Key Points
Question
Is the quality of stroke care better at hospitals participating in Get With The Guidelines–Stroke?
Findings
In a longitudinal cohort study, 546 patients developed an ischemic stroke during follow-up. The odds of receiving 5 of 10 quality care metrics were higher among 207 patients admitted to a hospital participating in Get With The Guidelines–Stroke compared with 339 admitted to a nonparticipating hospital.
Meaning
These data collected independently of the Get With The Guidelines–Stroke program document were associated with increased frequency of many aspects of care quality for hospitalized patients with ischemic stroke at hospitals participating in Get With The Guidelines–Stroke.
Abstract
Importance
Get With The Guidelines–Stroke (GWTG-Stroke) is an American Heart Association/American Stroke Association stroke-care quality-improvement program; however, to our knowledge, there has not been a direct comparison of the quality of care between patients hospitalized at participating hospitals and those at nonparticipating hospitals.
Objective
To contrast quality of stroke care measures for patients admitted to hospitals participating and not participating in GWTG-Stroke.
Design, Setting, and Participants
Subpopulation of 546 participants with ischemic stroke occurring during a 9-year follow-up of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study, a population-based cohort study of 30 239 randomly selected black and white participants 45 years and older recruited between 2003 and 2007. Of those with stroke, 207 (36%) were treated in a hospital participating in GWTG-Stroke and 339 in a nonparticipating hospital. Data were analyzed between July 29, 2017, and April 17, 2018.
Main Outcomes and Measures
Quality of care measures including use of tissue plasminogen activator, performance of swallowing evaluation, antithrombotic use in first 48 hours, lipid profile assessment, discharge receiving antithrombotic therapy, discharge receiving a statin, neurologist evaluation, providing weight loss and exercise counseling, education on stroke risk factors and warning signs, and assessment for rehabilitation.
Results
Participants treated at participating hospitals had a mean (SD) age of 74 (8) years and 100 of 207 were men (48%), while those seen at nonparticipating hospitals had a mean (SD) age of 73 (9) years, and 161 of 339 were men (48%). Those seen in participating hospitals were more likely to receive 5 of 10 evidence-based interventions recommended for patients hospitalized with ischemic stroke, including receiving tissue plasminogen activator (RR, 3.74; 95% CI, 1.65-8.50), education on risk factors (RR, 1.54; 95% CI, 1.16-2.05), having an evaluation for swallowing (RR, 1.25; 95% CI, 1.04-1.50), a lipid evaluation (RR, 1.18; 95% CI, 1.05-1.32), and an evaluation by a neurologist (RR, 1.12; 95% CI, 1.05-1.20). Those seen in participating hospitals received a mean of 5.4 (95% CI, 5.2-5.6) interventions compared with 4.8 (95% CI, 4.6-5.0) in nonparticipating hospitals (P < .001).
Conclusions and Relevance
These data collected independently of the GWTG-Stroke program document improved stroke care for patients with ischemic stroke hospitalized at participating hospitals.
This longitudinal cohort study compares quality of stroke care measures for patients admitted to hospitals participating and not participating in Get With The Guidelines–Stroke.
Introduction
Get With The Guidelines–Stroke (GWTG-Stroke) was developed by the American Heart Association/American Stroke Association as a stroke-care quality-improvement program and as a national stroke registry, based on prior successful work in coronary artery disease treatment.1,2 The program uses the Patient Management Tool (PMT), an online, interactive assessment tool developed by Quintiles Real World and Late Phase Research to improve stroke care and secondary prevention through increasing compliance with published guideline recommendations.3 These guidelines include use of tissue plasminogen activator (tPA) in eligible patients, early use of antithrombotic medication, prophylaxis for deep vein thrombosis, discharge on antithrombotic medications and anticoagulation medications (for those with atrial fibrillation), smoking cessation intervention, assessment and management of low-density lipoproteins, weight counseling, and screening for dysphagia.
