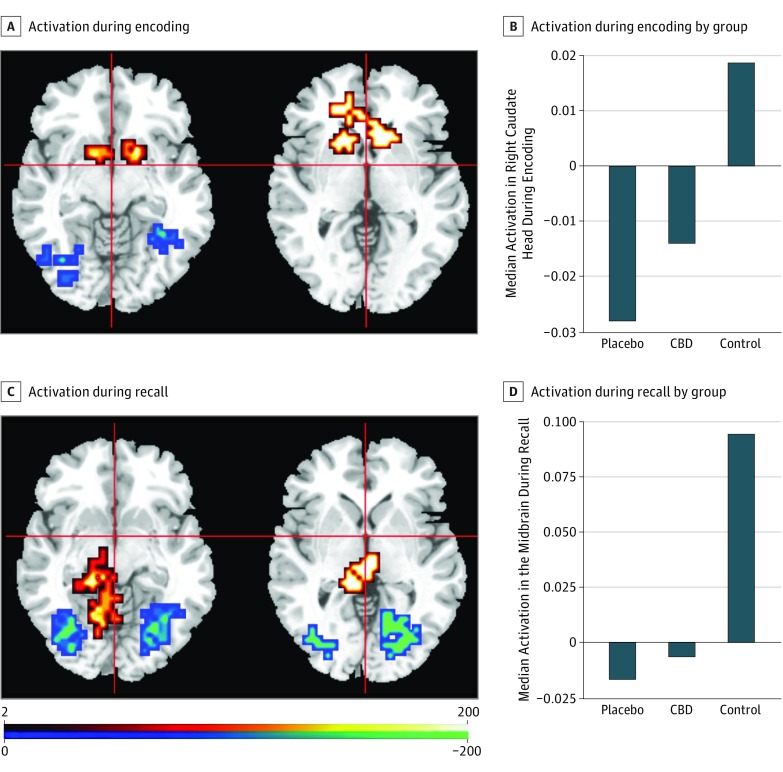
This analysis identified clusters where there was a linear pattern of activation across the 3 groups of participants. In these clusters, activation in the CBD group was intermediate to that in the placebo and control groups.
Encoding
There were 7 clusters where encoding-related engagement was greatest in the placebo group, lowest in the control group, and at an intermediate level in the CBD group. These involved the right inferior frontal and middle frontal gyri and the insula; the left insula and putamen; 3 clusters in the precentral gyri; the right fusiform gyrus and adjacent cerebellum; and the left cerebellum and fusiform gyrus (Table 3; Figure 2A and B) (eFigure 3 in Supplement 2). The right inferior frontal gyrus, left insula, and precentral clusters overlapped with the regions where participants receiving placebo showed increased activation during encoding relative to the control group in the earlier paired comparison.
Table 3. Linear Relationship in Activation Across 16 Participants at Clinical High Risk of Psychosis Receiving Placebo, 19 Healthy Controls, and 15 Participants Receiving Cannabidiol (CBD).
| Region | Coordinates of Peak (TAL) | Cluster Size, No. of Voxels | P Valuea | ||
|---|---|---|---|---|---|
| X | Y | Z | |||
| Verbal Encoding | |||||
| Placebo > CBD > control | |||||
| Inferior frontal gyrus extending to middle frontal gyrus and insula | 40 | 37 | 10 | 135 | <.001 |
| Insula extending to putamen | −36 | 11 | 10 | 112 | <.001 |
| Precentral gyrus | −40 | −11 | 30 | 39 | .004 |
| Precentral gyrus | −51 | −4 | 16 | 34 | .003 |
| Precentral gyrus | 40 | −11 | 39 | 124 | <.001 |
| Fusiform gyrus extending to cerebellum | 43 | −44 | −13 | 53 | .003 |
| Cerebellum extending to fusiform gyrus | −22 | −52 | −16 | 100 | <.001 |
| Placebo < CBD < control | |||||
| Caudate head extending to anterior | −14 | 22 | 0 | 44 | .004 |
| Subcallosal gyrus/caudate head | 14 | 11 | −10 | 87 | .001 |
| Caudate tail extending to posterior cingulate | 18 | −37 | 13 | 65 | .004 |
| Precuneus extending to cuneus | 4 | −63 | 30 | 185 | <.001 |
| Verbal Recall | |||||
| Placebo > CBD > control | |||||
| Inferior frontal gyrus extending to middle frontal gyrus and insula | 47 | 11 | 23 | 120 | <.001 |
| Precuneus extending to cuneus, lingual, middle occipital, and fusiform gyri and cerebellum | 25 | −74 | 7 | 176 | <.001 |
| Cerebellum extending to fusiform, lingual, and inferior occipital gyri | −36 | −63 | −13 | 73 | .002 |
| Placebo < CBD < control | |||||
| Parahippocampal gyrus extending to midbrain and cerebellum | −18 | −26 | −13 | 82 | .001 |
| Thalamus | −7 | −26 | −3 | 33 | .003 |
| Transverse temporal gyrus extending to superior temporal gyrus | −50 | −26 | 13 | 33 | .004 |
| Precentral gyrus extending to cingulate gyrus and body of caudate | −36 | 18 | 36 | 60 | .002 |
Abbreviation: TAL, Talairach coordinate system.