Get With The Guidelines–Stroke has been implemented in more than 2000 hospitals, treating approximately half of the patients discharged with stroke in the United States.4 Temporal improvement in the proportion adherent to the measures of stroke care quality has been shown following implementation, with increases in guideline adherence in most or all guidelines in hospitals regardless of the size or teaching status of the hospital.2,5,6 These same hospitals have shown improvements in hospital outcomes such as reduced length of stay and improvements in risk-adjusted in-hospital mortality.6 The validity of these findings appears strong because concerns that the observed improvements are truly occurring and not a product of a bias introduced through better record keeping have been addressed.7 Finally, the proportion of patients discharged to home, 30-day mortality, and 1-year mortality for patients admitted to GWTG-Stroke hospitals have been shown to be better than the outcomes of patients admitted to matched hospitals not participating in GWTG-Stroke.8 These successes of the program have been acknowledged by the implementation of similar programs in other countries.9
However, it is not clear whether the temporal improvements in guideline adherence for the GWTG-Stroke hospitals result from the implementation of the program at these specific hospitals or whether there is a national upturn of acceptance for guidelines that is improving care at all hospitals (including those participating in GWTG-Stroke). While temporal improvement in guideline adherence in GWTG hospitals has been well documented,2,5,6 to our knowledge, there are no similar data on quality of care in non–GWTG-Stroke hospitals (ie, control hospitals). As such, data collected as part of the GWTG-Stroke program cannot be used alone to document better care compared with non–GWTG-Stroke hospitals. The goal of this study was to use national data describing hospital care quality that were collected independently of the GWTG-Stroke program to assess the association of the GWTG-Stroke program with the quality of care of patients with stroke.
Methods
The SAS code used for this analysis is available through written agreement with authors from the corresponding author, and the data set is available through a data use agreement with University of Alabama at Birmingham. The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study is a longitudinal cohort study that enrolled 30 239 community-dwelling black and white participants 45 years and older from across the continental United States. Potential participants were selected from a commercially available list and were recruited through a combination of mail and telephone contact. Information on demographics, medical history, cerebrovascular risk factors, and psychosocial measures was collected using a structured interview. An in-person examination was conducted approximately 2 to 3 weeks later and included collection of height, weight, waist circumference, blood pressure, venipuncture and urine collection, and an electrocardiogram.10
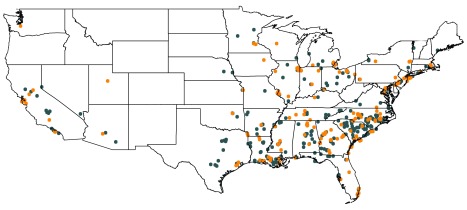
Participants were then contacted at 6-month intervals for ascertainment of suspected stroke events. Hospital records were retrieved and reviewed for stroke adjudication and abstracted for information describing stroke care. Exclusions included medical records with insufficient information for review, those with discharge from the emergency department or seen only in the outpatient setting (not admitted to the hospital), those dying during stroke hospitalization or who were discharged to hospice, or those who had evidence of joining and then leaving the GWTG-Stroke program (n = 16 events), collectively resulting in 546 adjudicated ischemic strokes in the analysis. The residential location for these participants is shown in the Figure. The name and American Hospital Association hospital code for the treating hospital was matched with information from the GWTG-Stroke program to classify each hospital as participating or not participating with the GWTG-Stroke program at the time of the patient admission. There were 14 participants (2.6%) who were admitted to 1 hospital and transferred to a different hospital, and receiving the stroke intervention was considered positive if they received it at either hospital. Being a resident of the Stroke Belt was defined as residence in North Carolina, South Carolina, Georgia, Tennessee, Alabama, Mississippi, Arkansas, or Louisiana. Education and income status were self-reported.
Figure. Residential Location of Reasons for Geographic and Racial Differences in Stroke Participants in Analysis.
Orange represents admission to a Get With The Guidelines–Stroke (GWTG-Stroke) hospital and blue represents admission to a non–GWTG-Stroke hospital. A large number of admissions in major urban centers are overlaid.
Written informed consent was obtained at the follow-up in-home examination for all participants. Study methods were reviewed and approved by institutional review boards at the University of Alabama at Birmingham, the University of Cincinnati, Cincinnati, Ohio, and the University of Vermont.
The outcomes for this report are 10 stroke care interventions, most of which are also targeted for improvement by GWTG-Stroke. The retrieved medical records were abstracted to assess whether these interventions were met, with confirmation by 2 authors (K.C.A. and J.D.R.). Table 1 provides these metrics, along with the justification for inclusion in this report. The denominator was all patients with ischemic stroke; this differs from GWTG program quality metrics where the denominator is instead limited to patients eligible for the specific intervention (for example, the proportion receiving tPA among those eligible for treatment). The review was performed blinded to whether the hospital participated in GWTG-Stroke.
Table 1. Stroke Care Interventions With Justification Using Criteria Proposed by Get With The Guidelines–Stroke.
| Stroke Intervention Measure | Justificationa |
|---|---|
| Was IV tPA administered? | Proxy for stroke reporting measure: acute |
| Was there documentation of a swallowing evaluation? | Stroke quality measure: acute |
| Was there documentation of the patient receiving an antithrombotic in the first 48 h? | Stroke achievement measure: acute |
| Was there documentation of the lipid profile being checked? | Proxy for stroke quality measure: at or by discharge, “LDL documented” |
| Was there documentation of the patient being discharged receiving an antithrombotic? | Stroke achievement measure: at or by discharge |
| Was there documentation of the patient being discharged receiving a statin? | Proxy for stroke quality measure: at or by discharge, “intensive statin therapy” |
| Was there documentation of a neurologist's evaluation? | Stroke intervention suggested by authors |
| Was there documentation of the patient receiving weight loss and exercise recommendations? | Proxy for stroke quality measure: at or by discharge, “weight recommendation” |
| Was there documentation of the patient receiving stroke education on risk factors, warning signs, or how to activate EMS? | Stroke quality measure: at or by discharge |
| Was there documentation of the patient being assessed for rehabilitation services? | Stroke quality measure: at or by discharge |
Abbreviations: EMS, emergency medical services; IV, intravenous; LDL, low-density lipoprotein; tPA, tissue plasminogen activator.
Justifications using criteria proposed in the American Heart Association/American Stroke Association Stroke Fact Sheet.11
The proportion of patients receiving each of 10 stroke interventions was calculated among the participants with stroke treated at hospitals with and without participation in GWTG-Stroke. Poisson regression (with robust variance estimates) was used to provide crude relative risk for participants meeting each of the quality indicators and to provide estimated relative risk after adjustment for: (1) participant or hospital differences for those seen (and not seen) at GWTG-Stroke hospitals (age, sex, stroke belt residence, number of hospital beds [tertile], and the presence of Graduate Medical Education residency training programs [as a measure of the technical sophistication of the hospital]) and (2) temporal change in the stroke care with further adjustment for the year of the stroke event. Linear regression was used to assess differences in the mean number of stroke interventions received after adjustment for the same factors. Sensitivity analysis was conducted using generalized estimation equations to account for clustering of study participants in a hospital. Two-sided statistical tests and confidence bounds at the α = .05 level were used, and analysis was performed using SAS, version 9.4 (SAS Institute Inc).
Results
Between 2003 and 2015, 207 of 546 REGARDS participants (38%) experiencing an ischemic stroke were treated in a hospital currently participating in the GWTG-Stroke program, with the remainder in a non–GWTG-Stroke hospital. The characteristics of the population are provided in Table 2, where those hospitalized in a GWTG-Stroke hospital were of similar age, race/ethnicity, sex, and risk factor profile as those in a non–GWTG-Stroke hospital; however, fewer residents of the Stroke Belt were treated in a GWTG hospital (n = 97 of 207 [46.9%] vs n = 206 of 339 [60.8%]; P = .002). Data on outcomes were available in all participants, with the exception of 1 patient where it could not be determined whether they received stroke education on risk factors and warning signs, 2 patients where counseling for weight loss and exercise could not be determined, and 3 patients where it could not be determined whether a lipid profile was performed. Compared with the hospitals where participants did not receive GWTG-Stroke care, the hospitals where participants received GWTG-Stroke care tended to have a larger number of beds, have a higher daily census, have more Medicare and Medicaid discharges, and participate in resident training (Table 3).