Corrected for less than 1 false-positive cluster.
Figure 2. Effect of Cannabidiol (CBD) on Brain Activation Compared With Placebo in Participants at Clinical High Risk of Psychosis and Healthy Control Participants.
A, Clusters where activation during encoding differed across the 3 groups in a linear relationship. In the head of caudate (red/yellow), activation was greatest in healthy controls, lowest in participants at clinical high risk receiving placebo, and intermediate in participants at clinical high risk receiving CBD. The opposite pattern was seen in occipital regions (blue). B, Activation in each group in the right caudate head during encoding in arbitrary units as indexed using the median sum of squares ratio. The sum of squares ratio statistic refers to the ratio of the sum of squares of deviations from the mean image intensity due to the model (over the whole time series) to the sum of squares of deviations due to the residuals. C, Clusters where there was a linear group difference in activation during recall. In the parahippocampal region and midbrain (red/yellow), activation was greatest in controls, lowest in those receiving placebo, and intermediate in those receiving CBD. The opposite pattern was seen in occipital regions (blue). D, Median activation in each group in the midbrain during recall in arbitrary units as indexed using the median sum of squares ratio. The right side of the brain is shown on the right of the images.
There were 4 clusters where there was a linear between-group relationship in the opposite direction (ie, lowest in the placebo group, highest in the control group, and at an intermediate level in the CBD group). These involved the left caudate head and putamen and the anterior cingulate cortex; the right subcallosal gyrus and caudate head; the tail of the right caudate and adjacent posterior cingulate cortex; and the precuneus and right cuneus (Table 3; Figure 2A and B) (eFigure 3 in Supplement 2). All 4 clusters overlapped with clusters where controls had shown greater activation than the placebo group during encoding in the previous paired comparison.
Recall
In 3 clusters, recall-related engagement was greatest in participants receiving placebo, lowest in controls, and at an intermediate level in participants receiving CBD. These clusters comprised the right inferior frontal gyrus extending to the ipsilateral middle frontal gyrus and insula; the precuneus extending to the cuneus, lingual, middle occipital, and fusiform gyri and the cerebellum on the right side; and the cerebellum extending to the fusiform, lingual, and inferior occipital gyri on the left side (Table 3; Figure 2C and D) (eFigure 3 in Supplement 2). All 3 clusters overlapped with clusters where the placebo group had shown greater activation than controls during recall in the paired comparison.
Conversely, there were 4 clusters where activation was lowest in the placebo group, greatest in the control group, and at an intermediate level in the CBD group. These included the left parahippocampal gyrus, the midbrain, and the cerebellum; the left thalamus; the left transverse temporal gyrus extending to the superior temporal gyrus; and the left precentral and cingulate gyri and caudate body (Table 3; Figure 2C and D) (eFigure 3 in Supplement 2). The left parahippocampal gyrus and transverse temporal gyrus clusters overlapped with clusters where controls had shown greater activation than participants receiving placebo during recall in the paired group comparison.
Relationship Between Recall Performance and Brain Activation
Across all participants, the total recall score was directly correlated with the level of left parahippocampal activation during recall (r = 0.28; P = .046) (eResults in Supplement 2).
Discussion
As expected and in line with data from previous neuroimaging comparisons of participants at CHR of psychosis with controls,52,53,54 we found that under placebo conditions, participants at CHR showed differential activation relative to controls in several regions. These regions of differential response included the 3 areas thought to be critical to the pathophysiology of the CHR state: the striatum (during verbal encoding) and the MTL and midbrain (during verbal recall).
To test our main hypothesis, we identified regions where there was a linear pattern of activation across the 3 groups such that the level of activation in participants at CHR receiving CBD was intermediate to that of participants at CHR receiving placebo and control participants. We found that this pattern of differential activation was evident in the striatum during encoding and in the parahippocampal cortex and midbrain during recall. Moreover, these regions of differential activation overlapped with the areas where participants at CHR receiving placebo had shown altered activation in the paired comparison with controls. These findings suggest that during verbal encoding, the administration of a single dose of CBD attenuated the reduction in the striatal response evident in participants at CHR receiving placebo relative to controls. Similarly, administration of CBD appeared to attenuate the reduction in the parahippocampal and midbrain responses during verbal recall that was seen in participants receiving placebo relative to controls. Although this interpretation is cautious because the findings are based on cross-sectional as opposed to within-participant comparisons, these data suggest that in these regions, CBD may partially normalize responses to verbal encoding and recall in individuals at CHR. As there were no significant differences in memory performance, this differential activation was not attributable to differential task performance.
Short-term effects of CBD on responses in these areas in participants at CHR are consistent with previous data from 2 studies that used a single dose of CBD in healthy volunteers.17,18 These studies indicated that in controls, CBD augmented parahippocampal and striatal activation during the same learning task17 as used in the present study and had a similar effect on parahippocampal and striatal responses during an attentional salience task.18 In both of these studies, the administration of a single dose of THC induced transient psychotic symptoms, and the effect of THC on parahippocampal and striatal activation was the opposite to that of CBD.
Preclinical models suggest that overactivity in the MTL region drives subcortical dopamine dysfunction through projections to the striatum and midbrain.55,56 Moreover, neuroimaging studies in individuals at CHR indicate that the subsequent onset of psychosis is linked to alterations in MTL structure31 and function32,34 and to elevated striatal and midbrain dopamine function.57,58,59 Effects of CBD on parahippocampal, striatal, and midbrain function in participants at CHR are thus of particular interest, as these areas may play a critical role in the pathophysiology of psychosis.30 A partial normalization of dysfunction in these regions could contribute to the therapeutic effects of CBD that have been reported in patients with psychosis26,27 and anxiety disorders.25
The molecular mechanism of action that may underlie the effects of CBD in individuals at CHR is unclear. Cannabidiol has effects on a number of signaling pathways,11,60,61 including on the CB1 receptors,62,63 and may modulate glutamatergic neurotransmission, particularly in the hippocampus, through multiple pathways64,65,66 and striatal glutamatergic and CB1 receptor expression.67 In patients with psychosis, the effects of CBD on psychotic symptoms have been associated with its influence on levels of the endogenous cannabinoid anandamide.26 Therefore, future studies need to investigate the neurochemical and receptor-level mechanisms that may underlie the antipsychotic effects of CBD.
Across all participants, the level of activation in the left parahippocampal cortex during verbal recall was directly correlated with total recall score during the task, consistent with the key role of this region in relational memory binding and retrieval68,69 and in supporting association-based recall.70 Attenuated parahippocampal engagement in participants receiving placebo is consistent with meta-analytic and independent evidence from studies in patients with established psychotic disorders, such as schizophrenia,71,72,73 and in studies in those at clinical34,74 and familial/genetic73,75 risk of psychosis (eDiscussion in Supplement 2).
Limitations
Our study had limitations. The most elegant way to investigate the short-term effects of CBD on psychotic symptoms would have been to use a within-participant, repeated-measures design as it would have allowed us to properly test whether a single dose of CBD normalizes the dysfunction in brain regions linked to psychosis. However, while such a design would have been ideal as opposed to a cross-sectional design, as in our previous studies using CBD in healthy volunteers,17,18,19 it would have been difficult to scan participants at CHR twice under 2 different drug conditions. The participants at CHR who were investigated in the CBD arm in the present study were not compared with the same participants while they were receiving placebo treatment but were instead compared with a separate group of participants at CHR receiving placebo. As a result, we cannot be certain that CBD effects in the striatum, parahippocampal cortex, and midbrain in participants receiving CBD (that we have shown as being intermediate compared with the placebo and control groups) reflected a partial normalization of dysfunction in these regions that predated CBD treatment. Therefore, this needs confirmation in future studies using a within-subject, repeated-measures design and with the same individuals at CHR tested with both placebo and CBD treatment. Nevertheless, it is worth noting that the 2 CHR groups were comparable on various demographic and clinical measures at baseline, and we were able to define regions where participants at CHR showed altered activation while receiving placebo relative to controls and then showed that administration of CBD modulated activation in a subset of these regions.
We were also unable to examine whether the effects of CBD differed between participants at CHR who later transitioned to psychosis compared with those who did not because only 1 patient transitioned per treatment arm. Future studies may investigate this in independent, larger cohorts or if more patients transition to psychosis from the present sample.