Table 2. Baseline Demographics of 546 Participants Admitted for Ischemic Stroke Who Were and Were Not Treated at GWTG-Stroke Hospitals.
| Characteristic | No. (%) | P Value | |
|---|---|---|---|
| Not Treated at GWTG-Stroke Hospital (n = 339) | Treated at GWTG-Stroke Hospital (n = 207) | ||
| Age, mean (SD), y | 73 (9) | 74 (8) | .31 |
| Age ≥65 y | 281 (82.9) | 183 (88.4) | .08 |
| African American/black | 148 (43.7) | 93 (44.9) | .77 |
| Men | 161 (47.5) | 100 (48.3) | .85 |
| History | |||
| Hypertension | 302 (89.1) | 179 (86.5) | .36 |
| Dyslipidemia | 299 (88.2) | 178 (86.0) | .45 |
| Diabetes mellitus | 126 (37.2) | 86 (41.5) | .31 |
| Coronary artery disease | 132 (38.9) | 84 (40.6) | .70 |
| Chronic kidney disease | 66 (19.5) | 47 (22.7) | .37 |
| Impaired cognition | 48 (14.2) | 26 (12.6) | .60 |
| Current smoker | 68 (20.1) | 44 (21.3) | .74 |
| Resident of the Stroke Belt | 206 (60.8) | 97 (46.9) | .002 |
| ≥High school education | 277 (82.0) | 177 (85.5) | .28 |
| Income < $20 000 | 76 (22.4) | 44 (21.3) | .75 |
Abbreviaton: GWTG-Stroke, Get With The Guidelines–Stroke.
Table 3. Characteristics of Hospitals to Which Participants Were Admitted for Ischemic Stroke by GWTG-Stroke Status.
| Characteristic | Median (IQR) | P Value | |
|---|---|---|---|
| Not Treated at GWTG-Stroke Hospital (n = 339) | Treated at GWTG-Stroke Hospital (n = 207) | ||
| Beds, total No. | 289 (149-460) | 425 (286-640) | <.001 |
| Mean daily census | 185 (95-319) | 294 (198-500) | <.001 |
| Medicare inpatient discharges | 6108 (2828-9049) | 9282 (6059-13 360) | <.001 |
| Medicaid inpatient discharges | 2127 (799-4226) | 3595 (1637-6431) | <.001 |
| Resident training approved by the Council for Graduate Medical Education, No. (%) | 138 (40.7) | 122 (58.9) | <.001 |
Abbreviations: GWTG-Stroke, Get With The Guidelines–Stroke; IQR, interquartile range.
Table 4 describes the differences in the likelihood of receiving 10 stroke interventions in a hospital participating vs not participating with GWTG-Stroke. Compared with hospitalization in a hospital not participating with GWTG-Stroke, REGARDS participants with ischemic stroke who were hospitalized in a GWTG-Stroke hospital were much more likely to receive tPA (19 of 207 [9.2%] vs 8 of 339 [2.4%]; model 1 RR, 3.74; 95% CI, 1.65-8.50), receive education on stroke risk factors (70 of 207 [33.8%] vs 77 of 338 [22.8%]; model 1 RR, 1.54; 95% CI, 1.16-2.05), be evaluated by a neurologist (189 of 207 [91.3%] vs 268 of 339 [79.1%]; model 1 RR, 1.12; 95% CI, 1.05-1.20), have a lipid profile performed (159 of 207 [76.8%] vs 215 of 336 [64.0%]; model 1 RR, 1.18; 95% CI, 1.05-1.32), and have a swallowing evaluation (113 of 207 [54.6%] vs 140 of 339 [41.3%]; model 1 RR, 1.25; 95% CI, 1.04-1.50). Further adjustment for year of the stroke (model 2) did not affect the interpretation of any of the estimated adjusted associations. While it failed to reach the formal level of statistical significance, participants hospitalized in a GWTG-Stroke hospital were more likely to receive a statin on discharge (144 of 207 [69.6%] vs 211 of 339 [62.2%]; model 1 RR, 1.10; 95% CI, 0.97-1.24).