Another important caveat worth considering relates to the rapid changes in cerebral perfusion that are known to occur with a single dose of psychoactive drugs, such as antipsychotic medications.76,77 Therefore, one cannot be certain whether the short-term effects of CBD observed here are consequences of its effects on local neuronal activity during the fMRI task as opposed to more general effects on cerebral blood flow. The fMRI acquisition and data analysis steps were designed to control for any nonspecific/generalized effects of CBD on regional perfusion, as we compared the effects of CBD during an active task condition (eg, encoding or recall) with its effects during a control (baseline) condition. While there is no reason to think that the short-term effects of CBD on regional perfusion would differ systematically between different task conditions, we cannot completely rule out this possibility. It is also unclear whether the effects of CBD will persist after longer-term dosing. Therefore, future studies investigating the effects of sustained dosing with CBD are warranted.
Finally, although we did not find an effect of CBD on memory task performance, we used a relatively easy verbal learning task, and the study was not powered to demonstrate differences at a behavioral level. A 2018 study27 in patients with schizophrenia found a trend for improved cognitive performance after 6 weeks of treatment with CBD, but the present study involved a single dose of CBD, and cognitive deficits in individuals at CHR are less severe than in patients with psychosis.78
Conclusions
This study suggests that a single dose of CBD in an experimental setting may partially normalize dysfunction in the MTL, striatum, and midbrain in individuals at CHR of psychosis. It would be useful to now investigate whether similar modulatory effects are evident in patients who have received a course of treatment with CBD in a clinical setting.
Trial protocol.
eMethods.
eFigure 1. CONSORT flow diagram.
eFigure 2. Plot showing CBD plasma levels in placebo and CBD arms.
eFigure 3. Acute effect of CBD on brain activation.
eResults.
eTable 1. Task-related activation during the encoding condition relative to baseline in healthy controls (n = 19).
eTable 2. Task-related activation during the recall condition relative to baseline in healthy controls (n = 19).
eDiscussion.
References
- 1.Moore TH, Zammit S, Lingford-Hughes A, et al. . Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328. doi: 10.1016/S0140-6736(07)61162-3 [DOI] [PubMed] [Google Scholar]
- 2.Schoeler T, Monk A, Sami MB, et al. . Continued versus discontinued cannabis use in patients with psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3(3):215-225. doi: 10.1016/S2215-0366(15)00363-6 [DOI] [PubMed] [Google Scholar]
- 3.Schoeler T, Petros N, Di Forti M, et al. . Effects of continuation, frequency, and type of cannabis use on relapse in the first 2 years after onset of psychosis: an observational study. Lancet Psychiatry. 2016;3(10):947-953. doi: 10.1016/S2215-0366(16)30188-2 [DOI] [PubMed] [Google Scholar]
- 4.Schoeler T, Petros N, Di Forti M, et al. . Association between continued cannabis use and risk of relapse in first-episode psychosis: a quasi-experimental investigation within an observational study. JAMA Psychiatry. 2016;73(11):1173-1179. doi: 10.1001/jamapsychiatry.2016.2427 [DOI] [PubMed] [Google Scholar]
- 5.Appiah-Kusi E, Leyden E, Parmar S, Mondelli V, McGuire P, Bhattacharyya S. Abnormalities in neuroendocrine stress response in psychosis: the role of endocannabinoids. Psychol Med. 2016;46(1):27-45. doi: 10.1017/S0033291715001786 [DOI] [PubMed] [Google Scholar]
- 6.Ranganathan M, Cortes-Briones J, Radhakrishnan R, et al. . Reduced brain cannabinoid receptor availability in schizophrenia. Biol Psychiatry. 2016;79(12):997-1005. doi: 10.1016/j.biopsych.2015.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leweke FM, Mueller JK, Lange B, Rohleder C. Therapeutic potential of cannabinoids in psychosis. Biol Psychiatry. 2016;79(7):604-612. doi: 10.1016/j.biopsych.2015.11.018 [DOI] [PubMed] [Google Scholar]
- 8.Zuardi AW. Cannabidiol: from an inactive cannabinoid to a drug with wide spectrum of action. Rev Bras Psiquiatr. 2008;30(3):271-280. doi: 10.1590/S1516-44462008000300015 [DOI] [PubMed] [Google Scholar]
- 9.Eggan SM, Lewis DA. Immunocytochemical distribution of the cannabinoid CB1 receptor in the primate neocortex: a regional and laminar analysis. Cereb Cortex. 2007;17(1):175-191. doi: 10.1093/cercor/bhj136 [DOI] [PubMed] [Google Scholar]
- 10.Glass M, Dragunow M, Faull RL. Cannabinoid receptors in the human brain: a detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77(2):299-318. doi: 10.1016/S0306-4522(96)00428-9 [DOI] [PubMed] [Google Scholar]
- 11.Pertwee RG. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol. 2008;153(2):199-215. doi: 10.1038/sj.bjp.0707442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D’Souza DC, Perry E, MacDougall L, et al. . The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29(8):1558-1572. doi: 10.1038/sj.npp.1300496 [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharyya S, Fusar-Poli P, Borgwardt S, et al. . Modulation of mediotemporal and ventrostriatal function in humans by Delta9-tetrahydrocannabinol: a neural basis for the effects of Cannabis sativa on learning and psychosis. Arch Gen Psychiatry. 2009;66(4):442-451. doi: 10.1001/archgenpsychiatry.2009.17 [DOI] [PubMed] [Google Scholar]
- 14.Bhattacharyya S, Atakan Z, Martin-Santos R, et al. . Preliminary report of biological basis of sensitivity to the effects of cannabis on psychosis: AKT1 and DAT1 genotype modulates the effects of δ-9-tetrahydrocannabinol on midbrain and striatal function. Mol Psychiatry. 2012;17(12):1152-1155. doi: 10.1038/mp.2011.187 [DOI] [PubMed] [Google Scholar]
- 15.D’Souza DC, Abi-Saab WM, Madonick S, et al. . Delta-9-tetrahydrocannabinol effects in schizophrenia: implications for cognition, psychosis, and addiction. Biol Psychiatry. 2005;57(6):594-608. doi: 10.1016/j.biopsych.2004.12.006 [DOI] [PubMed] [Google Scholar]
- 16.D’Souza DC, Sewell RA, Ranganathan M. Cannabis and psychosis/schizophrenia: human studies. Eur Arch Psychiatry Clin Neurosci. 2009;259(7):413-431. doi: 10.1007/s00406-009-0024-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhattacharyya S, Morrison PD, Fusar-Poli P, et al. . Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology. 2010;35(3):764-774. doi: 10.1038/npp.2009.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhattacharyya S, Crippa JA, Allen P, et al. . Induction of psychosis by Δ9-tetrahydrocannabinol reflects modulation of prefrontal and striatal function during attentional salience processing. Arch Gen Psychiatry. 2012;69(1):27-36. doi: 10.1001/archgenpsychiatry.2011.161 [DOI] [PubMed] [Google Scholar]
- 19.Bhattacharyya S, Falkenberg I, Martin-Santos R, et al. . Cannabinoid modulation of functional connectivity within regions processing attentional salience. Neuropsychopharmacology. 2015;40(6):1343-1352. doi: 10.1038/npp.2014.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Englund A, Morrison PD, Nottage J, et al. . Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment. J Psychopharmacol. 2013;27(1):19-27. doi: 10.1177/0269881112460109 [DOI] [PubMed] [Google Scholar]
- 21.Hindocha C, Freeman TP, Schafer G, et al. . Acute effects of delta-9-tetrahydrocannabinol, cannabidiol and their combination on facial emotion recognition: a randomised, double-blind, placebo-controlled study in cannabis users. Eur Neuropsychopharmacol. 2015;25(3):325-334. doi: 10.1016/j.euroneuro.2014.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morgan CJ, Curran HV. Effects of cannabidiol on schizophrenia-like symptoms in people who use cannabis. Br J Psychiatry. 2008;192(4):306-307. doi: 10.1192/bjp.bp.107.046649 [DOI] [PubMed] [Google Scholar]
- 23.Morgan CJ, Schafer G, Freeman TP, Curran HV. Impact of cannabidiol on the acute memory and psychotomimetic effects of smoked cannabis: naturalistic study: naturalistic study [published correction appears in Br J Psychiatry. 2010;197:416]. Br J Psychiatry. 2010;197(4):285-290. doi: 10.1192/bjp.bp.110.077503 [DOI] [PubMed] [Google Scholar]
- 24.Bergamaschi MM, Queiroz RH, Chagas MH, et al. . Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology. 2011;36(6):1219-1226. doi: 10.1038/npp.2011.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crippa JA, Derenusson GN, Ferrari TB, et al. . Neural basis of anxiolytic effects of cannabidiol (CBD) in generalized social anxiety disorder: a preliminary report. J Psychopharmacol. 2011;25(1):121-130. doi: 10.1177/0269881110379283 [DOI] [PubMed] [Google Scholar]