Table 4. Proportion of Patients With Ischemic Stroke Meeting 10 Stroke Quality of Care Indicators for Patients Admitted to Hospitals Participating and Not Participating With GWTG-Strokea.
| Characteristic | No. (%) | P Value | RR (95% CI) | |||
|---|---|---|---|---|---|---|
| Not Treated at GWTG-Stroke Hospital (n = 339) | Treated at GWTG-Stroke Hospital (n = 207) | Crude RR | Model 1b | Model 2c | ||
| Was IV tPA administered? | 8 (2.4) | 19 (9.2) | <.001 | 3.89 (1.73-8.72) | 3.74 (1.65-8.50) | 3.84 (1.69-8.76) |
| Was there documentation of a swallowing evaluation? | 140 (41.3) | 113 (54.6) | .003 | 1.32 (1.11-1.58) | 1.25 (1.04-1.50) | 1.24 (1.03-1.50) |
| Was there documentation of the patient receiving an antithrombotic in the first 48 h? | 295 (87.0) | 178 (86.0) | .73 | 0.99 (0.92-1.06) | 0.99 (0.93-1.06) | 0.99 (0.93-1.06) |
| Was there documentation of the lipid profile being checked? | 215 (64.0) | 159 (76.8) | .002 | 1.20 (1.08-1.34) | 1.18 (1.05-1.32) | 1.15 (1.03-1.30) |
| Was there documentation of the patient being discharged receiving an antithrombotic? | 310 (91.4) | 191 (92.3) | .734 | 1.01 (0.96-1.06) | 1.01 (0.96-1.07) | 1.01 (0.95-1.06) |
| Was there documentation of the patient being discharged receiving a statin? | 211 (62.2) | 144 (69.6) | .082 | 1.12 (0.99-1.26) | 1.10 (0.97-1.24) | 1.00 (0.88-1.13) |
| Was there documentation of a neurologist's evaluation? | 268 (79.1) | 189 (91.3) | <.001 | 1.15 (1.08-1.24) | 1.12 (1.05-1.20) | 1.10 (1.03-1.18) |
| Was there documentation of the patient receiving weight loss and exercise recommendations? | 59 (17.5) | 31 (15.0) | .464 | 0.86 (0.58-1.28) | 0.91 (0.60-1.37) | 0.96 (0.63-1.47) |
| Was there documentation of the patient receiving stroke education on risk factors, warning signs, how to activate EMS, etc? | 77 (22.8) | 70 (33.8) | .005 | 1.48 (1.13-1.95) | 1.54 (1.16-2.05) | 1.42 (1.06-1.90) |
| Was there documentation of the patient being assessed for rehabilitation services? | 258 (76.1) | 161 (77.8) | .654 | 1.02 (0.93-1.12) | 0.99 (0.90-1.08) | 1.00 (0.91-1.11) |
Abbreviations: EMS, emergency medical services; GWTG-Stroke, Get With The Guidelines–Stroke; REGARDS, Reasons for Geographic and Racial Differences in Stroke; RR, relative risk.
Both crude and adjusted relative risk (with 95% CI) hospitals (n = 207) as compared with non–GWTG-Stroke hospitals (n = 339) among REGARDS participants admitted for ischemic stroke.
Model 1: adjusted for age, sex, Stroke Belt residence, number of hospital beds (tertile), and the presence of approved Graduate Medical Education residency training programs.
Model 2: further adjusted for year of stroke.