- 26.Leweke FM, Piomelli D, Pahlisch F, et al. . Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2:e94. doi: 10.1038/tp.2012.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGuire P, Robson P, Cubala WJ, et al. . Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225-231. doi: 10.1176/appi.ajp.2017.17030325 [DOI] [PubMed] [Google Scholar]
- 28.Yung AR, Yuen HP, McGorry PD, et al. . Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39(11-12):964-971. doi: 10.1080/j.1440-1614.2005.01714.x [DOI] [PubMed] [Google Scholar]
- 29.Falkenberg I, Valmaggia L, Byrnes M, et al. . Why are help-seeking subjects at ultra-high risk for psychosis help-seeking? Psychiatry Res. 2015;228(3):808-815. doi: 10.1016/j.psychres.2015.05.018 [DOI] [PubMed] [Google Scholar]
- 30.Modinos G, Allen P, Grace AA, McGuire P. Translating the MAM model of psychosis to humans. Trends Neurosci. 2015;38(3):129-138. doi: 10.1016/j.tins.2014.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mechelli A, Riecher-Rössler A, Meisenzahl EM, et al. . Neuroanatomical abnormalities that predate the onset of psychosis: a multicenter study. Arch Gen Psychiatry. 2011;68(5):489-495. doi: 10.1001/archgenpsychiatry.2011.42 [DOI] [PubMed] [Google Scholar]
- 32.Allen P, Azis M, Modinos G, et al. . Increased resting hippocampal and basal ganglia perfusion in people at ultra high risk for psychosis: replication in a second cohort [published online December 27, 2017]. Schizophr Bull. doi: 10.1093/schbul/sbx169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Allen P, Chaddock CA, Egerton A, et al. . Resting hyperperfusion of the hippocampus, midbrain, and basal ganglia in people at high risk for psychosis. Am J Psychiatry. 2016;173(4):392-399. doi: 10.1176/appi.ajp.2015.15040485 [DOI] [PubMed] [Google Scholar]
- 34.Allen P, Chaddock CA, Howes OD, et al. . Abnormal relationship between medial temporal lobe and subcortical dopamine function in people with an ultra high risk for psychosis. Schizophr Bull. 2012;38(5):1040-1049. doi: 10.1093/schbul/sbr017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Squire LR, Zola SM. Structure and function of declarative and nondeclarative memory systems. Proc Natl Acad Sci U S A. 1996;93(24):13515-13522. doi: 10.1073/pnas.93.24.13515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.D’Ardenne K, Eshel N, Luka J, Lenartowicz A, Nystrom LE, Cohen JD. Role of prefrontal cortex and the midbrain dopamine system in working memory updating. Proc Natl Acad Sci U S A. 2012;109(49):19900-19909. doi: 10.1073/pnas.1116727109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schott BH, Seidenbecher CI, Fenker DB, et al. . The dopaminergic midbrain participates in human episodic memory formation: evidence from genetic imaging. J Neurosci. 2006;26(5):1407-1417. doi: 10.1523/JNEUROSCI.3463-05.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schott BH, Sellner DB, Lauer CJ, et al. . Activation of midbrain structures by associative novelty and the formation of explicit memory in humans. Learn Mem. 2004;11(4):383-387. doi: 10.1101/lm.75004 [DOI] [PubMed] [Google Scholar]
- 39.Murty VP, Sambataro F, Radulescu E, et al. . Selective updating of working memory content modulates meso-cortico-striatal activity. Neuroimage. 2011;57(3):1264-1272. doi: 10.1016/j.neuroimage.2011.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lewis SJ, Dove A, Robbins TW, Barker RA, Owen AM. Striatal contributions to working memory: a functional magnetic resonance imaging study in humans. Eur J Neurosci. 2004;19(3):755-760. doi: 10.1111/j.1460-9568.2004.03108.x [DOI] [PubMed] [Google Scholar]
- 41.Dahlin E, Neely AS, Larsson A, Bäckman L, Nyberg L. Transfer of learning after updating training mediated by the striatum. Science. 2008;320(5882):1510-1512. doi: 10.1126/science.1155466 [DOI] [PubMed] [Google Scholar]
- 42.McNab F, Klingberg T. Prefrontal cortex and basal ganglia control access to working memory. Nat Neurosci. 2008;11(1):103-107. doi: 10.1038/nn2024 [DOI] [PubMed] [Google Scholar]
- 43.Landau SM, Lal R, O’Neil JP, Baker S, Jagust WJ. Striatal dopamine and working memory. Cereb Cortex. 2009;19(2):445-454. doi: 10.1093/cercor/bhn095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spielberger CD. Manual for the State/Trait Anxiety Inventory (Form Y) (Self Evaluation Questionnaire). Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 45.Brammer MJ, Bullmore ET, Simmons A, et al. . Generic brain activation mapping in functional magnetic resonance imaging: a nonparametric approach. Magn Reson Imaging. 1997;15(7):763-770. doi: 10.1016/S0730-725X(97)00135-5 [DOI] [PubMed] [Google Scholar]