There was no evidence of an increased likelihood of receiving an antithrombotic medication within 48 hours (178 of 207 [86.0%] vs 295 of 339 [87.0%]; model 1 RR, 0.99; 95% CI, 0.93-1.06), being discharged receiving an antithrombotic (191 of 207 [92.3%] vs 310 of 339 [91.5%]; model 1 RR, 1.01; 95% CI, 0.96-1.07), receiving weight-loss counseling (31 of 206 [15.1%] vs 59 of 338 [17.5%]; model 1 RR, 0.91; 95% CI, 0.60-1.37), or being assessed for rehabilitation services (161 of 207 [77.8%] vs 258 of 339 [76.1%]; model 1 RR, 0.99; 95% CI, 0.90-1.08). The sensitivity analysis using generalized estimation equations techniques provided results that did not affect the interpretation of the findings (eTable in the Supplement).
Those discharged from a GWTG-Stroke hospital received a mean of 5.4 (95% CI, 5.2-5.6) guideline-recommended interventions, while those discharged from a non–GWTG-Stroke hospital received 4.8 (95% CI, 4.6-5.0; P < .001). The least squares means (SE) (after adjustment for age, sex, Stroke Belt residence, number of hospital beds [tertile], and the presence of Graduate Medical Education residency training programs) for the number of interventions were 5.3 (0.1) and 4.8 (0.1) respectively, a difference that remained highly significant (P < .001).
Discussion
For 5 of 10 interventions for patients with ischemic stroke, the likelihood of receiving that care was significantly higher for those REGARDS participants hospitalized at an institution participating in GWTG-Stroke. In addition, there was marginally significant evidence that an additional stroke intervention, statin use, was more frequently provided in GWTG-Stroke hospitals. Many of these interventions were targeted by GWTG-Stroke and suggesting that the program was effective in achieving improvements in health care delivery for stroke. Those seen at a participating hospital received 0.6 more stroke care interventions, a significant increase in the mean number of interventions from 4.8 to 5.4. This improvement is clearly statistically significant; however, it could be argued that it represents only a modest increase in the mean number of interventions delivered. Still, these data suggest that GWTG-Stroke participation may increase the likelihood that stroke care will meet standards of stroke interventions.
Among the 4 interventions not showing improvement in GWTG-Stroke hospitals, 3 had a high proportion of patients in non–GWTG-stroke hospitals already receiving the intervention. This high rate in the non–GWTG-Stroke hospitals may have acted as a ceiling effect, where improvement was difficult for receiving antithrombotic treatment (87% in the non–GWTG-Stroke hospitals), discharge receiving antithrombotic therapy (91%), and assessment for rehabilitation services (76%).
On a relative basis, the most dramatic difference associated with admission to a GWTG-Stroke hospital was for tPA use, where the relative risk of use was nearly 4 times higher for patients treated at a participating GWTG-Stroke hospital. However, tPA was still only used in less than 10% of the patients. It is likely that many of those where tPA was not used were not eligible for its use, a factor that is challenging to assess from medical records. Relatively large differences on an absolute scale (greater than 10%) were observed for the other stroke interventions. Adjustment for the year of stroke to account for potential temporal changes in the use of interventions did not change the interpretation of the associations.
One corollary of the observed differences in care in the GWTG-Stroke hospitals is that the data collected from GWTG-Stroke on the care of patients (and their outcomes) should not be generalized to represent the state of care in the United States. As previously noted, it is clear that patients cared for at a GWTG-Stroke participating hospital receive better care and have better outcomes,8 but not all patients are cared for at these hospitals. Currently, only approximately 50% of patients with stroke are treated at participating GWTG-Stroke hospitals4; therefore, a sizable proportion of the patients with stroke in the United States are receiving care and have outcomes that are not as good as that received at GWTG-Stroke participating hospitals.