- 46.Thirion B, Pinel P, Mériaux S, Roche A, Dehaene S, Poline JB. Analysis of a large fMRI cohort: statistical and methodological issues for group analyses. Neuroimage. 2007;35(1):105-120. doi: 10.1016/j.neuroimage.2006.11.054 [DOI] [PubMed] [Google Scholar]
- 47.Bullmore ET, Brammer MJ, Rabe-Hesketh S, et al. . Methods for diagnosis and treatment of stimulus-correlated motion in generic brain activation studies using fMRI. Hum Brain Mapp. 1999;7(1):38-48. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Friman O, Borga M, Lundberg P, Knutsson H. Adaptive analysis of fMRI data. Neuroimage. 2003;19(3):837-845. doi: 10.1016/S1053-8119(03)00077-6 [DOI] [PubMed] [Google Scholar]
- 49.Bullmore E, Long C, Suckling J, et al. . Colored noise and computational inference in neurophysiological (fMRI) time series analysis: resampling methods in time and wavelet domains. Hum Brain Mapp. 2001;12(2):61-78. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bullmore ET, Suckling J, Overmeyer S, Rabe-Hesketh S, Taylor E, Brammer MJ. Global, voxel, and cluster tests, by theory and permutation, for a difference between two groups of structural MR images of the brain. IEEE Trans Med Imaging. 1999;18(1):32-42. doi: 10.1109/42.750253 [DOI] [PubMed] [Google Scholar]
- 51.Talairach J, Tournoux P. Co-planar Stereotaxic Atlas of the Human Brain: 3-D Proportional System: An Approach to Cerebral Imaging. New York, NY: Thieme Medical; 1988. [Google Scholar]
- 52.Dutt A, Tseng HH, Fonville L, et al. . Exploring neural dysfunction in ‘clinical high risk’ for psychosis: a quantitative review of fMRI studies. J Psychiatr Res. 2015;61:122-134. doi: 10.1016/j.jpsychires.2014.08.018 [DOI] [PubMed] [Google Scholar]
- 53.Gifford G, Crossley N, Fusar-Poli P, et al. . Using neuroimaging to help predict the onset of psychosis. Neuroimage. 2017;145(pt B):209-217. doi: 10.1016/j.neuroimage.2016.03.075 [DOI] [PubMed] [Google Scholar]
- 54.Hager BM, Keshavan MS. Neuroimaging biomarkers for psychosis. Curr Behav Neurosci Rep. 2015;2015:1-10. [PMC free article] [PubMed] [Google Scholar]
- 55.Grace AA. Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression. Nat Rev Neurosci. 2016;17(8):524-532. doi: 10.1038/nrn.2016.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lodge DJ, Grace AA. Aberrant hippocampal activity underlies the dopamine dysregulation in an animal model of schizophrenia. J Neurosci. 2007;27(42):11424-11430. doi: 10.1523/JNEUROSCI.2847-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Allen P, Luigjes J, Howes OD, et al. . Transition to psychosis associated with prefrontal and subcortical dysfunction in ultra high-risk individuals. Schizophr Bull. 2012;38(6):1268-1276. doi: 10.1093/schbul/sbr194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Howes O, Bose S, Turkheimer F, et al. . Progressive increase in striatal dopamine synthesis capacity as patients develop psychosis: a PET study. Mol Psychiatry. 2011;16(9):885-886. doi: 10.1038/mp.2011.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Howes OD, Bose SK, Turkheimer F, et al. . Dopamine synthesis capacity before onset of psychosis: a prospective [18F]-DOPA PET imaging study. Am J Psychiatry. 2011;168(12):1311-1317. doi: 10.1176/appi.ajp.2011.11010160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Katona I. Cannabis and endocannabinoid signaling in epilepsy. Handb Exp Pharmacol. 2015;231:285-316. doi: 10.1007/978-3-319-20825-1_10 [DOI] [PubMed] [Google Scholar]
- 61.Iseger TA, Bossong MG. A systematic review of the antipsychotic properties of cannabidiol in humans. Schizophr Res. 2015;162(1-3):153-161. doi: 10.1016/j.schres.2015.01.033 [DOI] [PubMed] [Google Scholar]