Strengths and Limitations
The greatest strength of this study is that REGARDS participants were randomly sampled from across the continental United States (with oversampling of residents of the stroke belt and black individuals) and had residences in 1866 of the approximate 3000 counties in the United States.12 The REGARDS study did not play any role in guiding or suggesting a hospital for stroke care; therefore, the hospitals at which REGARDS participants were treated likely reflect a general sample of hospitals from across the nation. Perhaps the greatest limitation of the study was the need to rely on medical record evidence to assess whether the participant received the intervention. While the previous reports from GWTG-Stroke investigators also relied on medical record review, specific data collection is focused on determining eligibility, exclusions, and exceptions for quality metrics. In contrast, in this study, the heterogeneity of medical records from the array of hospitals across the nation made the assessment of care quality for this report more of a challenge. In some cases, there was insufficient documentation to construct a valid measure of an intervention, such as those receiving counseling for smoking cessation.
Conclusions
In summary, REGARDS data, completely independent from the GWTG-Stroke system, document dramatically higher quality of care provided by hospitals participating in the GWTG-Stroke program relative to those hospitals not participating in the GWTG-Stroke program. Additional efforts to enhance hospital participation in GWTG-Stroke may have meaningful benefits in stroke care and outcomes.
eTable. Estimates Calculated Using GEE
References
- 1.LaBresh KA, Gliklich R, Liljestrand J, Peto R, Ellrodt AG. Using “get with the guidelines” to improve cardiovascular secondary prevention. Jt Comm J Qual Saf. 2003;29(10):539-550. [DOI] [PubMed] [Google Scholar]
- 2.LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the “Get With The Guidelines” program. Arch Intern Med. 2008;168(4):411-417. [DOI] [PubMed] [Google Scholar]
- 3.American Heart Association/American Stroke Association Get With the Guidelines-Stroke: patient management tool. http://www.heart.org/HEARTORG/Professional/GetWithTheGuidelines/GetWithTheGuidelines-Stroke/Get-With-The-Guidelines-Stroke-Patient-Management-Tool_UCM_308035_Article.jsp#.Wbmc01F97D4. Accessed October 30, 2017.
- 4.Ormseth CH, Sheth KN, Saver JL, Fonarow GC, Schwamm LH. The American Heart Association’s Get With the Guidelines (GWTG)-Stroke development and impact on stroke care. Stroke Vasc Neurol. 2017;2(2):94-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwamm LH, Fonarow GC, Reeves MJ, et al. . Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119(1):107-115. [DOI] [PubMed] [Google Scholar]
- 6.Fonarow GC, Reeves MJ, Smith EE, et al. ; GWTG-Stroke Steering Committee and Investigators . Characteristics, performance measures, and in-hospital outcomes of the first one million stroke and transient ischemic attack admissions in get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes. 2010;3(3):291-302. [DOI] [PubMed] [Google Scholar]
- 7.Reeves MJ, Grau-Sepulveda MV, Fonarow GC, Olson DM, Smith EE, Schwamm LH. Are quality improvements in the get with the guidelines: stroke program related to better care or better data documentation? Circ Cardiovasc Qual Outcomes. 2011;4(5):503-511. [DOI] [PubMed] [Google Scholar]
- 8.Song S, Fonarow GC, Olson DM, et al. . Association of Get With The Guidelines-Stroke program participation and clinical outcomes for medicare beneficiaries with ischemic stroke. Stroke. 2016;47(5):1294-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsieh FI, Jeng JS, Chern CM, et al. ; BTS-Stroke Investigators . Quality improvement in acute ischemic stroke care in taiwan: the breakthrough collaborative in stroke. PLoS One. 2016;11(8):e0160426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howard VJ, Cushman M, Pulley L, et al. . The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135-143. [DOI] [PubMed] [Google Scholar]
- 11.American Heart Association/American Stroke Association Stroke fact sheet. https://www.heart.org/idc/groups/ahaecc-public/@wcm/@gwtg/documents/downloadable/ucm_491528.pdf. Accessed June 25, 2018.
- 12.Howard G. Ancel Keys Lecture: adventures (and misadventures) in understanding (and reducing) disparities in stroke mortality. Stroke. 2013;44(11):3254-3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Estimates Calculated Using GEE