- 62.Bisogno T, Hanus L, De Petrocellis L, et al. . Molecular targets for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol. 2001;134(4):845-852. doi: 10.1038/sj.bjp.0704327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thomas A, Baillie GL, Phillips AM, Razdan RK, Ross RA, Pertwee RG. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol. 2007;150(5):613-623. doi: 10.1038/sj.bjp.0707133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sylantyev S, Jensen TP, Ross RA, Rusakov DA. Cannabinoid- and lysophosphatidylinositol-sensitive receptor GPR55 boosts neurotransmitter release at central synapses. Proc Natl Acad Sci U S A. 2013;110(13):5193-5198. doi: 10.1073/pnas.1211204110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ledgerwood CJ, Greenwood SM, Brett RR, Pratt JA, Bushell TJ. Cannabidiol inhibits synaptic transmission in rat hippocampal cultures and slices via multiple receptor pathways. Br J Pharmacol. 2011;162(1):286-294. doi: 10.1111/j.1476-5381.2010.01015.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Linge R, Jiménez-Sánchez L, Campa L, et al. . Cannabidiol induces rapid-acting antidepressant-like effects and enhances cortical 5-HT/glutamate neurotransmission: role of 5-HT1A receptors. Neuropharmacology. 2016;103:16-26. doi: 10.1016/j.neuropharm.2015.12.017 [DOI] [PubMed] [Google Scholar]
- 67.Ren Y, Whittard J, Higuera-Matas A, Morris CV, Hurd YL. Cannabidiol, a nonpsychotropic component of cannabis, inhibits cue-induced heroin seeking and normalizes discrete mesolimbic neuronal disturbances. J Neurosci. 2009;29(47):14764-14769. doi: 10.1523/JNEUROSCI.4291-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Eichenbaum H, Yonelinas AP, Ranganath C. The medial temporal lobe and recognition memory. Annu Rev Neurosci. 2007;30:123-152. doi: 10.1146/annurev.neuro.30.051606.094328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang WC, Yonelinas AP, Ranganath C. Dissociable neural correlates of item and context retrieval in the medial temporal lobes. Behav Brain Res. 2013;254:102-107. doi: 10.1016/j.bbr.2013.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yonelinas AP, Hopfinger JB, Buonocore MH, Kroll NE, Baynes K. Hippocampal, parahippocampal and occipital-temporal contributions to associative and item recognition memory: an fMRI study. Neuroreport. 2001;12(2):359-363. doi: 10.1097/00001756-200102120-00035 [DOI] [PubMed] [Google Scholar]
- 71.Cirillo MA, Seidman LJ. Verbal declarative memory dysfunction in schizophrenia: from clinical assessment to genetics and brain mechanisms. Neuropsychol Rev. 2003;13(2):43-77. doi: 10.1023/A:1023870821631 [DOI] [PubMed] [Google Scholar]
- 72.Lepage M, Montoya A, Pelletier M, Achim AM, Menear M, Lal S. Associative memory encoding and recognition in schizophrenia: an event-related fMRI study. Biol Psychiatry. 2006;60(11):1215-1223. doi: 10.1016/j.biopsych.2006.03.043 [DOI] [PubMed] [Google Scholar]
- 73.Rasetti R, Mattay VS, White MG, et al. . Altered hippocampal-parahippocampal function during stimulus encoding: a potential indicator of genetic liability for schizophrenia. JAMA Psychiatry. 2014;71(3):236-247. doi: 10.1001/jamapsychiatry.2013.3911 [DOI] [PubMed] [Google Scholar]
- 74.Valli I, Stone J, Mechelli A, et al. . Altered medial temporal activation related to local glutamate levels in subjects with prodromal signs of psychosis. Biol Psychiatry. 2011;69(1):97-99. doi: 10.1016/j.biopsych.2010.08.033 [DOI] [PubMed] [Google Scholar]
- 75.Thermenos HW, Seidman LJ, Poldrack RA, et al. . Elaborative verbal encoding and altered anterior parahippocampal activation in adolescents and young adults at genetic risk for schizophrenia using FMRI. Biol Psychiatry. 2007;61(4):564-574. doi: 10.1016/j.biopsych.2006.04.044 [DOI] [PubMed] [Google Scholar]
- 76.Hawkins PCT, Wood TC, Vernon AC, et al. . An investigation of regional cerebral blood flow and tissue structure changes after acute administration of antipsychotics in healthy male volunteers. Hum Brain Mapp. 2018;39(1):319-331. doi: 10.1002/hbm.23844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lahti AC, Weiler MA, Medoff DR, Tamminga CA, Holcomb HH. Functional effects of single dose first- and second-generation antipsychotic administration in subjects with schizophrenia. Psychiatry Res. 2005;139(1):19-30. doi: 10.1016/j.pscychresns.2005.02.006 [DOI] [PubMed] [Google Scholar]
- 78.Simon AE, Cattapan-Ludewig K, Zmilacher S, et al. . Cognitive functioning in the schizophrenia prodrome. Schizophr Bull. 2007;33(3):761-771. doi: 10.1093/schbul/sbm018 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol.
eMethods.
eFigure 1. CONSORT flow diagram.
eFigure 2. Plot showing CBD plasma levels in placebo and CBD arms.
eFigure 3. Acute effect of CBD on brain activation.
eResults.
eTable 1. Task-related activation during the encoding condition relative to baseline in healthy controls (n = 19).
eTable 2. Task-related activation during the recall condition relative to baseline in healthy controls (n = 19).
eDiscussion.